Mediterranean Diet in Developmental Age: A Narrative Review of Current Evidences and Research Gaps
Abstract
:1. Introduction
2. Material and Methods
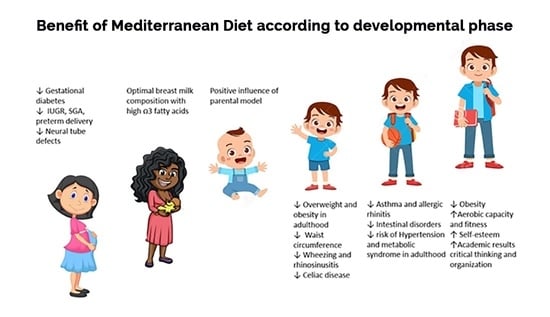
3. MD and Pregnancy
4. Mediterranean Diet, Nursing, and Weaning
5. MD in Preschool Age
6. MD in School Children
7. MD in Adolescents
8. Discussion and Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet. Lit. Rev. 2015, 7, 9139–9153. [Google Scholar]
- Brown, T.; Moore, T.H.M.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 7, CD001871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martorell, R. Improved nutrition in the first 1000 days and adult human capital and health. Am. J. Hum. Biol. 2017, 29, e22952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stewart-Brown, S.L.; Fletcher, L.; Wadsworth, M.E.J. Parent–child relationships and health problems in adulthood in three UK national birth cohort studies. Eur. J. Public Health 2005, 15, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Rossiter, C.; Cheng, H.; Appleton, J.; Campbell, K.J.; Denney-Wilson, E. Addressing obesity in the first 1000 days in high risk infants: Systematic review. Matern. Child Nutr. 2021, 17, e13178. [Google Scholar] [CrossRef]
- Morais Lopez, A.; Martinez Suarez, V.; Dalmau Serra, J.; Martinez Gomez, M.J.; Pena-Quintana, L.; Varea Calderon, V. Nutritional problems perceived by pediatricians in Spanish children younger than 3 years. Nutr. Hosp. 2012, 27, 2028–2047. [Google Scholar] [CrossRef] [Green Version]
- Richards, D.; Caldwell, P.H.; Go, H. Impact of social media on the health of children and young people. J. Paediatr. Child Health 2015, 51, 1152–1157. [Google Scholar] [CrossRef]
- Carlson, J.A.; Crespo, N.C.; Sallis, J.F.; Patterson, R.E.; Elder, J.P. Dietary-related and physical activity-related predictors of obesity in children: A 2-year prospective study. Child Obes. 2012, 8, 110–115. [Google Scholar] [CrossRef] [Green Version]
- Arima, Y.; Fukuoka, H. Developmental origins of health and disease theory in cardiology. J. Cardiol. 2020, 76, 14–17. [Google Scholar] [CrossRef]
- Havaš Auguštin, D.; Šarac, J.; Lovrić, M.; Živković, J.; Malev, O.; Fuchs, N.; Novokmet, N.; Turkalj, M.; Missoni, S. Adherence to Mediterranean Diet and Maternal Lifestyle during Pregnancy: Island–Mainland Differentiation in the CRIBS Birth Cohort. Nutrients 2020, 12, 2179. [Google Scholar] [CrossRef]
- Gila-Díaz, A.; Witte Castro, A.; Herranz Carrillo, G.; Singh, P.; Yakah, W.; Arribas, S.M.; Ramiro-Cortijo, D. Assessment of Adherence to the Healthy Food Pyramid in Pregnant and Lactating Women. Nutrients 2021, 13, 2372. [Google Scholar] [CrossRef] [PubMed]
- Jardí, C.; Aparicio, E.; Bedmar, C.; Aranda, N.; Abajo, S.; March, G.; Basora, J.; Arija, V.; ECLIPSES Study Group. Food Consumption during Pregnancy and Post-Partum. ECLIPSES Study. Nutrients 2019, 11, 2447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brantsæter, A.L.; Olafsdottir, A.S.; Forsum, E.; Olsen, S.F.; Thorsdottir, I. Does milk and dairy consumption during pregnancy influence fetal growth and infant birthweight? A systematic literature review. Food Amp. Nutr. Res. 2012, 56, 20050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaragoza-Martí, A.; Ruiz-Ródenas, N.; Herranz-Chofre, I.; Sánchez-SanSegundo, M.; Serrano Delgado, V.d.l.C.; Hurtado-Sánchez, J.A. Adherence to the Mediterranean Diet in Pregnancy and Its Benefits on Maternal-Fetal Health: A Systematic Review of the Literature. Front. Nutr. 2022, 9, 813942. [Google Scholar] [CrossRef]
- Amati, F.; Hassounah, S.; Swaka, A. The Impact of Mediterranean Dietary Patterns During Pregnancy on Maternal and Offspring Health. Nutrients 2019, 11, 1098. [Google Scholar] [CrossRef] [Green Version]
- Biagi, C.; Di Nunzio, M.; Bordoni, A.; Gori, D.; Lanari, M. Effect of Adherence to Mediterranean Diet during Pregnancy on Children’s Health: A Systematic Review. Nutrients 2019, 11, 997. [Google Scholar] [CrossRef] [Green Version]
- Crovetto, F.; Crispi, F.; Casas, R.; Martín-Asuero, A.; Borràs, R.; Vieta, E.; Estruch, R.; Gratacós, E.; Investigators, I.B.T. Effects of Mediterranean Diet or Mindfulness-Based Stress Reduction on Prevention of Small-for-Gestational Age Birth Weights in Newborns Born to At-Risk Pregnant Individuals: The IMPACT BCN Randomized Clinical Trial. JAMA 2021, 326, 2150–2160. [Google Scholar] [CrossRef]
- Assaf-Balut, C.; García de la Torre, N.; Fuentes, M.; Durán, A.; Bordiú, E.; Del Valle, L.; Valerio, J.; Jiménez, I.; Herraiz, M.A.; Izquierdo, N.; et al. A High Adherence to Six Food Targets of the Mediterranean Diet in the Late First Trimester is Associated with a Reduction in the Risk of Materno-Foetal Outcomes: The St. Carlos Gestational Diabetes Mellitus Prevention Study. Nutrients 2019, 11, 66. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Galiano, J.M.; Olmedo-Requena, R.; Barrios-Rodríguez, R.; Amezcua-Prieto, C.; Bueno-Cavanillas, A.; Salcedo-Bellido, I.; Jimenez-Moleon, J.J.; Delgado-Rodríguez, M. Effect of Adherence to a Mediterranean Diet and Olive Oil Intake during Pregnancy on Risk of Small for Gestational Age Infants. Nutrients 2018, 10, 1234. [Google Scholar] [CrossRef] [Green Version]
- García de la Torre, N.; Assaf-Balut, C.; Jiménez Varas, I.; del Valle, L.; Durán, A.; Fuentes, M.; del Prado, N.; Bordiú, E.; Valerio, J.J.; Herraiz, M.A.; et al. Effectiveness of Following Mediterranean Diet Recommendations in the Real World in the Incidence of Gestational Diabetes Mellitus (GDM) and Adverse Maternal-Foetal Outcomes: A Prospective, Universal, Interventional Study with a Single Group. The St Carlos Study. Nutrients 2019, 11, 1210. [Google Scholar]
- Lorite Mingot, D.; Gesteiro, E.; Bastida, S.; Sánchez-Muniz, F.J. Epigenetic effects of the pregnancy Mediterranean diet adherence on the offspring metabolic syndrome markers. J. Physiol. Biochem. 2017, 73, 495–510. [Google Scholar] [CrossRef] [PubMed]
- Bedard, A.; Northstone, K.; Henderson, A.J.; Shaheen, S.O. Mediterranean diet during pregnancy and childhood respiratory and atopic outcomes: Birth cohort study. Eur. Respir. J. 2020, 55, 1901215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mennella, J.A.; Jagnow, C.P.; Beauchamp, G.K. Prenatal and postnatal flavor learning by human infants. Pediatrics 2001, 107, E88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boss, M.; Gardner, H.; Hartmann, P. Normal Human Lactation: Closing the gap. F1000Research 2018, 7, 801. [Google Scholar] [CrossRef] [Green Version]
- Farella, I.; Panza, R.; Baldassarre, M.E. The Difficult Alliance between Vegan Parents and Pediatrician: A Case Report. Int. J. Environ. Res. Public Health 2020, 17, 6380. [Google Scholar] [CrossRef] [PubMed]
- Baldassarre, M.E.; Panza, R.; Farella, I.; Posa, D.; Capozza, M.; Mauro, A.D.; Laforgia, N. Vegetarian and Vegan Weaning of the Infant: How Common and How Evidence-Based? A Population-Based Survey and Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 4835. [Google Scholar] [CrossRef]
- Gila-Díaz, A.; Arribas, S.M.; López de Pablo, Á.L.; López-Giménez, M.R.; Phuthong, S.; Ramiro-Cortijo, D. Development and Validation of a Questionnaire to Assess Adherence to the Healthy Food Pyramid in Spanish Adults. Nutrients 2020, 12, 1656. [Google Scholar] [CrossRef]
- Gila-Díaz, A.; Díaz-Rullo Alcántara, N.; Herranz Carrillo, G.; Singh, P.; Arribas, S.M.; Ramiro-Cortijo, D. Multidimensional Approach to Assess Nutrition and Lifestyle in Breastfeeding Women during the First Month of Lactation. Nutrients 2021, 13, 1766. [Google Scholar] [CrossRef]
- Bravi, F.; Di Maso, M.; Eussen, S.R.B.M.; Agostoni, C.; Salvatori, G.; Profeti, C.; Tonetto, P.; Quitadamo, P.A.; Kazmierska, I.; Vacca, E.; et al. Dietary Patterns of Breastfeeding Mothers and Human Milk Composition: Data from the Italian MEDIDIET Study. Nutrients 2021, 13, 1722. [Google Scholar] [CrossRef]
- Perez Rodrigo, C.; Aranceta, J.; Salvador, G.; Varela-Moreiras, G. Food frequency questionnaires. Nutr. Hosp. 2015, 31 (Suppl. S3), 49–56. [Google Scholar] [CrossRef]
- Mazzocchi, A.; De Cosmi, V.; Scaglioni, S.; Agostoni, C. Towards a More Sustainable Nutrition: Complementary Feeding and Early Taste Experiences as a Basis for Future Food Choices. Nutrients 2021, 13, 2695. [Google Scholar] [CrossRef] [PubMed]
- Netting, M.J.; Middleton, P.F.; Makrides, M. Does maternal diet during pregnancy and lactation affect outcomes in offspring? A systematic review of food-based approaches. Nutrition 2014, 30, 1225–1241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Notario-Barandiaran, L.; Valera-Gran, D.; Gonzalez-Palacios, S.; Garcia-de-la-Hera, M.; Fernández-Barrés, S.; Pereda-Pereda, E.; Fernández-Somoano, A.; Guxens, M.; Iñiguez, C.; Romaguera, D.; et al. High adherence to a mediterranean diet at age 4 reduces overweight, obesity and abdominal obesity incidence in children at the age of 8. Int. J. Obes. 2020, 44, 1906–1917. [Google Scholar] [CrossRef] [PubMed]
- Arenaza, L.; Medrano, M.; Oses, M.; Amasene, M.; Díez, I.; Rodríguez-Vigil, B.; Labayen, I. The Effect of a Family-Based Lifestyle Education Program on Dietary Habits, Hepatic Fat and Adiposity Markers in 8–12-Year-Old Children with Overweight/Obesity. Nutrients 2020, 12, 1443. [Google Scholar] [CrossRef]
- Castro-Rodriguez, J.A.; Garcia-Marcos, L.; Alfonseda Rojas, J.D.; Valverde-Molina, J.; Sanchez-Solis, M. Mediterranean diet as a protective factor for wheezing in preschool children. J. Pediatr. 2008, 152, 823–828.e2. [Google Scholar] [CrossRef]
- Calatayud-Sáez, F.M.; Calatayud, B.; Calatayud, A. Effects of the Traditional Mediterranean Diet in Patients with Otitis Media with Effusion. Nutrients 2021, 13, 2181. [Google Scholar] [CrossRef]
- Barroso, M.; Beth, S.A.; Voortman, T.; Jaddoe, V.W.V.; van Zelm, M.C.; Moll, H.A.; Kiefte-de Jong, J.C. Dietary Patterns After the Weaning and Lactation Period Are Associated with Celiac Disease Autoimmunity in Children. Gastroenterology 2018, 154, 2087–2096.e7. [Google Scholar] [CrossRef] [Green Version]
- Sotos-Prieto, M.; Santos-Beneit, G.; Pocock, S.; Redondo, J.; Fuster, V.; Penalvo, J.L. Parental and self-reported dietary and physical activity habits in pre-school children and their socio-economic determinants. Public Health Nutr. 2015, 18, 275–285. [Google Scholar] [CrossRef] [Green Version]
- Pereira-da-Silva, L.; Rêgo, C.; Pietrobelli, A. The Diet of Preschool Children in the Mediterranean Countries of the European Union: A Systematic Review. Int. J. Environ. Res. Public Health 2016, 13, 572. [Google Scholar] [CrossRef] [Green Version]
- Roset-Salla, M.; Ramon-Cabot, J.; Salabarnada-Torras, J.; Pera, G.; Dalmau, A. Educational intervention to improve adherence to the Mediterranean diet among parents and their children aged 1–2 years. EniM clinical trial. Public Health Nutr. 2016, 19, 1131–1144. [Google Scholar] [CrossRef] [Green Version]
- Guthold, R.; Moller, A.B.; Adebayo, E.; Carvajal, L.; Ekman, C.; Fagan, L.; Ferguson, J.; Friedman, H.S.; Ba, M.G.; Hagell, A.; et al. Priority Areas for Adolescent Health Measurement. J. Adolesc. Health 2021, 68, 888–898. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino Idelson, P.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean Diet in children and adolescents: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Štefan, L.; Prosoli, R.; Juranko, D.; Čule, M.; Milinović, I.; Novak, D.; Sporiš, G. The Reliability of the Mediterranean Diet Quality Index (KIDMED) Questionnaire. Nutrients 2017, 9, 419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roccaldo, R.; Censi, L.; D’Addezio, L.; Toti, E.; Martone, D.; D’Addesa, D.; Cernigliaro, A.; Censi, L.; D’Addesa, D.; D’Amicis, A.; et al. Adherence to the Mediterranean diet in Italian school children (The ZOOM8 Study). Int. J. Food Sci. Nutr. 2014, 65, 621–628. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Ezzatvar, Y.; López-Gil, J.F.; Ramírez-Vélez, R.; Olloquequi, J.; Izquierdo, M. Is adherence to the Mediterranean diet associated with healthy habits and physical fitness? A systematic review and meta-analysis including 565 421 youths. Br. J. Nutr. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Tambalis, K.D.; Panagiotakos, D.B.; Moraiti, I.; Psarra, G.; Sidossis, L.S.; the ΕΥΖHΝ Study Group. Poor dietary habits in Greek schoolchildren are strongly associated with screen time: Results from the EYZHN (National Action for Children’s Health) Program. Eur. J. Clin. Nutr. 2018, 72, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Arnaoutis, G.; Georgoulis, M.; Psarra, G.; Milkonidou, A.; Panagiotakos, D.B.; Kyriakou, D.; Bellou, E.; Tambalis, K.D.; Sidossis, L.S. Association of Anthropometric and Lifestyle Parameters with Fitness Levels in Greek Schoolchildren: Results from the EYZHN Program. Front. Nutr. 2018, 5, 10. [Google Scholar] [CrossRef] [Green Version]
- De Batlle, J.; Garcia-Aymerich, J.; Barraza-Villarreal, A.; Antó, J.M.; Romieu, I. Mediterranean diet is associated with reduced asthma and rhinitis in Mexican children. Allergy 2008, 63, 1310–1316. [Google Scholar] [CrossRef]
- Gonzalez Barcala, F.J.; Pertega, S.; Bamonde, L.; Garnelo, L.; Perez Castro, T.; Sampedro, M.; Sanchez Lastres, J.; San Jose Gonzalez, M.A.; Lopez Silvarrey, A. Mediterranean diet and asthma in Spanish schoolchildren. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2010, 21, 1021–1027. [Google Scholar] [CrossRef]
- Agakidis, C.; Kotzakioulafi, E.; Petridis, D.; Apostolidou, K.; Karagiozoglou-Lampoudi, T. Mediterranean Diet Adherence is Associated with Lower Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents. Nutrients 2019, 11, 1283. [Google Scholar] [CrossRef] [Green Version]
- Archero, F.; Ricotti, R.; Solito, A.; Carrera, D.; Civello, F.; Di Bella, R.; Bellone, S.; Prodam, F. Adherence to the Mediterranean Diet among School Children and Adolescents Living in Northern Italy and Unhealthy Food Behaviors Associated to Overweight. Nutrients 2018, 10, 1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velázquez-López, L.; Santiago-Díaz, G.; Nava-Hernández, J.; Muñoz-Torres, A.V.; Medina-Bravo, P.; Torres-Tamayo, M. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatr. 2014, 14, 175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Ruiz, V.E.; Solé-Agustí, M.; Armero-Barranco, D.; Cauli, O. Weight Loss and Improvement of Metabolic Alterations in Overweight and Obese Children Through the I(2)AO(2) Family Program: A Randomized Controlled Clinical Trial. Biol. Res. Nurs. 2021, 23, 488–503. [Google Scholar] [CrossRef] [PubMed]
- Ojeda-Rodríguez, A.; Zazpe, I.; Morell-Azanza, L.; Chueca, M.J.; Azcona-Sanjulian, M.C.; Marti, A. Improved Diet Quality and Nutrient Adequacy in Children and Adolescents with Abdominal Obesity after a Lifestyle Intervention. Nutrients 2018, 10, 1500. [Google Scholar] [CrossRef] [Green Version]
- Lassale, C.; Fito, M.; Morales-Suarez-Varela, M.; Moya, A.; Gomez, S.F.; Schroder, H. Mediterranean diet and adiposity in children and adolescents: A systematic review. Obes. Rev. 2022, 23 (Suppl. S1), e13381. [Google Scholar] [CrossRef]
- Das, J.K.; Salam, R.A.; Thornburg, K.L.; Prentice, A.M.; Campisi, S.; Lassi, Z.S.; Koletzko, B.; Bhutta, Z.A. Nutrition in adolescents: Physiology, metabolism, and nutritional needs. Ann. N. Y. Acad. Sci. 2017, 1393, 21–33. [Google Scholar] [CrossRef]
- Peng, W.; Goldsmith, R.; Shimony, T.; Berry, E.M.; Sinai, T. Trends in the adherence to the Mediterranean diet in Israeli adolescents: Results from two national health and nutrition surveys, 2003 and 2016. Eur. J. Nutr. 2021, 60, 3625–3638. [Google Scholar] [CrossRef]
- Noale, M.; Nardi, M.; Limongi, F.; Siviero, P.; Caregaro, L.; Crepaldi, G.; Maggi, S. Adolescents in southern regions of Italy adhere to the Mediterranean diet more than those in the northern regions. Nutr. Res. 2014, 34, 771–779. [Google Scholar] [CrossRef]
- Jiménez Boraita, R.; Arriscado Alsina, D.; Gargallo Ibort, E.; Dalmau Torres, J.M. Factors associated with adherence to a Mediterranean diet in adolescents from La Rioja (Spain). Br. J. Nutr. 2020, 1–8. [Google Scholar] [CrossRef]
- Ozen, A.E.; Bibiloni Mdel, M.; Murcia, M.A.; Pons, A.; Tur, J.A. Adherence to the Mediterranean diet and consumption of functional foods among the Balearic Islands’ adolescent population. Public Health Nutr. 2015, 18, 659–668. [Google Scholar] [CrossRef] [Green Version]
- Mieziene, B.; Emeljanovas, A.; Novak, D.; Kawachi, I. The Relationship between Social Capital within Its Different Contexts and Adherence to a Mediterranean Diet Among Lithuanian Adolescents. Nutrients 2019, 11, 1332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamminen, N.; Reinikainen, J.; Appelqvist-Schmidlechner, K.; Borodulin, K.; Mäki-Opas, T.; Solin, P. Associations of physical activity with positive mental health: A population-based study. Ment. Health Phys. Act. 2020, 18, 100319. [Google Scholar] [CrossRef]
- Papadaki, S.; Mavrikaki, E. Greek adolescents and the Mediterranean diet: Factors affecting quality and adherence. Nutrition 2015, 31, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Goldsmith, R.; Berry, E.M. Demographic and lifestyle factors associated with adherence to the Mediterranean diet in relation to overweight/obesity among Israeli adolescents: Findings from the Mabat Israeli national youth health and nutrition survey. Public Health Nutr. 2017, 20, 883–892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novak, D.; Štefan, L.; Prosoli, R.; Emeljanovas, A.; Mieziene, B.; Milanović, I.; Radisavljević-Janić, S. Mediterranean Diet and Its Correlates among Adolescents in Non-Mediterranean European Countries: A Population-Based Study. Nutrients 2017, 9, 177. [Google Scholar] [CrossRef] [Green Version]
- Bibiloni Mdel, M.; Pich, J.; Córdova, A.; Pons, A.; Tur, J.A. Association between sedentary behaviour and socioeconomic factors, diet and lifestyle among the Balearic Islands adolescents. BMC Public Health 2012, 12, 718. [Google Scholar] [CrossRef] [Green Version]
- Antonogeorgos, G.; Panagiotakos, D.B.; Grigoropoulou, D.; Papadimitriou, A.; Anthracopoulos, M.; Nicolaidou, P.; Priftis, K.N. The mediating effect of parents’ educational status on the association between adherence to the Mediterranean diet and childhood obesity: The PANACEA study. Int. J. Public Health 2013, 58, 401–408. [Google Scholar] [CrossRef]
- Santos, R.; Moreira, C.; Abreu, S.; Lopes, L.; Ruiz, J.R.; Moreira, P.; Silva, P.; Mota, J. Parental education level is associated with clustering of metabolic risk factors in adolescents independently of cardiorespiratory fitness, adherence to the Mediterranean diet, or pubertal stage. Pediatr. Cardiol. 2014, 35, 959–964. [Google Scholar] [CrossRef]
- Vassiloudis, I.; Yiannakouris, N.; Panagiotakos, D.B.; Apostolopoulos, K.; Costarelli, V. Academic performance in relation to adherence to the Mediterranean diet and energy balance behaviors in Greek primary schoolchildren. J. Nutr. Educ. Behav. 2014, 46, 164–170. [Google Scholar] [CrossRef]
- Grosso, G.; Marventano, S.; Buscemi, S.; Scuderi, A.; Matalone, M.; Platania, A.; Giorgianni, G.; Rametta, S.; Nolfo, F.; Galvano, F.; et al. Factors associated with adherence to the Mediterranean diet among adolescents living in Sicily, Southern Italy. Nutrients 2013, 5, 4908–4923. [Google Scholar] [CrossRef] [Green Version]
- Cobo-Cuenca, A.I.; Garrido-Miguel, M.; Soriano-Cano, A.; Ferri-Morales, A.; Martínez-Vizcaíno, V.; Martín-Espinosa, N.M. Adherence to the Mediterranean Diet and Its Association with Body Composition and Physical Fitness in Spanish University Students. Nutrients 2019, 11, 2830. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galan-Lopez, P.; Sánchez-Oliver, A.J.; Ries, F.; González-Jurado, J.A. Mediterranean Diet, Physical Fitness and Body Composition in Sevillian Adolescents: A Healthy Lifestyle. Nutrients 2019, 11, 2009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agostinis-Sobrinho, C.; Santos, R.; Rosário, R.; Moreira, C.; Lopes, L.; Mota, J.; Martinkenas, A.; García-Hermoso, A.; Correa-Bautista, J.E.; Ramírez-Vélez, R. Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis. Nutrients 2018, 10, 815. [Google Scholar] [CrossRef] [Green Version]
- Chacón-Cuberos, R.; Zurita-Ortega, F.; Martínez-Martínez, A.; Olmedo-Moreno, E.M.; Castro-Sánchez, M. Adherence to the Mediterranean Diet Is Related to Healthy Habits, Learning Processes, and Academic Achievement in Adolescents: A Cross-Sectional Study. Nutrients 2018, 10, 1566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pelclová, J.; Štefelová, N.; Hodonská, J.; Dygrýn, J.; Gába, A.; Zając-Gawlak, I. Reallocating Time from Sedentary Behavior to Light and Moderate-to-Vigorous Physical Activity: What Has a Stronger Association with Adiposity in Older Adult Women? Int. J. Environ. Res. Public Health 2018, 15, 1444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teixeira, B.; Afonso, C.; Rodrigues, S.; Oliveira, A. Healthy and Sustainable Dietary Patterns in Children and Adolescents: A Systematic Review. Adv. Nutr. Bethesda Md 2021, nmab148. [Google Scholar] [CrossRef]
- Akhondzadeh, S. Personalized medicine: A tailor made medicine. Avicenna J. Med. Biotechnol. 2014, 6, 191. [Google Scholar]
- Piccini, P.; Montagnani, C.; de Martino, M. Gender disparity in pediatrics: A review of the current literature. Ital. J. Pediatr. 2018, 44, 1–6. [Google Scholar] [CrossRef]
- Eckl, M.R.; Brouwer-Brolsma, E.M.; Küpers, L.K. Maternal Adherence to the Mediterranean Diet during Pregnancy: A Review of Commonly Used a priori Indexes. Nutrients 2021, 13, 582. [Google Scholar] [CrossRef]
- Dalwood, P.; Marshall, S.; Burrows, T.L.; McIntosh, A.; Collins, C.E. Diet quality indices and their associations with health-related outcomes in children and adolescents: An updated systematic review. Nutr. J. 2020, 19, 118. [Google Scholar] [CrossRef]
- Tur, J.A.; Martinez, J.A. Guide and advances on childhood obesity determinants: Setting the research agenda. Obes. Rev. 2022, 23 (Suppl. S1), e13379. [Google Scholar] [CrossRef] [PubMed]
- De Filippo, C.; Cavalieri, D.; Di Paola, M.; Ramazzotti, M.; Poullet, J.B.; Massart, S.; Collini, S.; Pieraccini, G.; Lionetti, P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA 2010, 107, 14691–14696. [Google Scholar] [CrossRef] [Green Version]
- Del Chierico, F.; Vernocchi, P.; Dallapiccola, B.; Putignani, L. Mediterranean diet and health: Food effects on gut microbiota and disease control. Int. J. Mol. Sci. 2014, 15, 11678–11699. [Google Scholar] [CrossRef] [PubMed]
- Bawaked, R.A.; Gomez, S.F.; Homs, C.; Casas Esteve, R.; Cardenas, G.; Fíto, M.; Schröder, H. Association of eating behaviors, lifestyle, and maternal education with adherence to the Mediterranean diet in Spanish children. Appetite 2018, 130, 279–285. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farella, I.; Miselli, F.; Campanozzi, A.; Grosso, F.M.; Laforgia, N.; Baldassarre, M.E. Mediterranean Diet in Developmental Age: A Narrative Review of Current Evidences and Research Gaps. Children 2022, 9, 906. https://doi.org/10.3390/children9060906
Farella I, Miselli F, Campanozzi A, Grosso FM, Laforgia N, Baldassarre ME. Mediterranean Diet in Developmental Age: A Narrative Review of Current Evidences and Research Gaps. Children. 2022; 9(6):906. https://doi.org/10.3390/children9060906
Chicago/Turabian StyleFarella, Ilaria, Francesca Miselli, Angelo Campanozzi, Francesca Maria Grosso, Nicola Laforgia, and Maria Elisabetta Baldassarre. 2022. "Mediterranean Diet in Developmental Age: A Narrative Review of Current Evidences and Research Gaps" Children 9, no. 6: 906. https://doi.org/10.3390/children9060906