The Potential of Methocinnamox as a Future Treatment for Opioid Use Disorder: A Narrative Review
Abstract
:1. Introduction
2. Main Body
2.1. Methods
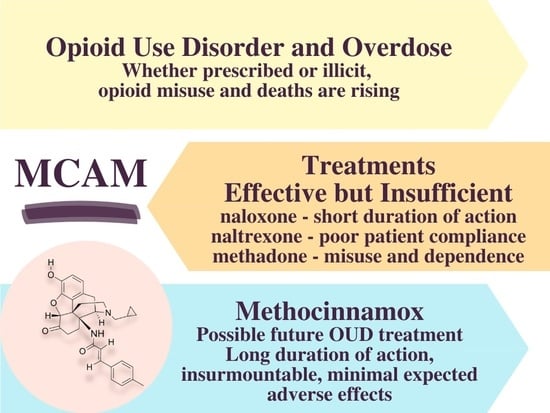
2.2. Opioid Epidemic
2.3. Pain Receptors
2.4. Current OUD Treatments
2.5. Methocinnamox
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- More than a Million Americans Have Died from Overdoses during the Opioid Epidemic. Available online: https://www.npr.org/2021/12/30/1069062738/more-than-a-million-americans-have-died-from-overdoses-during-the-opioid-epidemi (accessed on 23 January 2022).
- Coussens, N.P.; Sittampalam, G.S.; Jonson, S.G.; Hall, M.D.; Gorby, H.E.; Tamiz, A.P.; McManus, O.B.; Felder, C.C.; Rasmussen, K. The Opioid Crisis and the Future of Addiction and Pain Therapeutics. J. Pharmacol. Exp. Ther. 2019, 371, 396–408. [Google Scholar] [CrossRef] [PubMed]
- Bechara, A.; Berridge, K.C.; Bickel, W.K.; Morón, J.A.; Williams, S.B.; Stein, J.S. A Neurobehavioral Approach to Addiction: Implications for the Opioid Epidemic and the Psychology of Addiction. Psychol. Sci. Public Interest 2019, 20, 96–127. [Google Scholar] [CrossRef] [PubMed]
- Torralva, R.; Janowsky, A. Noradrenergic Mechanisms in Fentanyl-Mediated Rapid Death Explain Failure of Naloxone in the Opioid Crisis. J. Pharmacol. Exp. Ther. 2019, 371, 453–475. [Google Scholar] [CrossRef]
- Hoffman, K.A.; Ponce Terashima, J.; McCarty, D. Opioid Use Disorder and Treatment: Challenges and Opportunities. BMC Health Serv. Res. 2019, 19, 884. [Google Scholar] [CrossRef] [PubMed]
- Raehal, K.M.; Bohn, L.M. Mu Opioid Receptor Regulation and Opiate Responsiveness. AAPS J. 2005, 7, E587–E591. [Google Scholar] [CrossRef] [Green Version]
- Pan, Z.Z. Mu-Opposing Actions of the Kappa-Opioid Receptor. Trends Pharmacol. Sci. 1998, 19, 94–98. [Google Scholar] [CrossRef]
- Tofighi, B.; Williams, A.R.; Chemi, C.; Suhail-Sindhu, S.; Dickson, V.; Lee, J.D. Patient Barriers and Facilitators to Medications for Opioid Use Disorder in Primary Care: An in-Depth Qualitative Survey on Buprenorphine and Extended-Release Naltrexone. Subst. Use Misuse 2019, 54, 2409–2419. [Google Scholar] [CrossRef]
- Skolnick, P. On the Front Lines of the Opioid Epidemic: Rescue by Naloxone. Eur. J. Pharmacol. 2018, 835, 147–153. [Google Scholar] [CrossRef]
- Ryan, S.A.; Dunne, R.B. Pharmacokinetic Properties of Intranasal and Injectable Formulations of Naloxone for Community Use: A Systematic Review. Pain Manag. 2018, 8, 231–245. [Google Scholar] [CrossRef] [Green Version]
- Hammerslag, L.R.; Hofford, R.S.; Kang, Q.; Kryscio, R.J.; Beckmann, J.S.; Bardo, M.T. Changes in Fentanyl Demand Following Naltrexone, Morphine, and Buprenorphine in Male Rats. Drug Alcohol Depend. 2020, 207, 107804. [Google Scholar] [CrossRef]
- Moss, R.B.; Carlo, D.J. Higher Doses of Naloxone Are Needed in the Synthetic Opioid Era. Subst. Abuse Treat. Prev. Policy 2019, 14, 6. [Google Scholar] [CrossRef] [Green Version]
- DEA: “Lazarus Parties” or “Narcan Parties” are Real. Available online: https://foxsanantonio.com/news/yami-investigates/dea-lazarus-parties-or-narcan-parties-are-real (accessed on 23 January 2022).
- Minozzi, S.; Amato, L.; Vecchi, S.; Davoli, M.; Kirchmayer, U.; Verster, A. Oral Naltrexone Maintenance Treatment for Opioid Dependence. Cochrane Database Syst. Rev. 2011, 4, CD001333. [Google Scholar] [CrossRef]
- Mattick, R.P.; Kimber, J.; Breen, C.; Davoli, M. Buprenorphine Maintenance versus Placebo or Methadone Maintenance for Opioid Dependence. Cochrane Database Syst. Rev. 2004, 3, CD002207. [Google Scholar] [CrossRef]
- Hswen, Y.; Zhang, A.; Brownstein, J.S. Leveraging Black-Market Street Buprenorphine Pricing to Increase Capacity to Treat Opioid Addiction, 2010–2018. Prev. Med. 2020, 137, 106105. [Google Scholar] [CrossRef] [PubMed]
- Simpson, K.J.; Moran, M.T.; McCall, K.L.; Herbert, J.; Foster, M.L.; Simoyan, O.M.; Shah, D.T.; Desrosiers, C.; Nichols, S.D.; Piper, B.J. Increasing Heroin, Cocaine, and Buprenorphine Arrests Reported to the Maine Diversion Alert Program. Forensic Sci. Int. 2019, 303, 109924. [Google Scholar] [CrossRef] [PubMed]
- Sordo, L.; Barrio, G.; Bravo, M.J.; Indave, B.I.; Degenhardt, L.; Wiessing, L.; Ferri, M.; Pastor-Barriuso, R. Mortality Risk during and after Opioid Substitution Treatment: Systematic Review and Meta-Analysis of Cohort Studies. BMJ 2017, 357, j1550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maguire, D.R.; Gerak, L.R.; Sanchez, J.J.; Javors, M.A.; Disney, A.; Husbands, S.M.; France, C.P. Effects of Acute and Repeated Treatment with Methocinnamox, a Mu Opioid Receptor Antagonist, on Fentanyl Self-Administration in Rhesus Monkeys. Neuropsychopharmacology 2020, 45, 1986–1993. [Google Scholar] [CrossRef]
- Broadbear, J.H.; Sumpter, T.L.; Burke, T.F.; Husbands, S.M.; Lewis, J.W.; Woods, J.H.; Traynor, J.R. Methocinnamox Is a Potent, Long-Lasting, and Selective Antagonist of Morphine-Mediated Antinociception in the Mouse: Comparison with Clocinnamox, Beta-Funaltrexamine, and Beta-Chlornaltrexamine. J. Pharmacol. Exp. Ther. 2000, 294, 933–940. [Google Scholar] [PubMed]
- Gerak, L.R.; Gould, G.G.; Daws, L.C.; France, C.P. Methocinnamox Produces Sustained Antagonism of the Antinociceptive Effects of Morphine and Persistent Decreases in [3H]DAMGO Binding to μ Opioid Receptors in Rat Cortex. FASEB J. 2020, 34, 1. [Google Scholar] [CrossRef]
- Maguire, D.R.; Gerak, L.R.; Woods, J.H.; Husbands, S.M.; Disney, A.; France, C.P. Long-Lasting Effects of Methocinnamox on Opioid Self-Administration in Rhesus Monkeys. J. Pharmacol. Exp. Ther. 2019, 368, 88–99. [Google Scholar] [CrossRef] [Green Version]
- Zamora, J.C.; Kotipalli, V.; Jennings, E.M.; Disney, A.; Husbands, S.; Winger, G.; Clarke, W.P.; Woods, J.H.; Berg, K.A. Methocinnamox (MCAM) Is a Selective, Long Acting Antagonist at Mu Opioid Receptors In Vitro. FASEB J. 2019, 33, 498.8. [Google Scholar] [CrossRef]
- Townsend, E.A. The Lasting Impact of Methocinnamox on Opioid Self-Administration. Neuropsychopharmacology 2020, 45, 1963–1964. [Google Scholar] [CrossRef] [PubMed]
- Minervini, V.; France, C. Long-Term Antagonism of Mu Opioid Receptors by Methocinnamox (MCAM) without Adverse Effects on Memory. FASEB J. 2020, 34, 1. [Google Scholar] [CrossRef]
- Lyden, J.; Binswanger, I.A. The United States Opioid Epidemic. Semin. Perinatol. 2019, 43, 123–131. [Google Scholar] [CrossRef]
- Courtwright, D.T. Preventing and Treating Narcotic Addiction—A Century of Federal Drug Control. N. Engl. J. Med. 2015, 373, 2095–2097. [Google Scholar] [CrossRef] [PubMed]
- Levy, N.; Sturgess, J.; Mills, P. “Pain as the Fifth Vital Sign” and Dependence on the “Numerical Pain Scale” Is Being Abandoned in the US: Why? Br. J. Anaesth. 2018, 120, 435–438. [Google Scholar] [CrossRef] [Green Version]
- Van Zee, A. The Promotion and Marketing of OxyContin: Commercial Triumph, Public Health Tragedy. Am. J. Public Health 2009, 99, 221–227. [Google Scholar] [CrossRef]
- Jones, M.R.; Viswanath, O.; Peck, J.; Kaye, A.D.; Gill, J.S.; Simopoulos, T.T. A Brief History of the Opioid Epidemic and Strategies for Pain Medicine. Pain Ther. 2018, 7, 13–21. [Google Scholar] [CrossRef] [Green Version]
- Singh, V.M.; Browne, T.; Montgomery, J. The Emerging Role of Toxic Adulterants in Street Drugs in the US Illicit Opioid Crisis. Public Health Rep. 2020, 135, 6–10. [Google Scholar] [CrossRef]
- Seth, P.; Scholl, L.; Rudd, R.A.; Bacon, S. Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants—United States, 2015–2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 349–358. [Google Scholar] [CrossRef]
- Stoicea, N.; Costa, A.; Periel, L.; Uribe, A.; Weaver, T.; Bergese, S.D. Current Perspectives on the Opioid Crisis in the US Healthcare System: A Comprehensive Literature Review. Medicine 2019, 98, e15425. [Google Scholar] [CrossRef] [PubMed]
- Hagemeier, N.E. Introduction to the Opioid Epidemic: The Economic Burden on the Healthcare System and Impact on Quality of Life. Am. J. Manag. Care 2018, 24, S200–S206. [Google Scholar] [PubMed]
- Pashmineh Azar, A.R.; Cruz-Mullane, A.; Podd, J.C.; Lam, W.S.; Kaleem, S.H.; Lockard, L.B.; Mandel, M.R.; Chung, D.Y.; Simoyan, O.M.; Davis, C.S.; et al. Rise and Regional Disparities in Buprenorphine Utilization in the United States. Pharmacoepidemiol. Drug Saf. 2020, 29, 708–715. [Google Scholar] [CrossRef]
- Furst, J.A.; Mynarski, N.J.; McCall, K.L.; Piper, B.J. Pronounced Regional Disparities in United States Methadone Distribution. Ann. Pharmacother. 2021, 56, 10600280211028262. [Google Scholar] [CrossRef]
- Frank, R.G.; Fry, C.E. The Impact of Expanded Medicaid Eligibility on Access to Naloxone. Addiction 2019, 114, 1567–1574. [Google Scholar] [CrossRef]
- Drug Overdose Deaths in the U.S. Top 100,000 Annually|cdc.gov. Available online: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm (accessed on 24 January 2022).
- Understanding the Epidemic|CDC’s Response to the Opioid Overdose Epidemic|cdc.gov. Available online: https://www.cdc.gov/opioids/basics/epidemic.html (accessed on 23 January 2022).
- Han, Y.; Yan, W.; Zheng, Y.; Khan, M.Z.; Yuan, K.; Lu, L. The Rising Crisis of Illicit Fentanyl Use, Overdose, and Potential Therapeutic Strategies. Transl. Psychiatry 2019, 9, 1–9. [Google Scholar] [CrossRef] [Green Version]
- McIver, J.S. Seeking Solutions to the Opioid Crisis. P.T. 2017, 42, 478. [Google Scholar]
- Saloner, B.; McGinty, E.E.; Beletsky, L.; Bluthenthal, R.; Beyrer, C.; Botticelli, M.; Sherman, S.G. A Public Health Strategy for the Opioid Crisis. Public Health Rep. 2018, 133, 24S–34S. [Google Scholar] [CrossRef] [Green Version]
- Caton, L.; Cheng, H.; Garneau, H.C.; Fisher, T.; Harris-Mills, B.; Hurley, B.; Newman, S.; McGovern, M.P. COVID-19 Adaptations in the Care of Patients with Opioid Use Disorder: A Survey of California Primary Care Clinics. J. Gen. Intern. Med. 2021, 36, 998–1005. [Google Scholar] [CrossRef]
- Drake, J.; Charles, C.; Bourgeois, J.W.; Daniel, E.S.; Kwende, M. Exploring the Impact of the Opioid Epidemic in Black and Hispanic Communities in the United States. Drug Sci. Policy Law 2020, 6, 1–11. [Google Scholar] [CrossRef]
- As the Pandemic Ushered in Isolation and Financial Hardship, Overdose Deaths Reached New Heights. Available online: https://www.statnews.com/2021/02/16/as-pandemic-ushered-in-isolation-financial-hardship-overdose-deaths-reached-new-heights/ (accessed on 4 April 2022).
- Kolodny, A.; Courtwright, D.T.; Hwang, C.S.; Kreiner, P.; Eadie, J.L.; Clark, T.W.; Alexander, G.C. The Prescription Opioid and Heroin Crisis: A Public Health Approach to an Epidemic of Addiction. Annu. Rev. Public Health 2015, 36, 559–574. [Google Scholar] [CrossRef]
- France, C.P.; Ahern, G.P.; Averick, S.; Disney, A.; Enright, H.A.; Esmaeli-Azad, B.; Federico, A.; Gerak, L.R.; Husbands, S.M.; Kolber, B.; et al. Countermeasures for Preventing and Treating Opioid Overdose. Clin. Pharmacol. Ther. 2020, 109, 578–590. [Google Scholar] [CrossRef]
- Volkow, N.D.; Blanco, C. The Changing Opioid Crisis: Development, Challenges and Opportunities. Mol. Psychiatry 2021, 26, 218–233. [Google Scholar] [CrossRef]
- Gerak, L.R.; Latham, E.A.; Woods, J.H.; Disney, A.; Husbands, S.M.; France, C.P. Methocinnamox: Sustained Antagonism of the Antinociceptive Effects of Morphine and Not Spiradoline in Rats. FASEB J. 2019, 33, 498.10. [Google Scholar] [CrossRef]
- Jennings, E.M.; Disney, A.; Husbands, S.; Winger, G.; Berg, K.A.; Clarke, W.P.; Woods, J.H. Methocinnamox (MCAM) Is an Effective Long-Term Antagonist of Peripheral Mu, but Not Kappa or Delta Opioid Receptors In Vivo. FASEB J. 2019, 33, 498.9. [Google Scholar] [CrossRef]
- Bidlack, J.M. Mixed κ/μ partial opioid agonists as potential treatments for cocaine dependence. Adv. Pharmacol. 2014, 69, 387–418. [Google Scholar] [CrossRef]
- Manglik, A.; Lin, H.; Aryal, D.K.; McCorvy, J.D.; Dengler, D.; Corder, G.; Levit, A.; Kling, R.C.; Bernat, V.; Hübner, H.; et al. Structure-Based Discovery of Opioid Analgesics with Reduced Side Effects. Nature 2016, 537, 185–190. [Google Scholar] [CrossRef] [Green Version]
- Mafi, A.; Kim, S.-K.; Goddard, W.A. Mechanism of β-Arrestin Recruitment by the μ-Opioid G Protein-Coupled Receptor. Proc. Natl. Acad. Sci. USA 2020, 117, 16346–16355. [Google Scholar] [CrossRef]
- Gibula-Tarlowska, E.; Kotlinska, J.H. Crosstalk between Opioid and Anti-Opioid Systems: An Overview and Its Possible Therapeutic Significance. Biomolecules 2020, 10, 1376. [Google Scholar] [CrossRef]
- Al-Hasani, R.; Bruchas, M.R. Molecular Mechanisms of Opioid Receptor-Dependent Signaling and Behavior. Anesthesiology 2011, 115, 1363–1381. [Google Scholar] [CrossRef] [Green Version]
- Corder, G.; Castro, D.C.; Bruchas, M.R.; Scherrer, G. Endogenous and Exogenous Opioids in Pain. Annu. Rev. Neurosci. 2018, 41, 453–473. [Google Scholar] [CrossRef] [PubMed]
- Mondal, D.; Kolev, V.; Warshel, A. Exploring the Activation Pathway and Gi-Coupling Specificity of the μ-Opioid Receptor. Proc. Natl. Acad. Sci. USA 2020, 117, 26218–26225. [Google Scholar] [CrossRef] [PubMed]
- Smrcka, A.V. G Protein Βγ Subunits: Central Mediators of G Protein-Coupled Receptor Signaling. Cell Mol. Life Sci. 2008, 65, 2191–2214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shenoy, S.S.; Lui, F. Biochemistry, Endogenous Opioids; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK532899/ (accessed on 23 January 2022).
- National Academies of Sciences, Engineering and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on Medication-Assisted Treatment for Opioid Use Disorder; Mancher, M.; Leshner, A.I. The Effectiveness of Medication-Based Treatment for Opioid Use Disorder; National Academies Press: Washington, DC, USA, 2019. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541393/ (accessed on 23 January 2022).
- Lipiński, P.F.J.; Kosson, P.; Matalińska, J.; Roszkowski, P.; Czarnocki, Z.; Jarończyk, M.; Misicka, A.; Dobrowolski, J.C.; Sadlej, J. Fentanyl Family at the Mu-Opioid Receptor: Uniform Assessment of Binding and Computational Analysis. Molecules 2019, 24, 740. [Google Scholar] [CrossRef] [Green Version]
- Minervini, V.; Lu, H.Y.; Padarti, J.; Osteicoechea, D.C.; France, C.P. Interactions between kappa and mu opioid receptor agonists: Effects of the ratio of drugs in mixtures. Psychopharmacology 2018, 235, 2245–2256. [Google Scholar] [CrossRef]
- Navratilova, E.; Ji, G.; Phelps, C.; Qu, C.; Hein, M.; Yakhnitsa, V.; Neugebauer, V.; Porreca, F. Kappa Opioid Signaling in the Central Nucleus of the Amygdala Promotes Disinhibition and Aversiveness of Chronic Neuropathic Pain. Pain 2019, 160, 824–832. [Google Scholar] [CrossRef]
- Zhou, W.; Li, Y.; Meng, X.; Liu, A.; Mao, Y.; Zhu, X.; Meng, Q.; Jin, Y.; Zhang, Z.; Tao, W. Switching of Delta Opioid Receptor Subtypes in Central Amygdala Microcircuits Is Associated with Anxiety States in Pain. J. Biol. Chem. 2021, 296, 100277. [Google Scholar] [CrossRef]
- Al-Eitan, L.N.; Rababa’h, D.M.; Alghamdi, M.A. Genetic Susceptibility of Opioid Receptor Genes Polymorphism to Drug Addiction: A Candidate-Gene Association Study. BMC Psychiatry 2021, 21, 5. [Google Scholar] [CrossRef]
- Liu, S.S.; Pickens, S.; Burma, N.E.; Ibarra-Lecue, I.; Yang, H.; Xue, L.; Cook, C.; Hakimian, J.K.; Severino, A.L.; Lueptow, L.; et al. Kappa Opioid Receptors Drive a Tonic Aversive Component of Chronic Pain. J. Neurosci. 2019, 39, 4162–4178. [Google Scholar] [CrossRef] [Green Version]
- Massaly, N.; Copits, B.A.; Wilson-Poe, A.R.; Hipólito, L.; Markovic, T.; Yoon, H.J.; Liu, S.; Walicki, M.C.; Bhatti, D.L.; Sirohi, S.; et al. Pain-Induced Negative Affect Is Mediated via Recruitment of The Nucleus Accumbens Kappa Opioid System. Neuron 2019, 102, 564–573. [Google Scholar] [CrossRef]
- Rosenblum, A.; Marsch, L.A.; Joseph, H.; Portenoy, R.K. Opioids and the Treatment of Chronic Pain: Controversies, Current Status, and Future Directions. Exp. Clin. Psychopharmacol. 2008, 16, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Mercadante, S.; Arcuri, E.; Santoni, A. Opioid-Induced Tolerance and Hyperalgesia. CNS Drugs 2019, 33, 943–955. [Google Scholar] [CrossRef] [PubMed]
- Kosten, T.R.; George, T.P. The Neurobiology of Opioid Dependence: Implications for Treatment. Sci. Pract. Perspect. 2002, 1, 13–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srivastava, A.; Kahan, M.; Nader, M. Primary Care Management of Opioid Use Disorders: Abstinence, Methadone, or Buprenorphine-Naloxone? Can. Fam. Physician 2017, 63, 200–205. [Google Scholar]
- Heo, Y.-A.; Scott, L.J. Buprenorphine/Naloxone (Zubsolv®): A Review in Opioid Dependence. CNS Drugs 2018, 32, 875–882. [Google Scholar] [CrossRef]
- Sullivan, M.A.; Bisaga, A.; Pavlicova, M.; Carpenter, K.M.; Choi, C.J.; Mishlen, K.; Levin, F.R.; Mariani, J.J.; Nunes, E.V. A Randomized Trial Comparing Extended-Release Injectable Suspension and Oral Naltrexone, Both Combined With Behavioral Therapy, for the Treatment of Opioid Use Disorder. Am. J. Psychiatry. 2019, 176, 129–137. [Google Scholar] [CrossRef]
- Chen, K.Y.; Chen, L.; Mao, J. Buprenorphine-Naloxone Therapy in Pain Management. Anesthesiology 2014, 120, 1262–1274. [Google Scholar] [CrossRef] [Green Version]
- Kapur, B.M.; Hutson, J.R.; Chibber, T.; Luk, A.; Selby, P. Methadone: A Review of Drug-Drug and Pathophysiological Interactions. Crit. Rev. Clin. Lab. Sci. 2011, 48, 171–195. [Google Scholar] [CrossRef]
- Jarvis, B.P.; Holtyn, A.F.; Subramaniam, S.; Tompkins, D.A.; Oga, E.A.; Bigelow, G.E.; Silverman, K. Extended-Release Injectable Naltrexone for Opioid Use Disorder: A Systematic Review. Addiction 2018, 113, 1188–1209. [Google Scholar] [CrossRef]
- Morgan, J.R.; Schackman, B.R.; Leff, J.A.; Linas, B.P.; Walley, A.Y. Injectable Naltrexone, Oral Naltrexone, and Buprenorphine Utilization and Discontinuation among Individuals Treated for Opioid Use Disorder in a United States Commercially Insured Population. J. Subst. Abuse. Treat. 2018, 85, 90–96. [Google Scholar] [CrossRef]
- Sudakin, D. Naltrexone: Not Just for Opioids Anymore. J. Med. Toxicol. 2016, 12, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Bostwick, J.M.; Bucci, J.A. Internet Sex Addiction Treated with Naltrexone. Mayo Clin. Proc. 2008, 83, 226–230. [Google Scholar] [CrossRef] [Green Version]
- Garayar Cantero, M.; Canseco Martín, M.; Aguado García, Á.; Ruiz-Sánchez, D.; Valtueña, J.; Manchado López, P. Use of Low-Dose Naltrexone in the Treatment of Severe Hailey-Hailey Disease: One Case Report. Dermatol. Ther. 2019, 32, e12892. [Google Scholar] [CrossRef] [PubMed]
- David, S.P.; Lancaster, T.; Stead, L.F.; Evins, A.E.; Prochaska, J.J. Opioid Antagonists for Smoking Cessation. Cochrane Database Syst. Rev. 2013, 6, CD003086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larochelle, M.R.; Bernson, D.; Land, T.; Stopka, T.J.; Wang, N.; Xuan, Z.; Bagley, S.M.; Liebschutz, J.M.; Walley, A.Y. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality: A Cohort Study. Ann. Intern. Med. 2018, 169, 137–145. [Google Scholar] [CrossRef]
- Ferrari, A.; Coccia, C.P.R.; Bertolini, A.; Sternieri, E. Methadone--Metabolism, Pharmacokinetics and Interactions. Pharmacol. Res. 2004, 50, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Whelan, P.J.; Remski, K. Buprenorphine vs Methadone Treatment: A Review of Evidence in Both Developed and Developing Worlds. J. Neurosci. Rural Pract. 2012, 3, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Welsh, C.; Valadez-Meltzer, A. Buprenorphine: A (relatively) new treatment for opioid dependence. Psychiatry 2005, 2, 29–39. [Google Scholar] [PubMed]
- Anderson, I.B.; Kearney, T.E. Use of Methadone. West. J. Med. 2000, 172, 43–46. [Google Scholar] [CrossRef]
- Sirohi, S.; Dighe, S.V.; Madia, P.A.; Yoburn, B.C. The relative potency of inverse opioid agonists and a neutral opioid antagonist in precipitated withdrawal and antagonism of analgesia and toxicity. J. Pharmacol. Exp. Ther. 2009, 330, 513–519. [Google Scholar] [CrossRef] [Green Version]
- Rzasa Lynn, R.; Galinkin, J. Naloxone Dosage for Opioid Reversal: Current Evidence and Clinical Implications. Ther. Adv. Drug Saf. 2018, 9, 63–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schumacher, M.A.; Basbaum, A.I.; Naidu, R.K. Opioid Agonists & Antagonists. In Basic & Clinical Pharmacology; Katzung, B.G., Ed.; McGraw-Hill Education: New York, NY, USA, 2017; Available online: https://accessmedicine.mhmedical.com/content.aspx?bookid=2249§ionid=175220393 (accessed on 14 February 2021).
- Gracely, R.H.; Dubner, R.; Wolskee, P.J.; Deeter, W.R. Placebo and Naloxone Can Alter Post-Surgical Pain by Separate Mechanisms. Nature 1983, 306, 264–265. [Google Scholar] [CrossRef] [PubMed]
- Eippert, F.; Bingel, U.; Schoell, E.D.; Yacubian, J.; Klinger, R.; Lorenz, J.; Büchel, C. Activation of the Opioidergic Descending Pain Control System Underlies Placebo Analgesia. Neuron 2009, 63, 533–543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wachman, E.M.; Saia, K.; Miller, M.; Valle, E.; Shrestha, H.; Carter, G.; Werler, M.; Jones, H. Naltrexone Treatment for Pregnant Women With Opioid Use Disorder Compared With Matched Buprenorphine Control Subjects. Clin. Ther. 2019, 41, 1681–1689. [Google Scholar] [CrossRef]
- Tran, T.H.; Griffin, B.L.; Stone, R.H.; Vest, K.M.; Todd, T.J. Methadone, Buprenorphine, and Naltrexone for the Treatment of Opioid Use Disorder in Pregnant Women. Pharmacotherapy 2017, 37, 824–839. [Google Scholar] [CrossRef]
- Krupitsky, E.; Nunes, E.V.; Ling, W.; Illeperuma, A.; Gastfriend, D.R.; Silverman, B.L. Injectable Extended-Release Naltrexone for Opioid Dependence: A Double-Blind, Placebo-Controlled, Multicentre Randomised Trial. Lancet 2011, 377, 1506–1513. [Google Scholar] [CrossRef]
- Naloxone. Available online: https://go.drugbank.com/drugs/DB01183 (accessed on 26 January 2022).
- Naloxone Monograph for Professionals. Available online: https://www.drugs.com/monograph/naloxone.html (accessed on 26 January 2022).
- Naltrexone. Available online: https://go.drugbank.com/drugs/DB00704 (accessed on 26 January 2022).
- Naltrexone Monograph for Professionals. Available online: https://www.drugs.com/monograph/naltrexone.html (accessed on 26 January 2022).
- Methadone. Available online: https://go.drugbank.com/drugs/DB00333 (accessed on 26 January 2022).
- Methadone Monograph for Professionals. Available online: https://www.drugs.com/monograph/methadone.html (accessed on 26 January 2022).
- Opioid Prescribing: Methadone Risk Mitigation. Available online: https://www.apsf.org/article/opioid-prescribing-methadone-risk-mitigation/ (accessed on 4 April 2022).
- Buprenorphine. Available online: https://go.drugbank.com/drugs/DB00921 (accessed on 26 January 2022).
- Buprenorphine Monograph for Professionals. Available online: https://www.drugs.com/monograph/buprenorphine.html (accessed on 26 January 2022).
- Jimenez, V.M.; Castaneda, G.; France, C.P. Methocinnamox (MCAM) Reverses and Prevents Fentanyl-Induced Ventilatory Depression in Rats. J. Pharmacol. Exp. Ther. 2021, 377, 29–38. [Google Scholar] [CrossRef]
- Gerak, L.R.; Maguire, D.R.; Woods, J.H.; Husbands, S.M.; Disney, A.; France, C.P. Reversal and Prevention of the Respiratory-Depressant Effects of Heroin by the Novel μ-Opioid Receptor Antagonist Methocinnamox in Rhesus Monkeys. J. Pharmacol. Exp. Ther. 2019, 368, 229–236. [Google Scholar] [CrossRef] [Green Version]
- Zamora, J.C.; Smith, H.R.; Jennings, E.M.; Chavera, T.S.; Kotipalli, V.; Jay, A.; Husbands, S.M.; Disney, A.; Berg, K.A.; Clarke, W.P. Long-term Antagonism and Allosteric Regulation of Mu Opioid Receptors by the Novel Ligand, Methocinnamox. Pharmacol. Res. Perspect. 2021, 9, e00887. [Google Scholar] [CrossRef]
- Gerak, L.R.; Minervini, V.; Latham, E.; Ghodrati, S.; Lillis, K.V.; Wooden, J.; Disney, A.; Husbands, S.M.; France, C.P. Methocinnamox Produces Long-Lasting Antagonism of the Behavioral Effects of µ-Opioid Receptor Agonists but Not Prolonged Precipitated Withdrawal in Rats. J. Pharmacol. Exp. Ther. 2019, 371, 507–516. [Google Scholar] [CrossRef]
- Something better than Naloxone. Available online: https://www.wqad.com/article/news/health/your-health/your-health-mcam/526-cda2622a-69a3-4962-885a-a2185e9507d6 (accessed on 3 April 2022).
- National Institute on Drug Abuse—A Novel Opioid Receptor Antagonist for Treating Abuse and Overdose. Available online: https://taggs.hhs.gov/Detail/AwardDetail?arg_AwardNum=R01DA048417&arg_ProgOfficeCode=114 (accessed on 14 February 2021).
- National Institute of Health—Funded Projects. Available online: https://www.heal.nih.gov/funding/awarded (accessed on 14 February 2021).
- Sansom, W. Long-lasting treatment drug could slow the opioid crisis. UT Health. 9 March 2020. Available online: https://news.uthscsa.edu/long-lasting-treatment-drug-could-slow-the-opioid-crisis/ (accessed on 3 April 2022).
- Compound Summary Methocinnamox. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/46877713 (accessed on 15 May 2021).
- Maguire, D.; Gerak, L.; Disney, A.; Husbands, S.; France, C. Effects of Acute and Repeated Methocinnamox Treatment on Fentanyl Self-administration in Rhesus Monkeys. FASEB J. 2020, 34, 1. [Google Scholar] [CrossRef]
- Minervini, V.; Disney, A.; Husbands, S.M.; France, C.P. Methocinnamox (MCAM) Antagonizes the Behavioral Suppressant Effects of Morphine without Impairing Delayed Matching-to-Sample Accuracy in Rhesus Monkeys. Psychopharmacology 2020, 237, 3057–3065. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, V.; Maguire, D.; Gerak, L.; France, C. Methocinnamox (MCAM) Reverses and Provides Extended Protection from Fentanyl-Induced Respiratory Depression in Awake Unrestrained Rats. FASEB J. 2020, 34, 1. [Google Scholar] [CrossRef]
- Peckham, E.M.; Barkley, L.M.; Divin, M.F.; Cicero, T.J.; Traynor, J.R. Comparison of the Antinociceptive Effect of Acute Morphine in Female and Male Sprague-Dawley Rats Using the Long-Lasting Mu-Antagonist Methocinnamox. Brain Res. 2005, 1058, 137–147. [Google Scholar] [CrossRef] [PubMed]
- New Drug Blocks the Fatal Effects of Opioids? Available online: https://www.wndu.com/content/news/New-drug-blocks-the-fatal-effects-of-opioids-568493251.html (accessed on 3 April 2022).

| Treatment Drug | Method of Administration | Mechanism of Action | Onset of Action | Duration of Action | Strengths | Limitations |
|---|---|---|---|---|---|---|
| naloxone | Intravenous Intramuscular Subcutaneous Intranasal Inhalation | Reversible μ, κ and δ competitive antagonist | 1–5 min | 1–2 h | Rescue from overdose, wide therapeutic window | Short DOA, community misuse, risk of renarcotization, precipitates withdrawal, drug-drug interactions, surmountable |
| naltrexone | Intravenous Intramuscular Subcutaneous 1 Oral | Reversible μ, κ and δ competitive antagonist | 15–30 min | >72 h | Use during pregnancy, extended-release formula | May precipitate withdrawal, patient noncompliance, drug-drug interactions |
| methadone | Intravenous Intramuscular Subcutaneous Oral | μ and δ agonist | 30–60 min | 4–8 h, single dose; 22–24 h, continuous dosing | Prevents withdrawal, reduces opioid cravings, pain relief | Patient noncompliance, dependence, misuse and diversion, restricted availability in US, close monitoring of dosage, many drug-drug interactions, ADRs |
| buprenorphine | Intravenous Intramuscular Subcutaneous Oral Buccal Sublingual Transdermal | Partial μ agonist, κ, δ competitive antagonist | 10–30 min | 2–24 h | Prevents withdrawal, use during pregnancy, prevents euphoria and overdose symptoms | Less potent than methadone, patient retention inferior to methadone, may precipitate withdrawal, drug-drug interactions, ADRs |
| MCAM | Intravenous Subcutaneous | Pseudo-irreversible μ, not competitive antagonist 2, reversible κ, δ competitive antagonism | 15–45 min | 5 days to 2 weeks | Long DOA, not surmountable, prevents renarcotization, lacks notable drug–drug interactions, antinociceptive concomitant treatment possible | Precipitates withdrawal, not yet tested in humans |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jordan, C.G.; Kennalley, A.L.; Roberts, A.L.; Nemes, K.M.; Dolma, T.; Piper, B.J. The Potential of Methocinnamox as a Future Treatment for Opioid Use Disorder: A Narrative Review. Pharmacy 2022, 10, 48. https://doi.org/10.3390/pharmacy10030048
Jordan CG, Kennalley AL, Roberts AL, Nemes KM, Dolma T, Piper BJ. The Potential of Methocinnamox as a Future Treatment for Opioid Use Disorder: A Narrative Review. Pharmacy. 2022; 10(3):48. https://doi.org/10.3390/pharmacy10030048
Chicago/Turabian StyleJordan, Colleen G., Amy L. Kennalley, Alivia L. Roberts, Kaitlyn M. Nemes, Tenzing Dolma, and Brian J. Piper. 2022. "The Potential of Methocinnamox as a Future Treatment for Opioid Use Disorder: A Narrative Review" Pharmacy 10, no. 3: 48. https://doi.org/10.3390/pharmacy10030048