Omics and Multi-Omics Analysis for the Early Identification and Improved Outcome of Patients with Psoriatic Arthritis
Abstract
:1. Introduction
1.1. Psoriasis and Psoriatic Arthritis
1.2. Current Diagnostic Practices and Disease Management Strategies
1.3. The Promise of Omics and Multi-Omics Technology
2. Genomics
2.1. Brief Overview of Relevant Genomics Technologies
2.2. Applications for Early Diagnosis, Prognosis and Treatment Monitoring
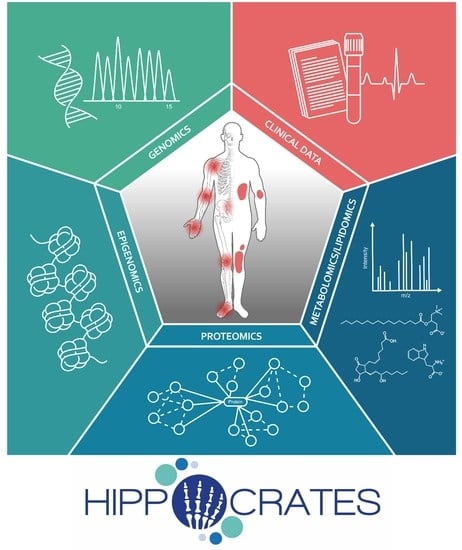
2.3. Case Studies/Examples in Psoriasis and PsA
3. Epigenomics
3.1. Brief Overview of Relevant Epigenomics Technologies
3.2. Applications for Early Diagnosis, Prognosis and Treatment Monitoring
3.3. Case Studies/Examples in Psoriasis and PsA
4. Proteomics
4.1. Brief Overview of Relevant Proteomics Technologies
4.2. Applications for Early Diagnosis, Prognosis and Treatment Monitoring
4.3. Case Studies/Examples in Psoriasis and PsA
| Gene Name | Biomarker | UniProt ID | Category | Secretion | Tissue Expression | Biological Function |
|---|---|---|---|---|---|---|
| ADIPOQ | Adiponectin | Q15848 | Lipid | Blood | Adipose tissue | ECM organization |
| APOA1 | ApoA | P02467 | Lipid | Blood | Liver | Metabolism |
| APOB | ApoB | P04114 | Lipid | Blood | Liver | Metabolism |
| CMC2 | C16ORF61 | Q9NRP2 | Skin | N/A | Non-specific | Mitochondria |
| COL2A1 | C2C | P02458 | Bone | ECM | Epididymis | Unknown function |
| CCL1 | CCL1 | P22362 | mRNA | Blood | T cells | Adaptive immune response |
| CCL20 | CCL20 | P78556 | mRNA | Blood | Smooth muscle tissue | Mixed function |
| CCL7 | CCL7 | P80098 | mRNA | Blood | Neutrophils | Humoral immune response |
| CD5L | CD5L | O43866 | Serum | Blood | Macrophages | Immune response |
| COMP | COMP | P49747 | Bone | ECM | Skin | Epidermis development |
| C9 | Complement C9 | P02748 | Serum | Blood | Liver | Hemostasis and lipid |
| COL2A1 | CPII | P02458 | Bone | ECM | Epididymis | Unknown function |
| CPN2 | CPN2 | P22792 | Skin | Blood | Liver | Hemostasis |
| CRP | CRP | P02741 | Inflammation | Blood | Liver | Hemostasis |
| COL1A1 | CTX | P02452 | Bone | ECM | Fibroblasts | ECM organization |
| CX3CL1 | CX3CL1 | P78423 | mRNA | Blood | Adipose tissue | ECM organization |
| CXCL10 | CXCL10 | P02778 | Cytokines | Blood | Immune cells | Immune response |
| CXCL12 | CXCL12 | P48061 | Skin | Blood | Fibroblasts | ECM organization |
| CXCL2 | CXCL2 | P19875 | mRNA | Blood | Liver | Metabolism |
| CXCL5 | CXCL5 | P42830 | mRNA | Blood | Salivary gland | Salivary secretion |
| DKK1 | DKK-1 | O94907 | Bone | Other | Adipose tissue | ECM organization |
| ESR1 | ESR | P03372 | Inflammation | N/A | Fibroblasts | ECM organization |
| FHL1 | FHL1 | Q13642 | Skin | N/A | Striated muscle | Muscle contraction |
| GSN | Gelsolin | P06396 | Serum | Blood | Fibroblasts | ECM organization |
| GPS1 | GPS1 | Q13098 | Skin | N/A | Non-specific | Mitochondria |
| HAT1 | HAT1 | O14929 | mRNA | N/A | Non-specific | Ribosome |
| IFI16 | IFI16 | Q16666 | Serum | N/A | Immune cells | Immune response |
| IL12A | IL-12/23 p40 | P29459 | Cytokines | Blood | Brain and skin | Unknown function |
| IL12B | IL-12/23 p40 | P29460 | Cytokines | Blood | Non-specific | Cell cycle regulation |
| IL9 | IL-12/23 p40 | P15248 | Cytokines | Blood | N/A | N/A |
| IL17A | IL-17 | Q16552 | Cell culture secretion | Blood | Immune cells | Immune response |
| IL17C | IL-17C | Q9P0M4 | mRNA | Blood | Testis | DNA repair |
| IL17F | IL-17F | Q96PD4 | mRNA | Blood | B cells | Humoral immune response |
| IL2 | IL-2 | P60568 | Cell culture secretion | Blood | N/A | N/A |
| IL23 | IL-23 | Q9NPF7 | Cytokines | Blood | B cells | Humoral immune response |
| IL23R | IL23R | Q5VWK5 | Skin | N/A | Intestine | Brush border |
| IL3 | IL-3 | P08700 | mRNA | Blood | N/A | N/A |
| IL33 | IL-33 | O95760 | Cytokines | Blood | Fibroblasts | ECM organization |
| IL34 | IL-34 | Q6ZMJ4 | Cytokines | Blood | Macrophages | Immune response |
| EBI3 | IL-35 | Q14213 | Cytokines | Blood | Placenta | Pregnancy |
| IL12A | IL-35 | P29459 | Cytokines | Blood | Brain and skin | Unknown function |
| IL36A | IL-36a | Q9UHA7 | Cytokines | Blood | Esophagus | Epithelial cell function |
| IL1F10 | IL-38 | Q8WWZ1 | Cytokines | Blood | Skin | Cornification |
| IL6 | IL-6 | P05231 | Cytokines, mRNA | Blood | Adipose tissue | ECM organization |
| CXCL8 | IL-8 | P10145 | mRNA | Blood | Neutrophils | Humoral immune response |
| INS | Insulin | P01308 | Lipid | Blood | Pancreas | Digestion |
| ISG20 | ISG20 | Q96AZ6 | mRNA | N/A | Immune cells | Immune response |
| ITGB5 | ITGB5 | P18084 | Serum | N/A | Adipose tissue | ECM organization |
| ITGB5 | ITGB5 | P18084 | Skin | N/A | Adipose tissue | ECM organization |
| KRT17 | K17 | Q04695 | Serum | N/A | Skin | Epidermis development |
| LEP | Leptin | P41159 | Lipid | Blood | Adipose tissue | ECM organization |
| LGALS3BP | M2BP | Q08380 | Serum | Blood | Stomach | Digestion |
| CSF1 | M-CSF | P09603 | Cytokines | Blood | Non-specific | Angiogenesis |
| MMP3 | MMP3 | P08254 | Bone, mRNA | ECM | Salivary gland | Salivary secretion |
| MPO | MPO | P05164 | Serum | Membrane | Neutrophils | Humoral immune response |
| NOTCH2NLA | NOTCH2NL | Q7Z3S9 | mRNA | Blood | Testis | DNA repair |
| TNFRSF11B | OPG | O00300 | Bone | Other | Kidney | Transmembrane transport |
| POSTN | POSTN | Q15063 | Skin | ECM | Skin | Epidermis development |
| PTPA | PPP2R4 | Q15257 | Skin | N/A | Non-specific | Mitochondria |
| PRL | PRL | P01236 | Serum | Blood | Pituitary gland | Hormone signaling |
| TNFSF11 | RANKL | O14788 | Bone | Blood | Immune cells | Immune response |
| SETD2 | SETD2 | Q9BYW2 | mRNA | N/A | Non-specific | Transcription |
| IL2RA | sIL2R | P01589 | Serum | N/A | Immune cells | Immune response |
| IL2RB | sIL2R | P14784 | Serum | N/A | Immune cells | Immune response |
| IL2RG | sIL2R | P31785 | Serum | N/A | T cells | Adaptive immune response |
| SNCA | SNCA | P37840 | Skin | Membrane | Brain and bone marrow | Chromatin organization |
| SRP14 | SRP14 | P37108 | Skin | N/A | Non-specific | Mitochondria |
| SRPX | SRPX | P78539 | Skin | Unknown | Adipose tissue | ECM organization |
| STAT3 | STAT3 | P40763 | mRNA | N/A | Non-specific | Mitochondria and proteasome |
| STAT6 | STAT6 | P42226 | mRNA | N/A | Macrophages | Immune response |
| STIP1 | STIP1 | P31948 | Serum | N/A | Non-specific | Unknown function |
| SYK | SYK | P43405 | mRNA | N/A | Non-specific | Transcription |
| TBX21 | TBX21 | Q9UL17 | mRNA | N/A | Immune cells | Immune response |
| TNF | TNF-alpha | P01375 | Cytokines | Blood | Neutrophils | Inflammatory response |
| VCP | VCP | P55072 | Serum | N/A | Non-specific | Mitochondria |
| FLT4 | VEGFR-3 | P35916 | Serum | Blood | Non-specific | Transcription |
| CHI3L1 | YKL-40 | P36222 | Serum | Blood | Liver | Metabolism |
5. Metabolomics
5.1. Brief Overview of Relevant Metabolomics Technologies
5.2. Applications for Early Diagnosis, Prognosis and Treatment Monitoring
5.3. Case Studies/Examples in Psoriasis and PsA
6. Lipidomics
6.1. Brief Overview of Relevant Lipidomics Technologies
6.2. Applications for Early Diagnosis, Prognosis and Treatment Monitoring
6.3. Case Studies/Examples in Psoriasis and PsA
7. Complementary Technologies—Multiple Sequential Immunohistochemistry
8. Data Management/Integration and Artificial Intelligence
9. The Advantage of Multi-Omics Evaluation
10. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Damiani, G.; Bragazzi, N.L.; Karimkhani Aksut, C.; Wu, D.; Alicandro, G.; McGonagle, D.; Guo, C.; Dellavalle, R.; Grada, A.; Wong, P.; et al. The Global, Regional, and National Burden of Psoriasis: Results and Insights from the Global Burden of Disease 2019 Study. Front. Med. 2021, 8, 743180. [Google Scholar] [CrossRef]
- Armstrong, A.W.; Read, C. Pathophysiology, Clinical Presentation, and Treatment of Psoriasis: A Review. JAMA 2020, 323, 1945–1960. [Google Scholar] [CrossRef] [PubMed]
- Ritchlin, C.T.; Colbert, R.A.; Gladman, D.D. Psoriatic Arthritis. N. Engl. J. Med. 2017, 376, 957–970. [Google Scholar] [CrossRef] [PubMed]
- Simon, D.; Watad, A.; Rodrigues-Manica, S.; Perricone, C. Editorial: Early Origins of Psoriatic Arthritis. Front. Med. 2021, 8, 794229. [Google Scholar] [CrossRef]
- Kumthekar, A.; Ogdie, A. Obesity and Psoriatic Arthritis: A Narrative Review. Rheumatol. Ther. 2020, 7, 447–456. [Google Scholar] [CrossRef]
- Ogdie, A.; Harrison, R.W.; McLean, R.R.; Lin, T.-C.; Lebwohl, M.; Strober, B.E.; Zhuo, J.; Patel, V.; Mease, P.J. Prospective Cohort Study of Psoriatic Arthritis Risk in Patients With Psoriasis in a Real-World Psoriasis Registry. J. Am. Acad. Dermatol. 2022; in press. [Google Scholar] [CrossRef]
- Gisondi, P.; Bellinato, F.; Maurelli, M.; Geat, D.; Zabotti, A.; McGonagle, D.; Girolomoni, G. Reducing the Risk of Developing Psoriatic Arthritis in Patients with Psoriasis. Psoriasis 2022, 12, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Pezzolo, E.; Naldi, L. The relationship between smoking, psoriasis and psoriatic arthritis. Expert Rev. Clin. Immunol. 2019, 15, 41–48. [Google Scholar] [CrossRef]
- Owczarczyk-Saczonek, A.; Purzycka-Bohdan, D.; Nedoszytko, B.; Reich, A.; Szczerkowska-Dobosz, A.; Bartosiñska, J.; Batycka-Baran, A.; Czajkowski, R.; Dobrucki, I.T.; Dobrucki, L.W.; et al. Pathogenesis of psoriasis in the “omic” era. Part III. Metabolic disorders, metabolomics, nutrigenomics in psoriasis. Postepy Dermatol. Alergol. 2020, 37, 452–467. [Google Scholar] [CrossRef]
- Kocic, H.; Damiani, G.; Stamenkovic, B.; Tirant, M.; Jovic, A.; Tiodorovic, D.; Peris, K. Dietary compounds as potential modulators of microRNA expression in psoriasis. Ther. Adv. Chronic Dis. 2019, 10, 2040622319864805. [Google Scholar] [CrossRef] [Green Version]
- Scher, J.U.; Ogdie, A.; Merola, J.F.; Ritchlin, C. Preventing psoriatic arthritis: Focusing on patients with psoriasis at increased risk of transition. Nat. Rev. Rheumatol. 2019, 15, 153–166. [Google Scholar] [CrossRef]
- Ogdie, A.; Schwartzman, S.; Husni, M.E. Recognizing and managing comorbidities in psoriatic arthritis. Curr. Opin. Rheumatol. 2015, 27, 118–126. [Google Scholar] [CrossRef]
- Weigle, N.; McBane, S. Psoriasis. Am. Fam. Physician 2013, 87, 626–633. [Google Scholar]
- Raychaudhuri, S.K.; Maverakis, E.; Raychaudhuri, S.P. Diagnosis and classification of psoriasis. Autoimmun. Rev. 2014, 13, 490–495. [Google Scholar] [CrossRef]
- Johnson, M.A.N.; Armstrong, A.W. Clinical and histologic diagnostic guidelines for psoriasis: A critical review. Clin. Rev. Allergy Immunol. 2013, 44, 166–172. [Google Scholar] [CrossRef]
- Pennington, S.R.; FitzGerald, O. Early Origins of Psoriatic Arthritis: Clinical, Genetic and Molecular Biomarkers of Progression from Psoriasis to Psoriatic Arthritis. Front. Med. 2021, 8, 723944. [Google Scholar] [CrossRef]
- Raychaudhuri, S.P.; Wilken, R.; Sukhov, A.C.; Raychaudhuri, S.K.; Maverakis, E. Management of psoriatic arthritis: Early diagnosis, monitoring of disease severity and cutting edge therapies. J. Autoimmun. 2017, 76, 21–37. [Google Scholar] [CrossRef]
- Ghasemi, M.; Nabipour, I.; Omrani, A.; Alipour, Z.; Assadi, M. Precision medicine and molecular imaging: New targeted approaches toward cancer therapeutic and diagnosis. Am. J. Nucl. Med. Mol. Imaging 2016, 6, 310–327. [Google Scholar]
- Vargas, A.J.; Harris, C.C. Biomarker development in the precision medicine era: Lung cancer as a case study. Nat. Rev. Cancer 2016, 16, 525–537. [Google Scholar] [CrossRef]
- Grivas, A.; Fragoulis, G.; Garantziotis, P.; Banos, A.; Nikiphorou, E.; Boumpas, D. Unraveling the complexities of psoriatic arthritis by the use of -Omics and their relevance for clinical care. Autoimmun. Rev. 2021, 20, 102949. [Google Scholar] [CrossRef]
- Caputo, V.; Strafella, C.; Termine, A.; Dattola, A.; Mazzilli, S.; Lanna, C.; Cosio, T.; Campione, E.; Novelli, G.; Giardina, E.; et al. Overview of the molecular determinants contributing to the expression of Psoriasis and Psoriatic Arthritis phenotypes. J. Cell. Mol. Med. 2020, 24, 13554–13563. [Google Scholar] [CrossRef]
- Generali, E.; Scirè, C.A.; Favalli, E.G.; Selmi, C. Biomarkers in psoriatic arthritis: A systematic literature review. Expert Rev. Clin. Immunol. 2016, 12, 651–660. [Google Scholar] [CrossRef] [Green Version]
- O’Rielly, D.D.; Jani, M.; Rahman, P.; Elder, J.T. The Genetics of Psoriasis and Psoriatic Arthritis. J. Rheumatol. Suppl. 2019, 95, 46–50. [Google Scholar] [CrossRef]
- Shi, C.; Rattray, M.; Barton, A.; Bowes, J.; Orozco, G. Using functional genomics to advance the understanding of psoriatic arthritis. Rheumatology 2020, 59, 3137–3146. [Google Scholar] [CrossRef]
- Bowes, J.; Loehr, S.; Budu-Aggrey, A.; Uebe, S.; Bruce, I.N.; Feletar, M.; Marzo-Ortega, H.; Helliwell, P.; Ryan, A.W.; Kane, D.; et al. PTPN22 is associated with susceptibility to psoriatic arthritis but not psoriasis: Evidence for a further PsA-specific risk locus. Ann. Rheum. Dis. 2015, 74, 1882–1885. [Google Scholar] [CrossRef]
- Cortes, A.; Brown, M.A. Promise and pitfalls of the Immunochip. Arthritis Res. Ther. 2011, 13, 101. [Google Scholar] [CrossRef]
- Budu-Aggrey, A.; Bowes, J.; Barton, A. Identifying a novel locus for psoriatic arthritis. Rheumatology 2016, 55, 25–32. [Google Scholar] [CrossRef]
- Ramírez, J.; Fernández-Sueiro, J.L.; López-Mejías, R.; Montilla, C.; Arias, M.; Moll, C.; Alsina, M.; Sanmarti, R.; Lozano, F.; Cañete, J.D. FCGR2A/CD32A and FCGR3A/CD16A variants and EULAR response to tumor necrosis factor-α blockers in psoriatic arthritis: A longitudinal study with 6 months of followup. J. Rheumatol. 2012, 39, 1035–1041. [Google Scholar] [CrossRef]
- Bowes, J.; Ashcroft, J.; Dand, N.; Jalali-Najafabadi, F.; Bellou, E.; Ho, P.; Marzo-Ortega, H.; Helliwell, P.S.; Feletar, M.; Ryan, A.W.; et al. Cross-phenotype association mapping of the MHC identifies genetic variants that differentiate psoriatic arthritis from psoriasis. Ann. Rheum. Dis. 2017, 76, 1774–1779. [Google Scholar] [CrossRef]
- Okada, Y.; Han, B.; Tsoi, L.C.; Stuart, P.E.; Ellinghaus, E.; Tejasvi, T.; Chandran, V.; Pellett, F.; Pollock, R.; Bowcock, A.M.; et al. Fine mapping major histocompatibility complex associations in psoriasis and its clinical subtypes. Am. J. Hum. Genet. 2014, 95, 162–172. [Google Scholar] [CrossRef]
- O’Rielly, D.D.; Rahman, P. Genetic, Epigenetic and Pharmacogenetic Aspects of Psoriasis and Psoriatic Arthritis. Rheum. Dis. Clin. N. Am. 2015, 41, 623–642. [Google Scholar] [CrossRef]
- Bowes, J.; Budu-Aggrey, A.; Huffmeier, U.; Uebe, S.; Steel, K.; Hebert, H.L.; Wallace, C.; Massey, J.; Bruce, I.N.; Bluett, J.; et al. Dense genotyping of immune-related susceptibility loci reveals new insights into the genetics of psoriatic arthritis. Nat. Commun. 2015, 6, 6046. [Google Scholar] [CrossRef] [Green Version]
- Budu-Aggrey, A.; Bowes, J.; Loehr, S.; Uebe, S.; Zervou, M.I.; Helliwell, P.; Ryan, A.W.; Kane, D.; Korendowych, E.; Giardina, E.; et al. Replication of a distinct psoriatic arthritis risk variant at the IL23R locus. Ann. Rheum. Dis. 2016, 75, 1417–1418. [Google Scholar] [CrossRef]
- Stuart, P.E.; Nair, R.P.; Tsoi, L.C.; Tejasvi, T.; Das, S.; Kang, H.M.; Ellinghaus, E.; Chandran, V.; Callis-Duffin, K.; Ike, R.; et al. Genome-wide Association Analysis of Psoriatic Arthritis and Cutaneous Psoriasis Reveals Differences in Their Genetic Architecture. Am. J. Hum. Genet. 2015, 97, 816–836. [Google Scholar] [CrossRef]
- Chandran, V.; Bull, S.B.; Pellett, F.J.; Ayearst, R.; Pollock, R.A.; Gladman, D.D. Killer-cell immunoglobulin-like receptor gene polymorphisms and susceptibility to psoriatic arthritis. Rheumatology 2014, 53, 233–239. [Google Scholar] [CrossRef]
- Cascella, R.; Strafella, C.; Ragazzo, M.; Manzo, L.; Costanza, G.; Bowes, J.; Hüffmeier, U.; Potenza, S.; Sangiuolo, F.; Reis, A.; et al. KIF3A and IL-4 are disease-specific biomarkers for psoriatic arthritis susceptibility. Oncotarget 2017, 8, 95401–95411. [Google Scholar] [CrossRef]
- Aterido, A.; Cañete, J.D.; Tornero, J.; Ferrándiz, C.; Pinto, J.A.; Gratacós, J.; Queiró, R.; Montilla, C.; Torre-Alonso, J.C.; Pérez-Venegas, J.J.; et al. Genetic variation at the glycosaminoglycan metabolism pathway contributes to the risk of psoriatic arthritis but not psoriasis. Ann. Rheum. Dis. 2019, 78, 355–364. [Google Scholar] [CrossRef]
- Barski, A.; Cuddapah, S.; Cui, K.; Roh, T.-Y.; Schones, D.E.; Wang, Z.; Wei, G.; Chepelev, I.; Zhao, K. High-resolution profiling of histone methylations in the human genome. Cell 2007, 129, 823–837. [Google Scholar] [CrossRef]
- Park, P.J. ChIP-seq: Advantages and challenges of a maturing technology. Nat. Rev. Genet. 2009, 10, 669–680. [Google Scholar] [CrossRef]
- Schadt, E.E.; Banerjee, O.; Fang, G.; Feng, Z.; Wong, W.H.; Zhang, X.; Kislyuk, A.; Clark, T.A.; Luong, K.; Keren-Paz, A.; et al. Modeling kinetic rate variation in third generation DNA sequencing data to detect putative modifications to DNA bases. Genome Res. 2013, 23, 129–141. [Google Scholar] [CrossRef]
- Zhang, Z.; Pugh, B.F. High-resolution genome-wide mapping of the primary structure of chromatin. Cell 2011, 144, 175–186. [Google Scholar] [CrossRef]
- Merelli, I.; Tordini, F.; Drocco, M.; Aldinucci, M.; Liò, P.; Milanesi, L. Integrating multi-omic features exploiting Chromosome Conformation Capture data. Front. Genet. 2015, 6, 40. [Google Scholar] [CrossRef] [Green Version]
- Carini, C.; Hunter, E.; Ramadass, A.S.; Green, J.; Akoulitchev, A.; McInnes, I.B.; Goodyear, C.S. Chromosome conformation signatures define predictive markers of inadequate response to methotrexate in early rheumatoid arthritis. J. Transl. Med. 2018, 16, 18. [Google Scholar] [CrossRef]
- Hunter, E.; Dezfouli, M.; Koutsothanasi, C.; Wilson, A.; Santos, F.C.; Salter, M.; Westra, J.W.; Powell, R.; Dring, A.; Egan, B.; et al. Development and validation of blood-based predictive biomarkers for response to PD-(L)-1 checkpoint inhibitors: Evidence of a universal systemic core of 3D immunogenetic profiling across multiple oncological indications. medRxiv 2021. [Google Scholar] [CrossRef]
- Hunter, E.; Koutsothanasi, C.; Wilson, A.; Santos, F.C.; Salter, M.; Powell, R.; Dring, A.; Brajer, P.; Egan, B.; Westra, J.W.; et al. 3D genomic capture of regulatory immuno-genetic profiles in COVID-19 patients for prognosis of severe COVID disease outcome. bioRxiv 2021. [Google Scholar] [CrossRef]
- Tordini, F.; Aldinucci, M.; Milanesi, L.; Liò, P.; Merelli, I. The Genome Conformation as an Integrator of Multi-Omic Data: The Example of Damage Spreading in Cancer. Front. Genet. 2016, 7, 194. [Google Scholar] [CrossRef]
- Mahendran, S.M.; Chandran, V. Exploring the Psoriatic Arthritis Proteome in Search of Novel Biomarkers. Proteomes 2018, 6, 5. [Google Scholar] [CrossRef]
- Qi, F.; Tan, Y.; Yao, A.; Yang, X.; He, Y. Psoriasis to Psoriatic Arthritis: The Application of Proteomics Technologies. Front. Med. 2021, 8, 681172. [Google Scholar] [CrossRef]
- Mc Ardle, A.; Kwasnik, A.; Szentpetery, A.; Hernandez, B.; Parnell, A.; de Jager, W.; de Roock, S.; FitzGerald, O.; Pennington, S.R. Identification and Evaluation of Serum Protein Biomarkers That Differentiate Psoriatic Arthritis From Rheumatoid Arthritis. Arthritis Rheumatol. 2022, 74, 81–91. [Google Scholar] [CrossRef]
- Adhikari, S.; Nice, E.C.; Deutsch, E.W.; Lane, L.; Omenn, G.S.; Pennington, S.R.; Paik, Y.-K.; Overall, C.M.; Corrales, F.J.; Cristea, I.M.; et al. A high-stringency blueprint of the human proteome. Nat. Commun. 2020, 11, 5301. [Google Scholar] [CrossRef]
- Bateman, N.W.; Goulding, S.P.; Shulman, N.J.; Gadok, A.K.; Szumlinski, K.K.; MacCoss, M.J.; Wu, C.C. Maximizing peptide identification events in proteomic workflows using data-dependent acquisition (DDA). Mol. Cell. Proteom. 2014, 13, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, C.; Gillet, L.; Rosenberger, G.; Amon, S.; Collins, B.C.; Aebersold, R. Data-independent acquisition-based SWATH-MS for quantitative proteomics: A tutorial. Mol. Syst. Biol. 2018, 14, e8126. [Google Scholar] [CrossRef] [PubMed]
- Suhre, K.; McCarthy, M.I.; Schwenk, J.M. Genetics meets proteomics: Perspectives for large population-based studies. Nat. Rev. Genet. 2021, 22, 19–37. [Google Scholar] [CrossRef]
- Zhong, W.; Edfors, F.; Gummesson, A.; Bergström, G.; Fagerberg, L.; Uhlén, M. Next generation plasma proteome profiling to monitor health and disease. Nat. Commun. 2021, 12, 2493. [Google Scholar] [CrossRef]
- Petrera, A.; von Toerne, C.; Behler, J.; Huth, C.; Thorand, B.; Hilgendorff, A.; Hauck, S.M. Multiplatform Approach for Plasma Proteomics: Complementarity of Olink Proximity Extension Assay Technology to Mass Spectrometry-Based Protein Profiling. J. Proteome Res. 2021, 20, 751–762. [Google Scholar] [CrossRef] [PubMed]
- Pietzner, M.; Wheeler, E.; Carrasco-Zanini, J.; Cortes, A.; Koprulu, M.; Wörheide, M.A.; Oerton, E.; Cook, J.; Stewart, I.D.; Kerrison, N.D.; et al. Mapping the proteo-genomic convergence of human diseases. Science 2021, 374, eabj1541. [Google Scholar] [CrossRef] [PubMed]
- Ignjatovic, V.; Geyer, P.E.; Palaniappan, K.K.; Chaaban, J.E.; Omenn, G.S.; Baker, M.S.; Deutsch, E.W.; Schwenk, J.M. Mass Spectrometry-Based Plasma Proteomics: Considerations from Sample Collection to Achieving Translational Data. J. Proteome Res. 2019, 18, 4085–4097. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, E.W.; Omenn, G.S.; Sun, Z.; Maes, M.; Pernemalm, M.; Palaniappan, K.K.; Letunica, N.; Vandenbrouck, Y.; Brun, V.; Tao, S.-C.; et al. Advances and Utility of the Human Plasma Proteome. J. Proteome Res. 2021, 20, 5241–5263. [Google Scholar] [CrossRef] [PubMed]
- Uhlén, M.; Karlsson, M.J.; Hober, A.; Svensson, A.-S.; Scheffel, J.; Kotol, D.; Zhong, W.; Tebani, A.; Strandberg, L.; Edfors, F.; et al. The human secretome. Sci. Signal. 2019, 12, 609. [Google Scholar] [CrossRef]
- Tebani, A.; Gummesson, A.; Zhong, W.; Koistinen, I.S.; Lakshmikanth, T.; Olsson, L.M.; Boulund, F.; Neiman, M.; Stenlund, H.; Hellström, C.; et al. Integration of molecular profiles in a longitudinal wellness profiling cohort. Nat. Commun. 2020, 11, 4487. [Google Scholar] [CrossRef]
- Cretu, D.; Gao, L.; Liang, K.; Soosaipillai, A.; Diamandis, E.P.; Chandran, V. Differentiating Psoriatic Arthritis From Psoriasis Without Psoriatic Arthritis Using Novel Serum Biomarkers. Arthritis Care Res. 2018, 70, 454–461. [Google Scholar] [CrossRef]
- Cretu, D.; Liang, K.; Saraon, P.; Batruch, I.; Diamandis, E.P.; Chandran, V. Quantitative tandem mass-spectrometry of skin tissue reveals putative psoriatic arthritis biomarkers. Clin. Proteom. 2015, 12, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Dalmády, S.; Kiss, M.; Képíró, L.; Kovács, L.; Sonkodi, G.; Kemény, L.; Gyulai, R. Higher levels of autoantibodies targeting mutated citrullinated vimentin in patients with psoriatic arthritis than in patients with psoriasis vulgaris. Clin. Dev. Immunol. 2013, 2013, 474028. [Google Scholar] [CrossRef]
- Hansson, C.; Eriksson, C.; Alenius, G.-M. S-calprotectin (S100A8/S100A9): A potential marker of inflammation in patients with psoriatic arthritis. J. Immunol. Res. 2014, 2014, 696415. [Google Scholar] [CrossRef] [PubMed]
- Alenius, G.-M.; Eriksson, C.; Rantapää Dahlqvist, S. Interleukin-6 and soluble interleukin-2 receptor alpha-markers of inflammation in patients with psoriatic arthritis? Clin. Exp. Rheumatol. 2009, 27, 120–123. [Google Scholar] [PubMed]
- Abji, F.; Pollock, R.A.; Liang, K.; Chandran, V.; Gladman, D.D. Brief Report: CXCL10 Is a Possible Biomarker for the Development of Psoriatic Arthritis among Patients with Psoriasis. Arthritis Rheumatol. 2016, 68, 2911–2916. [Google Scholar] [CrossRef]
- Grazio, S.; Razdorov, G.; Erjavec, I.; Grubisic, F.; Kusic, Z.; Punda, M.; Anticevic, D.; Vukicevic, S.; Grgurevic, L. Differential expression of proteins with heparin affinity in patients with rheumatoid and psoriatic arthritis: A preliminary study. Clin. Exp. Rheumatol. 2013, 31, 665–671. [Google Scholar] [PubMed]
- Chandran, V.; Shen, H.; Pollock, R.A.; Pellett, F.J.; Carty, A.; Cook, R.J.; Gladman, D.D. Soluble biomarkers associated with response to treatment with tumor necrosis factor inhibitors in psoriatic arthritis. J. Rheumatol. 2013, 40, 866–871. [Google Scholar] [CrossRef]
- Fiocco, U.; Sfriso, P.; Oliviero, F.; Roux-Lombard, P.; Scagliori, E.; Cozzi, L.; Lunardi, F.; Calabrese, F.; Vezzù, M.; Dainese, S.; et al. Synovial effusion and synovial fluid biomarkers in psoriatic arthritis to assess intraarticular tumor necrosis factor-α blockade in the knee joint. Arthritis Res. Ther. 2010, 12, R148. [Google Scholar] [CrossRef] [PubMed]
- van Kuijk, A.W.R.; DeGroot, J.; Koeman, R.C.; Sakkee, N.; Baeten, D.L.; Gerlag, D.M.; Tak, P.P. Soluble biomarkers of cartilage and bone metabolism in early proof of concept trials in psoriatic arthritis: Effects of adalimumab versus placebo. PLoS ONE 2010, 5, e12556. [Google Scholar] [CrossRef]
- Collins, E.S.; Butt, A.Q.; Gibson, D.S.; Dunn, M.J.; Fearon, U.; van Kuijk, A.W.; Gerlag, D.M.; Pontifex, E.; Veale, D.J.; Tak, P.P.; et al. A clinically based protein discovery strategy to identify potential biomarkers of response to anti-TNF-α treatment of psoriatic arthritis. Proteom. Clin. Appl. 2016, 10, 645–662. [Google Scholar] [CrossRef]
- Mahendran, S.M.; Keystone, E.C.; Krawetz, R.J.; Liang, K.; Diamandis, E.P.; Chandran, V. Elucidating the endogenous synovial fluid proteome and peptidome of inflammatory arthritis using label-free mass spectrometry. Clin. Proteom. 2019, 16, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulder, M.L.M.; van Hal, T.W.; Wenink, M.H.; Koenen, H.J.P.M.; van den Hoogen, F.H.J.; de Jong, E.M.G.J.; van den Reek, J.M.P.A.; Vriezekolk, J.E. Clinical, laboratory, and genetic markers for the development or presence of psoriatic arthritis in psoriasis patients: A systematic review. Arthritis Res. Ther. 2021, 23, 168. [Google Scholar] [CrossRef]
- Leijten, E.; Tao, W.; Pouw, J.; van Kempen, T.; Olde Nordkamp, M.; Balak, D.; Tekstra, J.; Muñoz-Elías, E.; DePrimo, S.; Drylewicz, J.; et al. Broad proteomic screen reveals shared serum proteomic signature in patients with psoriatic arthritis and psoriasis without arthritis. Rheumatology 2021, 60, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, M.; Zhang, C.; Méar, L.; Zhong, W.; Digre, A.; Katona, B.; Sjöstedt, E.; Butler, L.; Odeberg, J.; Dusart, P.; et al. A single-cell type transcriptomics map of human tissues. Sci. Adv. 2021, 7, eabh2169. [Google Scholar] [CrossRef] [PubMed]
- Wishart, D.S. Metabolomics for Investigating Physiological and Pathophysiological Processes. Physiol. Rev. 2019, 99, 1819–1875. [Google Scholar] [CrossRef] [PubMed]
- López-López, Á.; López-Gonzálvez, Á.; Barker-Tejeda, T.C.; Barbas, C. A review of validated biomarkers obtained through metabolomics. Expert Rev. Mol. Diagn. 2018, 18, 557–575. [Google Scholar] [CrossRef]
- Di, Y.; Afifi, L.; Jeon, C.; Trivedi, M.; Chang, H.W.; Lee, K.; Liao, W. The metabolomics of psoriatic disease. Psoriasis 2017, 7, 1–15. [Google Scholar] [CrossRef]
- Koussiouris, J.; Looby, N.; Anderson, M.; Kulasingam, V.; Chandran, V. Metabolomics Studies in Psoriatic Disease: A Review. Metabolites 2021, 11, 375. [Google Scholar] [CrossRef] [PubMed]
- Dorochow, E.; Köhm, M.; Hahnefeld, L.; Gurke, R. Metabolic Profiling in Rheumatoid Arthritis, Psoriatic Arthritis, and Psoriasis: Elucidating Pathogenesis, Improving Diagnosis, and Monitoring Disease Activity. J. Pers. Med. 2022, 12, 924. [Google Scholar] [CrossRef]
- Madsen, R.K.; Lundstedt, T.; Gabrielsson, J.; Sennbro, C.-J.; Alenius, G.-M.; Moritz, T.; Rantapää-Dahlqvist, S.; Trygg, J. Diagnostic properties of metabolic perturbations in rheumatoid arthritis. Arthritis Res. Ther. 2011, 13, R19. [Google Scholar] [CrossRef] [PubMed]
- Souto-Carneiro, M.; Tóth, L.; Behnisch, R.; Urbach, K.; Klika, K.D.; Carvalho, R.A.; Lorenz, H.-M. Differences in the serum metabolome and lipidome identify potential biomarkers for seronegative rheumatoid arthritis versus psoriatic arthritis. Ann. Rheum. Dis. 2020, 79, 499–506. [Google Scholar] [CrossRef] [Green Version]
- Armstrong, A.W.; Wu, J.; Johnson, M.A.; Grapov, D.; Azizi, B.; Dhillon, J.; Fiehn, O. Metabolomics in psoriatic disease: Pilot study reveals metabolite differences in psoriasis and psoriatic arthritis. F1000Research 2014, 3, 248. [Google Scholar] [CrossRef]
- Coras, R.; Kavanaugh, A.; Boyd, T.; Huynh, D.; Lagerborg, K.A.; Xu, Y.-J.; Rosenthal, S.B.; Jain, M.; Guma, M. Choline metabolite, trimethylamine N-oxide (TMAO), is associated with inflammation in psoriatic arthritis. Clin. Exp. Rheumatol. 2019, 37, 481–484. [Google Scholar]
- Paine, A.; Brookes, P.S.; Bhattacharya, S.; Li, D.; La Garcia-Hernandez, M.D.L.; Tausk, F.; Ritchlin, C. Dysregulation of bile acids, lipids, and nucleotides in psoriatic arthritis revealed by unbiased profiling of serum metabolites. Arthritis Rheumatol. 2022. [Google Scholar] [CrossRef]
- Wang, N.; Yang, L.; Shang, L.; Liang, Z.; Wang, Y.; Feng, M.; Yu, S.; Li, X.; Gao, C.; Li, Z.; et al. Altered Fecal Metabolomics and Potential Biomarkers of Psoriatic Arthritis Differing From Rheumatoid Arthritis. Front. Immunol. 2022, 13, 812996. [Google Scholar] [CrossRef]
- Alonso, A.; Julià, A.; Vinaixa, M.; Domènech, E.; Fernández-Nebro, A.; Cañete, J.D.; Ferrándiz, C.; Tornero, J.; Gisbert, J.P.; Nos, P.; et al. Urine metabolome profiling of immune-mediated inflammatory diseases. BMC Med. 2016, 14, 133. [Google Scholar] [CrossRef]
- Kapoor, S.R.; Filer, A.; Fitzpatrick, M.A.; Fisher, B.A.; Taylor, P.C.; Buckley, C.D.; McInnes, I.B.; Raza, K.; Young, S.P. Metabolic profiling predicts response to anti-tumor necrosis factor α therapy in patients with rheumatoid arthritis. Arthritis Rheum. 2013, 65, 1448–1456. [Google Scholar] [CrossRef]
- Maceyka, M.; Spiegel, S. Sphingolipid metabolites in inflammatory disease. Nature 2014, 510, 58–67. [Google Scholar] [CrossRef]
- Dennis, E.A.; Norris, P.C. Eicosanoid storm in infection and inflammation. Nat. Rev. Immunol. 2015, 15, 511–523. [Google Scholar] [CrossRef]
- Serhan, C.N. Discovery of specialized pro-resolving mediators marks the dawn of resolution physiology and pharmacology. Mol. Aspects Med. 2017, 58, 1–11. [Google Scholar] [CrossRef]
- Zhang, C.; Wang, K.; Yang, L.; Liu, R.; Chu, Y.; Qin, X.; Yang, P.; Yu, H. Lipid metabolism in inflammation-related diseases. Analyst 2018, 143, 4526–4536. [Google Scholar] [CrossRef]
- Lin, D.A.; Boyce, J.A. Lysophospholipids as Mediators of Immunity. Adv. Immunol. 2006, 89, 141–167. [Google Scholar] [CrossRef]
- Brouwers, H.; von Hegedus, J.; Toes, R.; Kloppenburg, M.; Ioan-Facsinay, A. Lipid mediators of inflammation in rheumatoid arthritis and osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2015, 29, 741–755. [Google Scholar] [CrossRef]
- Fan, F.; Mundra, P.A.; Fang, L.; Galvin, A.; Moore, X.L.; Weir, J.M.; Wong, G.; White, D.A.; Chin-Dusting, J.; Sparrow, M.P.; et al. Lipidomic Profiling in Inflammatory Bowel Disease: Comparison Between Ulcerative Colitis and Crohn’s Disease. Inflamm. Bowel Dis. 2015, 21, 1511–1518. [Google Scholar] [CrossRef]
- Schwanke, R.C.; Marcon, R.; Bento, A.F.; Calixto, J.B. EPA- and DHA-derived resolvins’ actions in inflammatory bowel disease. Eur. J. Pharmacol. 2016, 785, 156–164. [Google Scholar] [CrossRef]
- Scoville, E.A.; Allaman, M.M.; Brown, C.T.; Motley, A.K.; Horst, S.N.; Williams, C.S.; Koyama, T.; Zhao, Z.; Adams, D.W.; Beaulieu, D.B.; et al. Alterations in Lipid, Amino Acid, and Energy Metabolism Distinguish Crohn’s Disease from Ulcerative Colitis and Control Subjects by Serum Metabolomic Profiling. Metabolomics 2018, 14, 17. [Google Scholar] [CrossRef]
- Grill, M.; Högenauer, C.; Blesl, A.; Haybaeck, J.; Golob-Schwarzl, N.; Ferreirós, N.; Thomas, D.; Gurke, R.; Trötzmüller, M.; Köfeler, H.C.; et al. Members of the endocannabinoid system are distinctly regulated in inflammatory bowel disease and colorectal cancer. Sci. Rep. 2019, 9, 2358. [Google Scholar] [CrossRef]
- Bazarganipour, S.; Hausmann, J.; Oertel, S.; El-Hindi, K.; Brachtendorf, S.; Blumenstein, I.; Kubesch, A.; Sprinzl, K.; Birod, K.; Hahnefeld, L.; et al. The Lipid Status in Patients with Ulcerative Colitis: Sphingolipids are Disease-Dependent Regulated. J. Clin. Med. 2019, 8, 971. [Google Scholar] [CrossRef]
- Zeng, C.; Wen, B.; Hou, G.; Lei, L.; Mei, Z.; Jia, X.; Chen, X.; Zhu, W.; Li, J.; Kuang, Y.; et al. Lipidomics profiling reveals the role of glycerophospholipid metabolism in psoriasis. Gigascience 2017, 6, 1–11. [Google Scholar] [CrossRef]
- Sorokin, A.V.; Norris, P.C.; English, J.T.; Dey, A.K.; Chaturvedi, A.; Baumer, Y.; Silverman, J.; Playford, M.P.; Serhan, C.N.; Mehta, N.N. Identification of proresolving and inflammatory lipid mediators in human psoriasis. J. Clin. Lipidol. 2018, 12, 1047–1060. [Google Scholar] [CrossRef]
- Coras, R.; Kavanaugh, A.; Boyd, T.; Huynh, Q.; Pedersen, B.; Armando, A.M.; Dahlberg-Wright, S.; Marsal, S.; Jain, M.; Paravar, T.; et al. Pro- and anti-inflammatory eicosanoids in psoriatic arthritis. Metabolomics 2019, 15, 65. [Google Scholar] [CrossRef]
- Wójcik, P.; Biernacki, M.; Wroński, A.; Łuczaj, W.; Waeg, G.; Žarković, N.; Skrzydlewska, E. Altered Lipid Metabolism in Blood Mononuclear Cells of Psoriatic Patients Indicates Differential Changes in Psoriasis Vulgaris and Psoriatic Arthritis. Int. J. Mol. Sci. 2019, 20, 4249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sethi, S.; Brietzke, E. Recent advances in lipidomics: Analytical and clinical perspectives. Prostaglandins Other Lipid Mediat. 2017, 128–129, 8–16. [Google Scholar] [CrossRef]
- Looby, N.; Roszkowska, A.; Reyes-Garcés, N.; Yu, M.; Bączek, T.; Kulasingam, V.; Pawliszyn, J.; Chandran, V. Serum metabolic fingerprinting of psoriasis and psoriatic arthritis patients using solid-phase microextraction-liquid chromatography-high-resolution mass spectrometry. Metabolomics 2021, 17, 59. [Google Scholar] [CrossRef]
- Ambrożewicz, E.; Wójcik, P.; Wroński, A.; Łuczaj, W.; Jastrząb, A.; Žarković, N.; Skrzydlewska, E. Pathophysiological Alterations of Redox Signaling and Endocannabinoid System in Granulocytes and Plasma of Psoriatic Patients. Cells 2018, 7, 159. [Google Scholar] [CrossRef]
- Kishikawa, T.; Arase, N.; Tsuji, S.; Maeda, Y.; Nii, T.; Hirata, J.; Suzuki, K.; Yamamoto, K.; Masuda, T.; Ogawa, K.; et al. Large-scale plasma-metabolome analysis identifies potential biomarkers of psoriasis and its clinical subtypes. J. Dermatol. Sci. 2021, 102, 78–84. [Google Scholar] [CrossRef]
- Hoch, T.; Schulz, D.; Eling, N.; Gómez, J.M.; Levesque, M.P.; Bodenmiller, B. Multiplexed imaging mass cytometry of the chemokine milieus in melanoma characterizes features of the response to immunotherapy. Sci. Immunol. 2022, 7, eabk1692. [Google Scholar] [CrossRef]
- Schubert, W.; Bonnekoh, B.; Pommer, A.J.; Philipsen, L.; Böckelmann, R.; Malykh, Y.; Gollnick, H.; Friedenberger, M.; Bode, M.; Dress, A.W.M. Analyzing proteome topology and function by automated multidimensional fluorescence microscopy. Nat. Biotechnol. 2006, 24, 1270–1278. [Google Scholar] [CrossRef]
- Schriml, L.M. A decade of GigaScience: 10 years of the evolving genomic and biomedical standards landscape. Gigascience 2022, 11, giac047. [Google Scholar] [CrossRef]
- Field, D.; Amaral-Zettler, L.; Cochrane, G.; Cole, J.R.; Dawyndt, P.; Garrity, G.M.; Gilbert, J.; Glöckner, F.O.; Hirschman, L.; Karsch-Mizrachi, I.; et al. The Genomic Standards Consortium. PLoS Biol. 2011, 9, e1001088. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.F.; Paton, N.W.; Lilley, K.S.; Binz, P.-A.; Julian, R.K.; Jones, A.R.; Zhu, W.; Apweiler, R.; Aebersold, R.; Deutsch, E.W.; et al. The minimum information about a proteomics experiment (MIAPE). Nat. Biotechnol. 2007, 25, 887–893. [Google Scholar] [CrossRef]
- Fiehn, O.; Kristal, B.; van Ommen, B.; Sumner, L.W.; Sansone, S.-A.; Taylor, C.; Hardy, N.; Kaddurah-Daouk, R. Establishing reporting standards for metabolomic and metabonomic studies: A call for participation. Omics A J. Integr. Biol. 2006, 10, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Köfeler, H.C.; Ahrends, R.; Baker, E.S.; Ekroos, K.; Han, X.; Hoffmann, N.; Holčapek, M.; Wenk, M.R.; Liebisch, G. Recommendations for good practice in MS-based lipidomics. J. Lipid Res. 2021, 62, 100138. [Google Scholar] [CrossRef] [PubMed]
- Burla, B.; Arita, M.; Arita, M.; Bendt, A.K.; Cazenave-Gassiot, A.; Dennis, E.A.; Ekroos, K.; Han, X.; Ikeda, K.; Liebisch, G.; et al. MS-based lipidomics of human blood plasma: A community-initiated position paper to develop accepted guidelines. J. Lipid Res. 2018, 59, 2001–2017. [Google Scholar] [CrossRef] [PubMed]
- Coman Schmid, D.; Crameri, K.; Oesterle, S.; Rinn, B.; Sengstag, T.; Stockinger, H. SPHN—The BioMedIT Network: A Secure IT Platform for Research with Sensitive Human Data. Stud. Health Technol. Inform. 2020, 270, 1170–1174. [Google Scholar] [CrossRef]
- Wehrens, R.; Hageman, J.A.; van Eeuwijk, F.; Kooke, R.; Flood, P.J.; Wijnker, E.; Keurentjes, J.J.B.; Lommen, A.; van Eekelen, H.D.L.M.; Hall, R.D.; et al. Improved batch correction in untargeted MS-based metabolomics. Metabolomics 2016, 12, 88. [Google Scholar] [CrossRef]
- Lancaster, S.M.; Sanghi, A.; Wu, S.; Snyder, M.P. A Customizable Analysis Flow in Integrative Multi-Omics. Biomolecules 2020, 10, 1606. [Google Scholar] [CrossRef]
- Kohl, M.; Megger, D.A.; Trippler, M.; Meckel, H.; Ahrens, M.; Bracht, T.; Weber, F.; Hoffmann, A.-C.; Baba, H.A.; Sitek, B.; et al. A practical data processing workflow for multi-OMICS projects. Biochim. Biophys. Acta 2014, 1844, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Jouan-Rimbaud Bouveresse, D.; Pinto, R.C.; Schmidtke, L.M.; Locquet, N.; Rutledge, D.N. Identification of significant factors by an extension of ANOVA–PCA based on multi-block analysis. Chemom. Intell. Lab. Syst. 2011, 106, 173–182. [Google Scholar] [CrossRef]
- Boccard, J.; Rutledge, D.N. A consensus orthogonal partial least squares discriminant analysis (OPLS-DA) strategy for multiblock Omics data fusion. Anal. Chim. Acta 2013, 769, 30–39. [Google Scholar] [CrossRef]
- Picard, M.; Scott-Boyer, M.-P.; Bodein, A.; Périn, O.; Droit, A. Integration strategies of multi-omics data for machine learning analysis. Comput. Struct. Biotechnol. J. 2021, 19, 3735–3746. [Google Scholar] [CrossRef] [PubMed]
- Kingsmore, K.M.; Puglisi, C.E.; Grammer, A.C.; Lipsky, P.E. An introduction to machine learning and analysis of its use in rheumatic diseases. Nat. Rev. Rheumatol. 2021, 17, 710–730. [Google Scholar] [CrossRef] [PubMed]
- Xing, L.; Yu, L.; Zhou, N.; Zhang, Z.; Pu, Y.; Wu, J.; Shu, H. Exploration of biomarkers of psoriasis through combined multiomics analysis. Res. Sq. 2022; Preprint. [Google Scholar] [CrossRef]
- Stafford, I.S.; Kellermann, M.; Mossotto, E.; Beattie, R.M.; MacArthur, B.D.; Ennis, S. A systematic review of the applications of artificial intelligence and machine learning in autoimmune diseases. NPJ Digit. Med. 2020, 3, 30. [Google Scholar] [CrossRef] [PubMed]
- Wörheide, M.A.; Krumsiek, J.; Kastenmüller, G.; Arnold, M. Multi-omics integration in biomedical research—A metabolomics-centric review. Anal. Chim. Acta 2021, 1141, 144–162. [Google Scholar] [CrossRef]
- Petricoin, E.F.; Ardekani, A.M.; Hitt, B.A.; Levine, P.J.; Fusaro, V.A.; Steinberg, S.M.; Mills, G.B.; Simone, C.; Fishman, D.A.; Kohn, E.C.; et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet 2002, 359, 572–577. [Google Scholar] [CrossRef]
- Park, Y.-J.; Chung, M.K.; Hwang, D.; Kim, W.-U. Proteomics in Rheumatoid Arthritis Research. Immune Netw. 2015, 15, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, H.; Ota, M.; Fujio, K. Multiomics landscape of synovial fibroblasts in rheumatoid arthritis. Inflamm. Regen. 2021, 41, 7. [Google Scholar] [CrossRef]
- Tasaki, S.; Suzuki, K.; Kassai, Y.; Takeshita, M.; Murota, A.; Kondo, Y.; Ando, T.; Nakayama, Y.; Okuzono, Y.; Takiguchi, M.; et al. Multi-omics monitoring of drug response in rheumatoid arthritis in pursuit of molecular remission. Nat. Commun. 2018, 9, 2755. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, A.A.; Hao, S.; Jauhiainen, A.; Elfström, K.M.; Egevad, L.; Nordström, T.; Heintz, E.; Clements, M.S. The cost-effectiveness of prostate cancer screening using the Stockholm3 test. PLoS ONE 2021, 16, e0246674. [Google Scholar] [CrossRef]

| Chromosome | Gene or Locus | Variant ID | Ref. |
|---|---|---|---|
| 6 | HLA-B | Amino acid position 45 | [30] |
| 6 | HLA-B | Amino acid position 97 | [29] |
| 1 | IL23R | rs12044149 | [32,33,34] |
| 5 | 5q31 (IL4, KIF3A) | rs715285 | [36] |
| 1 | PTPN22 | rs2476601 | [25] |
| 6 | TNFAIP3 | rs9321623 | [34] |
| 19 | KIR2D | [35] | |
| 2 | B3GNT2 | [37] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gurke, R.; Bendes, A.; Bowes, J.; Koehm, M.; Twyman, R.M.; Barton, A.; Elewaut, D.; Goodyear, C.; Hahnefeld, L.; Hillenbrand, R.; et al. Omics and Multi-Omics Analysis for the Early Identification and Improved Outcome of Patients with Psoriatic Arthritis. Biomedicines 2022, 10, 2387. https://doi.org/10.3390/biomedicines10102387
Gurke R, Bendes A, Bowes J, Koehm M, Twyman RM, Barton A, Elewaut D, Goodyear C, Hahnefeld L, Hillenbrand R, et al. Omics and Multi-Omics Analysis for the Early Identification and Improved Outcome of Patients with Psoriatic Arthritis. Biomedicines. 2022; 10(10):2387. https://doi.org/10.3390/biomedicines10102387
Chicago/Turabian StyleGurke, Robert, Annika Bendes, John Bowes, Michaela Koehm, Richard M. Twyman, Anne Barton, Dirk Elewaut, Carl Goodyear, Lisa Hahnefeld, Rainer Hillenbrand, and et al. 2022. "Omics and Multi-Omics Analysis for the Early Identification and Improved Outcome of Patients with Psoriatic Arthritis" Biomedicines 10, no. 10: 2387. https://doi.org/10.3390/biomedicines10102387