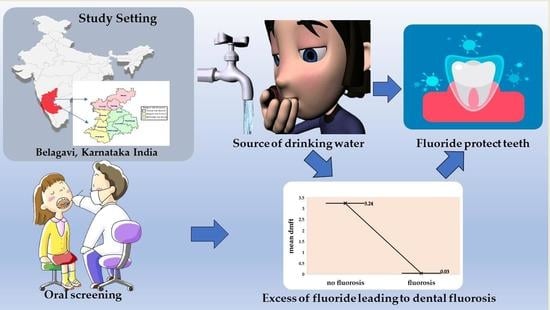
Pediatric Dental Fluorosis and Its Correlation with Dental Caries and Oral-Health-Related Quality of Life: A Descriptive Cross-Sectional Study among Preschool Children Living in Belagavi
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Size Calculation and Sampling Technique
- Prevalence of Dental Fluorosis: (p) = 77%;
- Free of Dental Fluorosis: (q) = (1 − p) = 23%;
- Absolute Admissible Error: (d) = 2.5%.
- Children 3–5 years of age attending government-sponsored child-care development Centers at Belagavi;
- Children whose parents were willing to give written informed consent.
- Physically or medically compromised children;
- Children with debilitating diseases or suffering from uncontrolled systemic conditions.
2.2. Clinical Examinations
2.3. Questionnaires and Data Collection
2.3.1. Development of the Questionnaire
2.3.2. Details of the Questionnaire
2.3.3. Data Collection Procedure
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hong, L.; Levy, S.M.; Warren, J.J.; Bergus, G.R.; Dawson, D.V.; Wefel, J.S.; Broffitt, B. Primary tooth fluorosis and amoxicillin use during infancy. J. Public Health Dent. 2004, 64, 38–44. [Google Scholar] [CrossRef]
- Levy, S.M.; Hillis, S.L.; Warren, J.J.; Broffitt, B.A.; Mahbubul Islam, A.K.; Wefel, J.S.; Kanellis, M.J. Primary tooth fluorosis and fluoride intake during the first year of life. Community Dent. Oral Epidemiol. 2002, 30, 286–295. [Google Scholar] [CrossRef]
- Susheela, A.K. Fluorosis management programme in India. Curr. Sci. 1999, 77, 1250–1256. [Google Scholar]
- Mann, J.; Mahmoud, W.; Ernest, M.; Sgan-Cohen, H.; Shoshan, N.; Gedalia, I. Fluorosis and dental caries in 6–8-year-old children in a 5 ppm fluoride area. Community Dent. Oral Epidemiol. 1990, 18, 77–79. [Google Scholar] [CrossRef]
- Fomon, S.J.; Ekstrand, J.; Ziegler, E.E. Fluoride intake and prevalence of dental fluorosis: Trends in fluoride intake with special attention to infants. J. Public Health Dent. 2000, 60, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Ruan, J.P.; Wang, Z.L.; Yang, Z.Q.; Bårdsen, A.; Åstrøm, A.N.; Bjorvatn, K. Dental fluorosis in primary teeth: A study in rural schoolchildren in Shaanxi Province, China. Int. J. Paediatr. Dent. 2005, 15, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Do, L.G.; Spencer, A. Oral health-related quality of life of children by dental caries and fluorosis experience. J. Public Health Dent. 2007, 67, 132–139. [Google Scholar] [CrossRef]
- Robinson, P.G.; Nalweyiso, N.; Busingye, J.; Whitworth, J. Subjective impacts of dental caries and fluorosis in rural Ugandan children. Community Dent. Health 2005, 22, 231. [Google Scholar] [PubMed]
- Pakkhesal, M.; Riyahi, E.; Naghavi Alhosseini, A.A.; Amdjadi, P.; Behnampour, N. Impact of dental caries on oral health related quality of life among preschool children: Perceptions of parents. BMC Oral Health 2021, 21, 1–8. [Google Scholar] [CrossRef]
- Reddy, K.S.; Puppala, R.; Kethineni, B.; Reddy, H.; Reddy, A.; Kalyan, V.S. Prevalence of Dental Fluorosis Among 6–12-Year-Old School Children of Mahabubnagar District, Telangana State, India—A Cross-Sectional Study. J. Indian Assoc. Public Health Dent. 2017, 15, 42. [Google Scholar]
- Belgaum—Central Ground Water Board (CGWB). Available online: http://cgwb.gov.in/District_Profile/karnataka/2012/Belgaum_brochure%202012 (accessed on 11 December 2022).
- Kumar, V.; Ankola, A.; Sankeshwari, R.; Jalihal, S.; Atre, S.; Mallineni, S.K. Determination of the oral health status and behaviors, treatment needs, and guardians’ perception of oral health among preschool children attending Integrated Child Developmental Scheme Anganwadi centers of Belagavi, South India: A cross-sectional study. J. Clin. Transl. Res. 2021, 7, 436. [Google Scholar] [PubMed]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Priya, H.; Acharya, S.; Kumar, M.; Bhat, M.; Purohit, B. Oral Health Status and Treatment Need Among Preschool Children Attending Anganwadi Centres—A Comparative Study. Oral Health Prev. Dent. 2012, 10, 355. [Google Scholar]
- Shivayogimath, C.B.; Hiremath, M.N.; Shivalingappa, S.N. Prevalence of dental Fluorosis among residents of nine villages in and around mundaragi of Gadag district in Karnataka. India Elixir Pollut. 2012, 50, 10410. [Google Scholar]
- Chowdhury, C.R.; Shahnawaz, K.; Kumari, D.; Chowdhury, A.; Bedi, R.; Lynch, E.; Harding, S.; Grootveld, M. Spatial distribution mapping of drinking water fluoride levels in Karnataka, India: Fluoride-related health effects. Perspect. Public Health 2016, 136, 353–360. [Google Scholar]
- Divyalalitha, N.; Manipal, S.; Bharatwaj, V.V.; Prabu, D. The impact of integration of a dental module into the existing integrated child development services scheme in Chennai, India. J. Family Med. Prim. Care 2020, 9, 4841–4846. [Google Scholar] [CrossRef]
- Pontigo-Loyola, A.P.; Medina-Solís, C.E.; Lara-Carrillo, E.; Patiño-Marín, N.; Escoffié-Ramirez, M.; Mendoza-Rodríguez, M.; De La Rosa-Santillana, R.; Maupomé, G. Impact of socio-demographic, socioeconomic, and water variables on dental fluorosis in adolescents growing up during the implementation of a fluoridated domestic salt program. Odontology 2014, 102, 105–115. [Google Scholar] [CrossRef]
- Angulo, M.; Cuitiño, E.; Molina-Frechero, N.; Emilson, C.G. The association between the prevalence of dental fluorosis and the socio-economic status and area of residence of 12-year-old students in Uruguay. Acta Odontol. Scand. 2020, 78, 26–30. [Google Scholar] [CrossRef]
- Thylstrup, A. Distribution of dental fluorosis in the primary dentition. Community Dent. Oral Epidemiol. 1978, 6, 329–337. [Google Scholar] [CrossRef]
- Sami, E.; Vichayanrat, T.; Satitvipawee, P. Dental fluorosis and its relation to socioeconomic status, parents’ knowledge and awareness among 12-year-old school children in Quetta, Pakistan. Southeast Asian J. Trop. Med. Public Health 2015, 46, 360. [Google Scholar]
- Warren, J.J.; Levy, S.M.; Kanellis, M.J. Prevalence of dental fluorosis in the primary dentition. J. Public Health Dent. 2001, 61, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Marshall, T.A.; Levy, S.M.; Warren, J.J.; Broffitt, B.; Eichenberger-Gilmore, J.M.; Stumbo, P.J. Associations between intakes of fluoride from beverages during infancy and dental fluorosis of primary teeth. J. Am. Coll. Nutr. 2004, 23, 108–116. [Google Scholar] [CrossRef]
- Larsen, M.J.; Senderovitz, F.; Kirkegaard, E.; Poulsen, S.; Fejerskov, O. Dental Fluorosis in the Primary and the Permanent Dentition in Fluoridated Areas with Consumption of either Powdered Milk or Natural Cow’s Milk. J. Dent. Res. 1988, 67, 822–825. [Google Scholar] [CrossRef] [PubMed]
- Duarte, M.B.S.; Carvalho, V.R.; Hilgert, L.A.; Ribeiro, A.P.D.; Leal, S.C.; Takeshita, E.M. Is there an association between dental caries, fluorosis, and molar-incisor hypomineralization? J. Appl. Oral Sci. 2021, 29, e20200890. [Google Scholar] [CrossRef]
- Sajadi, F.S.; Pishbin, L.; Azhari, S.H.; Moosazadeh, M. Impact of oral and dental health on children’s and parents’ quality of life based on early childhood oral health impact scale (ECOHIS) index. Int. J. Dent. Sci. Res. 2015, 3, 28–31. [Google Scholar] [CrossRef]
- Scarpelli, A.C.; Oliveira, B.H.; Tesch, F.C.; Leão, A.T.; Pordeus, I.A.; Paiva, S.M. Psychometric properties of the Brazilian version of the Early Childhood Oral Health Impact Scale (B-ECOHIS). BMC Oral Health 2011, 11, 19. [Google Scholar] [CrossRef] [Green Version]
- Sakaryali, D.; Bani, M.; Cinar, C.; Alacam, A. Evaluation of the impact of early childhood caries, traumatic dental injury, and malocclusion on oral health-related quality of life for Turkish preschool children and families. Niger J. Clin. Pract. 2019, 22, 817. [Google Scholar] [CrossRef]
| Number of Participants | Enamel Fluorosis | p-Value | |
|---|---|---|---|
| Age | |||
| 3 years | 493 (41.08) | 3 (0.6) | 0.106 |
| 4 years | 518 (43.17) | 3 (0.58) | |
| 5 years | 189 (15.75) | 4 (2.1) | |
| Gender | |||
| Male | 589 (49.08) | 6 (1.01) | 0.488 |
| Female | 611 (50.92) | 4 (0.7) | |
| Socio-economic status | |||
| Upper | 36 (3) | 0 | 0.004 * |
| Upper middle | 175 (14.58) | 0 | |
| Lower middle | 216 (18) | 5 (13.8) | |
| Lower | 773 (64.42) | 5 (2.9) | |
| Migration status | |||
| Non-migrant | 923 (76.92) | 2 (0.22) | ≤0.001 * |
| Migrant | 277 (23.08) | 8 (2.9) | |
| Duration in government-development center | |||
| 1 year | 505 (42.08) | 10 (100) | ≤0.001 * |
| 2 years | 506 (42.17) | 0 | |
| 3 years | 189 (15.75) | 0 | |
| Level of education of mother | |||
| Primary school | 644 (53.67) | 8 (1.24) | 0.093 |
| High school | 556 (46.33) | 2 (0.36) | |
| Age of stating tooth brushing | |||
| <2 years | 527 | 9 (1.71) | 0.003 * |
| >2 years | 673 | 1 (0.15) | |
| Variable Group | Mean ± SD | p-Value |
|---|---|---|
| dmft, no fluorosis | 3.24 ± 1.75 | 0.001 * |
| dmft, fluorosis | 0.03 ± 0.02 |
| Number of Subjects | Enamel Fluorosis | Non-Enamel Fluorosis | Relative Risk | Odds Ratio (OR) | p-Value | ||
|---|---|---|---|---|---|---|---|
| Migration status | Non-migrant | 923 | 2 | 921 | 0.08 | 1 a | 0.001 * |
| Migrant | 277 | 8 | 269 | 13.15 | 2.43 | ||
| Brushing frequency | ≥2 times/day | 683 | 10 | 673 | 0.015 | 1.23 | 0.002 * |
| <2/day | 517 | 0 | 517 | 1 a |
| Parents Perception | Never N (%) | Hardly Ever N (%) | Occasionally N (%) | Often N (%) | Very Often N (%) | p-Value |
|---|---|---|---|---|---|---|
| Oral/dental pain | 486 (40.5) | 227 (18.92) | 126 (10.5) | 157 (13.08) | 204 (17) | 0.0044 * |
| Male | 283 (48.05) | 59 (10.02) | 77 (13.07) | 65 (11.03) | 105 (17.83) | |
| Female | 203 (33.22) | 168 (27.49) | 49 (8.02) | 92 (15.06) | 99 (16.20) | |
| Difficulty eating and drinking | 829 (69.08) | 215 (17.92) | 71 (5.92) | 65 (5.42) | 20(1.67) | 0.083 |
| Male | 481 (81.66) | 36 (6.11) | 16 (2.72) | 40 (6.79) | 16 (2.72) | |
| Female | 348 (56.95) | 179 (29.30) | 55 (9.00) | 25 (4.09) | 4 (0.65) | |
| Difficulty pronouncing words | 963 (80.25) | 105 (8.75) | 28 (2.33) | 58 (4.83) | 46 (3.83) | 0.533 |
| Male | 459 (77.93) | 59 (10.02) | 18 (3.06) | 27 (4.58) | 26 (4.41) | |
| Female | 504 (82.49) | 46 (7.53) | 10 (1.64) | 31 (5.07) | 20 (3.27) | |
| Trouble sleeping | 213(17.75) | 262(21.83) | 377(31.42) | 181(15.08) | 167(13.92) | ≤0.001 * |
| Male | 111 (18.84) | 96 (16.30) | 254 (43.12) | 75 (12.73) | 53 (8.99) | |
| Female | 102 (16.69) | 166 (27.17) | 123 (20.13) | 106 (17.35) | 114 (18.66) | |
| Irritable or frustrated | 398 (33.17) | 316 (26.33) | 150 (12.5) | 207 (17.25) | 129 (10.75) | ≤0.001 * |
| Male | 186 (31.58) | 169 (28.69) | 62 (10.53) | 109 (18.50) | 63 (10.70) | |
| Female | 212 (34.70) | 147 (24.96) | 88 (14.40) | 98 (16.04) | 66 (10.80) | |
| Avoids talking or smiling or laughing | 533 (44.42) | 245 (20.42) | 224 (18.67) | 92 (7.67) | 106 (8.83) | 0.067 |
| Male | 284 (48.22) | 101 (17.15) | 124 (21.05) | 36 (6.11) | 44 (7.47) | |
| Female | 249 (40.75) | 144 (23.57) | 100 (16.37) | 56 (9.16) | 62 (10.15) | |
| Child’s teeth and gums cleaning | 27 (2.25) | 189 (15.75) | 363 (30.25) | 438 (36.5) | 183 (15.25) | ≤0.001 * |
| Male | 15 (2.55) | 72 (1.22) | 184 (31.24) | 232 (39.39) | 86 (14.60) | |
| Female | 12 (1.96) | 117 (19.15) | 179 (29.30) | 206 (33.71) | 97 (15.87) | |
| Rinsing child’s mouth after every meal | 192 (16) | 284 (23.67) | 305 (25.42) | 260 (21.67) | 159 (13.25) | 0.368 |
| Male | 78 (13.24) | 164 (27.84) | 113 (19.18) | 146 (24.79) | 88 (14.94) | |
| Female | 114 (18.66) | 120 (19.64) | 192 (31.42) | 114 (18.66) | 71 (11.62) | |
| Brushing twice daily | 56 (4.67) | 276 (23) | 439 (36.58) | 211 (17.58) | 218 (18.17) | ≤0.001 * |
| Male | 18 (3.06) | 145 (24.62) | 229 (38.88) | 96 (15.71) | 101 (17.15) | |
| Female | 38 (6.22) | 131 (21.44) | 210 (34.37) | 115 (18.82) | 117 (19.15) | |
| Quantity of toothpaste supervised | 351 (29.25) | 454 (37.83) | 295 (24.58) | 86 (7.17) | 14 (1.17) | ≤0.001 * |
| Male | 168 (28.52) | 241 (40.92) | 137 (23.26) | 38 (6.45) | 5 (0.85) | |
| Female | 183 (29.95) | 213 (34.86) | 158 (25.86) | 48 (7.85) | 9 (1.47) | |
| Changing the toothbrush | 265 (22.08) | 337 (28.08) | 226 (18.83) | 197 (16.42) | 175 (14.58) | 0.293 |
| Male | 136 (23.09) | 138 (23.43) | 134 (22.75) | 89 (15.11) | 92 (15.62) | |
| Female | 129 (21.11) | 199 (32.57) | 92 (15.06) | 108 (17.67) | 83 (13.58) | |
| Dentist visit for check up | 368 (30.67) | 218 (18.17) | 207 (17.25) | 238 (19.83) | 169 (14.08) | 0.062 |
| Male | 190 (32.26) | 116 (19.69) | 85 (14.43) | 115 (19.52) | 83 (14.09) | |
| Female | 178 (29.13) | 102 (16.69) | 122 (19.97) | 123 (20.13) | 86 (14.07) | |
| Overall Mean ± SD # | 10.74 ± 2.06 | |||||
| Dmft Index Scores | Dean’s Fluorosis Index Scores | ||
|---|---|---|---|
| ECOHIS score | Correlation coefficient (rho) | 0.375 | −0.142 |
| Sig. (2-tailed) p-value | ≤0.001 * | 0.028 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumar, V.; Gaunkar, R.; Thakker, J.; Ankola, A.V.; Iranna Hebbal, M.; Khot, A.J.P.; Goyal, V.; Ali, A.; Eldwakhly, E. Pediatric Dental Fluorosis and Its Correlation with Dental Caries and Oral-Health-Related Quality of Life: A Descriptive Cross-Sectional Study among Preschool Children Living in Belagavi. Children 2023, 10, 286. https://doi.org/10.3390/children10020286
Kumar V, Gaunkar R, Thakker J, Ankola AV, Iranna Hebbal M, Khot AJP, Goyal V, Ali A, Eldwakhly E. Pediatric Dental Fluorosis and Its Correlation with Dental Caries and Oral-Health-Related Quality of Life: A Descriptive Cross-Sectional Study among Preschool Children Living in Belagavi. Children. 2023; 10(2):286. https://doi.org/10.3390/children10020286
Chicago/Turabian StyleKumar, Vaibhav, Ridhima Gaunkar, Jasleen Thakker, Anil V. Ankola, Mamata Iranna Hebbal, Atrey J. Pai Khot, Virinder Goyal, Amel Ali, and Elzahraa Eldwakhly. 2023. "Pediatric Dental Fluorosis and Its Correlation with Dental Caries and Oral-Health-Related Quality of Life: A Descriptive Cross-Sectional Study among Preschool Children Living in Belagavi" Children 10, no. 2: 286. https://doi.org/10.3390/children10020286