Will Global Climate Change Alter Fundamental Human Immune Reactivity: Implications for Child Health?
Abstract
:1. Introduction
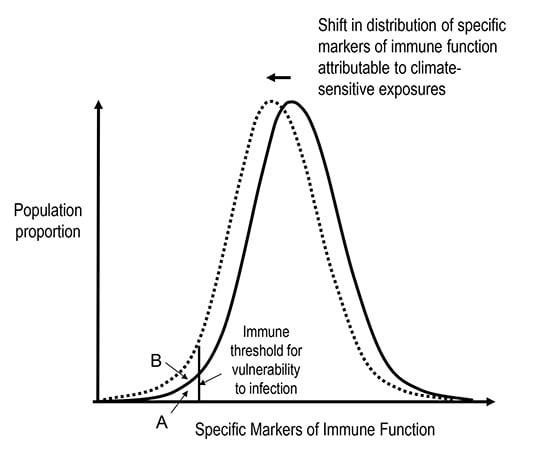
2. Developmental Immunology
3. Clinically Significant Immune Dysfunction: Breaching the Threshold

4. How Can Global Climate Change Affect the Function of a Child’s Immune System?

5. Under-Nutrition, Climate Change and Immune Function
5.1. Under-Nutrition and Human Immune Function
5.2. Climate Change and Under-Nutrition
5.3. Under-Nutrition as a Mediator of Climate-Change Induced Immune Suppression
6. Psychological Stress, Climate Change and the Immune System
6.1. Psychological Stress and Immune Function
6.2. Psychological Stress and Climate Change
I. Acute traumatic stress following an extreme event:
III. Anxiety and fear for the future in a Climate Changed World
6.3. Psychological Stress as a Mediator of Climate Change Induced Immune Dysfunction
7. Ultraviolet Radiation, Climate Change and Immune Function
7.1. Ultraviolet Radiation
7.2. UV Radiation and the Human Immune System
- Suppression of the activity of cutaneous antigen presenting cells (APC) (leading to migration away from skin, and impaired interaction with T cells in the lymph node);
- Promotion of specialised regulatory T cells (Treg) which produce immune inhibitory cytokines (particularly IL-10);
- Inhibition of cytotoxic and memory T cell production and function.
- Cutaneous production of vitamin D, of which the active form (1,25 hydroxyvitamin D3) has been shown to down-regulate cell-mediated immune function processes (e.g., enhanced Treg cell function) and promote innate immune processes (e.g., anti-microbial peptide production) [88].
7.3. Climate Change and UV Radiation
7.4. Ultraviolet Radiation as a Mediator of Climate Change-Induced Immune Dysfunction
8. Conclusions and Implications
Author Contributions
Conflicts of Interest
References
- Stocker, T.; Qin, D.; Plattner, G.; Tignor, M.; Allen, S.; Boschung, J.; Nauels, A.; Xia, Y.; Bex, V.; Midgley, P. (Eds.) Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Stocker, T.; Qin, D.; Plattner, G.; Tignor, M.; Allen, S.; Boschung, J.; Nauels, A.; Xia, Y.; Bex, V.; Midgley, P. (Eds.) Cambridge University Press: Cambridge, UK; New York, NY, USA, 2013.
- Confalonieri, U.; Menne, B. Human Health. In Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; Parry, M.L., Canziani, O.F., Palutikof, J.P., van der Linden, P.J., Hanson, C.E., Eds.; Cambridge University Press: Cambridge, UK, 2007; pp. 391–431. [Google Scholar]
- Field, C.; Barros, V.; Dokken, D.; Mach, K.; Mastrandrea, M.; Billir, T.; Chatterjee, M.; Ebi, K.; Estrada, Y.; Genova, R. (Eds.) Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Field, C.; Barros, V.; Dokken, D.; Mach, K.; Mastrandrea, M.; Billir, T.; Chatterjee, M.; Ebi, K.; Estrada, Y.; Genova, R. (Eds.) Cambridge University Press: Cambridge, UK; New York, NY, USA, 2014; pp. 1–32.
- Sheffield, P.E.; Landrigan, P.J. Global climate change and children’s health: threats and strategies for prevention. Environ. Health Perspect. 2011, 119, 291–298. [Google Scholar] [CrossRef] [PubMed]
- McMichael, A.J.; Campbell-Lendrum, D.; Kovats, S.; Edwards, S.; Wilkinson, P.; Wilson, T.; Nichols, R.; Hales, S.; Tanser, F.; Le Sueur, D.; Schlesinger, M.; Andronova, N. Global and Regional Burden of Disease due to Selected Major Risk Factors. In Comparative Quantification of Health Risks; Ezzati, M., Lopez, A.D., Rodgers, A., Murray, C.J., Eds.; World Health Organization: Geneva, 2004; pp. 1543–1650. [Google Scholar]
- Beggs, P.J.; Bambrick, H.J. Is the Global Rise of Asthma an Early Impact of Anthropogenic Climate Change? Environ. Health Perspect. 2005, 113, 915–919. [Google Scholar] [CrossRef]
- Strand, L.B.; Barnett, A.G.; Tong, S. Maternal exposure to ambient temperature and the risks of preterm birth and stillbirth in Brisbane, Australia. Am. J. Epidemiol. 2012, 175, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Prescott, S.L. Early-life environmental determinants of allergic diseases and the wider pandemic of inflammatory noncommunicable diseases. J. Allergy Clin. Immunol. 2013, 131, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Amarasekera, M.; Prescott, S.L.; Palmer, D.J. Nutrition in early life, immune-programming and allergies: the role of epigenetics. Asian Pac. J. Allergy Immunol. 2013, 31, 175–182. [Google Scholar] [PubMed]
- Hostetter, M.K. What we don’t see. N. Engl. J. Med. 2012, 366, 1328–1334. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Cousens, S.; Johnson, H.L.; Lawn, J.E.; Rudan, I.; Bassani, D.G.; Jha, P.; Campbell, H.; Walker, C.F.; Cibulskis, R.; Eisele, T.; Liu, L.; Mathers, C. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010, 375, 1969–1987. [Google Scholar] [CrossRef] [PubMed]
- Levy, O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat. Rev. Immunol. 2007, 7, 379–390. [Google Scholar] [CrossRef] [PubMed]
- Holt, P.G.; Jones, C.A. The development of the immune system during pregnancy and early life. Allergy 2000, 55, 688–697. [Google Scholar] [CrossRef] [PubMed]
- Murphy, K.; Travers, P.; Walport, M. Janeway’s immunobiology, 7th ed.; Garland Science: New York and London, 2008; p. 887. [Google Scholar]
- Jaspan, H.B.; Lawn, S.D.; Safrit, J.T.; Bekker, L.-G. The maturing immune system: implications for development and testing HIV-1 vaccines for children and adolescents. AIDS 2006, 20, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Klein Klouwenberg, P.; Bont, L. Neonatal and infantile immune responses to encapsulated bacteria and conjugate vaccines. Clin. Dev. Immunol. 2008, 2008, 628963. [Google Scholar] [CrossRef]
- PrabhuDas, M.; Adkins, B.; Gans, H.; King, C.; Levy, O.; Ramilo, O.; Siegrist, C.-A. Challenges in infant immunity: implications for responses to infection and vaccines. Nat. Immunol. 2011, 12, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Dockrell, D.; Edwards, S.; Angus, B.; Barton, S.; Beeching, N.; Bergin, C.; Boffito, M.; Breen, R.; Cartledge, J.; Clarke, S.; Fisher, M.; Freedman, A.; Gazzard, B.; Grant, A.; Greig, J.; Jones, R.; Khoo, S.; Leen, C.; Lipman, M.; Manji, H.; Miller, R.; Mitchell, S.; Ong, E.; Pozniak, A.; Schmid, M.; Shiew, M.; Singer, M.; Wilkins, E.; Williams, I.; Wood, C.; Weston, R. British HIV Association and British Infection Association guidelines for the treatment of opportunistic infection in HIV-seropositive individuals 2011. HIV Med. 2011, 12 Suppl 2, 1–140. [Google Scholar] [CrossRef]
- Hortobagyi, G.N.; Smith, T.L.; Swenerton, K.D.; Legha, S.S.; Buzdar, A.U.; Blumenschein, G.R.; Gutterman, J.U.; Hersh, E.M. Prognostic value of prechemotherapy skin tests in patients with metastatic breast carcinoma. Cancer 1981, 47, 1369–1376. [Google Scholar] [CrossRef] [PubMed]
- Christou, N.V; Meakins, J.L.; Gordon, J.; Yee, J.; Hassan-Zahraee, M.; Nohr, C.W.; Shizgal, H.M.; MacLean, L.D. The delayed hypersensitivity response and host resistance in surgical patients. 20 years later. Ann. Surg. 1995, 222, 534–546, discussion 546–548. [Google Scholar]
- Van Loveren, H.; Germolec, D.; Koren, H.; Luster, M.; Nolan, C.; Repetto, R.; Smith, E.; Vos, J.; Vogt, R. Report of the Bilthoven Symposium: Advancement of Epidemiological Studies in Assessing the Human Health Effects of Immunotoxic Agents in the Environment and the Workplace. Biomarkers 1999, 4, 135–157. [Google Scholar] [CrossRef] [PubMed]
- Norval, M. Immunosuppression induced by ultraviolet radiation: relevance to public health. Bull. World Health Organ. 2002, 80, 906–907. [Google Scholar] [PubMed]
- IPCC Working Group 2: Impacts, Adaptation and Vulnerability. Available online: http://www.ipcc.ch/report/ar5/wg2/ (accessed on 10 July 2014).
- Koelle, K.; Rodó, X.; Pascual, M.; Yunus, M.; Mostafa, G. Refractory periods and climate forcing in cholera dynamics. Nature 2005, 436, 696–700. [Google Scholar] [CrossRef] [PubMed]
- McMichael, A.J. Globalization, climate change, and human health. N. Engl. J. Med. 2013, 368, 1335–1343. [Google Scholar] [CrossRef] [PubMed]
- Björkstén, B. Environmental influences on the development of the immune system: consequences for disease outcome. Nestle Nutr. Workshop Ser. Pediatr. Program. 2008, 61, 243–254. [Google Scholar] [PubMed]
- Calder, P.C.; Krauss-Etschmann, S.; de Jong, E.C.; Dupont, C.; Frick, J.-S.; Frokiaer, H.; Heinrich, J.; Garn, H.; Koletzko, S.; Lack, G.; Mattelio, G.; Renz, H.; Sangild, P.T.; Schrezenmeir, J.; Stulnig, T.M.; Thymann, T.; Wold, A.E.; Koletzko, B. Early nutrition and immunity - progress and perspectives. Br. J. Nutr. 2006, 96, 774–790. [Google Scholar] [CrossRef] [PubMed]
- McMichael, C.; Barnett, J.; McMichael, A.J. An ill wind? Climate change, migration, and health. Environ. Health Perspect. 2012, 120, 646–654. [Google Scholar] [CrossRef] [PubMed]
- Segerstrom, S.C.; Miller, G.E. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol. Bull. 2004, 130, 601–630. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K.; McGuire, L.; Robles, T.F.; Glaser, R. Psychoneuroimmunology: psychological influences on immune function and health. J. Consult. Clin. Psychol. 2002, 70, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Hu, Y.; Han, D.; Wang, M. Chronic heat stress weakened the innate immunity and increased the virulence of highly pathogenic avian influenza virus H5N1 in mice. J. Biomed. Biotechnol. 2011, 2011, 367846. [Google Scholar] [CrossRef]
- Meng, D.; Hu, Y.; Xiao, C.; Wei, T.; Zou, Q.; Wang, M. Chronic heat stress inhibits immune responses to H5N1 vaccination through regulating CD4+ CD25+ Foxp3+ Tregs. Biomed Res. Int. 2013, 2013, 160859. [Google Scholar] [CrossRef]
- Strazdins, L.; Skeat, H. Weathering the future: Climate change, children and young people and decision making. A report to the Australian Research Alliance for Children and Youth (ARACY), 2011.
- Chandra, R.K. Nutrition and the immune system: an introduction. Am. J. Clin. Nutr. 1997, 66, 460S. [Google Scholar] [PubMed]
- Schaible, U.E.; Kaufmann, S.H.E. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007, 4, e115. [Google Scholar] [CrossRef]
- Scrimshaw, N.S.; SanGiovanni, J.P. Synergism of nutrition, infection, and immunity: an overview. Am. J. Clin. Nutr. 1997, 66, 464S–477S. [Google Scholar] [PubMed]
- Chandra, R.K. Nutrition and the immune system from birth to old age. Eur. J. Clin. Nutr. 2002, 56 Suppl 3, S73–S76. [Google Scholar] [CrossRef]
- Garre, M.A.; Boles, J.M.; Youinou, P.Y. Current concepts in immune derangement due to undernutrition. J. Parenter. Enter. Nutr. 1987, 11, 309–313. [Google Scholar] [CrossRef]
- Savino, W.; Dardenne, M.; Velloso, L.A.; Dayse Silva-Barbosa, S. The thymus is a common target in malnutrition and infection. Br. J. Nutr. 2007, 98 Suppl 1, S11–S16. [Google Scholar]
- Kizito, D.; Tweyongyere, R.; Namatovu, A.; Webb, E.L.; Muhangi, L.; Lule, S.A.; Bukenya, H.; Cose, S.; Elliott, A.M. Factors affecting the infant antibody response to measles immunisation in Entebbe-Uganda. BMC Public Health 2013, 13, 619. [Google Scholar] [CrossRef] [PubMed]
- Gaayeb, L.; Sarr, J.B.; Cames, C.; Pinçon, C.; Hanon, J.-B.; Ndiath, M.O.; Seck, M.; Herbert, F.; Sagna, A.B.; Schacht, A.-M.; Remoue, F.; Riveau, G.; Hermann, E. Effects of malnutrition on children’s immunity to bacterial antigens in Northern Senegal. Am. J. Trop. Med. Hyg. 2014, 90, 566–573. [Google Scholar] [CrossRef] [PubMed]
- Schmidhuber, J.; Tubiello, F.N. Global food security under climate change. Proc. Natl. Acad. Sci. U. S. A. 2007, 104, 19703–19708. [Google Scholar] [CrossRef] [PubMed]
- Parry, M.; Rosenzweig, C.; Iglesias, A.; Livermore, M.; Fischer, G. Effects of climate change on global food production under SRES emissions and socio-economic scenarios. Glob. Environ. Chang. 2004, 14, 53–67. [Google Scholar]
- Ziska, L.H.; Bunce, J.A.; Shimono, H.; Gealy, D.R.; Baker, J.T.; Newton, P.C.D.; Reynolds, M.P.; Jagadish, K.S.V.; Zhu, C.; Howden, M.; Wilson, L.T. Food security and climate change: on the potential to adapt global crop production by active selection to rising atmospheric carbon dioxide. Proc. Biol. Sci. 2012, 279, 4097–4105. [Google Scholar]
- Nelson, G.C.; Rosegrant, M.W.; Koo, J.; Robertson, R.; Sulser, T.; Zhu, T.; Ringler, C.; Msangi, S.; Palazzo, A.; Batka, M.; Magalhaes, M.; Valmonte-Santos, R.; Ewing, M.; Lee, D. Climate Change Impact on Agriculture and Costs of Adaptation; Washington D.C, 2009; p. 30. [Google Scholar]
- Fischer, G.; Shah, M.; Tubiello, F.N.; van Velhuizen, H. Socio-economic and climate change impacts on agriculture: an integrated assessment, 1990-2080. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2005, 360, 2067–2083. [Google Scholar] [CrossRef] [PubMed]
- Knox, J.; Hess, T.; Daccache, A.; Wheeler, T. Climate change impacts on crop productivity in Africa and South Asia. Environ. Res. Lett. 2012, 7, 034032. [Google Scholar] [CrossRef]
- Zhang, Y.; Bi, P.; Hiller, J.E. Climate variations and Salmonella infection in Australian subtropical and tropical regions. Sci. Total Environ. 2010, 408, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Allard, R.; Plante, C.; Garnier, C.; Kosatsky, T. The reported incidence of campylobacteriosis modelled as a function of earlier temperatures and numbers of cases, Montreal, Canada, 1990-2006. Int. J. Biometeorol. 2011, 55, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Checkley, W.; Epstein, L.D.; Gilman, R.H.; Figueroa, D.; Cama, R.I.; Patz, J.A.; Black, R.E. Effect of El Niño and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet 2000, 355, 442–450. [Google Scholar] [PubMed]
- Griffith, D.C.; Kelly-Hope, L.A.; Miller, M.A. Review of reported cholera outbreaks worldwide, 1995-2005. Am. J. Trop. Med. Hyg. 2006, 75, 973–977. [Google Scholar] [PubMed]
- Food and Agriculture Organization (FAO). The State of Food and Agriculture; Rome, 2013. [Google Scholar]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; de Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar]
- Lloyd, S.J.; Kovats, R.S.; Chalabi, Z. Climate change, crop yields, and undernutrition: development of a model to quantify the impact of climate scenarios on child undernutrition. Environ. Health Perspect. 2011, 119, 1817–1823. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological stress and disease. JAMA 2007, 298, 1685–1687. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.M.; Miller, G.E.; Chen, E. Parent psychological states predict changes in inflammatory markers in children with asthma and healthy children. Brain. Behav. Immun. 2008, 22, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.E.; Chen, E. Harsh family climate in early life presages the emergence of a proinflammatory phenotype in adolescence. Psychol. Sci. 2010, 21, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Caserta, M.T.; Wyman, P.A.; Wang, H.; Moynihan, J.; O’Connor, T.G. Associations among depression, perceived self-efficacy, and immune function and health in preadolescent children. Dev. Psychopathol. 2011, 23, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Doom, J.R.; Gunnar, M.R. Stress physiology and developmental psychopathology: past, present, and future. Dev. Psychopathol. 2013, 25, 1359–1373. [Google Scholar] [CrossRef] [PubMed]
- Hostinar, C.E.; Gunnar, M.R. Future directions in the study of social relationships as regulators of the HPA axis across development. J. Clin. Child Adolesc. Psychol. 2013, 42, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Lumeng, J.C.; Miller, A.; Peterson, K.E.; Kaciroti, N.; Sturza, J.; Rosenblum, K.; Vazquez, D.M. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite 2014, 73, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, E.; Frostell, A.; Ludvigsson, J.; Faresjö, M. Psychological stress in children may alter the immune response. J. Immunol. 2014, 192, 2071–2081. [Google Scholar] [CrossRef] [PubMed]
- Theall, K.P.; Drury, S.S.; Shirtcliff, E.A. Cumulative neighborhood risk of psychosocial stress and allostatic load in adolescents. Am. J. Epidemiol. 2012, 176 Suppl, S164–S174. [Google Scholar] [CrossRef]
- Doan, S.N.; Dich, N.; Evans, G.W. Childhood Cumulative Risk and Later Allostatic Load: Mediating Role of Substance Use. Health Psychol. 2013. [Google Scholar]
- Danese, A.; McEwen, B.S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 2012, 106, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Zung, A.; Blumenfeld, O.; Shehadeh, N.; Dally Gottfried, O.; Tenenbaum Rakover, Y.; Hershkovitz, E.; Gillis, D.; Zangen, D.; Pinhas-Hamiel, O.; Hanukoglu, A.; Rachmiel, M.; Shalitin, S. Increase in the incidence of type 1 diabetes in Israeli children following the Second Lebanon War. Pediatr. Diabetes 2012, 13, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Fritze, J.G.; Blashki, G.A.; Burke, S.; Wiseman, J. Hope, despair and transformation: Climate change and the promotion of mental health and wellbeing. Int. J. Ment. Health Syst. 2008, 2, 13. [Google Scholar]
- Larrance, R.; Anastario, M.; Lawry, L. Health status among internally displaced persons in Louisiana and Mississippi travel trailer parks. Ann. Emerg. Med. 2007, 49, 590–601, 601.e1–601.e12. [Google Scholar] [CrossRef] [PubMed]
- Kar, N.; Mohapatra, P.K.; Nayak, K.C.; Pattanaik, P.; Swain, S.P.; Kar, H.C. Post-traumatic stress disorder in children and adolescents one year after a super-cyclone in Orissa, India: exploring cross-cultural validity and vulnerability factors. BMC Psychiatry 2007, 7, 8. [Google Scholar] [CrossRef]
- Prince, M.; Patel, V.; Saxena, S.; Maj, M.; Maselko, J.; Phillips, M.R.; Rahman, A. No health without mental health. Lancet 2007, 370, 859–877. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.J.; Taylor, S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar]
- Inter-Agency Standing Committee (IASC). IASC Guidelines on Mental Health and Psychosocial support in Emergency Settings; Geneva, 2007. [Google Scholar]
- International Organization for Migration (IOM). Migration and Climate Change; Geneva, 2008. [Google Scholar]
- Soeteman, R.J.H.; Yzermans, C.J.; Kerssens, J.J.; Dirkzwager, A.J.E.; Donker, G.A.; ten Veen, P.M.H.; van den Bosch, W.J.H.M.; van der Zee, J. Health problems presented to family practices in the Netherlands 1 year before and 1 year after a disaster. J. Am. Board Fam. Med. 2007, 20, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Dean, J.G.; Stain, H.J. Mental health impact for adolescents living with prolonged drought. Aust. J. Rural Health 2010, 18, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, N.; Butler, C.D.; Hanigan, I. Inter-annual rainfall variations and suicide in New South Wales, Australia, 1964-2001. Int. J. Biometeorol. 2006, 50, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Dyer, J. Psychological effects of the nuclear arms race on children. Med. War 1986, 2, 261–262. [Google Scholar] [CrossRef] [PubMed]
- Tucci, J.; Mitchell, J.; Goddard, C. Children’s fears, hopes and heroes Modern childhood in Australia; Melbourne, 2007. [Google Scholar]
- Bartlett, S. The Implications of Climate Change for Children in Lower-Income Countries. J. Trop. Pediatr. 2008, 18. [Google Scholar]
- Ironson, G.; Wynings, C.; Schneiderman, N.; Baum, A.; Rodriguez, M.; Greenwood, D.; Benight, C.; Antoni, M.; LaPerriere, A.; Huang, H.S.; Klimas, N.; Fletcher, M.A. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosom. Med. 2007, 59, 128–141. [Google Scholar] [CrossRef]
- Bikle, D.D. Vitamin D and immune function: understanding common pathways. Curr. Osteoporos. Rep. 2009, 7, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.M.; McMichael, A.J.; Smith, W.; Armstrong, B.K. Solar Ultraviolet Radiation Global burden of disease from solar ultraviolet radiation. In Environmental Burden of Disease Series; Prüss-üstün, A., Zeeb, H., Mathers, C., Repacholi, M., Eds.; World Health Organisation, 2006. [Google Scholar]
- Halliday, G.M.; Rana, S. Waveband and dose dependency of sunlight-induced immunomodulation and cellular changes. Photochem. Photobiol. 2008, 84, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Aucamp, P.J. Questions and answers about the effects of the depletion of the ozone layer on humans and the environment. Photochem. Photobiol. Sci. 2007, 6, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Godar, D.E. UV doses worldwide. Photochem. Photobiol. 2005, 81, 736–749. [Google Scholar] [CrossRef] [PubMed]
- Norval, M.; Halliday, G.M. The consequences of UV-induced immunosuppression for human health. Photochem. Photobiol. 2011, 87, 965–977. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, S.E.; Byrne, S.N. The Immunologic Revolution: Photoimmunology. J. Invest. Dermatol. 2011, 132, 896–905. [Google Scholar] [CrossRef] [PubMed]
- Hart, P.H.; Gorman, S.; Finlay-Jones, J.J. Modulation of the immune system by UV radiation: more than just the effects of vitamin D? Nat. Rev. Immunol. 2011, 11, 1–13. [Google Scholar]
- Jeevan, A.; Kripke, M.L. Ozone depletion and the immune system. Lancet 1993, 342, 1159–1160. [Google Scholar] [CrossRef] [PubMed]
- Sleijffers, A.; Garssen, J.; Van Loveren, H. Ultraviolet radiation, resistance to infectious diseases, and vaccination responses. Methods 2002, 28, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Norval, M. The effect of ultraviolet radiation on human viral infections. Photochem. Photobiol. 2006, 82, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Norval, M.; Woods, G.M. UV-induced immunosuppression and the efficacy of vaccination. Photochem. Photobiol. Sci. 2011, 10, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- Sleijffers, A.; Garssen, J.; de Gruijl, F.R.; Boland, G.J.; van Hattum, J.; van Vloten, W.A.; van Loveren, H. UVB exposure impairs immune responses after hepatitis B vaccination in two different mouse strains. Photochem. Photobiol. 2002, 75, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Sleijffers, A.; Garssen, J.; de Gruijl, F.; Boland, G.; van Hattum, J.; van Vloten, W.; van Loveren, H. Influence of ultraviolet B exposure on immune responses following hepatitis B vaccination in human volunteers. J Invest Dermatol 2001, 117, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Sleijffers, A.; Yucesoy, B.; Kashon, M.; Garssen, J.; De Gruijl, F.R.; Boland, G.J.; Van Hattum, J.; Luster, M.I.; Van Loveren, H. Cytokine polymorphisms play a role in susceptibility to ultraviolet B-induced modulation of immune responses after hepatitis B vaccination. J. Immunol. 2003, 170, 3423–3428. [Google Scholar] [CrossRef] [PubMed]
- John, T.J.; Jayabal, P. Oral polio vaccination of children in the tropics. I. The poor seroconversion rates and the absence of viral interference. Am. J. Epidemiol. 1972, 96, 263–269, ST – Oral polio vaccination of children in. [Google Scholar]
- Swartz, T.A.; Skalska, P.; Gerichter, C.G.; Cockburn, W.C. Routine administration of oral polio vaccine in a subtropical area. Factors possibly influencing sero-conversion rates. J. Hyg. (Lond). 1972, 70, 719–726. [Google Scholar] [PubMed]
- Linder, N.; Abudi, Y.; Abdalla, W.; Badir, M.; Amitai, Y.; Samuels, J.; Mendelson, E.; Levy, I. Effect of season of inoculation on immune response to rubella vaccine in children. J. Trop. Pediatr. 2011, 57, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.K.; Bhatia, V.; Swami, H.M. Outbreak of measles amongst vaccinated children in a slum of Chandigarh. Indian J. Med. Sci. 2004, 58, 47–53. [Google Scholar] [PubMed]
- Ponsonby, A.; Lucas, R.; van der Mei, A. Vitamin D and Three Autoimmune Diseases-Multiple Sclerosis, Type 1 Diabetes , Rheumatoid Arthritis. Photochem. Photobiol. 2005, 81, 1267–1275. [Google Scholar] [CrossRef] [PubMed]
- Gatenby, P.; Lucas, R.; Swaminathan, A. Vitamin D deficiency and risk for rheumatic diseases: an update. Curr. Opin. Rheumatol. 2013, 25, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Di Rosa, M.; Malaguarnera, M.; Nicoletti, F.; Malaguarnera, L. Vitamin D3: a helpful immuno-modulator. Immunology 2011, 134, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Thomas, P.; Swaminathan, A.; Lucas, R.M. Climate change and health with an emphasis on interactions with ultraviolet radiation: a review. Glob. Chang. Biol. 2012, 18, 2392–2405. [Google Scholar] [CrossRef]
- Hegglin, M.I.; Shepherd, T.G. Large climate-induced changes in ultraviolet index and stratosphere-to-troposphere ozone flux. Nat. Geosci. 2009, 2, 687–691. [Google Scholar] [CrossRef]
- McKenzie, R.L.; Aucamp, P.J.; Bais, A.F.; Björn, L.O.; Ilyas, M. Changes in biologically-active ultraviolet radiation reaching the Earth’s surface. Photochem. Photobiol. Sci. Off. J. Eur. Photochem. Assoc. Eur. Soc. Photobiol. 2007, 6, 218–231. [Google Scholar]
- McKenzie, R.L.; Aucamp, P.J.; Bais, A.F.; Björn, L.O.; Ilyas, M.; Madronich, S. Ozone depletion and climate change: impacts on UV radiation. Photochem. Photobiol. Sci. 2011, 10, 182–198. [Google Scholar] [CrossRef] [PubMed]
- Diffey, B.L.; Gibson, C.J.; Haylock, R.; McKinlay, A.F. Outdoor ultraviolet exposure of children and adolescents. Br. J. Dermatol. 1996, 134, 1030–1034. [Google Scholar]
- Andrady, A.L.; Aucamp, P.J.; Austin, A.T.; Bais, A.F.; Ballaré, C.L.; Björn, L.O.; Bornman, J.F.; Caldwell, M.; Cullen, A.P.; Erickson, D.J.; de Gruijl, F.R.; Häder, D.-P.; He, W.; Ilyas, M.; Longstreth, J.; Lucas, R.; McKenzie, R.L.; Madronich, S.; Norval, M.; Paul, N.D.; Redhwi, H.H.; Robinson, S.; Shao, M.; Solomon, K.R.; Sulzberger, B.; Takizawa, Y.; Tang, X.; Torikai, A.; van der Leun, J.C.; Williamson, C.E.; Wilson, S.R.; Worrest, R.C.; Zepp, R.G. Environmental effects of ozone depletion and its interactions with climate change: progress report, 2011. Photochem. Photobiol. Sci. 2012, 11, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Staples, J.; Ponsonby, A.-L.; Lim, L. Low maternal exposure to ultraviolet radiation in pregnancy, month of birth, and risk of multiple sclerosis in offspring: longitudinal analysis. BMJ 2010, 340, c1640. [Google Scholar] [CrossRef]
- Willer, C.J.; Dyment, D.A.; Sadovnick, A.D.; Rothwell, P.M.; Murray, T.J.; Ebers, G.C. Timing of birth and risk of multiple sclerosis: population based study. BMJ 2005, 330, 120. [Google Scholar] [CrossRef]
- Mitchell, D. The relationship between vitamin D and cancer. Clin. J. Oncol. Nurs. 2011, 15, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Pludowski, P.; Holick, M.F.; Pilz, S.; Wagner, C.L.; Hollis, B.W.; Grant, W.B.; Shoenfeld, Y.; Lerchbaum, E.; Llewellyn, D.J.; Kienreich, K.; Soni, M. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality-a review of recent evidence. Autoimmun. Rev. 2013, 12, 976–989. [Google Scholar] [CrossRef] [PubMed]
- Goettsch, W.; Garssen, J.; Slob, W.; de Gruijl, F.R.; Van Loveren, H. Risk assessment for the harmful effects of UVB radiation on the immunological resistance to infectious diseases. Environ. Health Perspect. 1998, 106, 71–77. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Swaminathan, A.; Lucas, R.M.; Harley, D.; McMichael, A.J. Will Global Climate Change Alter Fundamental Human Immune Reactivity: Implications for Child Health? Children 2014, 1, 403-423. https://doi.org/10.3390/children1030403
Swaminathan A, Lucas RM, Harley D, McMichael AJ. Will Global Climate Change Alter Fundamental Human Immune Reactivity: Implications for Child Health? Children. 2014; 1(3):403-423. https://doi.org/10.3390/children1030403
Chicago/Turabian StyleSwaminathan, Ashwin, Robyn M. Lucas, David Harley, and Anthony J. McMichael. 2014. "Will Global Climate Change Alter Fundamental Human Immune Reactivity: Implications for Child Health?" Children 1, no. 3: 403-423. https://doi.org/10.3390/children1030403