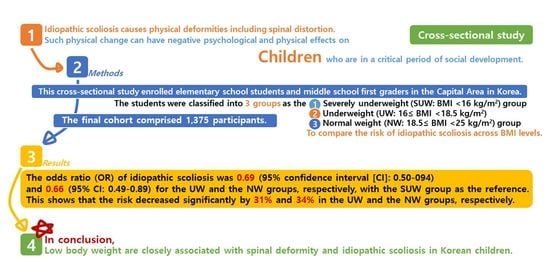
Low Body Mass Index Levels and Idiopathic Scoliosis in Korean Children: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
2.1. Study Subjects
2.2. Measurements
2.2.1. Body Measurements
2.2.2. Identifying Scoliosis
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Effect of BMI on Spinal Deformity and the Risk Factors of Idiopathic Scoliosis
3.3. Risk for Idiopathic Scoliosis According to BMI
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, S.M. Spinal curves and scoliosis. Radiol. Technol. 2007, 79, 44–65. [Google Scholar] [PubMed]
- Hockenberry, M.J.; Wilson, D. Wong’s Nursing Care of Infants and Children; Elsevier Health Sciences: Berlin, Germany, 2014. [Google Scholar]
- Sapountzi-Krepia, D.S.; Valavanis, J.; Panteleakis, G.P.; Zangana, D.T.; Vlachojiannis, P.C.; Sapkas, G.S. Perceptions of body image, happiness and satisfaction in adolescents wearing a Boston brace for scoliosis treatment. J. Adv. Nurs. 2001, 35, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Suh, S.-W.; Modi, H.N.; Yang, J.-H.; Hong, J.-Y. Idiopathic scoliosis in Korean schoolchildren: A prospective screening study of over 1 million children. Eur. Spine J. 2011, 20, 1087–1094. [Google Scholar] [CrossRef] [Green Version]
- Popko, J.; Kwiatkowski, M.; Gałczyk, M. Scoliosis: Review of Diagnosis and Treatment. Pol. J. Appl. Sci. 2018, 4, 31–35. [Google Scholar]
- Wick, J.M.; Konze, J.; Alexander, K.; Sweeney, C. Infantile and juvenile scoliosis: The crooked path to diagnosis and treatment. AORN J. 2009, 90, 347–380. [Google Scholar] [CrossRef]
- Smith, F.; Latchford, G.; Hall, R.; Millner, P.; Dickson, R. Indications of disordered eating behaviour in adolescent patients with idiopathic scoliosis. Bone Jt. J. 2002, 84, 392–394. [Google Scholar] [CrossRef]
- Smith, F.M.; Latchford, G.J.; Hall, R.M.; Dickson, R.A. Do chronic medical conditions increase the risk of eating disorder? A cross-sectional investigation of eating pathology in adolescent females with scoliosis and diabetes. J. Adolesc. Health 2008, 42, 58–63. [Google Scholar] [CrossRef]
- Wake, M.; Clifford, S.; Patton, G.; Waters, E.; Williams, J.; Canterford, L.; Carlin, J. Morbidity patterns among the underweight, overweight and obese between 2 and 18 years: Population-based cross-sectional analyses. Int. J. Obes. 2013, 37, 86–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yong, F.; Wong, H.-K.; Chow, K.-Y. Prevalence of adolescent idiopathic scoliosis among female school children in Singapore. Ann. Acad. Med. Singap. 2009, 38, 1056. [Google Scholar]
- Grieken, A.; Renders, C.; Wijtzes, A.; Hirasing, R.; Raat, H. Overweight, Obesity and Underweight Is Associated with Adverse Psychosocial and Physical Health Outcomes among 7-Year-Old Children: The ‘Be Active, Eat Right’ Study. PLoS ONE 2013, 8, 1–7. [Google Scholar]
- Li, X.; Shen, J.; Liang, J.; Zhou, X.; Yang, Y.; Wang, D.; Wang, S.; Wang, L.; Wang, H.; Du, Q. Effect of core-based exercise in people with scoliosis: A systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 669–680. [Google Scholar] [CrossRef]
- Liu, D.; Yang, Y.; Yu, X.; Yang, J.; Xuan, X.; Yang, J.; Huang, Z. Effects of specific exercise therapy on adolescent patients with idiopathic scoliosis: A prospective controlled cohort study. Spine 2020, 45, 1039. [Google Scholar] [CrossRef]
- Gao, A.; Li, J.; Shao, R.; Yu, M.; Wu, T.; Wang, Y.; Liu, X. Improvement of health-related quality of life and radiographic parameters in adolescent idiopathic scoliosis patients after Schroth exercises. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Jeon, K.; Kim, D.-I. The Association between Low Body Weight and Scoliosis among Korean Elementary School Students. Int. J. Environ. Res. Public Health 2018, 15, 2613. [Google Scholar] [CrossRef] [Green Version]
- Frerich, J.M.; Hertzler, K.; Knott, P.; Mardjetko, S. Comparison of radiographic and surface topography measurements in adolescents with idiopathic scoliosis. Open Orthop. J. 2012, 6, 261. [Google Scholar] [CrossRef] [Green Version]
- Krott, N.L.; Wild, M.; Betsch, M. Meta-analysis of the validity and reliability of rasterstereographic measurements of spinal posture. Eur. Spine J. 2020, 29, 2392–2401. [Google Scholar] [CrossRef] [PubMed]
- Drerup, B.; Hierholzer, E. Back shape measurement using video rasterstereography and three-dimensional reconstruction of spinal shape. Clin. Biomech. 1994, 9, 28–36. [Google Scholar] [CrossRef]
- Schroder, J. Posture analysis: Variations and reliability of biomechnical parameters in bepedal standing by means of Formetric-system. In Proceedings of the 14th Annual Congress of the European College of Sports Science, Oslo, Norway, 24–27 June 2009. [Google Scholar]
- Janicki, J.A.; Alman, B. Scoliosis: Review of diagnosis and treatment. Paediatr. Child Health 2007, 12, 771. [Google Scholar] [CrossRef] [Green Version]
- Goldbloom, R.B. Screening for idiopathic adolescent scoliosis. In Canadian Task Force on the Periodic Health Examination; CMAJ: Ottawa, Canada, 1994; pp. 346–354. [Google Scholar]
- Lonstein, J.E.; Bjorklund, S.; Wanninger, M.H.; Nelson, R.P. Voluntary school screening for scoliosis in Minnesota. J. Bone Jt. Surg. Am. 1982, 64, 481–488. [Google Scholar]
- Ohtsuka, Y.; Yamagata, M.; Arai, S.; Kitahara, H.; Minami, S. School screening for scoliosis by the Chiba University Medical School screening program: Results of 1.24 million students over an 8-year period. Spine 1988, 13, 1251–1257. [Google Scholar]
- Willner, S.; Udén, A. A prospective prevalence study of scoliosis in Southern Sweden. Acta Orthop. Scand. 1982, 53, 233–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soucacos, P.N.; Zacharis, K.; Soultanis, K.; Gelalis, J.; Xenakis, T.; Beris, A.E. Risk factors for idiopathic scoliosis: Review of a 6-year prospective study. Orthopedics 2000, 23, 833–838. [Google Scholar] [CrossRef]
- Wong, H.-K.; Hui, J.H.; Rajan, U.; Chia, H.-P. Idiopathic scoliosis in Singapore schoolchildren: A prevalence study 15 years into the screening program. Spine 2005, 30, 1188–1196. [Google Scholar] [CrossRef]
- Wang, W.; Wang, Z.; Zhu, Z.; Zhu, F.; Qiu, Y. Body composition in males with adolescent idiopathic scoliosis: A case–control study with dual-energy X-ray absorptiometry. BMC Musculoskelet. Disord. 2016, 17, 107. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Wang, C.; Hu, W.; Hu, F.; Liu, W.; Zhang, X. Disordered leptin and ghrelin bioactivity in adolescent idiopathic scoliosis (AIS): A systematic review and meta-analysis. J. Orthop. Surg. Res. 2020, 15, 1–9. [Google Scholar] [CrossRef]
- Bae, S.H.; Goh, T.S.; Kim, D.S.; Lee, J.S. Leptin in adolescent idiopathic scoliosis—A meta-analysis. J. Clin. Neurosci. 2020, 71, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.-T.; Li, J.; Wang, Y.-J.; Xiao, L.-G.; Yang, G.-T.; Zhang, H.-Q. Ghrelin up-regulates cartilage-specific genes via the ERK/STAT3 pathway in chondrocytes of patients with adolescent idiopathic scoliosis. Biochem. Biophys. Res. Commun. 2019, 518, 259–265. [Google Scholar] [CrossRef]
- Baker, D.; Roberts, R.; Towell, T. Factors predictive of bone mineral density in eating-disordered women: A longitudinal study. Int. J. Eat. Disord. 2000, 27, 29–35. [Google Scholar] [CrossRef]

| Variables Total (n = 1375) | Male (n = 749) | Female (n = 626) | p-Value |
|---|---|---|---|
| Age (years) | 10.86 ± 1.29 | 10.89 ± 1.28 | 0.686 |
| Weight (kg) | 39.38 ± 9.27 | 38.11 ± 16.13 | 0.069 |
| Height (cm) | 144.22 ± 10.08 | 143.72 ± 10.98 | 0.377 |
| Lean Body Mass (kg) | 15.84 ± 4.18 | 14.40 ± 3.34 | <0.001 |
| Body Fat (kg) | 9.26 ± 4.74 | 9.69 ± 4.36 | 0.085 |
| Percent Body Fat (%) | 22.76 ± 8.36 | 24.88 ± 7.27 | <0.001 |
| BMI (kg/m2) | 18.70 ± 2.70 | 17.93 ± 2.55 | <0.001 |
| Trunk Length (mm) | 369.77 ± 34.04 | 373.46 ± 37.67 | 0.059 |
| Sagittal Imbalance (°) | 1.87 ± 2.97 | 1.70 ± 2.87 | 0.284 |
| Coronal Imbalance (°) | −0.20 ± 1.52 | −0.14 ± 1.49 | 0.418 |
| Pelvic Inclination (°) | 0.28 ± 2.98 | 0.24 ± 2.79 | 0.794 |
| Pelvic Torsion (°) | 0.78 ± 2.46 | 0.92 ± 2.26 | 0.309 |
| Pelvis Rotation (°) | −1.50 ± 4.51 | −1.23 ± 4.63 | 0.260 |
| Kyphotic Angle (°) | 42.39 ± 8.67 | 42.38 ± 9.35 | 0.994 |
| Lordotic Angle (°) | 34.55 ± 7.96 | 35.83 ± 8.05 | 0.003 |
| Trunk Torsion (°) | −0.11 ± 5.87 | 0.34 ± 5.43 | 0.134 |
| Scoliosis Angle (°) | 11.04 ± 4.49 | 11.55 ± 4.81 | 0.041 |
| Severely Underweight (BMI < 16) | Underweight (16 ≤ BMI < 18.5) | Normal Weight (18.5 ≤ BMI < 25) | |
|---|---|---|---|
| Boys (n = 750) | n = 113 | n = 272 | n = 365 |
| Age-Adjusted | |||
| Scoliosis Angle (°) | 12.41 ± 4.96 | 11.13 ± 4.24 * | 10.55 ± 4.44 * |
| Girls (n = 625) | n = 157 | n = 228 | n = 240 |
| Age-Sdjusted | |||
| Scoliosis Angle (°) | 11.79 ± 4.62 | 11.33 ± 5.14 | 11.60 ± 4.63 |
| All Subjects (n = 1375) | n = 270 | n = 500 | n = 605 |
| Age and Gender-Adjusted | |||
| Scoliosis Angle (°) | 12.04 ± 4.77 | 11.22 ± 4.67 | 10.97 ± 4.54 * |
| Lean Mass (kg) | 11.98 ± 2.10 | 14.60 ± 3.22 * | 17.10 ± 3.90 * ^ |
| Body Fat (kg) | 4.93 ± 1.51 | 7.31 ± 2.24 * | 13.25 ± 3.89 * ^ |
| Percent Body Fat (%) | 17.24 ± 5.00 | 20.78 ± 6.00 * | 29.07 ± 6.96 * ^ |
| Trunk Length (mm) | 357.25 ± 29.91 | 369.40 ± 37.12 | 379.46 ± 34.90 * ^ |
| Sagittal Imbalance (°) | 1.01 ± 2.92 | 1.70 ± 2.97 * | 2.22 ± 2.82 * ^ |
| Coronal Imbalance (°) | −0.23 ± 1.55 | −0.21 ± 1.43 | −0.12 ± 1.55 |
| Pelvic Inclination (°) | 0.28 ± 3.13 | 0.30 ± 2.71 | 0.22 ± 2.93 |
| Pelvic Torsion (°) | 1.20 ± 2.36 | 0.94 ± 2.25 | 0.60 ± 2.45 * ^ |
| Pelvis Rotation (°) | −0.80 ± 5.01 | −1.47 ± 4.55 | −1.55 ± 4.36 |
| Kyphotic Angle (°) | 38.64 ± 9.47 | 41.44 ± 8.48 * | 44.83 ± 8.45 * ^ |
| Lordotic Angle (°) | 33.02 ± 8.07 | 35.16 ± 8.39 * | 36.02 ± 7.49 * ^ |
| Trunk Torsion (°) | 0.61 ± 6.98 | 0.02 ± 5.37 | −0.09 ± 5.24 |
| Severely Underweight (BMI < 16) | Underweight (16 ≤ BMI < 18.5) | Normal Weight (18.5 ≤ BMI < 25) | ||
|---|---|---|---|---|
| Boys (n = 750) | n = 113 | n = 272 | n = 365 | |
| OR (95% CI) | ||||
| Scoliosis | 1 | 0.73 (0.46–1.17) | 0.50 (0.32–0.78) | |
| Age-Adjusted OR (95% CI) | ||||
| Scoliosis | 1 | 0.76 (0.47–1.22) | 0.53 (0.33–0.83) | |
| Girls (n = 625) | n = 157 | n = 228 | n = 240 | |
| OR (95% CI) | ||||
| Scoliosis | 1 | 0.61 (0.40–0.94) | 0.96 (0.63–1.47) | |
| Age-Adjusted OR (95% CI) | ||||
| Scoliosis | 1 | 0.63 (0.41–0.97) | 0.99 (0.64–1.54) | |
| All Subjects (n = 1375) | n = 270 | n = 500 | n = 605 | |
| OR (95% CI) | ||||
| Scoliosis | 1 | 0.69 (0.50–0.94) | 0.66 (0.49–0.89) | |
| Gender-Adjusted OR (95% CI) | ||||
| Scoliosis | 1 | 0.69 (0.51–0.95) | 0.67 (0.49–0.91) | |
| Age and Gender-Adjusted OR (95% CI) | ||||
| Scoliosis | 1 | 0.72 (0.52–0.98) | 0.70 (0.51–0.96) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, K.-k.; Kim, D.-i. Low Body Mass Index Levels and Idiopathic Scoliosis in Korean Children: A Cross-Sectional Study. Children 2021, 8, 570. https://doi.org/10.3390/children8070570
Jeon K-k, Kim D-i. Low Body Mass Index Levels and Idiopathic Scoliosis in Korean Children: A Cross-Sectional Study. Children. 2021; 8(7):570. https://doi.org/10.3390/children8070570
Chicago/Turabian StyleJeon, Kyoung-kyu, and Dong-il Kim. 2021. "Low Body Mass Index Levels and Idiopathic Scoliosis in Korean Children: A Cross-Sectional Study" Children 8, no. 7: 570. https://doi.org/10.3390/children8070570