Ultrasound Shear Wave Elastography, Shear Wave Dispersion and Attenuation Imaging of Pediatric Liver Disease with Histological Correlation
Abstract
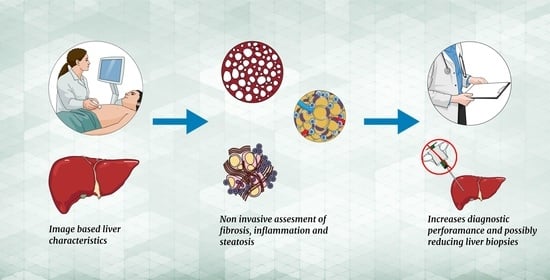
:1. Introduction
2. Materials and Methods
2.1. Liver Measurements
2.2. Histopathology Scoring
2.3. Grading of Fibrosis
2.4. Grading of Inflammation
2.5. Grading of Steatosis
2.6. Reliability Valuation
2.7. Statistics
3. Results
3.1. Patient Characteristics and Liver Measures
3.2. Liver Biomarkers and Histopathology
3.2.1. SWE
3.2.2. SWD
3.2.3. ATI
3.3. Image-Based Liver Biomarkers and Serological Markers
3.4. Patients with Increased Serological Liver Markers without an Established Liver Disease
3.5. Controls
3.6. Comparison between Patients and Controls
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Seth, A.; Orkin, S.; Yodoshi, T.; Liu, C.; Fei, L.; Hardy, J.; Trout, A.T.; Arce Clachar, A.C.; Bramlage, K.; Xanthakos, S. Severe obesity is associated with liver disease severity in pediatric non-alcoholic fatty liver disease. Pediatric Obes. 2020, 15, e12581. [Google Scholar] [CrossRef] [PubMed]
- Banc-Husu, A.M.; Bass, L.M. Transient Elastography in Pediatric Liver Disease. J. Pediatric Gastroenterol. Nutr. 2021, 73, 141–144. [Google Scholar] [CrossRef]
- Barr, R.G.; Ferraioli, G.; Palmeri, M.L.; Goodman, Z.D.; Garcia-Tsao, G.; Rubin, J.; Garra, B.; Myers, R.P.; Wilson, S.R.; Rubens, D.; et al. Elastography Assessment of Liver Fibrosis: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology 2015, 276, 845–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bravo, A.A.; Sheth, S.G.; Chopra, S. Liver biopsy. N. Engl. J. Med. 2001, 344, 495–500. [Google Scholar] [CrossRef]
- Alhashmi, G.H.; Gupta, A.; Trout, A.T.; Dillman, J.R. Two-dimensional ultrasound shear wave elastography for identifying and staging liver fibrosis in pediatric patients with known or suspected liver disease: A clinical effectiveness study. Pediatric Radiol. 2020, 50, 1255–1262. [Google Scholar] [CrossRef]
- Lee, S.; Choi, Y.H.; Cho, Y.J.; Lee, S.B.; Cheon, J.E.; Kim, W.S.; Ko, J.S.; Koh, J.; Kang, G.H. The usefulness of noninvasive liver stiffness assessment using shear-wave elastography for predicting liver fibrosis in children. BMC Med. Imaging 2021, 21, 68. [Google Scholar] [CrossRef]
- Trout, A.T.; Xanthakos, S.A.; Bennett, P.S.; Dillman, J.R. Liver Shear Wave Speed and Other Quantitative Ultrasound Measures of Liver Parenchyma: Prospective Evaluation in Healthy Children and Adults. AJR Am. J. Roentgenol. 2020, 214, 557–565. [Google Scholar] [CrossRef]
- Ormachea, J.; Parker, K.J.; Barr, R.G. An initial study of complete 2D shear wave dispersion images using a reverberant shear wave field. Phys. Med. Biol. 2019, 64, 145009. [Google Scholar] [CrossRef] [Green Version]
- Lipman, S.L.; Rouze, N.C.; Palmeri, M.L.; Nightingale, K.R. Impact of Acoustic Radiation Force Excitation Geometry on Shear Wave Dispersion and Attenuation Estimates. Ultrasound Med. Biol. 2018, 44, 897–908. [Google Scholar] [CrossRef]
- Chen, S.; Fatemi, M.; Greenleaf, J.F. Quantifying elasticity and viscosity from measurement of shear wave speed dispersion. J. Acoust. Soc. Am. 2004, 115, 2781–2785. [Google Scholar] [CrossRef]
- Chen, S.; Urban, M.W.; Pislaru, C.; Kinnick, R.; Greenleaf, J.F. Liver elasticity and viscosity quantification using shearwave dispersion ultrasound vibrometry (SDUV). In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 2252–2255. [Google Scholar]
- Popa, A.; Bende, F.; Șirli, R.; Popescu, A.; Bâldea, V.; Lupușoru, R.; Cotrău, R.; Fofiu, R.; Foncea, C.; Sporea, I. Quantification of Liver Fibrosis, Steatosis, and Viscosity Using Multiparametric Ultrasound in Patients with Non-Alcoholic Liver Disease: A “Real-Life” Cohort Study. Diagnostics 2021, 11, 783. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Lee, J.Y.; Bae, J.S.; Yi, N.J.; Lee, K.W.; Suh, K.S.; Kim, H.; Lee, K.B.; Han, J.K. Shear-Wave Dispersion Slope from US Shear-Wave Elastography: Detection of Allograft Damage after Liver Transplantation. Radiology 2019, 293, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, K.; Moriyasu, F.; Oshiro, H.; Takeuchi, H.; Yoshimasu, Y.; Kasai, Y.; Furuichi, Y.; Itoi, T. Viscoelasticity Measurement in Rat Livers Using Shear-Wave US Elastography. Ultrasound Med. Biol. 2018, 44, 2018–2024. [Google Scholar] [CrossRef]
- Sporea, I.; Lupușoru, R.; Șirli, R. Ultrasound Based Elastography Techniques for the Evaluation of Nonalcoholic Liver Disease. Available online: https://www.intechopen.com/online-first/80274 (accessed on 30 April 2022).
- Cailloce, R.; Tavernier, E.; Brunereau, L.; Fievet, A.; Falip, C.; Dujardin, F.; Willot, S.; Patat, F.; Morel, B. Liver shear wave elastography and attenuation imaging coefficient measures: Prospective evaluation in healthy children. Abdom. Radiol. 2021, 46, 4629–4636. [Google Scholar] [CrossRef] [PubMed]
- Ferraioli, G.; Kumar, V.; Ozturk, A.; Nam, K.; de Korte, C.L.; Barr, R.G. US Attenuation for Liver Fat Quantification: An AIUM-RSNA QIBA Pulse-Echo Quantitative Ultrasound Initiative. Radiology 2022, 302, 495–506. [Google Scholar] [CrossRef]
- Tada, T.; Iijima, H.; Kobayashi, N.; Yoshida, M.; Nishimura, T.; Kumada, T.; Kondo, R.; Yano, H.; Kage, M.; Nakano, C.; et al. Usefulness of Attenuation Imaging with an Ultrasound Scanner for the Evaluation of Hepatic Steatosis. Ultrasound Med. Biol. 2019, 45, 2679–2687. [Google Scholar] [CrossRef] [PubMed]
- Hebelka, H.; de Lange, C.; Boström, H.; Ekvall, N.; Lagerstrand, K. Shear Wave Elastography in the Differentiation of Nonfibrotic Versus Fibrotic Liver Disease in Children: A Prospective Study with Histological Correlation. JPGN Rep. 2022, 3, e156. [Google Scholar] [CrossRef]
- Sugimoto, K.; Moriyasu, F.; Oshiro, H.; Takeuchi, H.; Yoshimasu, Y.; Kasai, Y.; Itoi, T. Clinical utilization of shear wave dispersion imaging in diffuse liver disease. Ultrasonography 2020, 39, 3–10. [Google Scholar] [CrossRef] [Green Version]
- Batts, K.P.; Ludwig, J. Chronic hepatitis. An update on terminology and reporting. Am. J. Surg. Pathol. 1995, 19, 1409–1417. [Google Scholar] [CrossRef]
- Yoo, J.; Lee, J.M.; Joo, I.; Lee, D.H.; Yoon, J.H.; Kang, H.J.; Ahn, S.J. Reproducibility of ultrasound attenuation imaging for the noninvasive evaluation of hepatic steatosis. Ultrasonography 2020, 39, 121–129. [Google Scholar] [CrossRef] [Green Version]
- Deffieux, T.; Gennisson, J.-L.; Bousquet, L.; Corouge, M.; Cosconea, S.; Amroun, D.; Tripon, S.; Terris, B.; Mallet, V.; Sogni, P. Investigating liver stiffness and viscosity for fibrosis, steatosis and activity staging using shear wave elastography. J. Hepatol. 2015, 62, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Cho, E.J.; Bae, J.S.; Lee, J.Y.; Yu, S.J.; Kim, H.; Lee, K.B.; Han, J.K.; Choi, B.I. Accuracy of Two-Dimensional Shear Wave Elastography and Attenuation Imaging for Evaluation of Patients with Nonalcoholic Steatohepatitis. Clin. Gastroenterol Hepatol. 2021, 19, 797–805.e7. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, K.; Moriyasu, F.; Oshiro, H.; Takeuchi, H.; Abe, M.; Yoshimasu, Y.; Kasai, Y.; Sakamaki, K.; Hara, T.; Itoi, T. The Role of Multiparametric US of the Liver for the Evaluation of Nonalcoholic Steatohepatitis. Radiology 2020, 296, 532–540. [Google Scholar] [CrossRef]
- Schulz, M.; Kleinjans, M.; Strnad, P.; Demir, M.; Holtmann, T.M.; Tacke, F.; Wree, A. Shear Wave Elastography and Shear Wave Dispersion Imaging in the Assessment of Liver Disease in Alpha1-Antitrypsin Deficiency. Diagnostics 2021, 11, 629. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Sanchez, W.; Callstrom, M.R.; Gorman, B.; Lewis, J.T.; Sanderson, S.O.; Greenleaf, J.F.; Xie, H.; Shi, Y.; Pashley, M. Assessment of liver viscoelasticity by using shear waves induced by ultrasound radiation force. Radiology 2013, 266, 964–970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bae, J.S.; Lee, D.H.; Lee, J.Y.; Kim, H.; Yu, S.J.; Lee, J.-H.; Cho, E.J.; Lee, Y.B.; Han, J.K.; Choi, B.I. Assessment of hepatic steatosis by using attenuation imaging: A quantitative, easy-to-perform ultrasound technique. Eur. Radiol. 2019, 29, 6499–6507. [Google Scholar] [CrossRef]
- Etchell, E.; Jugé, L.; Hatt, A.; Sinkus, R.; Bilston, L.E. Liver stiffness values are lower in pediatric subjects than in adults and increase with age: A multifrequency MR elastography study. Radiology 2017, 283, 222–230. [Google Scholar] [CrossRef]
- Barr, R.G.; Wilson, S.R.; Rubens, D.; Garcia-Tsao, G.; Ferraioli, G. Update to the Society of Radiologists in Ultrasound Liver Elastography Consensus Statement. Radiology 2020, 296, 263–274. [Google Scholar] [CrossRef]
- Mays, P.K.; McAnulty, R.; Laurent, G.J. Age-related changes in total protein and collagen metabolism in rat liver. Hepatology 1991, 14, 1224–1229. [Google Scholar] [CrossRef]
- Burgio, M.D.; Ronot, M.; Reizine, E.; Rautou, P.-E.; Castera, L.; Paradis, V.; Garteiser, P.; Van Beers, B.; Vilgrain, V. Quantification of hepatic steatosis with ultrasound: Promising role of attenuation imaging coefficient in a biopsy-proven cohort. Eur. Radiol. 2020, 30, 2293–2301. [Google Scholar] [CrossRef]
- Ferraioli, G.; Barr, R.G.; Dillman, J.R. Elastography for Pediatric Chronic Liver Disease: A Review and Expert Opinion. J. Ultrasound Med. 2021, 40, 909–928. [Google Scholar] [CrossRef] [PubMed]


| Number of Patients | |
|---|---|
| Liver transplants, yearly check-ups and acute indications | 8 |
| Unspecified—increased serological liver markers | 8 |
| Autoimmune hepatitis | 7 |
| Alfa-1-antitrypsin deficiency | 4 |
| Cholestatic disease | 2 |
| Primary and autoimmune sclerosing cholangitis | 1 |
| Non-alcoholic steatohepatitis (NASH) | 1 |
| Steatosis | 1 |
| Under Anesthesia | Awake | p-Value | |
|---|---|---|---|
| SWE (kPa) | 5.4 (2.9; 39.3) n = 41 | 5.4 (3; 20.1) n = 25 | 0.17 |
| SWD (m/s kHz) | 13 (8.4; 24.2) n = 41 | 13.6 (9.4; 16.9) n = 25 | 0.15 |
| ATI (dB/cm/MHz) | 0.56 (0.45; 0.94) n = 27 | 0.54 (0.38; 0.85) n = 19 | 0.14 |
| Fibrosis Grade | n (%) | SWE (kPa) Median (Min; Max) |
| 0 | 10 (31.3) | 4.9 (2.9; 8.1) |
| 1 | 12 (37.5) | 5.9 (5.3; 9.4) |
| 2 | 7 (21.9) | 13.5 (4.7; 39.3) |
| 3 | 3 (9.4) | 23.6 (13.9; 33.3) |
| Inflammation grade | SWD (m/s/kHz) | |
| 0 | 14 (43.8) | 13.1 (8.4; 17.2) |
| 1 | 13 (40.6) | 13.6 (11.3; 17.2) |
| 2 | 4 (12.5) | 16.1 (10.7; 24.2) |
| 3 | 1 (3.1) | 15.8 (15.3; 16.3) |
| Steatosis score | ATI (dB/cm/MHz) | |
| 0 | 22 (95.6) | 0.56 (0.4; 0.94) |
| 1 | 1 (4.4) | 0.82 |
| Patient (n = 32) | Control (n = 15) | p-Value | |
|---|---|---|---|
| Male | 22 (68.8%) | 8 (53.3%) | 0.48 |
| Female | 10 (31.3%) | 7 (46.7%) | |
| Age (years) | 12.1 (0.1; 17.9) | 11.8 (0.1; 17.9) | 0.75 |
| Height (cm) | 148.5 (57; 191.3) | 149 (86; 177) | 0.78 |
| Weight (kg) | 37.5 (4.5; 96) | 44 (11; 71) | 0.91 |
| BMI (kg/m2) | 17.7 (13.5; 28.9) | 17.7 (13; 26.7) | 0.78 |
| INR (prothrombin time) | 1.05 (0.9; 1.6) | 1 (0.9; 1.2) | 0.12 |
| AST (µkat/L) | 15 (3; 15) | N/A | |
| ALT (µkat/L) | 0.8 (0.22; 16) | 0.14 (0.1; 0.4) | <0.005 |
| White cell count (×109/L) | 5.4 (2.2; 12.2) | 8.4 (5.1; 25.5) | <0.035 |
| Thrombocytes (×109/L) | 239 (44; 444) | 333 (149; 707) | <0.02 |
| Gamma-GT (µkat/L) | 0.53 (0.15; 10) | 0.83 (0.16; 1.5) | 0.9 |
| Bilirubin (µkat/L) | 8.6 (3.3; 357) | 6.2 (5; 7.2) | <0.17 |
| SWE (kPa) | 6.2 (2.9; 39.3) | 4.6 (3.3; 7.5) | <0.002 |
| SWD (m/s/kHz) | 14.4 (8.4; 24.2) | 11.7 (9.4; 13.7) | <0.005 |
| ATI (dB/cm/MHz) | 0.56 (0.4; 0.94) n = 23 | 0.54 (0.45; 0.85) n = 11 | 0.87 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cetinic, I.; de Lange, C.; Simrén, Y.; Ekvall, N.; Östling, M.; Stén, L.; Boström, H.; Lagerstrand, K.; Hebelka, H. Ultrasound Shear Wave Elastography, Shear Wave Dispersion and Attenuation Imaging of Pediatric Liver Disease with Histological Correlation. Children 2022, 9, 692. https://doi.org/10.3390/children9050692
Cetinic I, de Lange C, Simrén Y, Ekvall N, Östling M, Stén L, Boström H, Lagerstrand K, Hebelka H. Ultrasound Shear Wave Elastography, Shear Wave Dispersion and Attenuation Imaging of Pediatric Liver Disease with Histological Correlation. Children. 2022; 9(5):692. https://doi.org/10.3390/children9050692
Chicago/Turabian StyleCetinic, Ivan, Charlotte de Lange, Yvonne Simrén, Nils Ekvall, Maja Östling, Liselotte Stén, Håkan Boström, Kerstin Lagerstrand, and Hanna Hebelka. 2022. "Ultrasound Shear Wave Elastography, Shear Wave Dispersion and Attenuation Imaging of Pediatric Liver Disease with Histological Correlation" Children 9, no. 5: 692. https://doi.org/10.3390/children9050692