Psychiatric Disorders and Obesity in Childhood and Adolescence—A Systematic Review of Cross-Sectional Studies
Abstract
:1. Introduction
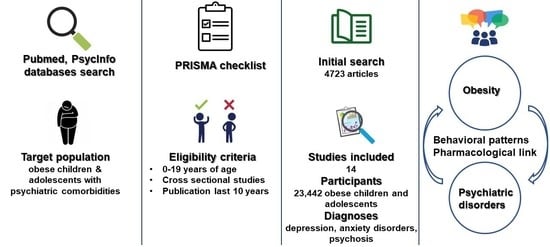
2. Materials and Methods
- ▪ the research question formulation
- ▪ the extensive literature review of the topic
- ▪ the data extraction and evaluation, and lastly
- ▪ the data presentation and analysis.
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Data Extraction
2.4. Data Evaluation
3. Results
3.1. Study Selection
3.2. Basic Characteristics of Included Studies
3.3. Quality Evaluation of the Included Studies
3.4. Main Findings Regarding the Research Question
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Helath Organization. Obesity and Overweight 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 11 November 2022).
- Whitlock, G.; Lewington, S.; Sherliker, P.; Clarke, R.; Emberson, J.; Halsey, J.; Qizilbash, N.; Collins, R.; Peto, R. Prospective Studies Collaboration Body-Mass Index and Cause-Specific Mortality in 900,000 Adults: Collaborative Analyses of 57 Prospective Studies. Lancet 2009, 373, 1083–1096. [Google Scholar] [CrossRef] [PubMed]
- Zanganeh, M.; Adab, P.; Li, B.; Frew, E. A Systematic Review of Methods, Study Quality, and Results of Economic Evaluation for Childhood and Adolescent Obesity Intervention. Int. J. Environ. Res. Public Health 2019, 16, 485. [Google Scholar] [CrossRef] [PubMed]
- Psaltopoulou, T.; Tzanninis, S.; Ntanasis-Stathopoulos, I.; Panotopoulos, G.; Kostopoulou, M.; Tzanninis, I.-G.; Tsagianni, A.; Sergentanis, T.N. Prevention and Treatment of Childhood and Adolescent Obesity: A Systematic Review of Meta-Analyses. World J. Pediatr. 2019, 15, 350–381. [Google Scholar] [CrossRef]
- Kitani, R.A.; Letsou, K.; Kokka, I.; Kanaka-Gantenbein, C.; Bacopoulou, F. Difference in Hair Cortisol Concentrations between Obese and Non-Obese Children and Adolescents: A Systematic Review. Children 2022, 9, 715. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Guo, J.; Zhang, X.; Lu, Y.; Miao, J.; Xue, H. Obesity Is a Risk Factor for Central Precocious Puberty: A Case-Control Study. BMC Pediatr. 2021, 21, 509. [Google Scholar] [CrossRef]
- Centers for Disease Control Prevention Clinical Growth Charts 2017.
- Schwimmer, J.B. Health-Related Quality of Life of Severely Obese Children and Adolescents. JAMA 2003, 289, 1813. [Google Scholar] [CrossRef] [PubMed]
- Ottova, V.; Erhart, M.; Rajmil, L.; Dettenborn-Betz, L.; Ravens-Sieberer, U. Overweight and Its Impact on the Health-Related Quality of Life in Children and Adolescents: Results from the European KIDSCREEN Survey. Qual. Life Res. 2012, 21, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Keating, C.L.; Moodie, M.L.; Swinburn, B.A. The Health-Related Quality of Life of Overweight and Obese Adolescents—A Study Measuring Body Mass Index and Adolescent-Reported Perceptions. Int. J. Pediatr. Obes. 2011, 6, 434–441. [Google Scholar] [CrossRef]
- Meixner, L.; Cohrdes, C.; Schienkiewitz, A.; Mensink, G.B.M. Health-Related Quality of Life in Children and Adolescents with Overweight and Obesity: Results from the German KIGGS Survey. BMC Public Health 2020, 20, 1722. [Google Scholar] [CrossRef]
- Britz, B.; Siegfried, W.; Ziegler, A.; Lamertz, C.; Herpertz-Dahlmann, B.; Remschmidt, H.; Wittchen, H.-U.; Hebebrand, J. Rates of Psychiatric Disorders in a Clinical Study Group of Adolescents with Extreme Obesity and in Obese Adolescents Ascertained via a Population Based Study. Int. J. Obes. 2000, 24, 1707–1714. [Google Scholar] [CrossRef] [Green Version]
- Turco, G.; Bobbio, T.; Reimão, R.; Rossini, S.; Pereira, H.; Barros Filho, A. Quality of Life and Sleep in Obese Adolescents. Arq. Neuro-Psiquiatr. 2013, 71, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Schreckenbach, J.; Reis, O.; Häßler, F. Übergewicht von Kindern und Jugendlichen und sein Zusammenhang mit internalisierenden und externalisierenden psychischen Auffälligkeiten. Prax. Der Kinderpsychol. Und Kinderpsychiatr. 2021, 70, 182–197. [Google Scholar] [CrossRef] [PubMed]
- Hestetun, I.; Svendsen, M.V.; Oellingrath, I.M. Associations between Overweight, Peer Problems, and Mental Health in 12–13-Year-Old Norwegian Children. Eur. Child Adolesc. Psychiatry 2015, 24, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Onal Sonmez, A. Attention Deficit Hyperactivity Disorder Symptoms and Behavioral Problems in Children and Adolescents with Obesity. Sisli Etfal 2019. [Google Scholar] [CrossRef]
- Washington, R.L. Childhood Obesity: Issues of Weight Bias. Prev. Chronic Dis. 2011, 8, A94. [Google Scholar] [PubMed]
- Yu, B. Kindergarten Obesity and Academic Achievement: The Mediating Role of Weight Bias. Front. Psychol. 2021, 12, 640474. [Google Scholar] [CrossRef]
- Nutter, S.; Russell-Mayhew, S.; Alberga, A.S.; Arthur, N.; Kassan, A.; Lund, D.E.; Sesma-Vazquez, M.; Williams, E. Positioning of Weight Bias: Moving towards Social Justice. J. Obes. 2016, 2016, 3753650. [Google Scholar] [CrossRef]
- Mental Disorders Collaborators. Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Barican, J.L.; Yung, D.; Schwartz, C.; Zheng, Y.; Georgiades, K.; Waddell, C. Prevalence of Childhood Mental Disorders in High-Income Countries: A Systematic Review and Meta-Analysis to Inform Policymaking. Evid. Based Ment. Health 2022, 25, 36–44. [Google Scholar] [CrossRef]
- Kokka, I.; Mourikis, I.; Nicolaides, N.C.; Darviri, C.; Chrousos, G.P.; Kanaka-Gantenbein, C.; Bacopoulou, F. Exploring the Effects of Problematic Internet Use on Adolescent Sleep: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 760. [Google Scholar] [CrossRef]
- Kokka, I.; Chrousos, G.P.; Darviri, C.; Bacopoulou, F. Measuring Adolescent Chronic Stress: A Review of Established Biomarkers and Psychometric Instruments. Horm. Res. Paediatr. 2022. [Google Scholar] [CrossRef]
- World Health Organization Adolescent Mental Health 2018.
- Lewinsohn, P. Major Depressive Disorder in Older AdolescentsPrevalence, Risk Factors, and Clinical Implications. Clin. Psychol. Rev. 1998, 18, 765–794. [Google Scholar] [CrossRef]
- da Luz, F.; Hay, P.; Touyz, S.; Sainsbury, A. Obesity with Comorbid Eating Disorders: Associated Health Risks and Treatment Approaches. Nutrients 2018, 10, 829. [Google Scholar] [CrossRef]
- Blasco, B.V.; García-Jiménez, J.; Bodoano, I.; Gutiérrez-Rojas, L. Obesity and Depression: Its Prevalence and Influence as a Prognostic Factor: A Systematic Review. Psychiatry Investig. 2020, 17, 715–724. [Google Scholar] [CrossRef]
- McElroy, S.L.; Frye, M.A.; Suppes, T.; Dhavale, D.; Keck, P.E.; Leverich, G.S.; Altshuler, L.; Denicoff, K.D.; Nolen, W.A.; Kupka, R.; et al. Correlates of Overweight and Obesity in 644 Patients With Bipolar Disorder. J. Clin. Psychiatry 2002, 63, 207–213. [Google Scholar] [CrossRef]
- McElroy, S.L.; Kotwal, R.; Malhotra, S.; Nelson, E.B.; Keck, P.E.; Nemeroff, C.B. Are Mood Disorders and Obesity Related? A Review for the Mental Health Professional. J. Clin. Psychiatry 2004, 65, 634–651. [Google Scholar] [CrossRef]
- Dickerson, F.B.; Brown, C.H.; Kreyenbuhl, J.A.; Fang, L.; Goldberg, R.W.; Wohlheiter, K.; Dixon, L.B. Obesity among Individuals with Serious Mental Illness. Acta Psychiatr. Scand. 2006, 113, 306–313. [Google Scholar] [CrossRef]
- Theisen, F.M.; Linden, A.; Geller, F.; Schäfer, H.; Martin, M.; Remschmidt, H.; Hebebrand, J. Prevalence of Obesity in Adolescent and Young Adult Patients with and without Schizophrenia and in Relationship to Antipsychotic Medication. J. Psychiatr. Res. 2001, 35, 339–345. [Google Scholar] [CrossRef]
- Fentie, D.; Derese, T. Prevalence and Associated Factors of Overweight/Obesity among Severely Ill Psychiatric Patients in Eastern Ethiopia: A Comparative Cross-Sectional Study. PLoS ONE 2022, 17, e0264461. [Google Scholar] [CrossRef]
- Tondo, L.; Baldessarini, R.J. Psychotropic Medicines: Increased Appetite Rather than Weight Gain. Lancet Psychiatry 2022, 9, e8. [Google Scholar] [CrossRef]
- Panizzutti, B.; Bortolasci, C.C.; Spolding, B.; Kidnapillai, S.; Connor, T.; Richardson, M.F.; Truong, T.T.T.; Liu, Z.S.J.; Gray, L.; Kim, J.H.; et al. Biological Mechanism(s) Underpinning the Association between Antipsychotic Drugs and Weight Gain. J. Clin. Med. 2021, 10, 4095. [Google Scholar] [CrossRef]
- van Wijnen, L.G.C.; Boluijt, P.R.; Hoeven-Mulder, H.B.; Bemelmans, W.J.E.; Wendel-Vos, G.C.W. Weight Status, Psychological Health, Suicidal Thoughts, and Suicide Attempts in Dutch Adolescents: Results From the 2003 E-MOVO Project. Obesity 2010, 18, 1059–1061. [Google Scholar] [CrossRef] [PubMed]
- Goodman, E.; Whitaker, R.C. A Prospective Study of the Role of Depression in the Development and Persistence of Adolescent Obesity. Pediatrics 2002, 110, 497–504. [Google Scholar] [CrossRef]
- Liem, E.T.; Sauer, P.J.J.; Oldehinkel, A.J.; Stolk, R.P. Association Between Depressive Symptoms in Childhood and Adolescence and Overweight in Later Life: Review of the Recent Literature. Arch. Pediatr. Adolesc. Med. 2008, 162, 981. [Google Scholar] [CrossRef] [PubMed]
- Girela-Serrano, B.M.; Guerrero-Jiménez, M.; Spiers, A.D.V.; Gutiérrez-Rojas, L. Obesity and Overweight among Children and Adolescents with Bipolar Disorder from the General Population: A Review of the Scientific Literature and a Meta-analysis. Early Interv. Psychiatry 2022, 16, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Moreira-Maia, C.R.; St. Fleur, D.; Morcillo-Peñalver, C.; Rohde, L.A.; Faraone, S.V. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. AJP 2016, 173, 34–43. [Google Scholar] [CrossRef]
- Sutaria, S.; Devakumar, D.; Yasuda, S.S.; Das, S.; Saxena, S. Is Obesity Associated with Depression in Children? Systematic Review and Meta-Analysis. Arch. Dis. Child 2019, 104, 64–74. [Google Scholar] [CrossRef]
- Burke, N.L.; Storch, E.A. A Meta-Analysis of Weight Status and Anxiety in Children and Adolescents. J. Dev. Behav. Pediatr. 2015, 36, 133–145. [Google Scholar] [CrossRef]
- Moradi, M.; Mozaffari, H.; Askari, M.; Azadbakht, L. Association between Overweight/Obesity with Depression, Anxiety, Low Self-Esteem, and Body Dissatisfaction in Children and Adolescents: A Systematic Review and Meta-Analysis of Observational Studies. Crit. Rev. Food Sci. Nutr. 2022, 62, 555–570. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Montero, I.; Leon, O.G. A Guide for Naming Research Studies in Psychology. Int. J. Clin. Health Psychol. 2007, 7, 847–862. [Google Scholar]
- Goodburn, E.; Ross, D.; World Helath Organization. A Picture of Health?: A Review and Annotated Bibliography of the Health of Young People in Developing Countries. Available online: https://apps.who.int/iris/handle/10665/62500 (accessed on 25 January 2023).
- Lang, I.A.; Kipping, R.R.; Jago, R.; Lawlor, D.A. Variation in Childhood and Adolescent Obesity Prevalence Defined by International and Country-Specific Criteria in England and the United States. Eur. J. Clin. Nutr. 2011, 65, 143–150. [Google Scholar] [CrossRef]
- Dumith, S.C.; Farias Júnior, J.C. Sobrepeso e Obesidade Em Crianças e Adolescentes: Comparação de Três Critérios de Classificação Baseados No Índice de Massa Corporal. Rev. Panam. Salud Publica 2010, 28, 30–35. [Google Scholar] [CrossRef] [PubMed]
- McCuen-Wurst, C.; Ruggieri, M.; Allison, K.C. Disordered Eating and Obesity: Associations between Binge-Eating Disorder, Night-Eating Syndrome, and Weight-Related Comorbidities: Disordered Eating and Obesity. Ann. N.Y. Acad. Sci. 2018, 1411, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a Critical Appraisal Tool to Assess the Quality of Cross-Sectional Studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef] [PubMed]
- Jüni, P. The Hazards of Scoring the Quality of Clinical Trials for Meta-Analysis. JAMA 1999, 282, 1054. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H. Gender and Ethnic Differences in the Association Between Obesity and Depression Among Black Adolescents. J. Racial Ethn. Health Disparities 2015, 2, 481–493. [Google Scholar] [CrossRef]
- Chen, G.; Guo, G.; Gong, J.; Xiao, S. The Association Between Body Dissatisfaction and Depression: An Examination of the Moderating Effects of Gender, Age, and Weight Status in a Sample of Chinese Adolescents. J. Psychol. Couns. Sch. 2015, 25, 245–260. [Google Scholar] [CrossRef]
- Hoare, E.; Millar, L.; Fuller-Tyszkiewicz, M.; Skouteris, H.; Nichols, M.; Jacka, F.; Swinburn, B.; Chikwendu, C.; Allender, S. Associations between Obesogenic Risk and Depressive Symptomatology in Australian Adolescents: A Cross-Sectional Study. J. Epidemiol. Community Health 2014, 68, 767–772. [Google Scholar] [CrossRef]
- Lindberg, L.; Hagman, E.; Danielsson, P.; Marcus, C.; Persson, M. Anxiety and Depression in Children and Adolescents with Obesity: A Nationwide Study in Sweden. BMC Med. 2020, 18, 30. [Google Scholar] [CrossRef]
- Rottenberg, J.; Yaroslavsky, I.; Carney, R.M.; Freedland, K.E.; George, C.J.; Baji, I.; Dochnal, R.; Gádoros, J.; Halas, K.; Kapornai, K.; et al. The Association Between Major Depressive Disorder in Childhood and Risk Factors for Cardiovascular Disease in Adolescence. Psychosom. Med. 2014, 76, 122–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ting, W.-H.; Huang, C.-Y.; Tu, Y.-K.; Chien, K.-L. Association between Weight Status and Depressive Symptoms in Adolescents: Role of Weight Perception, Weight Concern, and Dietary Restraint. Eur. J. Pediatr. 2012, 171, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- Moharei, F.; Norooziasl, S.; Behdani, F.; Ghaemi, N. Evaluating of Psychiatric Behavior in Obese Children and Adolescents. Iran J. Child Neurol. 2018, 12, 26–36. [Google Scholar]
- Jensen, K.G.; Correll, C.U.; Rudå, D.; Klauber, D.G.; Stentebjerg-Olesen, M.; Fagerlund, B.; Jepsen, J.R.M.; Fink-Jensen, A.; Pagsberg, A.K. Pretreatment Cardiometabolic Status in Youth With Early-Onset Psychosis: Baseline Results From the TEA Trial. J. Clin. Psychiatry 2017, 78, e1035–e1046. [Google Scholar] [CrossRef]
- Shapiro, J.; Mindra, S.; Timmins, V.; Swampillai, B.; Scavone, A.; Collinger, K.; Collins, J.; Goldstein, B.I. Controlled Study of Obesity Among Adolescents with Bipolar Disorder. J. Child Adolesc. Psychopharmacol. 2017, 27, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.S.; Espil, F.M.; Viana, A.G.; Janicke, D.M. Associations Between Anxiety Symptoms and Child and Family Factors in Pediatric Obesity. J. Dev. Behav. Pediatr. 2015, 36, 664–672. [Google Scholar] [CrossRef]
- Roberts, R.E.; Duong, H.T. Do Anxiety Disorders Play a Role in Adolescent Obesity? Ann. Behav. Med. 2016, 50, 613–621. [Google Scholar] [CrossRef]
- Lankinen, V.; Fröjd, S.; Marttunen, M.; Kaltiala-Heino, R. Perceived Rather than Actual Overweight Is Associated with Mental Health Problems in Adolescence. Nord. J. Psychiatry 2018, 72, 89–96. [Google Scholar] [CrossRef]
- Thompson, J.E.; Allyson Phillips, B.; McCracken, A.; Thomas, K.; Ward, W.L. Social Anxiety in Obese Youth in Treatment Setting. Child Adolesc. Soc. Work J. 2013, 30, 37–47. [Google Scholar] [CrossRef]
- Rojo, M.; Solano, S.; Lacruz, T.; Baile, J.I.; Blanco, M.; Graell, M.; Sepúlveda, A.R. Linking Psychosocial Stress Events, Psychological Disorders and Childhood Obesity. Children 2021, 8, 211. [Google Scholar] [CrossRef]
- Vasileiou, K.; Barnett, J.; Thorpe, S.; Young, T. Characterising and Justifying Sample Size Sufficiency in Interview-Based Studies: Systematic Analysis of Qualitative Health Research over a 15-Year Period. BMC Med. Res. Methodol. 2018, 18, 148. [Google Scholar] [CrossRef] [PubMed]
- Eaton, W.W.; Neufeld, K.; Chen, L.-S.; Cai, G. A Comparison of Self-Report and Clinical Diagnostic Interviews for Depression: Diagnostic Interview Schedule and Schedules for Clinical Assessment in Neuropsychiatry in the Baltimore Epidemiologic Catchment Area Follow-Up. Arch. Gen. Psychiatry 2000, 57, 217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kansra, A.R.; Lakkunarajah, S.; Jay, M.S. Childhood and Adolescent Obesity: A Review. Front. Pediatr. 2021, 8, 581461. [Google Scholar] [CrossRef]
- Brown, C.L.; Halvorson, E.E.; Cohen, G.M.; Lazorick, S.; Skelton, J.A. Addressing Childhood Obesity. Pediatr. Clin. N. Am. 2015, 62, 1241–1261. [Google Scholar] [CrossRef] [PubMed]
- Caqueo-Urízar, A.; Flores, J.; Escobar, C.; Urzúa, A.; Irarrázaval, M. Psychiatric Disorders in Children and Adolescents in a Middle-Income Latin American Country. BMC Psychiatry 2020, 20, 104. [Google Scholar] [CrossRef]
- Berg, N.; Nummi, T.; Bean, C.G.; Westerlund, H.; Virtanen, P.; Hammarström, A. Risk Factors in Adolescence as Predictors of Trajectories of Somatic Symptoms over 27 Years. Eur. J. Public Health 2022, 32, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Kokka, I.; Mourikis, I.; Michou, M.; Vlachakis, D.; Darviri, C.; Zervas, I.; Kanaka-Gantenbein, C.; Bacopoulou, F. Validation of the Greek Version of Social Media Disorder Scale. In GeNeDis 2020; Vlamos, P., Ed.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2021; Volume 1338, pp. 107–116. ISBN 978-3-030-78774-5. [Google Scholar]
- Moitra, P.; Madan, J.; Shaikh, N.I. Eating Habits and Sleep Patterns of Adolescents with Depression Symptoms in Mumbai, India. Matern. Child Nutr. 2020, 16. [Google Scholar] [CrossRef]
- Fulton, S.; Décarie-Spain, L.; Fioramonti, X.; Guiard, B.; Nakajima, S. The Menace of Obesity to Depression and Anxiety Prevalence. Trends Endocrinol. Metab. 2022, 33, 18–35. [Google Scholar] [CrossRef]
- Gafoor, R.; Booth, H.P.; Gulliford, M.C. Antidepressant Utilisation and Incidence of Weight Gain during 10 Years’ Follow-up: Population Based Cohort Study. BMJ 2018, k1951. [Google Scholar] [CrossRef]
- Reekie, J.; Hosking, S.P.M.; Prakash, C.; Kao, K.-T.; Juonala, M.; Sabin, M.A. The Effect of Antidepressants and Antipsychotics on Weight Gain in Children and Adolescents: Antidepressants/Psychotics and Weight in Youth. Obes. Rev. 2015, 16, 566–580. [Google Scholar] [CrossRef]
- Emslie, G.J.; Ventura, D.; Korotzer, A.; Tourkodimitris, S. Escitalopram in the Treatment of Adolescent Depression: A Randomized Placebo-Controlled Multisite Trial. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 721–729. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, B.S.; Glass, T.A.; Pollak, J.; Hirsch, A.G.; Bailey-Davis, L.; Moran, T.H.; Bandeen-Roche, K. Depression, Its Comorbidities and Treatment, and Childhood Body Mass Index Trajectories: Depression, Antidepressants, and Childhood BMI Trajectory. Obesity 2016, 24, 2585–2592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Psarraki, E.E.; Kokka, I.; Bacopoulou, F.; Chrousos, G.P.; Artemiadis, A.; Darviri, C. Is There a Relation between Major Depression and Hair Cortisol? A Systematic Review and Meta-Analysis. Psychoneuroendocrinology 2021, 124, 105098. [Google Scholar] [CrossRef] [PubMed]
- Ferraù, F.; Korbonits, M. Metabolic Syndrome in Cushing’s Syndrome Patients. In Frontiers of Hormone Research; Popovic, V., Korbonits, M., Eds.; S. Karger AG: Basel, Switzerland, 2018; Volume 49, pp. 85–103. ISBN 978-3-318-06334-9. [Google Scholar]
- Cho, S.J.; Lee, H.J.; Rhee, S.J.; Kim, E.Y.; Kim, K.-N.; Yoon, D.H.; Ahn, Y.M. The Relationship between Visceral Adiposity and Depressive Symptoms in the General Korean Population. J. Affect. Disord. 2019, 244, 54–59. [Google Scholar] [CrossRef]
- Klok, M.D.; Jakobsdottir, S.; Drent, M.L. The Role of Leptin and Ghrelin in the Regulation of Food Intake and Body Weight in Humans: A Review. Obes. Rev. 2007, 8, 21–34. [Google Scholar] [CrossRef]
- Ge, T.; Fan, J.; Yang, W.; Cui, R.; Li, B. Leptin in Depression: A Potential Therapeutic Target. Cell Death Dis. 2018, 9, 1096. [Google Scholar] [CrossRef]
- Gogtay, N.; Vyas, N.S.; Testa, R.; Wood, S.J.; Pantelis, C. Age of Onset of Schizophrenia: Perspectives From Structural Neuroimaging Studies. Schizophr. Bull. 2011, 37, 504–513. [Google Scholar] [CrossRef]
- Cohn, T.A.; Remington, G.; Zipursky, R.B.; Azad, A.; Connolly, P.; Wolever, T.M. Insulin Resistance and Adiponectin Levels in Drug-Free Patients with Schizophrenia: A Preliminary Report. Can. J. Psychiatry 2006, 51, 382–386. [Google Scholar] [CrossRef]
- Phutane, V.H.; Tek, C.; Chwastiak, L.; Ratliff, J.C.; Ozyuksel, B.; Woods, S.W.; Srihari, V.H. Cardiovascular Risk in a First-Episode Psychosis Sample: A ‘Critical Period’ for Prevention? Schizophr. Res. 2011, 127, 257–261. [Google Scholar] [CrossRef]
- Dasgupta, A.; Singh, O.P.; Rout, J.K.; Saha, T.; Mandal, S. Insulin Resistance and Metabolic Profile in Antipsychotic Naïve Schizophrenia Patients. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2010, 34, 1202–1207. [Google Scholar] [CrossRef]
- Bioque, M.; García-Portilla, M.A.P.; García-Rizo, C.; Cabrera, B.; Lobo, A.; González-Pinto, A.; Díaz-Caneja, C.M.; Corripio, I.; Vieta, E.; Castro-Fornieles, J.; et al. Evolution of Metabolic Risk Factors over a Two-Year Period in a Cohort of First Episodes of Psychosis. Schizophr. Res. 2018, 193, 188–196. [Google Scholar] [CrossRef]
- del Campo, A.; Bustos, C.; Mascayano, C.; Acuña-Castillo, C.; Troncoso, R.; Rojo, L.E. Metabolic Syndrome and Antipsychotics: The Role of Mitochondrial Fission/Fusion Imbalance. Front. Endocrinol. 2018, 9, 144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baeza, I.; Vigo, L.; de la Serna, E.; Calvo-Escalona, R.; Merchán-Naranjo, J.; Rodríguez-Latorre, P.; Arango, C.; Castro-Fornieles, J. The Effects of Antipsychotics on Weight Gain, Weight-Related Hormones and Homocysteine in Children and Adolescents: A 1-Year Follow-up Study. Eur. Child Adolesc. Psychiatry 2017, 26, 35–46. [Google Scholar] [CrossRef] [PubMed]
- De Hert, M.; Dobbelaere, M.; Sheridan, E.M.; Cohen, D.; Correll, C.U. Metabolic and Endocrine Adverse Effects of Second-Generation Antipsychotics in Children and Adolescents: A Systematic Review of Randomized, Placebo Controlled Trials and Guidelines for Clinical Practice. Eur. Psychiatr. 2011, 26, 144–158. [Google Scholar] [CrossRef] [PubMed]
- Biederman, J.; Mick, E.; Hammerness, P.; Harpold, T.; Aleardi, M.; Dougherty, M.; Wozniak, J. Open-Label, 8-Week Trial of Olanzapine and Risperidone for the Treatment of Bipolar Disorder in Preschool-Age Children. Biol. Psychiatry 2005, 58, 589–594. [Google Scholar] [CrossRef]
- Correll, C.U. Assessing and Maximizing the Safety and Tolerability of Antipsychotics Used in the Treatment of Children and Adolescents. J. Clin. Psychiatry 2008, 69 (Suppl. S4), 26–36. [Google Scholar]
- Correll, C.U. Cardiometabolic Risk of Second-Generation Antipsychotic Medications During First-Time Use in Children and Adolescents. JAMA 2009, 302, 1765. [Google Scholar] [CrossRef]
- Efe, Y.S.; Özbey, H.; Erdem, E.; Hatipoğlu, N. A Comparison of Emotional Eating, Social Anxiety and Parental Attitude among Adolescents with Obesity and Healthy: A Case-Control Study. Arch. Psychiatr. Nurs. 2020, 34, 557–562. [Google Scholar] [CrossRef]
- Boutelle, K.N.; Zucker, N.; Peterson, C.B.; Rydell, S.; Carlson, J.; Harnack, L.J. An Intervention Based on Schachter’s Externality Theory for Overweight Children: The Regulation of Cues Pilot. J. Pediatr. Psychol. 2014, 39, 405–417. [Google Scholar] [CrossRef]
- Rofey, D.L.; Kolko, R.P.; Iosif, A.-M.; Silk, J.S.; Bost, J.E.; Feng, W.; Szigethy, E.M.; Noll, R.B.; Ryan, N.D.; Dahl, R.E. A Longitudinal Study of Childhood Depression and Anxiety in Relation to Weight Gain. Child Psychiatry Hum. Dev. 2009, 40, 517–526. [Google Scholar] [CrossRef]
- Hewagalamulage, S.D.; Lee, T.K.; Clarke, I.J.; Henry, B.A. Stress, Cortisol, and Obesity: A Role for Cortisol Responsiveness in Identifying Individuals Prone to Obesity. Domest. Anim. Endocrinol. 2016, 56, S112–S120. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J. Obesity in Childhood and Adolescence: Evidence Based Clinical and Public Health Perspectives. Postgrad. Med. J. 2006, 82, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Boyko, E.J. Observational Research—Opportunities and Limitations. J. Diabetes Complicat. 2013, 27, 642–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeong, H.; Yim, H.W.; Lee, S.-Y.; Lee, H.K.; Potenza, M.N.; Kwon, J.-H.; Koo, H.J.; Kweon, Y.-S.; Bhang, S.; Choi, J.-S. Discordance between Self-Report and Clinical Diagnosis of Internet Gaming Disorder in Adolescents. Sci. Rep. 2018, 8, 10084. [Google Scholar] [CrossRef]
- Solmi, M.; Radua, J.; Olivola, M.; Croce, E.; Soardo, L.; Salazar de Pablo, G.; Il Shin, J.; Kirkbride, J.B.; Jones, P.; Kim, J.H.; et al. Age at Onset of Mental Disorders Worldwide: Large-Scale Meta-Analysis of 192 Epidemiological Studies. Mol. Psychiatry 2022, 27, 281–295. [Google Scholar] [CrossRef]
- McInnes, M.D.F.; Moher, D.; Thombs, B.D.; McGrath, T.A.; Bossuyt, P.M. The PRISMA-DTA Group (2018). Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. JAMA 2018, 319, 388–396. [Google Scholar] [CrossRef]


| First Author [Reference] | Publication Year | Sample Characteristics [Number of Participants (Mean Age ± SD or Age Range in Years) % Females] | Primary Diagnosis | Diagnosis Establishement | Main Results |
|---|---|---|---|---|---|
| Assari and Caldwell [51] | 2015 | 1170 (13–17) 52% | Depression | CIDI | Non-significant associations between obesity and MDD, significant interaction between ethnicity and obesity in MDD. |
| Chen [52] | 2015 | 1101 (12–18) 45.8% | Depression | CES-D | Depression was positively but weakly associated with obesity in younger adolescents (12–15 years), but not in older adolescents (15–18 years). |
| Hoare [53] | 2014 | 800 (13.1 ± 0.62) 55% | Depression | SMFQ | Obesity contributed significantly to depressive symptomatology, and some of these patterns differed across gender. Adolescents with greater sedentary behaviors reported greater symptomatic depression, before and after adjusting for covariates. |
| Lindberg [54] | 2020 | 12507 (6–18) 46.9% | Depression, anxiety | ICD-10 | Obesity was a significant risk factor for anxiety and depression in children and adolescents. Obese girls had 43% higher risk for anxiety and depression (p < 0.0001). The risk in obese boys was similar (p < 0.0001). |
| Rottenberg [55] | 2014 | 566 (7–14) NA | Depression | SCA-D | Individuals with a diagnosis of depression had higher rate of obesity than controls (OR 3.67, CI = 1.42–9.52). |
| Ting [56] | 2012 | 869 (15.7) 47% | Depression | CES-D | Depressive symptomatology significantly correlated with obesity (p = 0.02) and the association was mediated by perceived weight status, increased weight concern, and food uptake restraint. |
| Moharei [57] | 2018 | 160 (5–17) 47.5% | Anxiety, depression | STAIC, CDI | Non-significant differences in scores of anxiety and depression between obese and non-obese individuals. |
| Jensen [58] | 2017 | 113 (15.74 ± 1.36) 69.9% | Schizophrenia | ICD-10 | BMI did not differ between patients on first psychotic episode without antipsychotic treatment and controls (matched for sex, age, and parental education level). |
| Shapiro [59] | 2016 | 118 (16.0 ± 1.5) 62% | Bipolar disorder | KSADS-PL | Adolescents with bipolar disorder reported significantly higher obesity (18%) than controls (p = 0.02). Among those with psychiatric diagnosis, obesity was significantly associated with suicide attempt and self-injurious behavioral patterns. Antidepressants were associated with obesity, but only when medication did not involve selective serotonin reuptake inhibitors. |
| Lim [60] | 2015 | 199 (7–12) NA | Anxiety | CBCL | Children in the Obesity + Clinical Anxiety group reported more body dissatisfaction (p = 0.023) and lower total HRQOL (p = 0.005) than the control group. |
| Roberts [61] | 2016 | 3134 (11–17) 48.8% | Anxiety | DSM-IV | Significant association of anxiety with obesity. Any anxiety disorder was associated with a 46% increased possibility to be obese. |
| Lankinen [62] | 2017 | 2275 (15.6 ± 0.4) 48.9% | Depression, conduct disorder, social anxiety | BDI, SPIN, YSR | Perceived weight status was correlated with higher risk of self-reported depression in girls (p < 0.001) and boys (p = 0.001). Significant association was also found for social phobia (p = 0.05) in boys. |
| Thompson [63] | 2012 | 230 (<17) 44.5% | Social anxiety | SAS | Social anxiety was significantly and positively correlated with BMI. Extremely obese participants scored significantly higher in the social anxiety scale than obese. |
| Rojo [64] | 2021 | 200 (10.34 ± 1.31) 60% | Psychological stress events, psychiatric diagnoses | DSM-5 clinical interviews | Obese children presented a psychiatric disorder more often than overweight or normal-weight children. A predictive model revealed that a psychiatric diagnosis increased the risk of weight gain by 26. |
| Study Reference | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AXIS Item | 51 | 52 | 53 | 54 | 55 | 56 | 57 | 58 | 59 | 60 | 61 | 62 | 63 | 64 |
| Clearly stated objective | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Appropriate study design | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Justified sample size | N | N | N | N | N | N | N | N | N | N | N | N | N | N |
| Clearly defined population | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Clearly represented population | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Clear selection process of population | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Address and categorize non-responders | N | N | N | N | N | N | N | N | N | N | N | N | N | N |
| Appropriate variable measurement | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Use of established measurements | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Reported statisticalsignificance | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Methods sufficiently described | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Data description | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Concerns about non-response bias? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Information about non-responders | N | N | N | N | N | N | N | N | N | N | N | N | N | N |
| Internal consistency of results | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Adequate result presentation | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Justified results by discussion | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Report on limitations | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Pediatric Labeling Aproval Date | Pharmaceutical Substance | Indication | Therapeutic Category | Weight Gain Risk |
|---|---|---|---|---|
| 28/1/2022 | ziprasidone | BD-I (10 to 17 years) | SGA | Low |
| 27/12/2021 | brexpiprazole | Schizophrenia (13 to 17 years) | SGA | Low |
| 5/3/2018 | lurasidone | Treatment of MDE associated with BD-I | SGA | Low |
| 27/1/2017 | lurasidone | Treatment of schizophrenia in adolescents and irritability associated with autistic disorder in pediatric patients | SGA | Low |
| 12/3/2015 | asenapine | Schizophrenia and Acute Manic or Mixed Episodes Associated with BD-I | SGA | Moderate |
| 31/10/2014 | escitalopram | MDD | SSRI | Moderate |
| 16/10/2014 | duloxetine | GAD | SNRI | Low |
| 26/7/2013 | olanzapine/fluoxetine | Depressive episodes associated with BD-I | SGA/ SSRI | High |
| 30/4/2013 | quetiapine | Bipolar depression | SGA | Moderate |
| 18/10/2012 | duloxetine | MDD | SNRI | Moderate |
| 2/12/2009 | quetiapine | Schizophrenia (13 to 17 years) and bipolar mania (10 to 17 years) | SGA | Moderate |
| 19/3/2009 | escitalopram | MDD in adolescents | SSRI | Moderate |
| 14/8/2008 | olanzapine | schizophrenia; BD | SGA | High |
| 27/2/2008 | aripiprazole | BD-I | SGA | Moderate |
| 29/10/2007 | aripiprazole | Schizophrenia | SGA | Moderate |
| 22/8/2007 | risperidone | Schizophrenia;short-term treatment of acute manic or mixed Episodes associated with BD-I | SGA | High |
| 18/2/2005 | citalopram | MDD | SSRI | Moderate |
| 18/2/2005 | sertraline | MDD & OCD | SSRI | Low |
| 12/1/2005 | paroxetine | MDD | SSRI | Low |
| 12/1/2005 | mirtazapine | MDD | NaSSA | High |
| 12/1/2005 | nefazodone | MDD | SARI | Low |
| 5/5/2004 | venlafaxine | MDD | SNRI | Low |
| 3/1/2003 | fluoxetine | MDD & OCD | SSRI | Low |
| 19/7/2001 | buspirone | GAD | Anti-Anxiety Agents/Anxiolytics | Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kokka, I.; Mourikis, I.; Bacopoulou, F. Psychiatric Disorders and Obesity in Childhood and Adolescence—A Systematic Review of Cross-Sectional Studies. Children 2023, 10, 285. https://doi.org/10.3390/children10020285
Kokka I, Mourikis I, Bacopoulou F. Psychiatric Disorders and Obesity in Childhood and Adolescence—A Systematic Review of Cross-Sectional Studies. Children. 2023; 10(2):285. https://doi.org/10.3390/children10020285
Chicago/Turabian StyleKokka, Ioulia, Iraklis Mourikis, and Flora Bacopoulou. 2023. "Psychiatric Disorders and Obesity in Childhood and Adolescence—A Systematic Review of Cross-Sectional Studies" Children 10, no. 2: 285. https://doi.org/10.3390/children10020285