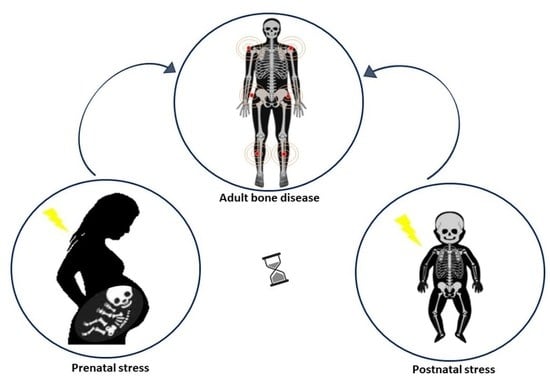
Early Life Stress (ELS) Effects on Fetal and Adult Bone Development
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. ELS Impact on Bone Development
3.1.1. Prenatal Stress Models
- Mouse
- Rat
- Rabbit
- Pig
3.1.2. Postnatal Stress Model
- Mouse
3.1.3. Perinatal Stress Model
- Rat
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, K.E.; Pollak, S.D. Early life stress and development: Potential mechanisms for adverse outcomes. J. Neurodev. Disord. 2020, 12, 34. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J.P. The origins of the developmental origins theory. J. Intern. Med. 2007, 261, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Talge, N.M.; Neal, C.; Glover, V. Early Stress, Translational Research and Prevention Science Network: Fetal and Neonatal Experience on Child and Adolescent Mental Health. Antenatal maternal stress and long-term effects on child neurodevelopment: How and why? J. Child Psychol. Psychiatry 2007, 48, 245–261. [Google Scholar] [CrossRef]
- Simeoni, U.; Armengaud, J.-B.; Siddeek, B.; Tolsa, J.-F. Perinatal Origins of Adult Disease. Neonatology 2018, 113, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, K.M.; Lillycrop, K.A.; Burdge, G.C.; Gluckman, P.D.; Hanson, M.A. Epigenetic Mechanisms and the Mismatch Concept of the Developmental Origins of Health and Disease. Pediatr. Res. 2007, 61, 5R–10R. [Google Scholar] [CrossRef]
- Goldberg, A.D.; Allis, C.D.; Bernstein, E. Epigenetics: A Landscape Takes Shape. Cell 2007, 128, 635–638. [Google Scholar] [CrossRef] [Green Version]
- Hales, C.N.; Barker, D.J. The thrifty phenotype hypothesis. Br. Med. Bull. 2001, 60, 5–20. [Google Scholar] [CrossRef] [Green Version]
- Heijmans, B.T.; Tobi, E.W.; Stein, A.D.; Putter, H.; Blauw, G.J.; Susser, E.S.; Slagboom, P.E.; Lumey, L.H. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc. Natl. Acad. Sci. USA 2008, 105, 17046–17049. [Google Scholar] [CrossRef] [Green Version]
- Murphy, M.O.; Cohn, D.M.; Loria, A.S. Developmental origins of cardiovascular disease: Impact of early life stress in humans and rodents. Neurosci. Biobehav. Rev. 2017, 74, 453–465. [Google Scholar] [CrossRef] [Green Version]
- Tyrka, A.R.; Price, L.H.; Kao, H.-T.; Porton, B.; Marsella, S.A.; Carpenter, L.L. Childhood Maltreatment and Telomere Shortening: Preliminary Support for an Effect of Early Stress on Cellular Aging. Biol. Psychiatry 2010, 67, 531–534. [Google Scholar] [CrossRef]
- Raabe, F.J.; Spengler, D. Epigenetic Risk Factors in PTSD and Depression. Front. Psychiatry 2013, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egger, G.; Liang, G.; Aparicio, A.; Jones, P.A. Epigenetics in human disease and prospects for epigenetic therapy. Nature 2004, 429, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Marini, F.; Cianferotti, L.; Brandi, M.L. Epigenetic Mechanisms in Bone Biology and Osteoporosis: Can They Drive Therapeutic Choices? Int. J. Mol. Sci. 2016, 17, 1329. [Google Scholar] [CrossRef] [Green Version]
- Coussons-Read, M.E. Effects of prenatal stress on pregnancy and human development: Mechanisms and pathways. Obstet. Med. 2013, 6, 52–57. [Google Scholar] [CrossRef] [Green Version]
- Alhusen, J.L.; Ray, E.; Sharps, P.; Bullock, L. Intimate Partner Violence During Pregnancy: Maternal and Neonatal Outcomes. J. Women’s Health 2015, 24, 100–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, J.-S.; Chin, K.-Y. Potential mechanisms linking psychological stress to bone health. Int. J. Med. Sci. 2021, 18, 604–614. [Google Scholar] [CrossRef] [PubMed]
- Lobato, G.; Reichenheim, M.E.; Moraes, C.L.; Peixoto-Filho, F.M.; Migowski, L.S. Psychologic intimate partner violence and the risk of intrauterine growth restriction in Rio de Janeiro. Int. J. Gynecol. Obstet. 2018, 143, 77–83. [Google Scholar] [CrossRef]
- Furlan, P.M.; Have, T.T.; Cary, M.; Zemel, B.; Wehrli, F.; Katz, I.R.; Gettes, D.R.; Evans, D.L. The role of stress-induced cortisol in the relationship between depression and decreased bone mineral density. Biol. Psychiatry 2005, 57, 911–917. [Google Scholar] [CrossRef]
- Cooper, C.; Harvey, N.; Cole, Z.; Hanson, M.; Dennison, E. Developmental Origins of Osteoporosis: The Role of Maternal Nutrition. Adv. Exp. Med. Biol. 2009, 646, 31–39. [Google Scholar] [CrossRef]
- Azuma, K.; Adachi, Y.; Hayashi, H.; Kubo, K.-Y. Chronic Psychological Stress as a Risk Factor of Osteoporosis. J. UOEH 2015, 37, 245–253. [Google Scholar] [CrossRef]
- Mezuk, B.; Eaton, W.W.; Golden, S.H. Depression and osteoporosis: Epidemiology and potential mediating pathways. Osteoporos. Int. 2008, 19, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palusci, V.J.; Botash, A.S. Race and Bias in Child Maltreatment Diagnosis and Reporting. Pediatrics 2021, 148, e2020049625. [Google Scholar] [CrossRef] [PubMed]
- Nigri, P.; Corsello, G.; Nigri, L.; Bali, D.; Kuli-Lito, G.; Plesca, D.; Pop, T.L.; Carrasco-Sanz, A.; Namazova-Baranova, L.; Mestrovic, J.; et al. Prevention and contrast of child abuse and neglect in the practice of European paediatricians: A multi-national pilot study. Ital. J. Pediatr. 2021, 47, 105. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.M.P.; Rogers, N.T.; Power, C. Adult retrospective report of child abuse and prospective indicators of childhood harm: A population birth cohort study. BMC Med. 2021, 19, 286. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.E.; Byun, S.K.; Shin, S.; Jang, J.Y.; Choi, B.-I.; Park, D.; Jeon, J.H.; Nahm, S.-S.; Kang, J.-K.; Hwang, S.-Y.; et al. Effect of Maternal Restraint Stress on Fetal Development of ICR Mice. Exp. Anim. 2008, 57, 19–25. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Yun, H.J.; Lee, J.-Y.; Kim, M.H. Prenatal Stress Induces Skeletal Malformations in Mouse Embryos. Biomed. Sci. Lett. 2015, 21, 15–22. [Google Scholar] [CrossRef] [Green Version]
- Choe, H.K.; Son, G.H.; Chung, S.; Kim, M.; Sun, W.; Kim, H.; Geum, D. Maternal stress retards fetal development in mice with transcriptome-wide impact on gene expression profiles of the limb. Stress 2011, 14, 194–204. [Google Scholar] [CrossRef]
- Azuma, K.; Ogura, M.; Kondo, H.; Suzuki, A.; Hayashi, S.; Iinuma, M.; Onozuka, M.; Kubo, K.-Y. Maternal Active Mastication during Prenatal Stress Ameliorates Prenatal Stress-Induced Lower Bone Mass in Adult Mouse Offspring. Int. J. Med. Sci. 2017, 14, 348–355. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez, P.N.; Lotto, F.P.; Hallgrímsson, B. Canalization and developmental instability of the fetal skull in a mouse model of maternal nutritional stress. Am. J. Phys. Anthr. 2014, 154, 544–553. [Google Scholar] [CrossRef]
- Wuertz-Kozak, K.; Roszkowski, M.; Cambria, E.; Block, A.; Kuhn, G.; Abele, T.; Hitzl, W.; Drießlein, D.; Müller, R.; Rapp, M.; et al. Effects of Early Life Stress on Bone Homeostasis in Mice and Humans. Int. J. Mol. Sci. 2020, 21, 6634. [Google Scholar] [CrossRef] [PubMed]
- Amugongo, S.K.; Hlusko, L.J. Impact of Maternal Prenatal Stress on Growth of the Offspring. Aging Dis. 2014, 5, 1–16. [Google Scholar] [CrossRef]
- Swolin-Eide, D.; Dahlgren, J.; Nilsson, C.; Wikland, K.A.; Holmang, A.; Ohlsson, C. Affected skeletal growth but normal bone mineralization in rat offspring after prenatal dexamethasone exposure. J. Endocrinol. 2002, 174, 411–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anevska, K.; Gallo, L.A.; Tran, M.; Jefferies, A.J.; Wark, J.D.; Wlodek, M.E.; Romano, T. Pregnant growth restricted female rats have bone gains during late gestation which contributes to second generation adolescent and adult offspring having normal bone health. Bone 2015, 74, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Anevska, K.; Cheong, J.N.; Wark, J.D.; Wlodek, M.E.; Romano, T. Maternal stress does not exacerbate long-term bone deficits in female rats born growth restricted, with differential effects on offspring bone health. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 314, R161–R170. [Google Scholar] [CrossRef]
- Dancause, K.N.; Cao, X.J.; Veru, F.; Xu, S.; Long, H.; Yu, C.; Laplante, D.P.; Walker, C.D.; King, S. Brief communication: Prenatal and early postnatal stress exposure influences long bone length in adult rat offspring. Am. J. Phys. Anthr. 2012, 149, 307–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breno, M.; Bots, J.; De Schaepdrijver, L.; Van Dongen, S. Fluctuating Asymmetry as Risk Marker for Stress and Structural Defects in a Toxicologic Experiment. Birth Defects Res. B Dev. Reprod. Toxicol. 2013, 98, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Bots, J.; Breno, M.; De Schaepdrijver, L.; Van Dongen, S. Maternal Stress Affects Fetal Growth but Not Developmental Instability in Rabbits. Symmetry 2016, 8, 101. [Google Scholar] [CrossRef] [Green Version]
- Śliwa, E.; Tatara, M.R.; Nowakowski, H.; Pierzynowski, S.G.; Studziński, T. Effect of maternal dexamethasone and alpha-ketoglutarate administration on skeletal development during the last three weeks of prenatal life in pigs. J. Matern. Fetal. Neonatal Med. 2006, 19, 489–493. [Google Scholar] [CrossRef]
- Pavone, V.; Lucenti, L. Awareness and Recognition: The Importance of the Orthopaedist in Child Abuse. Int. J. Sch. Cogn. Psychol. 2016, 3. [Google Scholar] [CrossRef]
- Pavone, V.; Vescio, A.; Lucenti, L.; Amico, M.; Caldaci, A.; Pappalardo, X.G.; Parano, E.; Testa, G. Diagnostic Tools in the Detection of Physical Child Abuse: A Systematic Review. Children 2022, 9, 1257. [Google Scholar] [CrossRef] [PubMed]
- Pandya, N.K.; Baldwin, K.; Kamath, A.F.; Wenger, D.R.; Hosalkar, H.S. Unexplained Fractures: Child Abuse or Bone Disease? A Systematic Review. Clin. Orthop. Relat. Res. 2011, 469, 805–812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulici, A.; Herdea, A.; Dragomirescu, M.-C.; Lungu, C.N. Obstetric fractures in caesarean delivery and risk factors as evaluated by paediatric surgeons. Int. Orthop. 2022, 46, 26. [Google Scholar] [CrossRef] [PubMed]
- Cuffe, J.S.M.; Turton, E.L.; Akison, L.K.; Bielefeldt-Ohmann, H.; Moritz, K.M. Prenatal corticosterone exposure programs sex-specific adrenal adaptations in mouse offspring. J. Endocrinol. 2017, 232, 37–48. [Google Scholar] [CrossRef] [Green Version]
- Mackem, S.; Lewandoski, M. Limb Development Takes a Measured Step Toward Systems Analysis. Sci. Signal. 2009, 2, pe33. [Google Scholar] [CrossRef]
- Singer, B.D. A Practical Guide to the Measurement and Analysis of DNA Methylation. Am. J. Respir. Cell Mol. Biol. 2019, 61, 417–428. [Google Scholar] [CrossRef]
- Graham, J. Fluctuating Asymmetry and Developmental Instability, a Guide to Best Practice. Symmetry 2021, 13, 9. [Google Scholar] [CrossRef]
- Lelovas, P.P.; Xanthos, T.T.; Thoma, S.E.; Lyritis, G.P.; Dontas, I.A. The Laboratory Rat as an Animal Model for Osteoporosis Research. Comp. Med. 2008, 58, 424–430. [Google Scholar]
- Sterns, J.D.; Smith, C.B.; Steele, J.R.; Stevenson, K.L.; Gallicano, G.I. Epigenetics and type II diabetes mellitus: Underlying mechanisms of prenatal predisposition. Front. Cell Dev. Biol. 2014, 2, 15. [Google Scholar] [CrossRef] [Green Version]
- Gallo, L.A.; Tran, M.; Master, J.S.; Moritz, K.M.; Wlodek, M.E. Maternal adaptations and inheritance in the transgenerational programming of adult disease. Cell Tissue Res. 2012, 349, 863–880. [Google Scholar] [CrossRef]
- Wlodek, M.E.; Westcott, K.T.; O’Dowd, R.; Serruto, A.; Wassef, L.; Moritz, K.M.; Moseley, J.M. Uteroplacental restriction in the rat impairs fetal growth in association with alterations in placental growth factors including PTHrP. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005, 288, R1620–R1627. [Google Scholar] [CrossRef] [PubMed]
- Romano, T.; Wark, J.D.; Wlodek, M.E. Physiological skeletal gains and losses in rat mothers during pregnancy and lactation are not observed following uteroplacental insufficiency. Reprod. Fertil. Dev. 2014, 26, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Gallo, L.A.; Tran, M.; Moritz, K.M.; Jefferies, A.J.; Wlodek, M.E. Pregnancy in aged rats that were born small: Cardiorenal and metabolic adaptations and second-generation fetal growth. FASEB J. 2012, 26, 4337–4347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheong, J.N.; Cuffe, J.S.M.; Jefferies, A.J.; Moritz, K.M.; Wlodek, M.E. Adrenal, metabolic and cardio-renal dysfunction develops after pregnancy in rats born small or stressed by physiological measurements during pregnancy. J. Physiol. 2016, 594, 6055–6068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lens, L.; Van Dongen, S.; Matthysen, E. Fluctuating Asymmetry as an Early Warning System in the Critically Endangered Taita Thrush. Conserv. Biol. 2002, 16, 479–487. [Google Scholar] [CrossRef] [Green Version]
- Painter, R.C.; Roseboom, T.J.; de Rooij, S.R. Long-term Effects of Prenatal Stress and Glucocorticoid Exposure. Birth Defects Res. C Embryo Today. 2012, 96, 315–324. [Google Scholar] [CrossRef]
- Dimasuay, K.G.; Boeuf, P.; Powell, T.L.; Jansson, T. Placental Responses to Changes in the Maternal Environment Determine Fetal Growth. Front. Physiol. 2016, 7, 12. [Google Scholar] [CrossRef] [Green Version]
- Hartmann, K.; Koenen, M.; Schauer, S.; Wittig-Blaich, S.; Ahmad, M.; Baschant, U.; Tuckermann, J.P. Molecular Actions of Glucocorticoids in Cartilage and Bone During Health, Disease, and Steroid Therapy. Physiol. Rev. 2016, 96, 409–447. [Google Scholar] [CrossRef] [Green Version]
- Ogueh, O.; Wright, E.M.; Jones, J.; Alaghband-Zadeh, J.; Nicolaides, K.H.; Johnson, M.R. Fetal bone metabolism in normal and rhesus isoimmunised pregnancies. BJOG 2001, 108, 986–992. [Google Scholar] [CrossRef]
- Martin, C.S.; Cooper, M.S.; Hardy, R.S. Endogenous Glucocorticoid Metabolism in Bone: Friend or Foe. Front. Endocrinol. 2021, 12, 733611. [Google Scholar] [CrossRef]
- Cai, X.; Yuan, Y.; Liao, Z.; Xing, K.; Zhu, C.; Xu, Y.; Yu, L.; Wang, L.; Wang, S.; Zhu, X.; et al. α-Ketoglutarate prevents skeletal muscle protein degradation and muscle atrophy through PHD3/ADRB2 pathway. FASEB J. 2018, 32, 488–499. [Google Scholar] [CrossRef] [PubMed]
- Shonkoff, J.P.; Boyce, W.T.; McEwen, B.S. Neuroscience, Molecular Biology, and the Childhood Roots of Health Disparities: Building a new framework for health promotion and disease prevention. JAMA 2009, 301, 2252–2259. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.V. Molecular mechanisms of early life stress—Lessons from mouse models. Neurosci. Biobehav. Rev. 2010, 34, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Teresi, J.A.; Burnes, D.; Skowron, E.A.; Dutton, M.A.; Mosqueda, L.; Lachs, M.S.; Pillemer, K. State of the science on prevention of elder abuse and lessons learned from child abuse and domestic violence prevention: Toward a conceptual framework for research. J. Elder Abus. Negl. 2016, 28, 263–300. [Google Scholar] [CrossRef] [Green Version]
- Cowart-Osborne, M.; Jackson, M.; Chege, E.; Baker, E.; Whitaker, D.; Self-Brown, S. Technology-Based Innovations in Child Maltreatment Prevention Programs: Examples from SafeCare®. Soc. Sci. 2014, 3, 427–440. [Google Scholar] [CrossRef] [Green Version]
- Heck, A.L.; Handa, R.J. Sex differences in the hypothalamic–pituitary–adrenal axis’ response to stress: An important role for gonadal hormones. Neuropsychopharmacology 2019, 44, 45–58. [Google Scholar] [CrossRef] [Green Version]
- Abeynayake, N.; Arthur, A.; Gronthos, S. Crosstalk between skeletal and neural tissues is critical for skeletal health. Bone 2021, 142, 115645. [Google Scholar] [CrossRef]
- Oton-Gonzalez, L.; Mazziotta, C.; Iaquinta, M.R.; Mazzoni, E.; Nocini, R.; Trevisiol, L.; D’Agostino, A.; Tognon, M.; Rotondo, J.C.; Martini, F. Genetics and Epigenetics of Bone Remodeling and Metabolic Bone Diseases. Int. J. Mol. Sci. 2022, 23, 1500. [Google Scholar] [CrossRef]
- Husain, A.; Jeffries, M.A. Epigenetics and Bone Remodeling. Curr. Osteoporos. Rep. 2017, 15, 450–458. [Google Scholar] [CrossRef]
- Bocheva, G.; Boyadjieva, N. Epigenetic regulation of fetal bone development and placental transfer of nutrients: Progress for osteoporosis. Interdiscip. Toxicol. 2011, 4, 167–172. [Google Scholar] [CrossRef] [Green Version]
- Simonić, E.; Peternel, S.; Stojnić-Soša, L.; Rončević-Gržeta, I.; Prpić-Massari, L.; Massari, D.; Periša, D.; Čabrijan, L. Negative and positive life experiences in patients with psoriatic arthritis. Rheumatol. Int. 2013, 33, 1587–1593. [Google Scholar] [CrossRef] [PubMed]
- Altalib, A.; Althomali, A.; Alshahrani, A.; Alfrayyan, A.; Aljughaiman, M.S. Osteogenesis Imperfecta and Child Abuse From a Forensic Point of View. Cureus 2021, 13, e12790. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-Y.; Kim, W.-J.; Kim, B.; Nho, J.-H.; Hong, C.-H.; Lee, S.-M.; Yoo, I.-D.; Lee, C.; Jung, K.-J. Differential Diagnosis between Child Abuse and Infantile Cortical Hyperostosis: A Case Report and Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 12269. [Google Scholar] [CrossRef] [PubMed]
- Verbruggen, S.W.; Kainz, B.; Shelmerdine, S.C.; Hajnal, J.V.; Rutherford, M.A.; Arthurs, O.J.; Phillips, A.T.M.; Nowlan, N.C. Stresses and strains on the human fetal skeleton during development. J. R. Soc. Interface 2018, 15, 20170593. [Google Scholar] [CrossRef] [PubMed]

| Ref. | ELS Type | Stress Procedure | Stress Effect on Dams | Anti-Stress Effect on Dams | Skeletal | Gender | Catch-Up Features | Molecular Analysis |
|---|---|---|---|---|---|---|---|---|
| Differences | ||||||||
| ● Mouse | ||||||||
| [26] | Pre (GD1-16) | 12 h of supine immobilization | Low maternal body weights during stress | no | Vertebral and sternal abnormalities, bipartite ossification; GR; embryos or fetus mortality. | no | no | no |
| [27] | Pre (GD7-9) | i.p. Dex (1 mg/kg or 10 mg/kg) | no | no | T13 or L1 vertebral anomalies. | Xiphoid process bigger in female embryos. | no | no |
| [28] | Pre (GD1-8) | 6 h stuck in a restrainer | no | no | Low fetal body weight; altered number of somites, limb bud formation, regression of interdigital webbing. | no | Suppression of Igf1 and Acta1 genes; lower expression of Aldh1a2 and Fgf8. | |
| [29] | Pre (GD12 to delivery) | 45 min/3 times a day stuck in a restrainer | no | Chew a wooden stick | Lower bone mass, decrease in trabecular bone mass in both vertebrae and distal femur of the offspring of non-chewing stressed mothers | no | no | no |
| [30] | Pre (GD1-18) | Caloric restriction | no | no | Reduced skull size | no | no | no |
| [31] | Post (PND1-14) | Maternal separation during the dark cycle for 3 h | no | no | Low birth weight and altered bone innervation. | no | no | Altered neurogenic and osteogenic markers. |
| ● Rat | ||||||||
| [32] | Pre (GD1-21) | 45 min/3 times a day stuck in an immobilization bag | Less food consumption, weight loss | no | no | no | Faster growth and higher weight gain in offspring. | no |
| [33] | Pre (GD9-13) | i.m. Dex (100 micro g/kg) | no | no | no | Transient increases in crown–rump length and tibia and femur lengths at 3–6 weeks of age; altered cortical bone dimensions in 12-week-old female. | no | no |
| [34] | Pre (GD18 in F0 pregnant mice); | Bilateral uterine vessel ligation in F0 mothers at GD18; | no | no | no | Shortened femurs, reduced trabecular and cortical BMC in females (F1). | Low birth weight in F2 male and female offspring were postnatally recovered. | no |
| [35] | Pre (GD18-19 in F1 pregnant mice) | Physiological measurements (tail cuff blood pressure, glucose tolerance test, metabolic cage experiment) at GD18-19. | ||||||
| [36] | Peri (GD14-21); (PND2-9) | light from 2000 h–0800 h, housing in a wire-mesh-floored pre-partum stress: cage (24 h), food deprivation (12 h), tilting the cage 45° (6 h), exposure to strobe light (1 h), forced swim (10 min), restraint (30 min), and wet bedding (10 h). Post-partum stress: strobe light, wet bedding, wire-mesh-floored cage, food deprivation, restraint, male in-truder (5 min), forced swim, and housing in a small cage. | no | no | no | Reduced tibia length. | Reduced femur length in males. | no |
| ● Rabbit | ||||||||
| [37] | Pre (GD6-19) | Toxic compound: antiprotozoal agent (80, 320, and 1280 mg/kg) | no | Limb abnormalities in high-dose group | no | no | no | no |
| [38] | Pre (GD6-19) | Semi-toxic compound: hydroxy-propyl methylcellulose (100, 500, and 1500 mg/kg) | Less food consumption, weight loss | Low birth weight, transient alterations in ossifications | no | no | no | |
| ● Pig | ||||||||
| [39] | Pre (last 24 GD) | i.m. Dex (3 mg/sow 48 h dosage) | AKG (0.4 g/kg BW/day dosage) | no | Bone markers altered; less mineralized humeri, heavier weight in piglets of AKG-treated mothers. | no | no | no |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pappalardo, X.G.; Testa, G.; Pellitteri, R.; Dell’Albani, P.; Rodolico, M.; Pavone, V.; Parano, E. Early Life Stress (ELS) Effects on Fetal and Adult Bone Development. Children 2023, 10, 102. https://doi.org/10.3390/children10010102
Pappalardo XG, Testa G, Pellitteri R, Dell’Albani P, Rodolico M, Pavone V, Parano E. Early Life Stress (ELS) Effects on Fetal and Adult Bone Development. Children. 2023; 10(1):102. https://doi.org/10.3390/children10010102
Chicago/Turabian StylePappalardo, Xena Giada, Gianluca Testa, Rosalia Pellitteri, Paola Dell’Albani, Margherita Rodolico, Vito Pavone, and Enrico Parano. 2023. "Early Life Stress (ELS) Effects on Fetal and Adult Bone Development" Children 10, no. 1: 102. https://doi.org/10.3390/children10010102