Lifestyle Risk Factors for Overweight/Obesity in Spanish Children
Abstract
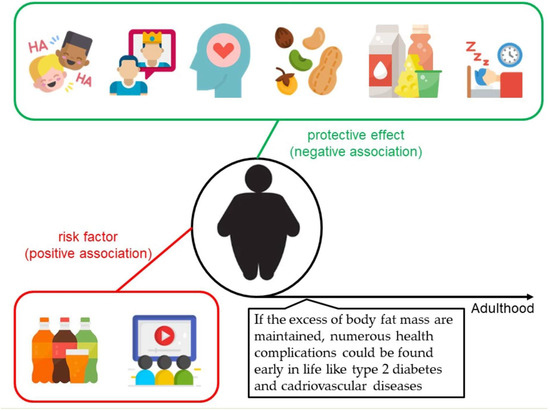
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Socioeconomic Variables
2.3. Anthropometric Measures
2.4. Beverage Consumption
2.5. Mediterranean Diet Adherence
2.6. Physical Activity
2.7. Screen Time
2.8. Sleep Duration
2.9. Emotional Well-Being and Self-Esteem
2.10. Statistical Analysis
3. Results
4. Discussion
4.1. Beverage Consumption and Obesity
4.2. Mediterranean Diet and Obesity
4.3. Total Screen Time (TST) and Obesity
4.4. Sleep Duration and Obesity
4.5. Emotional Well-Being and Self-Esteem
4.6. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- García-Solano, M.; Gutiérrez-González, E.; López-Sobaler, A.; Ruiz-Álvarez, M.; Bermejo López, L.; Aparicio, A.; García-López, M.A.; Yusta-Boyo, M.J.; de Dios, T.R.; Villalba, C.V.; et al. Weight status in the 6- to 9-year-old school population in Spain: Results of the ALADINO 2019 Study. Nutr. Hosp. 2021, 38, 943–953. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, P.; The, N.S.; Adair, L.S. Longitudinal Trends in Obesity in the United States From Adolescence to the Third Decade of Life. Obesity 2010, 18, 1801–1804. [Google Scholar] [CrossRef]
- Smith, J.D.; Fu, E.; Kobayashi, M.A. Prevention and Management of Childhood Obesity and Its Psychological and Health Comorbidities. Annu. Rev. Clin. Psychol. 2020, 16, 351–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franks, P.W.; Hanson, R.L.; Knowler, W.C.; Sievers, M.L.; Bennett, P.H.; Looker, H.C. Childhood Obesity, Other Cardiovascular Risk Factors, and Premature Death. N. Engl. J. Med. 2010, 362, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Horesh, A.; Tsur, A.M.; Bardugo, A.; Twig, G. Adolescent and Childhood Obesity and Excess Morbidity and Mortality in Young Adulthood—A Systematic Review. Curr. Obes. Rep. 2021, 10, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Dev, D.A.; McBride, B.A.; Fiese, B.H.; Jones, B.L.; Cho, H.; Behalf of The Strong Kids Research Team. Risk Factors for Overweight/Obesity in Preschool Children: An Ecological Approach. Child. Obes. 2013, 9, 399–408. [Google Scholar] [CrossRef] [Green Version]
- López-Sobaler, A.; Aparicio, A.; Salas-González, M.; Loria Kohen, V.; Bermejo López, L. Childhood obesity in Spain and associated factors. Nutr. Hosp. 2021, 38, 27–30. [Google Scholar] [CrossRef]
- Seral-Cortes, M.; Sabroso-Lasa, S.; De Miguel-Etayo, P.; Gonzalez-Gross, M.; Gesteiro, E.; Molina-Hidalgo, C.; De Henauw, S.; Erhardt, É.; Censi, L.; Manios, Y.; et al. Interaction Effect of the Mediterranean Diet and an Obesity Genetic Risk Score on Adiposity and Metabolic Syndrome in Adolescents: The HELENA Study. Nutrients 2020, 12, 3841. [Google Scholar] [CrossRef]
- LeDoux, T.A.; Hingle, M.D.; Baranowski, T. Relationship of fruit and vegetable intake with adiposity: A systematic review. Obes. Rev. 2010, 12, e143–e150. [Google Scholar] [CrossRef]
- Wu, A.J.; Aris, I.M.; Rifas-Shiman, S.L.; Oken, E.; Taveras, E.M.; Hivert, M.-F. Longitudinal associations of fruit juice intake in infancy with DXA-measured abdominal adiposity in mid-childhood and early adolescence. Am. J. Clin. Nutr. 2021, 114, 117–123. [Google Scholar] [CrossRef]
- Heras-Gonzalez, L.; Latorre, J.A.; Martinez-Bebia, M.; Gimenez-Blasi, N.; Olea-Serrano, F.; Mariscal-Arcas, M. Sugar consumption in schoolchildren from southern Spain and influence on the prevalence of obesity. PLoS ONE 2020, 15, e0242602. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Gordy, C.C.; Raynor, H.A.; Beddome, M.; Kilanowski, C.K.; Paluch, R. Increasing Fruit and Vegetable Intake and Decreasing Fat and Sugar Intake in Families at Risk for Childhood Obesity. Obes. Res. 2001, 9, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Liberali, R.; Kupek, E.; De Assis, M.A.A. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child. Obes. 2020, 16, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Goldsmith, R.; Shimony, T.; Berry, E.M.; Sinai, T. Trends in the adherence to the Mediterranean diet in Israeli adolescents: Results from two national health and nutrition surveys, 2003 and 2016. Eur. J. Nutr. 2021, 60, 3625–3638. [Google Scholar] [CrossRef]
- Sørensen, L.M.N.; Aamodt, G.; Brantsæter, A.L.; Meltzer, H.M.; Papadopoulou, E. Diet quality of Norwegian children at 3 and 7 years: Changes, predictors and longitudinal association with weight. Int. J. Obes. 2021, 46, 10–20. [Google Scholar] [CrossRef]
- Iglesia, I.; Intemann, T.; De Miguel-Etayo, P.; Pala, V.; Hebestreit, A.; Wolters, M.; Russo, P.; Veidebaum, T.; Papoutsou, S.; Nagy, P.; et al. Dairy Consumption at Snack Meal Occasions and the Overall Quality of Diet during Childhood. Prospective and Cross-Sectional Analyses from the IDEFICS/I.Family Cohort. Nutrients 2020, 12, 642. [Google Scholar] [CrossRef] [Green Version]
- George, E.S.; Gavrili, S.; Itsiopoulos, C.; Manios, Y.; Moschonis, G. Poor adherence to the Mediterranean diet is associated with increased likelihood of metabolic syndrome components in children: The Healthy Growth Study. Public Health Nutr. 2021, 24, 2823–2833. [Google Scholar] [CrossRef]
- Sprengeler, O.; Pohlabeln, H.; Bammann, K.; Buck, C.; Lauria, F.; Verbestel, V.; Eiben, G.; Konstabel, K.; Molnár, D.; Moreno, L.A.; et al. Trajectories of objectively measured physical activity and childhood overweight: Longitudinal analysis of the IDEFICS/I.Family cohort. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 1–12. [Google Scholar] [CrossRef]
- Farooq, A.; Basterfield, L.; Adamson, A.; Pearce, M.; Hughes, A.; Janssen, X.; Wilson, M.; Reilly, J. Moderate-To-Vigorous Intensity Physical Activity and Sedentary Behaviour across Childhood and Adolescence, and Their Combined Relationship with Obesity Risk: A Multi-Trajectory Analysis. Int. J. Environ. Res. Public Health 2021, 18, 7421. [Google Scholar] [CrossRef]
- Kanellopoulou, M.A.; Notara, V.; Magriplis, E.; Antonogeorgos, G.; Rojas-Gil, A.P.; Kornilaki, E.N.; Lagiou, A.; Yannakoulia, M.; Panagiotakos, D.B. Sleeping patterns and childhood obesity: An epidemiological study in 1,728 children in Greece. J. Clin. Sleep Med. 2021, 17, 1093–1101. [Google Scholar] [CrossRef]
- Decraene, M.; Verbestel, V.; Cardon, G.; Iotova, V.; Koletzko, B.; Moreno, L.; Miguel-Berges, M.; Gurzkowska, B.; Androutsos, O.; Manios, Y.; et al. Compliance with the 24-Hour Movement Behavior Guidelines and Associations with Adiposity in European Preschoolers: Results from the ToyBox-Study. Int. J. Environ. Res. Public Health 2021, 18, 7499. [Google Scholar] [CrossRef]
- Zheng, M.; Hesketh, K.D.; Wu, J.H.Y.; Heitmann, B.L.; Downing, K.; Campbell, K.J. Nighttime sleep duration trajectories were associated with body mass index trajectories in early childhood. Pediatr. Obes. 2020, 16, e12766. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, S.L.; Larkin, E.K.; Rosen, C.L.; Palermo, T.M.; Redline, S. Decreased Quality of Life Associated With Obesity in School-aged Children. Arch. Pediatr. Adolesc. Med. 2003, 157, 1206–1211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swallen, K.C.; Reither, E.N.; Haas, S.A.; Meier, A.M. Overweight, Obesity, and Health-Related Quality of Life Among Adolescents: The National Longitudinal Study of Adolescent Health. Pediatrics 2005, 115, 340–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wardle, J.; Cooke, L. The impact of obesity on psychological well-being. Best Pract. Res. Clin. Endocrinol. Metab. 2005, 19, 421–440. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.M.; Baune, B.T. Overweight, Medical Comorbidity and Health-related Quality of Life in a Community Sample of Women and Men. Obesity 2009, 17, 1627–1634. [Google Scholar] [CrossRef]
- Fontaine, K.R.; Barofsky, I. Obesity and health-related quality of life. Obes. Rev. 2001, 2, 173–182. [Google Scholar] [CrossRef]
- Falkner, N.H.; Neumark-Sztainer, D.; Story, M.; Jeffery, R.W.; Beuhring, T.; Resnick, M.D. Social, Educational, and Psychological Correlates of Weight Status in Adolescents. Obes. Res. 2001, 9, 32–42. [Google Scholar] [CrossRef]
- Sjöberg, R.L.; Nilsson, K.W.; Leppert, J. Obesity, Shame, and Depression in School-Aged Children: A Population-Based Study. Pediatrics 2005, 116, e389–e392. [Google Scholar] [CrossRef] [Green Version]
- Jansen, W.; van de Looij-Jansen, P.M.; de Wilde, E.J.; Brug, J. Feeling Fat Rather than Being Fat May Be Associated with Psychological Well-Being in Young Dutch Adolescents. J. Adolesc. Health. 2008, 42, 128–136. [Google Scholar] [CrossRef]
- Daniels, J. Weight and weight concerns: Are they associated with reported depressive symptoms in adolescents? J. Pediatr. Health. Care 2005, 19, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.; van den Berg, P.; Boutelle, K.; Hannan, P.; Neumark-Sztainer, D. Obesity, Body Dissatisfaction, and Emotional Well-Being in Early and Late Adolescence: Findings From the Project EAT Study. J. Adolesc. Health 2011, 48, 373–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nixon, C.A.; Moore, H.J.; Douthwaite, W.; Gibson, E.L.; Vogele, C.; Kreichauf, S.; Wildgruber, A.; Manios, Y.; Summerbell, C.D. ToyBox-study group Identifying effective behavioural models and behaviour change strategies underpinning preschool- and school-based obesity prevention interventions aimed at 4-6-year-olds: A systematic review. Obes. Rev. 2012, 13, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Stewart, A.; Marfell-Jones, M.; Olds, T.; De Ridder, H. International standards for anthropometric assessment. In International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropemetry: Lower Hutt, New Zealand, 2011. [Google Scholar]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [Green Version]
- Mouratidou, T.; Graffe, M.I.M.; Huybrechts, I.; De Decker, E.; De Craemer, M.; Androutsos, O.; Manios, Y.; Galcheva, S.; Lateva, M.; Gurzkowska, B.; et al. Reproducibility and relative validity of a semiquantitative food frequency questionnaire in European preschoolers: The ToyBox study. Nutrition 2019, 65, 60–67. [Google Scholar] [CrossRef] [Green Version]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Verbestel, V.; De Henauw, S.; Bammann, K.; Barba, G.; Hadjigeorgiou, C.; Eiben, G.; Konstabel, K.; Kovács, E.; Pitsiladis, Y.; Reisch, L.; et al. Are context-specific measures of parental-reported physical activity and sedentary behaviour associated with accelerometer data in 2–9-year-old European children? Public Health Nutr. 2014, 18, 860–868. [Google Scholar] [CrossRef]
- WHO. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children under 5 Years of Age; WHO: Geneva, Switzerland, 2019.
- Tremblay, M.S.; LeBlanc, A.; Janssen, I.; Kho, M.; Hicks, A.; Murumets, K.; Colley, R.C.; Duggan, M. Canadian Sedentary Behaviour Guidelines for Children and Youth. Appl. Physiol. Nutr. Metab. 2011, 36, 59–64. [Google Scholar] [CrossRef] [Green Version]
- Ravens-Sieberer, U.; Bullinger, M. Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Qual. Life Res. 1998, 7, 399–407. [Google Scholar] [CrossRef]
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef]
- Hu, F.B. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes. Rev. 2013, 14, 606–619. [Google Scholar] [CrossRef] [PubMed]
- Luger, M.; Lafontan, M.; Bes-Rastrollo, M.; Winzer, E.; Yumuk, V.; Farpour-Lambert, N. Sugar-Sweetened Beverages and Weight Gain in Children and Adults: A Systematic Review from 2013 to 2015 and a Comparison with Previous Studies. Obes. Facts 2017, 10, 674–693. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Schulze, M.B.; Hu, F.B. Intake of sugar-sweetened beverages and weight gain: A systematic review. Am. J. Clin. Nutr. 2006, 84, 274–288. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Peterson, K.E.; Gortmaker, S.L. Relation between consumption of sugar-sweetened drinks and childhood obesity: A prospective, observational analysis. Lancet 2001, 357, 505–508. [Google Scholar] [CrossRef]
- Bellisle, F.; Rolland-Cachera, M.F. How sugar-containing drinks might increase adiposity in children. Lancet 2001, 357, 490–491. [Google Scholar] [CrossRef] [PubMed]
- Duffey, K.J.; Poti, J. Modeling the Effect of Replacing Sugar-Sweetened Beverage Consumption with Water on Energy Intake, HBI Score, and Obesity Prevalence. Nutrients 2016, 8, 395. [Google Scholar] [CrossRef] [Green Version]
- Ros, E.; Singh, A.; O’Keefe, J.H. Nuts: Natural Pleiotropic Nutraceuticals. Nutrients 2021, 13, 3269. [Google Scholar] [CrossRef]
- St-Onge, M.-P. Dietary fats, teas, dairy, and nuts: Potential functional foods for weight control? Am. J. Clin. Nutr. 2005, 81, 7–15. [Google Scholar] [CrossRef] [Green Version]
- Sabaté, J. Nut consumption and body weight. Am. J. Clin. Nutr. 2003, 78, 647S–650S. [Google Scholar] [CrossRef] [Green Version]
- Brufau, G.; Boatella, J.; Rafecas, M. Nuts: Source of energy and macronutrients. Br. J. Nutr. 2006, 96, S24–S28. [Google Scholar] [CrossRef]
- Keys, A. Mediterranean diet and public health: Personal reflections. Am. J. Clin. Nutr. 1995, 61, 1321S–1323S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hachem, F.; Vanham, D.; Moreno, L.A. Territorial and Sustainable Healthy Diets. Food Nutr. Bull. 2020, 41, 87S–103S. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Marrugat, J.; Vila, J.; Covas, M.I.; Elosua, R. Adherence to the Traditional Mediterranean Diet Is Inversely Associated with Body Mass Index and Obesity in a Spanish Population. J. Nutr. 2004, 134, 3355–3361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goñi, I.L.; Arenaza, L.; Medrano, M.; García, N.; Cadenas-Sanchez, C.; Ortega, F.B. Associations between the adherence to the Mediterranean diet and cardiorespiratory fitness with total and central obesity in preschool children: The PREFIT project. Eur. J. Nutr. 2017, 57, 2975–2983. [Google Scholar] [CrossRef] [Green Version]
- Lazarou, C.; Panagiotakos, D.B.; Matalas, A.-L. Physical activity mediates the protective effect of the Mediterranean diet on children’s obesity status: The CYKIDS study. Nutrition 2010, 26, 61–67. [Google Scholar] [CrossRef]
- Farajian, P.; Risvas, G.; Karasouli, K.; Pounis, G.D.; Kastorini, C.M.; Panagiotakos, D.B.; Zampelas, A. Very high childhood obesity prevalence and low adherence rates to the Mediterranean diet in Greek children: The GRECO study. Atherosclerosis 2011, 217, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Fang, K.; Mu, M.; Liu, K.; He, Y. Screen time and childhood overweight/obesity: A systematic review and meta-analysis. Child: Care, Health Dev. 2019, 45, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Champagne, C.M.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; Johnson, W.D.; Kuriyan, R.; Kurpad, A.; et al. Relationship between lifestyle behaviors and obesity in children ages 9-11: Results from a 12-country study. Obesity 2015, 23, 1696–1702. [Google Scholar] [CrossRef]
- Pérez-Farinós, N.; Villar-Villalba, C.; Sobaler, A.M.L.; Saavedra, M.D.R.; Aparicio, A.; Sanz, S.S.; de Dios, T.R.; Castrodeza-Sanz, J.J.; Anta, R.M.O. The relationship between hours of sleep, screen time and frequency of food and drink consumption in Spain in the 2011 and 2013 ALADINO: A cross-sectional study. BMC Public Health 2017, 17, 33. [Google Scholar] [CrossRef] [Green Version]
- Miguel-Berges, M.L.; Santaliestra-Pasias, A.M.; Mouratidou, T.; De Miguel-Etayo, P.; Androutsos, O.; De Craemer, M.; Galcheva, S.; Koletzko, B.; Kulaga, Z.; Manios, Y.; et al. Combined Longitudinal Effect of Physical Activity and Screen Time on Food and Beverage Consumption in European Preschool Children: The ToyBox-Study. Nutrients 2019, 11, 1048. [Google Scholar] [CrossRef]
- Miguel-Berges, M.L.; Zachari, K.; Santaliestra-Pasias, A.M.; Mouratidou, T.; Androutsos, O.; Iotova, V.; Galcheva, S.; De Craemer, M.; Cardon, G.; Koletzko, B.; et al. Clustering of energy balance-related behaviours and parental education in European preschool children: The ToyBox study. Br. J. Nutr. 2017, 118, 1089–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miguel-Berges, M.L.; Santaliestra-Pasias, A.M.; Mouratidou, T.; Androutsos, O.; de Craemer, M.; Pinket, A.S.; Birnbaum, J.; Koletzko, B.; Iotova, V.; Usheva, N.; et al. Associations between food and beverage consumption and different types of sedentary behaviours in European preschoolers: The ToyBox-study. Eur. J. Nutr. 2016, 56, 1939–1951. [Google Scholar] [CrossRef] [PubMed]
- Santaliestra-Pasías, A.M.; Mouratidou, T.; Verbestel, V.; Huybrechts, I.; Gottrand, F.; Le Donne, C.; Cuenca-García, M.; Díaz, L.E.; Kafatos, A.; Manios, Y.; et al. Food Consumption and Screen-Based Sedentary Behaviors in European Adolescents. Arch. Pediatr. Adolesc. Med. 2012, 166, 1010–1020. [Google Scholar] [CrossRef] [Green Version]
- Butte, N.F.; Puyau, M.R.; Wilson, T.A.; Liu, Y.; Wong, W.W.; Adolph, A.L.; Zakeri, I.F. Role of physical activity and sleep duration in growth and body composition of preschool-aged children. Obesity 2016, 24, 1328–1335. [Google Scholar] [CrossRef] [Green Version]
- Hale, L.; Guan, S. Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Med. Rev. 2015, 21, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wells, J.C.K.; Hallal, P.C.; Reichert, F.F.; Menezes, A.M.B.; Araújo, C.L.P.; Victora, C.G. Sleep patterns and television viewing in relation to obesity and blood pressure: Evidence from an adolescent Brazilian birth cohort. Int. J. Obes. 2008, 32, 1042–1049. [Google Scholar] [CrossRef] [Green Version]
- Kuriyan, R.; Bhat, S.; Thomas, T.; Vaz, M.; Kurpad, A.V. Television viewing and sleep are associated with overweight among urban and semi-urban South Indian children. Nutr. J. 2007, 6, 25. [Google Scholar] [CrossRef] [Green Version]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.-B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-Analysis of Short Sleep Duration and Obesity in Children and Adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez-Gomez, D.; Moreno, L.A.; Romeo, J.; Rey-López, J.P.; Castillo, R.; Cabero, M.J.; Vicente-Rodriguez, G.; Gutiérrez, A.; Veiga, O.L. Combined influence of lifestyle risk factors on body fat in Spanish adolescents--the Avena study. Obes. Facts 2011, 4, 105–111. [Google Scholar] [CrossRef] [Green Version]
- Davison, K.K.; Birch, L.L. Weight Status, Parent Reaction, and Self-Concept in Five-Year-Old Girls. Pediatrics 2001, 107, 46–53. [Google Scholar] [CrossRef]
- Paxton, S.; Damiano, S. The Development of Body Image and Weight Bias in Childhood. Adv. Child Dev. Behav. 2016, 52, 269–298. [Google Scholar] [CrossRef] [PubMed]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc. Health Med. Ther. 2016, 7, 125–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Floody, P.A.D.; Caamaño-Navarrete, F.; Martínez-Salazar, C.; Jerez-Mayorga, D.; Carter-Thuiller, B.; Pinillos, F.G.; Román, P.L. Childhood obesity and its association with the feeling of unhappiness and low levels of self-esteem in children of public schools. Nutr. Hosp. 2018, 35, 533–537. [Google Scholar] [CrossRef]

| Boys (n = 529; 49.1%) | Girls (n = 546; 50.7%) | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p | |
| Age (years) | 7.96 (2.76) | 8.08 (2.69) | 0.305 |
| BMI (z-score) * | 0.71 (1.19) | 0.50 (1.15) | 0.006 |
| Waist circumference (cm) | 60.84 (9.09) | 59.53 (8.86) | 0.018 |
| n (%) | n (%) | ||
| BMI (categories) ** | |||
| Thinness | 17 (3.0) | 18 (3.0) | 0.825 |
| Normal weight | 344 (68.9) | 347 (69.1) | |
| Overweight | 95 (19.0) | 97 (19.3) | |
| Obesity | 43 (8.6) | 40 (8.0) | |
| Maternal education | |||
| Compulsory studies | 101 (17.01) | 124 (20.7) | 0.163 |
| Professional formation | 306 (51.17) | 186 (31.01) | |
| University studies | 179 (29.9) | 288 (48.16) |
| 3–6 y | 6–12 y | |||||||
|---|---|---|---|---|---|---|---|---|
| Portions/Day | Boys (n = 139; 13%) | Girls (n = 141; 13.2%) | Boys (n = 390; 36.2%) | Girls (n = 405; 37.6%) | ||||
| B | p | B | p | B | p | B | p | |
| Water | 0.06 | 0.567 | 0.18 | 0.042 | −0.03 | 0.637 | −0.036 | 0.592 |
| Soft drinks | −0.03 | 0.921 | −0.13 | 0.906 | 0.44 | 0.013 | 0.320 | 0.121 |
| Juices | 0.03 | 0.838 | −0.12 | 0.400 | 0.09 | 0.275 | −0.500 | 0.624 |
| Sugar-sweetened beverages * | 0.317 | 0.035 | 0.151 | 0.040 | 0.179 | 0.026 | 0.089 | 0.043 |
| Smoothies | 0.07 | 0.417 | −0.02 | 0.876 | −0.02 | 0.841 | 0.106 | 0.138 |
| Milk | −0.15 | 0.148 | −0.09 | 0.296 | −0.05 | 0.524 | −0.19 | 0.032 |
| Yoghurt | −0.03 | 0.831 | −0.37 | 0.093 | −0.07 | 0.596 | −0.17 | 0.222 |
| Dairy products ** | −0.115 | 0.813 | −0.173 | 0.023 | −0.023 | 0.101 | −0.125 | 0.035 |
| 3–6 y | 6–12 y | |||||||
|---|---|---|---|---|---|---|---|---|
| Ref: Yes | Boys (n = 139; 13%) | Girls (n = 141; 13.2%) | Boys (n = 390; 36.2%) | Girls (n = 405; 37.6%) | ||||
| OR * | p | OR * | p | OR * | p | OR * | p | |
| 1. Have a fruit or a natural juice every day | 2.807 | 0.082 | 0.837 | 0.832 | 1.436 | 0.267 | 1.048 | 0.893 |
| 2. Have a second piece of fruit every day | 1381 | 0.536 | 1.274 | 0.676 | 1.188 | 0.541 | 0.815 | 0.471 |
| 3. Eat fresh or cooked vegetables once a day (1 time/day) | 0.815 | 0.722 | 1.922 | 0.299 | 1.321 | 0.323 | 0.818 | 0.519 |
| 4. Eat fresh or cooked vegetables more than once a day (≥1 time/day) | 1.525 | 0.435 | 1.587 | 0.427 | 1.145 | 0.627 | 1.228 | 0.466 |
| 5. Eat fish (2–3 times/week) | 0.419 | 0.280 | 0.569 | 0.607 | 0.896 | 0.736 | 1.206 | 0.554 |
| 6. Visit a fast-food restaurant once or more a week (≥1 time/week) | 0.478 | 0.174 | 1.719 | 0.528 | 1.223 | 0.494 | 0.845 | 0.591 |
| 7. Eat legumes more than one time a week (≥1 time/week) | 0.325 | 0.298 | 1.875 | 0.404 | 0.634 | 0.257 | 1.648 | 0.163 |
| 8. Eat pasta or rice (5 days or more a week) (≥5 times/week) | 1.431 | 0.500 | 1.750 | 0.375 | 1.028 | 0.920 | 0.745 | 0.288 |
| 9. Have a cereal or derivative for breakfast | 1.867 | 0.217 | 1.213 | 0.743 | 1.612 | 0.102 | 0.876 | 0.679 |
| 10. Eat nuts (2–3 times/week) | 1.373 | 0.558 | 0.756 | 0.649 | 1.336 | 0.308 | 2.901 | 0.001 |
| 11. Use olive oil at home | 0.000 | 1.000 | 2.567 | 0.158 | 0.380 | 0.388 | 0.646 | 0.621 |
| 12. Have breakfast | 1.360 | 0.798 | 0.000 | 0.999 | 0.590 | 0.460 | 3.006 | 0.108 |
| 13. Have dairy for breakfast | 0.855 | 0.901 | 0.418 | 0.424 | 1.101 | 0.870 | 1.619 | 0.307 |
| 14. Have a breakfast of industrial pastries, cookies, cupcakes | 0.688 | 0.471 | 2.140 | 0.270 | 1.164 | 0.572 | 1.161 | 0.596 |
| 15. Take two yoghurts and/or 40 g cheese every day | 0.965 | 0.947 | 0.696 | 0.525 | 0.889 | 0.669 | 0.800 | 0.430 |
| 16. Take sweets and/or candies several times a day | 0.424 | 0.153 | 0.913 | 0.916 | 1.042 | 0.937 | 0.803 | 0.605 |
| B ** | p | B ** | p | B ** | p | B ** | p | |
| Total score MD | 0.009 | 0.864 | 0.004 | 0.929 | −0.013 | 0.813 | −0.008 | 0.614 |
| 3–6 y | 6–12 y | |||||||
|---|---|---|---|---|---|---|---|---|
| Boys (n = 139; 13%) | Girls (n = 141; 13.2%) | Boys (n = 390; 36.2%) | Girls (n = 405; 37.6%) | |||||
| B | p | B | p | B | p | B | p | |
| Sleep duration weekday (hours) | −0.106 | 0.247 | 0.093 | 0.421 | −0.147 | 0.035 | −0.142 | 0.040 |
| Sleep duration weekend (hours) | −0.221 | 0.009 | 0.101 | 0.286 | −0.187 | 0.001 | 0.001 | 0.889 |
| TST weekday (hours) | 0.019 | 0.020 | 0.001 | 0.661 | 0.001 | 0.138 | 0.021 | 0.007 |
| TST weekend (hours) | 0.401 | 0.035 | 0.001 | 0.246 | 0.000 | 0.309 | 0.001 | 0.289 |
| PA in club (min/day) | −0.100 | 0.740 | 0.001 | 0.920 | 0.001 | 0.129 | 0.001 | 0.653 |
| Go and back walking to school (min/day) | −0.008 | 0.242 | −0.007 | 0.549 | −0.016 | 0.119 | 0.007 | 0.374 |
| Ref: Always | 3–6 y | 6–12 y | ||||||
|---|---|---|---|---|---|---|---|---|
| In the Last Week | Boys (n = 139; 13%) | Girls (n = 141; 13.2%) | Boys (n = 390; 36.2%) | Girls (n = 405; 37.6%) | ||||
| OR | p | OR | p | OR | p | OR | p | |
| My child was laughing and had a lot of fun | 0.000 | 0.999 | 0.000 | 1.000 | 0.860 | 0.727 | 2.576 | 0.043 |
| My child did not feel good about doing anything | 3.429 | 0.999 | 0.390 | 0.473 | 0.396 | 0.206 | 0.589 | 0.579 |
| My child felt lonely | 2.048 | 0.368 | 2.057 | 0.407 | 0.402 | 0.373 | 0.585 | 0.574 |
| My child felt insecure and anxious | 4.026 | 0.999 | 2.567 | 0.158 | 1.007 | 0.993 | 0.859 | 0.838 |
| My child was proud of himself/herself | 0.401 | 0.397 | 4.714 | 0.056 | 0.734 | 0.346 | 1.335 | 0.388 |
| My child felt on top of the world | 1.074 | 0.892 | 0.703 | 0.594 | 0.751 | 0.364 | 0.993 | 0.981 |
| My child felt good about himself | 0.428 | 0.435 | 1.588 | 0.591 | 1.437 | 0.278 | 2.063 | 0.040 |
| My child had good ideas | 0.290 | 0.247 | 3.773 | 0.060 | 1.262 | 0.522 | 1.575 | 0.186 |
| My child felt comfortable with us as parents | 0.000 | 0.999 | 8.333 | 0.146 | 0.719 | 0.588 | 1.678 | 0.391 |
| My child was comfortable at home | 0.000 | 0.999 | 0.000 | 0.999 | 1.671 | 0.400 | 1.309 | 0.715 |
| We argue at home | 1.200 | 0.871 | 2.79 | 0.999 | 1.096 | 0.858 | 0.451 | 0.141 |
| My child felt overprotected by us | 0.760 | 0.643 | 2.057 | 0.317 | 0.502 | 0.025 | 0.916 | 0.783 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miguel-Berges, M.L.; De Miguel-Etayo, P.; Larruy-García, A.; Jimeno-Martinez, A.; Pellicer, C.; Moreno Aznar, L. Lifestyle Risk Factors for Overweight/Obesity in Spanish Children. Children 2022, 9, 1947. https://doi.org/10.3390/children9121947
Miguel-Berges ML, De Miguel-Etayo P, Larruy-García A, Jimeno-Martinez A, Pellicer C, Moreno Aznar L. Lifestyle Risk Factors for Overweight/Obesity in Spanish Children. Children. 2022; 9(12):1947. https://doi.org/10.3390/children9121947
Chicago/Turabian StyleMiguel-Berges, María L., Pilar De Miguel-Etayo, Alicia Larruy-García, Andrea Jimeno-Martinez, Carmen Pellicer, and Luis Moreno Aznar. 2022. "Lifestyle Risk Factors for Overweight/Obesity in Spanish Children" Children 9, no. 12: 1947. https://doi.org/10.3390/children9121947