Minimal Important Difference of the Psychosocial Impact of Dental Aesthetics Questionnaire Following Orthodontic Treatment: A Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analyses
2.2.1. Sensitivity
2.2.2. Responsiveness
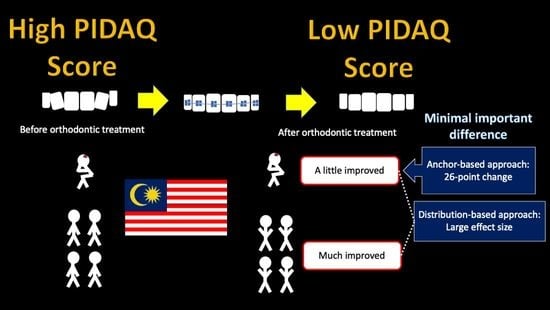
2.2.3. Determining the Minimal Important Difference (MID)
3. Results
3.1. Sensitivity
3.2. Responsiveness
3.3. Minimal Important Difference (MID)
4. Discussion
4.1. Limitations
4.2. Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Orthodontic Patients [Current Study] | School Children [26] | Young Adults [24] | |||
|---|---|---|---|---|---|
| Scale | T0 (N = 37) | T1 (N = 37) | T2 (N = 37) | All (N = 901) | All (N = 524) |
| Subscale | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| PIDAQ b | 52.2 (17.8) | 40.0 (15.9) | 25.6 (15.9) | 32.6 (16.2) | 36.3 (17.1) |
| Dental self-confidence (DSC) a | 5.3 (4.3) | 9.5 (5. 5) | 14.8 (6.3) | ||
| Reversed score DSC b | 18.9 (4.3) | 14.5 (5. 5) | 9.2 (6.3) | 11.3 (5.4) | 11.1 (5.2) |
| Social impact (SI) b | 15.3 (8.8) | 11.2 (7.2) | 7.5 (6.1) | 9.0 (6.6) | 11.1 (6.9) |
| Psychological impact (PI) b | 14.2 (5.6) | 11.4 (5.3) | 7.2 (4.6) | 9.8 (5.4) | 11.2 (5.3) |
| Aesthetic concern (AC) b | 4.1 (2.2) | 2.89 (1.9) | 1.7 (1.7) | 2.4 (1.9) | 2.9 (1.8) |
References
- Bellot-Arcis, C.; Montiel-Company, J.M.; Almerich-Silla, J.M. Psychosocial impact of malocclusion in Spanish adolescents. Korean J. Orthod. 2013, 43, 193–200. [Google Scholar] [CrossRef] [Green Version]
- Ghafari, M.; Bahadivand-Chegini, S.; Nadi, T.; Doosti-Irani, A. The global prevalence of dental healthcare needs and unmet dental needs among adolescents: A systematic review and meta-analysis. Epidemiol. Health 2019, 41, e2019046. [Google Scholar] [CrossRef] [PubMed]
- Copay, A.G.; Subach, B.R.; Glassman, S.D.; Polly, D.W., Jr.; Schuler, T.C. Understanding the minimum clinically important difference: A review of concepts and methods. Spine J. 2007, 7, 541–546. [Google Scholar] [CrossRef]
- Klages, U.; Claus, N.; Wehrbein, H.; Zentner, A. Development of a questionnaire for assessment of the psychosocial impact of dental aesthetics in young adults. Eur. J. Orthod. 2006, 28, 103–111. [Google Scholar] [CrossRef]
- Klages, U.; Erbe, C.; Sandru, S.D.; Brullman, D.; Wehrbein, H. Psychosocial impact of dental aesthetics in adolescence: Validity and reliability of a questionnaire across age-groups. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2015, 24, 379–390. [Google Scholar] [CrossRef]
- Montiel-Company, J.M.; Bellot-Arcis, C.; Almerich-Silla, J.M. Validation of the psychosocial impact of dental aesthetics questionnaire (Pidaq) in Spanish adolescents. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e168–e173. [Google Scholar] [CrossRef] [PubMed]
- Göranson, E.; Norevall, L.-I.; Bågesund, M.; Dimberg, L. Translation and validation of the Swedish version of the Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) for adolescents. Acta Odontol. Scand. 2020, 79, 241–247. [Google Scholar] [CrossRef]
- Alsanabani, A.A.M.; Yusof, Z.Y.M.; Wan Hassan, W.N.; Aldhorae, K.; Alyamani, H.A. Validity and Reliability of the Arabic Version of the Psychosocial Impact of Dental Aesthetics Questionnaire for Yemeni Adolescents. Children 2021, 8, 448. [Google Scholar] [CrossRef]
- Bucci, R.; Rongo, R.; Zito, E.; Valletta, R.; Michelotti, A.; D’Anto, V. Translation and validation of the italian version of the Psychosocial Impact of Dental Aesthetics Questionnaire (pidaq) among adolescents. Eur. J. Paediatr. Dent. 2017, 18, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.M.; Gonçalves, A.R.; Marega, T. Validity of the Psychosocial Impact of Dental Aesthetics Questionnaire for use on Brazilian adolescents. Dent. Press J. Orthod. 2016, 21, 67–72. [Google Scholar] [CrossRef]
- Kang, J.-M.; Kang, K.-H. Effect of malocclusion or orthodontic treatment on oral health-related quality of life in adults. Korean J. Orthod. 2014, 44, 304–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garg, K.; Tripathi, T.; Rai, P.; Sharma, N.; Kanase, A. Prospective Evaluation of Psychosocial Impact after One Year of Orthodontic Treatment Using PIDAQ Adapted for Indian Population. J. Clin. Diagn. Res. 2017, 11, ZC44–ZC48. [Google Scholar] [CrossRef] [PubMed]
- Masood, M.; Masood, Y.; Saub, R.; Newton, J.T. Need of minimal important difference for oral health-related quality of life measures. J. Public Health Dent. 2014, 74, 13–20. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Adolescence: A Period Needing Special Attention. Available online: http://apps.who.int/adolescent/second-decade/section2/page1/recognizing-adolescence.html (accessed on 13 February 2022).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988; 567p. [Google Scholar]
- Wan Hassan, W.N.; Yusof, Z.Y.M.; Shahidan, S.S.; Mohd Ali, S.F.; Makhbul, M.Z.M. Validation and reliability of the translated Malay version of the psychosocial impact of dental aesthetics questionnaire for adolescents. Health Qual. Life Outcomes 2017, 15, 23. [Google Scholar] [CrossRef] [Green Version]
- Wan Hassan, W.N.; Yusof, Z.Y.M.; Makhbul, M.Z.M.; Shahidan, S.S.; Mohd Ali, S.F.; Burhanudin, R.; Gere, M.J. Validation and reliability of the Malaysian English version of the psychosocial impact of dental aesthetics questionnaire for adolescents. Health Qual. Life Outcomes 2017, 15, 54. [Google Scholar] [CrossRef] [Green Version]
- Brook, P.H.; Shaw, W.C. The development of an index of orthodontic treatment priority. Eur. J. Orthod. 1989, 11, 309–320. [Google Scholar] [CrossRef] [Green Version]
- Roberts, C.T.; Richmond, S. The design and analysis of reliability studies for the use of epidemiological and audit indices in orthodontics. Br. J. Orthod. 1997, 24, 139–147. [Google Scholar] [CrossRef]
- Fayers, P.M.; Machin, D. Quality of Life: The Assessment, Analysis, and Reporting of Patient-Reported Outcomes, 3rd ed.; John Wiley & Sons Ltd.: Chichester, UK, 2016; p. 648. [Google Scholar]
- Wan Hassan, W.N.; Makhbul, M.Z.M.; Yusof, Z.Y.M. Use of the sociodental approach in estimating orthodontic treatment needs in adolescent patients. J. Orofac. Orthop. 2021, 1–11. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [Green Version]
- Department of Statistics Malaysia. Current Population Estimates, Malaysia, 2021. Available online: https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=155&bul_id=ZjJOSnpJR21sQWVUcUp6ODRudm5JZz09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09 (accessed on 1 April 2022).
- Tajudin, Z.M.; Wan Hassan, W.N.; Yusof, Z.Y.M.; Makhbul, M.Z.M. Impacts of Self Perceived Malocclusion on the Oral Health Related Quality of Life of Young Adults. Healthcare 2021, 9, 248. [Google Scholar] [CrossRef]
- Thabane, L.; Mbuagbaw, L.; Zhang, S.; Samaan, Z.; Marcucci, M.; Ye, C.; Thabane, M.; Giangregorio, L.; Dennis, B.; Kosa, D.; et al. A tutorial on sensitivity analyses in clinical trials: The what, why, when and how. BMC Med. Res. Methodol. 2013, 13, 92. [Google Scholar] [CrossRef] [Green Version]
- Wan Hassan, W.N.; Yusof, Z.Y.M.; Yuen, S.W.; Mohd Tajudin, Z.; Lokman, N.; Makhbul, M.Z.M. Prevalence, extent and severity of the psychosocial impact of dental aesthetics among Malaysian adolescents. Sains Malays. 2019, 48, 1729–1736. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using Effect Size-or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bills, D.A.; Handelman, C.S.; BeGole, E.A. Bimaxillary Dentoalveolar Protrusion: Traits and Orthodontic Correction. Angle Orthod. 2005, 75, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Mouelhi, Y.; Jouve, E.; Castelli, C.; Gentile, S. How is the minimal clinically important difference established in health-related quality of life instruments? Review of anchors and methods. Health Qual. Life Outcomes 2020, 18, 136. [Google Scholar] [CrossRef]
- Allen Dyken, R.; Sadowsky, P.L.; Hurst, D. Orthodontic Outcomes Assessment Using the Peer Assessment Rating Index. Angle Orthod. 2001, 71, 164–169. [Google Scholar] [CrossRef]
- Fox, N.A.; Daniels, C.; Gilgrass, T. A comparison of the Index of Complexity Outcome and Need (ICON) with the Peer Assessment Rating (PAR) and the Index of Orthodontic Treatment Need (IOTN). Br. Dent. J. 2002, 193, 225–230. [Google Scholar] [CrossRef] [Green Version]
| PIDAQ Scores | Global Health Transition Scale | |||||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T1 | T2 | ||||
| Characteristic | N (%) | Mean (SD) | Mean (SD) | Mean (SD) | A Little Improved, n (%) | Much Improved, n (%) | A Little Improved, n (%) | Much Improved, n (%) |
| Gender | ||||||||
| Male | 6 (16.2) | 57.0 (13.1) | 51.0 (23.8) | 22.3 (10.9) | 1 (6.3) | 5 (23.8) | 3 (42.9) | 3 (10.0) |
| Female | 31 (83.8) | 51.3 (18.6) | 37.9 (13.4) | 26.3 (16.8) | 15 (93.8) | 16 (76.2) | 4 (57.1) | 27 (90.0) |
| Age | ||||||||
| 11–14 | 19 (51.4) | 49.3 (17.4) | 37.2 (18.4) | 24.2 (16.6) | 9 (56.3) | 10 (47.6) | 5 (71.4) | 14 (46.7) |
| 15–18 | 18 (48.6) | 55.4 (18.1) | 42.9 (12.6) | 27.1 (15.5) | 7 (43.8) | 11 (52.4) | 2 (28.6) | 16 (53.3) |
| Ethnicity | ||||||||
| Malay | 21 (56.8) | 57.8 (19.9) | 41.2 (16.3) | 29.2 (15.2) | 6 (37.5) | 15 (71.4) | 4 (57.1) | 17 (56.7) |
| Chinese | 12 (32.4) | 47.0 (9.9) | 44.8 (11.6) | 23.4 (17.4) | 9 (56.3) | 3 (14.3) | 3 (42.9) | 9 (30.0) |
| India | 3 (8.1) | 35.3 (16.8) | 20.3 (12.1) | 16.3 (7.6) | 1 (6.3) | 2 (9.5) | 3 (10.0) | |
| Other | 1 (2.7) | 50.0 (0) | 16.0 (0) | 4.0 (0) | 1 (4.8) | 1 (3.3) | ||
| Normative need (NN) | ||||||||
| No NN | 8 (21.6) | 45.0 (20.4) | 35.8 (14.3) | 24.9 (18.1) | 3 (18.8) | 5 (23.8) | 8 (26.7) | |
| NN | 29 (78.4) | 54.2 (16.8) | 41.2 (16.4) | 25.8 (15.6) | 13 (81.3) | 16 (76.2) | 7 (100.0) | 22 (73.3) |
| Standardized Scores | Differences in Standardized Scores | |||||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T1−T0 | T2−T0 | ||||
| Scale Subscale | Mean (SD) | Mean (SD) | Mean (SD) | p-Value a; Effect Size (η2) | Mean Diff (95% CI); p-Value b | Effect Size (Descriptor) | Mean Diff (95% CI); p-Value b | Effect Size (Descriptor) |
| PIDAQ | 59.4 (20.2) | 45.5 (18.1) | 29.1 (18.1) | 0.000 a; 0.5 | −13.9 (−22.0, −5.8); 0.000 b | 0.7 (medium) | −30.3 (−40.0, −20.5); 0.000 b | 1.5 (large) |
| DSC | 22.2 (17.9) | 39.4 (22.8) | 61.5 (26.3) | 0.000 a; 0.5 | 17.2 (7.5, 27.0); 0.000 b | 1.0 (large) | 22.1 (10.1, 34.0); 0.000 b | 2.2 (large) |
| SI | 47.8 (27.4) | 35.0 (22.5) | 23.5 (19.0) | 0.000 a; 0.4 | −12.8 (−22.0, −3.6); 0.004 b | 0.5 (medium) | −24.3 (−35.4, −13.2); 0.000 b | 0.9 (large) |
| PI | 51.1 (23.2) | 47.4 (22.2) | 30.0 (19.3) | 0.000 a; 0.5 | −11.7 (−20.1, −3.4); 0.004 b | 0.2 (small) | −29.2 (−39.7, −18.6); 0.000 b | 0.9 (large) |
| AC | 51.0 (27.2) | 36.1 (23.3) | 20.9 (21.9) | 0.000 a; 0.4 | −14.9 (−25.8, −3.9); 0.005 b | 0.2 (small) | −30.1 (−42.4, −17.7); 0.000 b | 1.1 (large) |
| Within Group Differences | Between Group Differences | ||||||
|---|---|---|---|---|---|---|---|
| T1−T0 | T2−T0 | T2−T1 | At T0 | At T1 | At T2 | ||
| Group (n) | p-Value a; Effect Size (η2) | Mean Diff (95% CI); p-Value b; Effect Size (Descriptor) | Mean Diff (95% CI); p-Value b; Effect Size (Descriptor) | Mean Diff (95% CI); p-Value b; Effect Size (Descriptor) | Mean Diff (95% CI); p-Value c; Effect Size (Descriptor) | Mean Diff (95% CI); p-Value c; Effect Size (Descriptor) | Mean Diff (95% CI); p-Value c; Effect Size (Descriptor) |
| No NN (8) | 0.029 a; 0.459 | −9.3 (−24.6, 6.1); 0.307; 0.7 (medium) | −20.1 (−43.9, 3.6); 0.099; 1.0 (large) | −10.9 (−25.2, 3.4); 0.146; 0.9 (large) | −9.2 (−23.5, 5.0); 0.197; 0.5 (medium) | −5.4 (−18.4, 7.5); 0.401; 0.4 (small) | −1.0 (−14.0, 12.1); 0.883 0.1 (small) |
| NN (29) | 0.000 a; 0.526 | −13.1 (−21.7, −4.4); 0.002 b; 0.7 (medium) | −28.4 (−38.2, −18.6); 0.000 b; 1.4 (large) | −15.3 (−24.5, −6.2); 0.001 b; 0.8 (large) | |||
| Perceived Dental Appearance | PIDAQ Score | |||||
|---|---|---|---|---|---|---|
| T0 | T1 | T2 | ||||
| n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | |
| Very poor | 5 (13.5) | 57.4 (20.5) | ||||
| Poor | 11 (29.7) | 59.3 (19.8) | ||||
| Average | 19 (51.4) | 45.4 (14.2) | 6 (16.2) | 44.8 (8.2) | ||
| Good | 1 (2.7) | 50.0 | 24 (64.9) | 38.1 (18.2) | 20 (54.1) | 29.6 (15.0) |
| Excellent | 1 (2.7) | 75.0 | 7 (18.9) | 42.3 (12.3) | 17 (45.9) | 21.0 (16.1) |
| Mean rank | 1.14 | 2.22 | 2.66 | |||
| p-value a | 0.000 a | |||||
| Scale Subscale | Responsiveness at T1 | Responsiveness to Change at T2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | T0 | T1 | Mean Change | Effect Size, d | n | T0 | T2 | Mean Change | Effect Size, d | |
| Mean (SD) | Mean (SD) | (SD) p-Value | (Descriptor) | Mean (SD) | Mean (SD) | (SD) p-Value | (Descriptor) | |||
| A little improved a | ||||||||||
| PIDAQ | 16 | 42.9 (15.6) | 37.7 (15.4) | −5.3 (13.4) 0.140 | 0.4 (Small) | 7 | 51.4 (20.5) | 25.1 (11.7) | −26.2 (25.4) 0.034 * | 1.0 (Large) |
| DSC | 7.2 (4.7) | 9.4 (4.7) | 2.3 (3.7) 0.027 * | 0.6 (Medium) | 7.0 (5.0) | 14.6 (5.7) | 7.6 (8.0) 0.046 * | 1.0 (Large) | ||
| SI | 11.8 (7.4) | 10.4 (6.6) | −1.4 (5.7) 0.327 | 0.3 (Small) | 15.9 (9.2) | 7.3 (5.3) | −8.6 (9.9) 0.061 | 0.9 (Large) | ||
| PI | 11.4 (4.7) | 10.3 (4.8) | −1.2 (4.7) 0.332 | 0.2 (Small) | 14.4 (6.9) | 6.9 (4.1) | −7.6 (8.2) 0.050 | 0.9 (Large) | ||
| AC | 2.9 (1.8) | 2.5 (1.8) | −0.4 (1.8) 0.414 | 0.2 (Small) | 4.1 (2.3) | 1.6 (1.3) | −2.6 (3.0) 0.063 | 0.8 (Large) | ||
| Much improved a | ||||||||||
| PIDAQ | 21 | 59.3 (16.2) | 41.8 (16.5) | −17.6 (18.3) 0.000 * | 1.0 (Large) | 30 | 52.4 (17.4) | 25.7 (16.9) | −26.7 (20.1) 0.000 * | 1.3 (Large) |
| DSC | 3.9 (3.5) | 9.5 (6.1) | 5.6 (6.5) 0.001 * | 0.9 (Large) | 4.9 (4.1) | 14.8 (6.5) | 9.9 (6.7) 0.000 * | 1.4 (Large) | ||
| SI | 18.0 (9.0) | 11.8 (7.7) | −6.1 (7.6) 0.001 * | 0.8 (Large) | 15.2 (8.8) | 7.6 (6.3) | −7.6 (8.5) 0.000 * | 0.9 (Large) | ||
| PI | 16.3 (5.3) | 12.2 (5.6) | −4.0 (4.7) 0.001 * | 0.9 (Large) | 14.1 (5.3) | 7.3 (4.8) | −6.9 (5.7) 0.000 * | 1.2 (Large) | ||
| AC | 5.0 (2.0) | 3.2 (1.9) | −1.8 (2.2) 0.001 * | 0.8 (Large) | 4.1 (2.2) | 1.7 (1.9) | −2.4 (2.3) 0.000 * | 1.0 (Large) | ||
| Scale | Bland and Altman | MID | |||
|---|---|---|---|---|---|
| 95% Limits of Agreement | Post-Treatment (T2) | ||||
| Subscale | Mean | Lower | Upper | Mean Change a (SD) | Standardized Effect Size b (Descriptor) |
| PIDAQ | −0.9 | −10.3 | 8.5 | −26.2 (25.4) | 1.5 (large) |
| DSC | 0.2 | −5.3 | 5.6 | 7.6 (8.0) | 2.2 (large) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wan Hassan, W.N.; Makhbul, M.Z.M.; Yusof, Z.Y.M.; Othman, S.A. Minimal Important Difference of the Psychosocial Impact of Dental Aesthetics Questionnaire Following Orthodontic Treatment: A Cohort Study. Children 2022, 9, 506. https://doi.org/10.3390/children9040506
Wan Hassan WN, Makhbul MZM, Yusof ZYM, Othman SA. Minimal Important Difference of the Psychosocial Impact of Dental Aesthetics Questionnaire Following Orthodontic Treatment: A Cohort Study. Children. 2022; 9(4):506. https://doi.org/10.3390/children9040506
Chicago/Turabian StyleWan Hassan, Wan Nurazreena, Mohd Zambri Mohamed Makhbul, Zamros Yuzadi Mohd Yusof, and Siti Adibah Othman. 2022. "Minimal Important Difference of the Psychosocial Impact of Dental Aesthetics Questionnaire Following Orthodontic Treatment: A Cohort Study" Children 9, no. 4: 506. https://doi.org/10.3390/children9040506