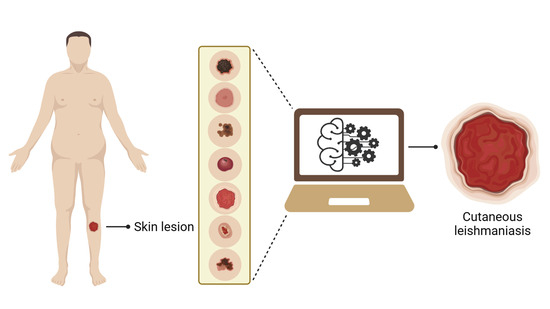
Automated Identification of Cutaneous Leishmaniasis Lesions Using Deep-Learning-Based Artificial Intelligence
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Picture Database
2.2. Algorithm: Training and Testing
2.3. Data Analysis
2.4. Ethical Consideration
3. Results
3.1. Training
3.2. AlexNet Performance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mathison, B.A.; Bradley, B.T. Review of the Clinical Presentation, Pathology, Diagnosis, and Treatment of Leishmaniasis. Lab. Med. 2023, 54, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Nazzaro, G.; Rovaris, M.; Veraldi, S. Leishmaniasis: A disease with many names. JAMA Dermatol. 2014, 150, 1204. [Google Scholar] [CrossRef] [PubMed]
- Burza, S.; Croft, S.L.; Boelaert, M. Leishmaniasis. Lancet 2018, 392, 951–970. [Google Scholar] [CrossRef] [PubMed]
- Alvar, J.; Vélez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Jannin, J.; Boer, M.D.; WHO Leishmaniasis Control Team. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 2012, 7, e35671. [Google Scholar] [CrossRef] [PubMed]
- Abadías-Granado, I.; Diago, A.; Cerro, P.A.; Palma-Ruiz, A.M.; Gilaberte, Y. Leishmaniasis cutánea y mucocutánea. Actas Dermosifiliogr. 2021, 112, 601–618. [Google Scholar] [CrossRef] [PubMed]
- Goto, H.; Lindoso, J.A.L. Cutaneous and mucocutaneous leishmaniasis. Infect. Dis. Clin. 2012, 26, 293–307. [Google Scholar] [CrossRef] [PubMed]
- Showler, A.J.; Boggild, A.K. Cutaneous leishmaniasis in travellers: A focus on epidemiology and treatment in 2015. Curr. Infect. Dis. Rep. 2015, 17, 37. [Google Scholar] [CrossRef] [PubMed]
- Aronson, N.E.; Joya, C.A. Cutaneous leishmaniasis: Updates in diagnosis and management. Infect. Dis. Clin. 2019, 33, 101–117. [Google Scholar] [CrossRef]
- Leishmaniasis. Available online: https://www.who.int/news-room/fact-sheets/detail/leishmaniasis (accessed on 24 July 2023).
- Mitropoulos, P.; Konidas, P.; Durkin-konidas, M. New World cutaneous leishmaniasis: Updated review of current and future diagnosis and treatment. J. Am. Acad. Dermatol. 2010, 63, 309–322. [Google Scholar] [CrossRef]
- Handler, M.Z.; Patel, P.A.; Kapila, R.; Al-Qubati, Y.; Schwartz, R.A. Cutaneous and mucocutaneous leishmaniasis: Differential diagnosis, diagnosis, histopathology, and management. J. Am. Acad. Dermatol. 2015, 73, 911–926. [Google Scholar] [CrossRef]
- Tirelli, F.; Vernal, S.; Roselino, A.M. Final diagnosis of 86 cases included in differential diagnosis of American tegumentary leishmaniasis in a Brazilian sample: A retrospective cross-sectional study. An. Bras. Dermatol. 2017, 92, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Vink, M.M.; Nahzat, S.M.; Rahimi, H.; Buhler, C.; Ahmadi, B.A.; Nader, M.; Zazai, F.R.; Yousufzai, A.S.; Loenen, M.V.; Schallig, H.D.F.H.; et al. Evaluation of point-of-care tests for cutaneous leishmaniasis diagnosis in Kabul, Afghanistan. EBioMed 2018, 37, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Gurel, M.S.; Tekin, B.; Uzun, S. Cutaneous leishmaniasis: A great imitator. Clin. Dermatol. 2020, 38, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Doupe, P.; Faghmous, J.; Basu, S. Machine learning for health services researchers. Val. Health 2019, 22, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Leha, A.; Hellenkamp, K.; Unsöld, B.; Mushemi-Blake, S.; Shah, A.M.; Hasenfuß, G.; Seidler, T. A machine learning approach for the prediction of pulmonary hypertension. PLoS ONE 2019, 14, e0224453. [Google Scholar] [CrossRef] [PubMed]
- Sippy, R.; Farrell, D.F.; Lichtenstein, D.A.; Nightingale, R.; Harris, M.A.; Toth, J.; Hantztidiamantis, P.; Usher, N.; Aponte, C.C.; Aguilar, J.B.; et al. Severity Index for Suspected Arbovirus (SISA): Machine learning for accurate prediction of hospitalization in subjects suspected of arboviral infection. PLoS Negl. Trop. Dis. 2020, 14, e0007969. [Google Scholar] [CrossRef] [PubMed]
- Bamorovat, M.; Sharifi, I.; Rashedi, E.; Shafiian, A.; Sharifi, F.; Khosravi, A.; Tahmouresi, A. A novel diagnostic and prognostic approach for unresponsive patients with anthroponotic cutaneous leishmaniasis using artificial neural networks. PLoS ONE 2021, 16, e0250904. [Google Scholar] [CrossRef]
- Han, S.S.; Moon, I.J.; Lim, W.; Suh, I.S.; Lee, S.Y.; Na, J.I.; Kim, S.H.; Chang, S.E. Keratinocytic skin cancer detection on the face using region-based convolutional neural network. JAMA Dermatol. 2020, 156, 29–37. [Google Scholar] [CrossRef]
- Tschandl, P.; Rinner, C.; Apalla, Z.; Argenziano, G.; Codella, N.; Halpern, A.; Janda, M.; Lallas, A.; Longo, C.; Malvehy, J.; et al. Human–computer collaboration for skin cancer recognition. Nat. Med. 2020, 26, 1229–1234. [Google Scholar] [CrossRef]
- Srinivasu, P.N.; SivaSai, J.G.; Ijaz, M.F.; Bhoi, A.K.; Kim, W.; Kang, J.J. Classification of skin disease using deep learning neural networks with MobileNet V2 and LSTM. Sensors 2021, 21, 2852. [Google Scholar] [CrossRef]
- De, A.; Sarda, A.; Gupta, S.; Das, S. Use of artificial intelligence in dermatology. Indian J. Dermatol. 2020, 65, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Goceri, E. Diagnosis of skin diseases in the era of deep learning and mobile technology. Comput. Biol. Med. 2021, 134, 104458. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, R.R.; Xu, Y.; Setian, L.; Souza-Santos, P.T.; Trivedi, A.; Cristofono, J.; Bhering, R.; White, K.; Sales, A.M.; Miller, G. Reimagining leprosy elimination with AI analysis of a combination of skin lesion pictures with demographic and clinical data. Lancet Reg. Health Am. 2022, 9, 1–9. [Google Scholar] [CrossRef]
- Jones, O.T.; Matin, R.N.; Van der Schaar, M.; Prathivadi Bhayankaram, K.; Ranmuthu, C.K.I.; Islam, M.S.; Behiyat, D.; Boscott, R.; Calanzani, N.; Emery, J.; et al. Artificial intelligence and machine learning algorithms for early detection of skin cancer in community and primary care settings: A systematic review. Lancet Dig. Health 2022, 4, e466–e476. [Google Scholar] [CrossRef] [PubMed]
- Smak Gregoor, A.M.; Sangers, T.E.; Bakker, L.J.; Hollestein, L.; Uyl–de Groot, C.A.; Nijsten, T.; Wakkee, M. An artificial intelligence based app for skin cancer detection evaluated in a population based setting. NPJ Dig. Med. 2023, 6, 90. [Google Scholar] [CrossRef] [PubMed]
- Noureldeen, A.M.; Masoud, K.S.; Almakhzoom, O.A. Deep learning model for Cutaneous leishmaniasis detection and classification using Yolov5. Afr. J. Adv. Pure Appl. Sci. 2023, 2, 270–280. [Google Scholar]
- Litjens, G.; Kooi, T.; Bejnordi, B.E.; Setio, A.A.A.; Ciompi, F.; Ghafoorian, M.; Van der Laak, J.A.W.M.; Van Ginneken, B.; Sánchez, C.I. A Survey on Deep Learning in Medical Image Analysis. Med. Imag. Anal. 2017, 42, 60–88. [Google Scholar] [CrossRef] [PubMed]
- Latif, J.; Xiao, C.; Imran, A.; Tu, S. Medical imaging using machine learning and deep learning algorithms: A Review. In Proceedings of the 2019 2nd International Conference on Computing, Mathematics and Engineering Technologies (iCoMET), Sukkur, Pakistan, 30–31 January 2019; pp. 1–5. [Google Scholar] [CrossRef]
- Souza, E.P.D.; Gomes, C.M.; Barroso, D.H.; Miranda, V.L.D.; Gurgel-Gonçalves, R. Aplicações do Deep Learning para diagnóstico de doenças e identificação de insetos vetores. Saúde Debat. 2020, 43, 147–154. [Google Scholar] [CrossRef]
- Gomes, C.M.; Paula, N.A.; Morais, O.O.; Soares, K.A.; Roselino, A.M.; Sampaio, R.N. Complementary exams in the diagnosis of American tegumentary leishmaniasis. An. Bras. Dermatol. 2014, 89, 701–709. [Google Scholar] [CrossRef]
- Pinheiro, A.B.S.; Kurizky, P.S.; Ferreira, M.D.F.; Mota, M.A.D.S.; Ribeiro, J.S.; Oliveira Filho, E.Z.D.; Souza, C.A.; Barroso, D.H.; Sampaio, R.N.R.; Gomes, C.M. The accuracy of the Montenegro skin test for leishmaniasis in PCR-negative patients. Rev. Soc. Bras. Med. Trop. 2020, 53, e20190433. [Google Scholar] [CrossRef]
- Barroso, D.H.; Gonçalves, R.T.; Barbosa, J.S.; Motta, J.D.O.C.; Freire, G.S.M.; Gomes, C.M.; Sampaio, R.N.R. Meglumine antimoniate was associated with a higher cure rate than liposomal amphotericin B in the treatment of American tegumentary leishmaniasis: A retrospective cohort study from a Leishmania braziliensis-endemic area. Front. Cell. Infect. Microbiol. 2022, 12, 1426. [Google Scholar] [CrossRef] [PubMed]
- Tegumentary Leishmaniasis Surveillance Manual. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/manual_vigilancia_leishmaniose_tegumentar.pdf (accessed on 30 August 2023).
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. ImageNet classification with deep convolutional neural networks. Comm. ACM 2017, 60, 84–90. [Google Scholar] [CrossRef]
- Motta, D.; Santos, A.Á.B.; Winkler, I.; Machado, B.A.S.; Pereira, D.A.D.I.; Cavalcanti, A.M.; Fonseca, E.O.L.; Kirchner, F.; Badaró, R. Application of convolutional neural networks for classification of adult mosquitoes in the field. PLoS ONE 2019, 14, e0210829. [Google Scholar] [CrossRef] [PubMed]
- Miranda, V.L.; Souza, E.P.; Bambil, D.; Khalighifar, A.; Peterson, A.T.; Nascimento, F.A.O.; Gurgel-Gonçalves, R.; Abad-Franch, F. Cellphone-picture based automated identification of Chagas disease vectors: Effects of bug genus and image orientation on the performance of five machine-learning algorithms. Ecol. Inf. 2023, 79, e102430. [Google Scholar] [CrossRef]
- Hamida, A.B.; Devanne, M.; Weber, J.; Truntzer, C.; Derangère, V.; Ghiringhelli, F.; Forestier, G.; Wemmert, C. Deep learning for colon cancer histopathological images analysis. Comput. Biol. Med. 2021, 136, 104730. [Google Scholar] [CrossRef]
- Kumar, L.S.; Hariharasitaraman, S.; Narayanasamy, K.; Thinakaran, K.; Mahalakshmi, J.; Pandimurugan, V. AlexNet approach for early stage Alzheimer’s disease detection from MRI brain images. Mater. Today Proc. 2022, 51, 58–65. [Google Scholar] [CrossRef]
- Newcombe, R.G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat Med. 1998, 17, 857–872. [Google Scholar] [CrossRef]
- RStudio Team. RStudio: Integrated Development for R. RStudio, PBC, Boston, MA. RStudio 2023.03.1.446. 2022. Available online: https://posit.co/products/open-source/rstudio/ (accessed on 14 August 2023).
- R Core Team. Available online: https://www.Rproject.org/ (accessed on 30 August 2023).
- Package ‘Hmisc’: Harrell Miscellaneous. Available online: http://www.who.int/mediacentre/factsheets/fs340/en/ (accessed on 30 August 2023).
- Abad-Franch, F. Chagas disease diagnosis and cure assessment: Getting formally hierarchical about a naturally hierarchical problem. PLoS Negl. Trop. Dis. 2020, 14, e0008751. [Google Scholar] [CrossRef]
- Bossuyt, P.M.M.; Reitsma, J.B.; Linnet, K.; Moons, K.G.M. Beyond diagnostic accuracy: The clinical utility of diagnostic tests. Clin. Chem. 2012, 58, 1636–1643. [Google Scholar] [CrossRef]
- Borges, L. Medidas de acurácia diagnóstica na pesquisa cardiovascular. Int. J. Cardiovasc. Sci. 2016, 29, 218–222. [Google Scholar] [CrossRef]
- Du-Harpur, X.; Watt, F.M.; Luscombe, N.M.; Lynch, M.D. What is AI? Applications of artificial intelligence to dermatology. Br. J. Dermatol. 2020, 183, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Hamet, P.; Tremblay, J. Artificial intelligence in medicine. Metabolism 2017, 69, S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Janiesch, C.; Zschech, P.; Heinrich, K. Machine learning and deep learning. Electron. Mark. 2021, 31, 685–695. [Google Scholar] [CrossRef]
- El Naqa, I.; Murphy, M.J. What is machine learning? In Machine Learning in Radiation Oncology; Springer: Cham, Switzerland, 2015; pp. 3–11. [Google Scholar] [CrossRef]
- Young, A.T.; Xiong, M.; Pfau, J.; Keiser, M.J.; Wei, M.L. Artificial intelligence in dermatology: A primer. J. Investig. Dermatol. 2020, 140, 1504–1512. [Google Scholar] [CrossRef] [PubMed]
- Choy, S.P.; Kim, B.J.; Paolino, A.; Tan, W.R.; Lim, S.M.L.; Seo, J.; Tan, S.P.; Francis, L.; Tsakok, T.; Simpson, M.; et al. Systematic review of deep learning image analyses for the diagnosis and monitoring of skin disease. NPJ Digit. Med. 2023, 6, 180. [Google Scholar] [CrossRef] [PubMed]
- AlSuwaidan, L. Deep Learning Based Classification of Dermatological Disorders. Biomed. Eng. Comput. Biol. 2023, 14, 11795972221138470. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Desrosiers, C.; Liu, X. Deep neural forest for out-of-distribution detection of skin lesion images. IEEE J. Biomed. Health Inform. 2023, 27, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Bisla, D.; Choromanska, A.; Berman, R.S.; Stein, J.A.; Polsky, D. Towards automated melanoma detection with deep learning: Data purification and augmentation. arXiv 2019, arXiv:1902.06061. [Google Scholar]
- Thieme, A.H.; Zheng, Y.; Machiraju, G.; Sadee, C.; Mittermaier, M.; Gertler, M.; Salinas, J.L.; Srinivasan, K.; Gyawali, P.; Carrillo-Perez, F.; et al. A deep-learning algorithm to classify skin lesions from mpox virus infection. Nat. Med. 2023, 29, 738–747. [Google Scholar] [CrossRef]
- Marletta, S.; L’Imperio, V.; Eccher, A.; Antonini, P.; Santonicco, N.; Girolami, I.; Dei Tos, A.P.; Sbaraglia, M.; Pagni, P.; Brunelli, M.; et al. Artificial intelligence-based tools applied to pathological diagnosis of microbiological diseases. Pathol. Res. Pract. 2023, 243, 154362. [Google Scholar] [CrossRef]
- Motulsky, H. Intuitive Biostatistics: A Nonmathematical Guide to Statistical Thinking, 3rd ed.; Oxford University Press: New York, NY, USA, 2014. [Google Scholar]
- Al-Khateeb, B. Primary health care and family physicians provide frontline care to the dermatology patients during the era of COVID-19: Recommendations and future directions. J. Family Med. Prim. Care 2020, 9, 5862. [Google Scholar] [CrossRef]
- Barroso, D.H.; Falcão, S.D.A.C.; Motta, J.D.O.C.D.; Sevilha dos Santos, L.; Takano, G.H.S.; Gomes, C.M.; Favali, C.B.F.; Lima, B.D.; Sampaio, R.N.R. PD-L1 may mediate T-cell exhaustion in a case of early diffuse leishmaniasis caused by Leishmania (L.) amazonensis. Front. Immunol. 2018, 9, 1021. [Google Scholar] [CrossRef]
- Carvalho, B.C.; Vital, T.; Osiro, J.; Gomes, C.M.; Noronha, E.; Dallago, B.; Rosa, A.C.; Carvalho, J.L.; Hagström, L.; Hecht, M.; et al. Multiparametric analysis of host and parasite elements in new world tegumentary leishmaniasis. Front. Cell. Infect. Microbiol. 2022, 12, 956112. [Google Scholar] [CrossRef]
- Zare, M.; Akbarialiabad, H.; Parsaei, H.; Asgari, Q.; Alinejad, A.; Bahreini, M.S.; Hosseini, S.H.; Ghofrani-Jahromi, M.; Shahriarirad, R.; Amirmoezzi, Y.; et al. A machine learning-based system for detecting leishmaniasis in microscopic images. BMC Infect. Dis. 2022, 22, 48. [Google Scholar] [CrossRef]
- Bolker, B.M.; Brooks, M.E.; Clark, C.J.; Geange, S.W.; Poulsen, J.R.; Stevens, M.H.H.; White, J.S.S. Generalized linear mixed models: A practical guide for ecology and evolution. Trends Ecol. Evol. 2009, 24, 127–135. [Google Scholar] [CrossRef]







| Group | Disease | n |
|---|---|---|
| Protozoosis | Cutaneous Leishmaniasis | 1787 |
| Bacterioses | Ecthyma | 55 |
| Erysipelas | 24 | |
| Impetigo | 26 | |
| Leprosy | 57 | |
| Pyodermite | 98 | |
| Tertiary syphilis | 12 | |
| Subtotal | 272 | |
| Fungal | Chromomycosis | 56 |
| Lichen planus | 18 | |
| Lichen simplex chronicus | 12 | |
| Paracoccidioidomycosis | 7 | |
| Sporotrichosis | 22 | |
| Tinea corporis | 18 | |
| Subtotal | 133 | |
| Non-infectious | Actinic keratosis | 8 |
| Basal cell carcinoma (BCC) | 31 | |
| Dermatitis | 12 | |
| Discoid lupus erythematosus (DLE) | 16 | |
| Eczema | 15 | |
| Fixed pigmentary erythema | 5 | |
| Livedoid vasculitis | 12 | |
| Lymphocytoma cutis | 8 | |
| Lymphoma | 9 | |
| Porokeratosis | 7 | |
| Psoriasis | 2 | |
| Rosacea | 3 | |
| Squamous cell carcinoma (SCC) | 40 | |
| Venous insufficiency | 98 | |
| Subtotal | 266 | |
| Grand total | 2458 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leal, J.F.d.C.; Barroso, D.H.; Trindade, N.S.; Miranda, V.L.d.; Gurgel-Gonçalves, R. Automated Identification of Cutaneous Leishmaniasis Lesions Using Deep-Learning-Based Artificial Intelligence. Biomedicines 2024, 12, 12. https://doi.org/10.3390/biomedicines12010012
Leal JFdC, Barroso DH, Trindade NS, Miranda VLd, Gurgel-Gonçalves R. Automated Identification of Cutaneous Leishmaniasis Lesions Using Deep-Learning-Based Artificial Intelligence. Biomedicines. 2024; 12(1):12. https://doi.org/10.3390/biomedicines12010012
Chicago/Turabian StyleLeal, José Fabrício de Carvalho, Daniel Holanda Barroso, Natália Santos Trindade, Vinícius Lima de Miranda, and Rodrigo Gurgel-Gonçalves. 2024. "Automated Identification of Cutaneous Leishmaniasis Lesions Using Deep-Learning-Based Artificial Intelligence" Biomedicines 12, no. 1: 12. https://doi.org/10.3390/biomedicines12010012