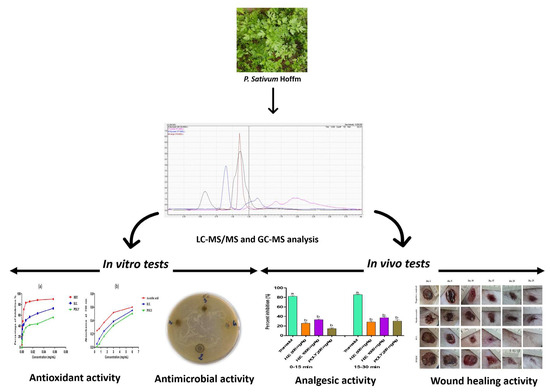
LC-MS/MS and GC/MS Profiling of Petroselinum sativum Hoffm. and Its Topical Application on Burn Wound Healing and Related Analgesic Potential in Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plant Material
2.2. Animal Material
2.3. Preparation of the Hydro-Ethanolic Extract
2.4. Preparation of the Polyphenolic Fraction
2.5. Phytochemical Analysis by LC-MS/MS
2.6. Phytochemical Analysis by GC-MS
2.7. Determination of Total Phenol and Flavonoid Contents
2.8. Assessment of Antioxidant Activity
2.8.1. Scavenging of the Free Radical (DPPH)
- IP: Inhibition Percentage.
- A0: OD of DPPH solution in the absence of the extract (negative control).
- A: OD of DPPH solution containing the extract.
2.8.2. Ferric Reducing Antioxidant Power (FRAP)
2.8.3. Total Antioxidant Capacity Test (TAC)
2.9. Antimicrobial Activity
2.9.1. Agar Well Diffusion Assay
2.9.2. Determination of the Minimum Inhibitory Concentration (MIC)
2.10. Analgesic Activity In Vivo
2.10.1. Abdominal Writhes
2.10.2. Formalin Induced Pain
2.11. Wound Healing Activity In Vivo
2.11.1. Ointments Preparation
2.11.2. Induction of Burn Injuries
- WC (%) = Rate of wound contraction.
- WS0 = Size of the wound at the first day.
- WSSD = Size of the wound at each specific day.
2.12. Statistical Analysis
3. Results
3.1. Phytochemical Analysis by LC-MS/MS
3.2. Phytochemical Analysis by GC-MS
3.3. Estimation of Total Phenol and Flavonoid Contents
3.4. Antioxidant Activity
3.4.1. DPPH and FRAP Assays
3.4.2. Total Antioxidant Capacity (TAC)
3.5. Antimicrobial Activity
3.6. Analgesic Activity
3.6.1. Abdominal Writhes
3.6.2. Formalin Induced Pain
3.7. Wound Healing Activity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Y.; Li, X.; Zou, D.; Liu, W.; Yang, J.; Zhu, N.; Huo, L.; Wang, M.; Hong, J.; Wu, P.; et al. Treatment of Type 2 Diabetes and Dyslipidemia with the Natural Plant Alkaloid Berberine. J. Clin. Endocrinol. Metab. 2008, 93, 2559–2565. [Google Scholar] [CrossRef]
- Zeilhofer, H.U. Prostanoids in Nociception and Pain. Biochem. Pharmacol. 2007, 73, 165–174. [Google Scholar] [CrossRef]
- Guo, S.; DiPietro, L.A. Factors Affecting Wound Healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef]
- Apak, R.; Güçlü, K.; Özyürek, M.; Karademir, S.E. Novel Total Antioxidant Capacity Index for Dietary Polyphenols and Vitamins C and E, Using Their Cupric Ion Reducing Capability in the Presence of Neocuproine: CUPRAC Method. J. Agric. Food Chem. 2004, 52, 7970–7981. [Google Scholar] [CrossRef] [PubMed]
- Mahdi, I.; Bakrim, W.B.; Bitchagno, G.T.M.; Annaz, H.; Mahmoud, M.F.; Sobeh, M. Unraveling the Phytochemistry, Traditional Uses, and Biological and Pharmacological Activities of Thymus Algeriensis Boiss. & Reut. Oxid. Med. Cell. Longev. 2022, 2022, 6487430. [Google Scholar]
- Rojkind, M.; Dominguez-Rosales, J.-A.; Nieto, N.; Greenwel, P. Role of Hydrogen Peroxide and Oxidative Stress in Healing Responses. Cell. Mol. Life Sci. CMLS 2002, 59, 1872–1891. [Google Scholar] [CrossRef] [PubMed]
- López, M.G.; Sánchez-Mendoza, I.R.; Ochoa-Alejo, N. Compartive Study of Volatile Components and Fatty Acids of Plants and in Vitro Cultures of Parsley (Petroselinum Crispum (Mill) Nym Ex Hill). J. Agric. Food Chem. 1999, 47, 3292–3296. [Google Scholar] [CrossRef] [PubMed]
- Aziz, N.; Kim, M.-Y.; Cho, J.Y. Anti-Inflammatory Effects of Luteolin: A Review of in Vitro, in Vivo, and in Silico Studies. J. Ethnopharmacol. 2018, 225, 342–358. [Google Scholar] [CrossRef]
- Chaves, D.S.A.; Frattani, F.S.; Assafim, M.; de Almeida, A.P.; Zingali, R.B.; Costa, S.S. Composition Chimique Phénolique de l’ Extrait de Petroselinum Crispum et Son Effet Sur l’hémostase. Nat. Prod. Commun. 2011, 6, 1934578X1100600709. [Google Scholar] [CrossRef]
- Haque, A.; Pant, A.B. Mitigating Covid-19 in the Face of Emerging Virus Variants, Breakthrough Infections and Vaccine Hesitancy. J. Autoimmun. 2022, 102792. [Google Scholar] [CrossRef]
- Slighoua, M.; Mahdi, I.; Amrati, F.E.; Boukhira, S.; Youbi, A.E.H.E.; Bari, A.; Bousta, D. Ethnopharmacological Survey of Medicinal Plants Used in the Traditional Treatment of Female Infertility in Fez Region, Morocco. Phytothérapie 2020, 18, 321–339. [Google Scholar] [CrossRef]
- Tümen, G.; Malyer, H.; Başer, K.H.C.; Öz Aydın, S. Plants Used in Anatolia for Wound Healing. In Proceedings of the IVth International Congress of Ethnobotany (ICEB 2005), Istanbul, Turkey, 21–26 August 2005; Volume 217, p. 221. [Google Scholar]
- Bakrim, W.B.; Nurcahyanti, A.D.R.; Dmirieh, M.; Mahdi, I.; Elgamal, A.M.; El Raey, M.A.; Wink, M.; Sobeh, M. Phytochemical Profiling of the Leaf Extract of Ximenia Americana Var. Caffra and Its Antioxidant, Antibacterial, and Antiaging Activities In Vitro and in Caenorhabditis Elegans: A Cosmeceutical and Dermatological Approach. Oxid. Med. Cell. Longev. 2022, 2022, e3486257. [Google Scholar] [CrossRef]
- Farzaei, M.H.; Abbasabadi, Z.; Ardekani, M.R.S.; Rahimi, R.; Farzaei, F. Parsley: A Review of Ethnopharmacology, Phytochemistry and Biological Activities. J. Tradit. Chin. Med. 2013, 33, 815–826. [Google Scholar] [CrossRef] [PubMed]
- Thangavelu, S.; Balasubramanian, B.; Palanisamy, S.; Shanmugam, V.; Natchiappan, S.; Kalibulla, S.I.; Rathinasamy, B.; Arumugam, V.A. Characterization and Phytoconstituents of Petroselinum Crispum (Mill) and Coriandrum Sativum (Linn) and Their Impacts on Inflammation—An in Vitro Analysis against Human Adenocarcinoma Cells with Molecular Docking. S. Afr. J. Bot. 2022, 146, 776–788. [Google Scholar] [CrossRef]
- AbdelKhalek, A.S.; Youssef, H.A.; Ali, M.F.; Ali, M.M.; Abdel-Hakiem, M.A.H.; Mahmoud, H.F.F. An Assessment of Clinical, Biometric, Cosmetic and Microscopic Outcomes of Four Suture Techniques for Cutaneous Closure of Laparotomy Wounds: An Experimental Study in Rabbits. J. Dairy Vet. Anim. Res. 2019, 8, 42–53. [Google Scholar] [CrossRef]
- Esther, T.L.H. Investigation of the Antioxidant, Anticancer, Wound Healing, Immunomodulatory and Dna Protective Activities of Coriandrum Sativum and Petroselinum Crispum/Esther Tang Lai Har. Ph.D. Thesis, University of Malaya, Kuala Lumpur, Malaysia, 2014. [Google Scholar]
- Behtash, N.; Kargarzadeh, F.; Shafaroudi, H. Analgesic Effects of Seed Extract from Petroselinum Crispum (Tagetes Minuta) in Animal Models. Toxicol. Lett. 2008, 180, S127–S128. [Google Scholar] [CrossRef]
- Eidi, A.; Eidi, M.; Badiei, L. Antinociceptive Effects of Ethanolic Extract of Parsley (Petroselinum Crispum L.) Leaves in Mice. Med. Sci. J. Islam. Azad Univesity Tehran Med. Branch 2009, 19, 181–186. [Google Scholar]
- Moazedi, A.A.; Mirzaie, D.N.; Seyyednejad, S.M.; Zadkarami, M.R.; Amirzargar, A. Spasmolytic Effect of Petroselinum Crispum (Parsley) on Rat’s Ileum at Different Calcium Chloride Concentrations. Pak. J. Biol. Sci. PJBS 2007, 10, 4036–4042. [Google Scholar] [CrossRef] [PubMed]
- Annaz, H.; Sane, Y.; Bitchagno, G.T.M.; Ben Bakrim, W.; Drissi, B.; Mahdi, I.; El Bouhssini, M.; Sobeh, M. Caper (Capparis Spinosa L.): An Updated Review on Its Phytochemistry, Nutritional Value, Traditional Uses, and Therapeutic Potential. Front. Pharmacol. 2022, 13. [Google Scholar] [CrossRef]
- Ngaffo, C.M.; Tankeo, S.B.; Guefack, M.-G.F.; Nayim, P.; Wamba, B.E.; Kuete, V.; Mbaveng, A.T. Phytochemical Analysis and Antibiotic-Modulating Activity of Cocos Nucifera, Glycine Max and Musa Sapientum Methanol Extracts against Multidrug Resistant Gram-Negative Bacteria. Investig. Med. Chem. Pharmacol. 2021, 4, 53. [Google Scholar]
- Terekhov, R.P.; Selivanova, I.A.; Anurova, M.N.; Zhevlakova, A.K.; Nikitin, I.D.; Cong, Z.; Ma, S.; Yang, F.; Dong, Z.; Liao, Y. Comparative Study of Wound-Healing Activity of Dihydroquercetin Pseudopolymorphic Modifications. Bull. Exp. Biol. Med. 2021, 170, 444–447. [Google Scholar]
- Dahm, H. Silver Nanoparticles in Wound Infections: Present Status and Future Prospects. In Nanotechnology in Skin, Soft Tissue, and Bone Infections; Rai, M., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 151–168. ISBN 978-3-030-35147-2. [Google Scholar]
- Sawyer, R.G.; Pruett, T.L. Wound Infections. Surg. Clin. N. Am. 1994, 74, 519–536. [Google Scholar] [CrossRef]
- Slighoua, M.; Mahdi, I.; Amrati, F.; Di Cristo, F.; Amaghnouje, A.; Grafov, A.; Boucetta, N.; Bari, A.; Bousta, D. Assessment of in Vivo Estrogenic and Anti-Inflammatory Activities of the Hydro-Ethanolic Extract and Polyphenolic Fraction of Parsley (Petroselinum Sativum Hoffm.). J. Ethnopharmacol. 2021, 265, 113290. [Google Scholar] [CrossRef] [PubMed]
- Lilienblum, W.; Dekant, W.; Foth, H.; Gebel, T.; Hengstler, J.G.; Kahl, R.; Kramer, P.-J.; Schweinfurth, H.; Wollin, K.-M. Alternative Methods to Safety Studies in Experimental Animals: Role in the Risk Assessment of Chemicals under the New European Chemicals Legislation (REACH). Arch. Toxicol. 2008, 82, 211–236. [Google Scholar] [CrossRef] [PubMed]
- Wafa, G.; Amadou, D.; Larbi, K.M.; Héla, E.F.O. Larvicidal Activity, Phytochemical Composition, and Antioxidant Properties of Different Parts of Five Populations of Ricinus Communis L. Ind. Crops Prod. 2014, 56, 43–51. [Google Scholar] [CrossRef]
- Amrati, F.E.-Z.; Bourhia, M.; Saghrouchni, H.; Slighoua, M.; Grafov, A.; Ullah, R.; Ezzeldin, E.; Mostafa, G.A.; Bari, A.; Ibenmoussa, S.; et al. Caralluma Europaea (Guss.) N.E.Br.: Anti-Inflammatory, Antifungal, and Antibacterial Activities against Nosocomial Antibiotic-Resistant Microbes of Chemically Characterized Fractions. Molecules 2021, 26, 636. [Google Scholar] [CrossRef] [PubMed]
- Slighoua, M.; Mahdi, I.; ez-zahra Amrati, F.; Boucetta, N.; Cristo, F.D.; Boukhira, S.; El youbi el Hamsas, A.; Tattou, M.I.; Grafov, A.; Bari, A.; et al. Pharmacological Effects of Lavandula Officinalis Chaix and Its Polyphenols: Focus on Their in Vivo Estrogenic and Anti-Inflammatory Properties. South Afr. J. Bot. 2022, 146, 354–364. [Google Scholar] [CrossRef]
- Amaghnouje, A.; Mechchate, H.; Es-safi, I.; Boukhira, S.; Aliqahtani, A.S.; Noman, O.M.; Nasr, F.A.; Conte, R.; Calarco, A.; Bousta, D. Subacute Assessment of the Toxicity and Antidepressant-Like Effects of Origanum Majorana L. Polyphenols in Swiss Albino Mice. Molecules 2020, 25, 5653. [Google Scholar] [CrossRef]
- Griffiths, W.J.; Wang, Y. Analysis of Neurosterols by GC–MS and LC–MS/MS. J. Chromatogr. B 2009, 877, 2778–2805. [Google Scholar] [CrossRef]
- Kabran, G.R.; Mamyrbekova-Bekro, J.A.; Pirat, J.-L.; Bekro, Y.-A.; Sommerer, N.; Verbaere, A.; Meudec, E. Identification de composés phénoliques extraits de deux plantes de la pharmacopée ivoirienne */Identification of phenolic compounds from two plants of ivorian pharmacopeia *. J. Société Ouest-Afr. Chim. 2014, 38, 57–63. [Google Scholar]
- Slinkard, K.; Singleton, V.L. Total Phenol Analysis: Automation and Comparison with Manual Methods. Am. J. Enol. Vitic. 1977, 28, 49–55. [Google Scholar] [CrossRef]
- Brand-Williams, W.; Cuvelier, M.E.; Berset, C. Use of a Free Radical Method to Evaluate Antioxidant Activity. LWT Food Sci. Technol. 1995, 28, 25–30. [Google Scholar] [CrossRef]
- Oyaizu, M. Studies on Products of Browning Reaction Antioxidative Activities of Products of Browning Reaction Prepared from Glucosamine. Jpn. J. Nutr. Diet. 1986, 44, 307–315. [Google Scholar] [CrossRef]
- Baali, F.; Boumerfeg, S.; Napoli, E.; Boudjelal, A.; Righi, N.; Deghima, A.; Baghiani, A.; Ruberto, G. Chemical Composition and Biological Activities of Essential Oils from Two Wild Algerian Medicinal Plants: Mentha Pulegium L. and Lavandula Stoechas L. J. Essent. Oil Bear. Plants 2019, 22, 821–837. [Google Scholar] [CrossRef]
- Mašković, P.Z.; Manojlović, N.T.; Mandić, A.I.; Mišan, A.Č.; Milovanović, I.L.; Radojković, M.M.; Cvijović, M.S.; Solujić, S.R. Phytochemical Screening and Biological Activity of Extracts of Plant Species Halacsya Sendtneri (Boiss.) Dörfl. Hem. Ind. 2012, 66, 43–51. [Google Scholar] [CrossRef] [Green Version]
- Balouiri, M.; Sadiki, M.; Ibnsouda, S.K. Methods for in Vitro Evaluating Antimicrobial Activity: A Review. J. Pharm. Anal. 2016, 6, 71–79. [Google Scholar] [CrossRef]
- Mabadahanye, K. Isolation and Analysing Chemical Profiles of Bioactive Compounds from South Africa Medicinal Plants with Activity against Pathogenic Organisms; University of Johannesburg: Johannesburg, South Africa, 2020; ISBN 9798544213154. [Google Scholar]
- Athanassiadis, B.; Abbott, P.V.; George, N.; Walsh, L.J. An in Vitro Study of the Antimicrobial Activity of Some Endodontic Medicaments and Their Bases Using an Agar Well Diffusion Assay. Aust. Dent. J. 2009, 54, 141–146. [Google Scholar] [CrossRef]
- Nalawade, T.M.; Bhat, K.G.; Sogi, S. Antimicrobial Activity of Endodontic Medicaments and Vehicles Using Agar Well Diffusion Method on Facultative and Obligate Anaerobes. Int. J. Clin. Pediatr. Dent. 2016, 9, 335. [Google Scholar]
- Hayet, E.; Maha, M.; Samia, A.; Mata, M.; Gros, P.; Raida, H.; Ali, M.M.; Mohamed, A.S.; Gutmann, L.; Mighri, Z. Antimicrobial, Antioxidant, and Antiviral Activities of Retama Raetam (Forssk.) Webb Flowers Growing in Tunisia. World J. Microbiol. Biotechnol. 2008, 24, 2933–2940. [Google Scholar] [CrossRef]
- Wayne, P.A. Clinical and Laboratory Standards Institute: Performance Standards for Antimicrobial Susceptibility Testing: 20th Informational Supplement. CLSI Doc. M100-S20 2010. [Google Scholar]
- Adeoyo, O.R.; Pletschke, B.I.; Dames, J.F. Molecular Identification and Antibacterial Properties of an Ericoid Associated Mycorrhizal Fungus. BMC Microbiol. 2019, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Scott, L.J.; Perry, C.M. Tramadol. Drugs 2000, 60, 139–176. [Google Scholar] [CrossRef]
- França, D.S.; Souza, A.L.; Almeida, K.R.; Dolabella, S.S.; Martinelli, C.; Coelho, M.M. B Vitamins Induce an Antinociceptive Effect in the Acetic Acid and Formaldehyde Models of Nociception in Mice. Eur. J. Pharmacol. 2001, 421, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Hajhashemi, V.; Ghannadi, A.; Sharif, B. Anti-Inflammatory and Analgesic Properties of the Leaf Extracts and Essential Oil of Lavandula Angustifolia Mill. J. Ethnopharmacol. 2003, 89, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Manglik, A.; Lin, H.; Aryal, D.K.; McCorvy, J.D.; Dengler, D.; Corder, G.; Levit, A.; Kling, R.C.; Bernat, V.; Hübner, H. Structure-Based Discovery of Opioid Analgesics with Reduced Side Effects. Nature 2016, 537, 185–190. [Google Scholar] [CrossRef]
- Wang, Y.; Hu, X.; Huang, H.; Jin, Z.; Gao, J.; Guo, Y.; Zhong, Y.; Li, Z.; Zong, X.; Wang, K. Optimization of 4-Arylthiophene-3-Carboxylic Acid Derivatives as Inhibitors of ANO1: Lead Optimization Studies toward Their Analgesic Efficacy for Inflammatory Pain. Eur. J. Med. Chem. 2022, 237, 114413. [Google Scholar] [CrossRef]
- De Miranda, F.G.G.; Vilar, J.C.; Alves, I.A.N.; de Holanda Cavalcanti, S.C.; Antoniolli, Â.R. Antinociceptive and Antiedematogenic Properties and Acute Toxicity of Tabebuia Avellanedae Lor. Ex Griseb. Inner Bark Aqueous Extract. BMC Pharmacol. 2001, 1, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Heidari, M.; Bahramsoltani, R.; Abdolghaffari, A.H.; Rahimi, R.; Esfandyari, M.; Baeeri, M.; Hassanzadeh, G.; Abdollahi, M.; Farzaei, M.H. Efficacy of Topical Application of Standardized Extract of Tragopogon Graminifolius in the Healing Process of Experimental Burn Wounds. J. Tradit. Complement. Med. 2019, 9, 54–59. [Google Scholar] [CrossRef]
- Slighoua, M.; Chebaibi, M.; Mahdi, I.; Amrati, F.E.; Conte, R.; Cordero, M.A.W.; Alotaibi, A.; Saghrouchni, H.; Agour, A.; Zair, T.; et al. The LC-MS/MS Identification and Analgesic and Wound Healing Activities of Lavandula Officinalis Chaix: In Vivo and In Silico Approaches. Plants 2022, 11, 3222. [Google Scholar] [CrossRef]
- Charles, D.J. Antioxidant Properties of Spices, Herbs and Other Sources [Electronic Resource]; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Omar, S.H. Oleuropein in Olive and Its Pharmacological Effects. Sci. Pharm. 2010, 78, 133–154. [Google Scholar] [CrossRef]
- Bhalla, M. Pharmacological Aspects of a Bioactive Compound Arbutin: A Comprehensive Review. Biointerface Res. Appl. Chem. 2022, 13, 119. [Google Scholar] [CrossRef]
- Gupta, G.; Siddiqui, M.A.; Khan, M.M.; Ajmal, M.; Ahsan, R.; Rahaman, M.A.; Ahmad, M.A.; Arshad, M.; Khushtar, M. Current Pharmacological Trends on Myricetin. Drug Res. 2020, 70, 448–454. [Google Scholar] [CrossRef]
- Ong, K.C.; Khoo, H.-E. Biological Effects of Myricetin. Gen. Pharmacol. Vasc. Syst. 1997, 29, 121–126. [Google Scholar] [CrossRef]
- Zhang, Q.-C.; Zhao, Y.; Bian, H.-M. Anti-Thrombotic Effect of a Novel Formula from Corni Fructus with Malic Acid, Succinic Acid and Citric Acid. Phytother. Res. 2014, 28, 722–727. [Google Scholar] [CrossRef]
- Wokoun, U.; Hellriegel, M.; Emons, G.; Gründker, C. Co-Treatment of Breast Cancer Cells with Pharmacologic Doses of 2-Deoxy-D-Glucose and Metformin: Starving Tumors. Oncol. Rep. 2017, 37, 2418–2424. [Google Scholar] [CrossRef]
- Zhang, J.; Li, L.; Kim, S.-H.; Hagerman, A.E.; Lü, J. Anti-Cancer, Anti-Diabetic and Other Pharmacologic and Biological Activities of Penta-Galloyl-Glucose. Pharm. Res. 2009, 26, 2066–2080. [Google Scholar] [CrossRef] [PubMed]
- Thevissen, K.; Marchand, A.; Chaltin, P.; Meert, E.M.K.; Cammue, B.P.A. Antifungal Carbazoles. Curr. Med. Chem. 2009, 16, 2205–2211. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, A.; Al Mahmud, Z.; Kumar Saha, S.; Abdur Rahman, S.M. Evaluation of Antinociceptive and Antidiarrhoeal Properties of Manilkara Zapota Leaves in Swiss Albino Mice. Pharm. Biol. 2016, 54, 1413–1419. [Google Scholar] [CrossRef] [PubMed]
- de Fátima Arrigoni-Blank, M.; Dmitrieva, E.G.; Franzotti, E.M.; Antoniolli, A.R.; Andrade, M.R.; Marchioro, M. Anti-Inflammatory and Analgesic Activity of Peperomia Pellucida (L.) HBK (Piperaceae). J. Ethnopharmacol. 2004, 91, 215–218. [Google Scholar] [CrossRef] [PubMed]
- Silva, V.G.; Silva, R.O.; Damasceno, S.R.; Carvalho, N.S.; Prudêncio, R.S.; Aragão, K.S.; Guimarães, M.A.; Campos, S.A.; Véras, L.M.; Godejohann, M. Anti-Inflammatory and Antinociceptive Activity of Epiisopiloturine, an Imidazole Alkaloid Isolated from Pilocarpus Microphyllus. J. Nat. Prod. 2013, 76, 1071–1077. [Google Scholar] [CrossRef]
- Fischer, L.G.; Leitão, R.; Etcheverry, S.R.; de Campos-Buzzi, F.; Vãzquez, A.A.; Heinzen, H.A.; Filho, V.C. Analgesic Properties of Extracts and Fractions from Erythrina Crista-Galli (Fabaceae) Leaves. Nat. Prod. Res. 2007, 21, 759–766. [Google Scholar] [CrossRef]
- Ahmadiani, A.; Hosseiny, J.; Semnanian, S.; Javan, M.; Saeedi, F.; Kamalinejad, M.; Saremi, S. Antinociceptive and Anti-Inflammatory Effects of Elaeagnus Angustifolia Fruit Extract. J. Ethnopharmacol. 2000, 72, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Daud, A.; Habib, N.; Riera, A.S. Anti-Inflammatory, Anti-Nociceptive and Antipyretic Effects of Extracts of Phrygilanthus Acutifolius Flowers. J. Ethnopharmacol. 2006, 108, 198–203. [Google Scholar] [CrossRef] [PubMed]
- McNamara, C.R.; Mandel-Brehm, J.; Bautista, D.M.; Siemens, J.; Deranian, K.L.; Zhao, M.; Hayward, N.J.; Chong, J.A.; Julius, D.; Moran, M.M. TRPA1 Mediates Formalin-Induced Pain. Proc. Natl. Acad. Sci. USA 2007, 104, 13525–13530. [Google Scholar] [CrossRef]
- Parvizpur, A.; Ahmadiani, A.; Kamalinejad, M. Probable Role of Spinal Purinoceptors in the Analgesic Effect of Trigonella Foenum (TFG) Leaves Extract. J. Ethnopharmacol. 2006, 104, 108–112. [Google Scholar] [CrossRef]
- Crovetti, G.; Martinelli, G.; Issi, M.; Barone, M.; Guizzardi, M.; Campanati, B.; Moroni, M.; Carabelli, A. Platelet Gel for Healing Cutaneous Chronic Wounds. Transfus. Apher. Sci. 2004, 30, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.J.; Heo, S.-I.; Wang, M.-H. Free Radical Scavenging and Total Phenolic Contents from Methanolic Extracts of Ulmus Davidiana. Food Chem. 2008, 108, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Haney, E.F.; Mansour, S.C.; Hancock, R.E. Antimicrobial Peptides: An Introduction. Antimicrob. Pept. 2017, 3–22. [Google Scholar]
- Shedoeva, A.; Leavesley, D.; Upton, Z.; Fan, C. Wound Healing and the Use of Medicinal Plants. Evid. Based Complement. Alternat. Med. 2019, 2019. [Google Scholar] [CrossRef]
- Babu, M.K.; Prasad, O.S.; Murthy, T.E. Comparison of the Dermal Wound Healing of Centella Asiatica Extract Impregnated Collagen and Cross Linked Collagen Scaffolds. J. Chem. Pharm. Res. 2011, 3, 353–362. [Google Scholar]
- Ramnath, V.; Sekar, S.; Sankar, S.; Sastry, T.P.; Mandal, A.B. In Vivo Evaluation of Composite Wound Dressing Material Containing Soya Protein and Sago Starch. Int. J. Pharm. Sci. 2012, 4, 414–419. [Google Scholar]
- Motealleh, B.; Zahedi, P.; Rezaeian, I.; Moghimi, M.; Abdolghaffari, A.H.; Zarandi, M.A. Morphology, Drug Release, Antibacterial, Cell Proliferation, and Histology Studies of Chamomile-loaded Wound Dressing Mats Based on Electrospun Nanofibrous Poly (ε-caprolactone)/Polystyrene Blends. J. Biomed. Mater. Res. B Appl. Biomater. 2014, 102, 977–987. [Google Scholar] [CrossRef]
- Brown, K.L.; Phillips, T.J. Nutrition and Wound Healing. Clin. Dermatol. 2010, 28, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, M.E.; Gottschlich, M.M.; Kopcha, R.; Khoury, J.; Warden, G.D. A Prospective Analysis of Serum Vitamin K in Severely Burned Pediatric Patients. J. Burn Care Rehabil. 1998, 19, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Caruelle, J.-P.; Barritault, D.; Jeanbat-Mimaud, V.; Cammas-Marion, S.; Langlois, V.; Guerin, P.; Barbaud, C. Bioactive Functionalized Polymer of Malic Acid for Bone Repair and Muscle Regeneration. J. Biomater. Sci. Polym. Ed. 2000, 11, 979–991. [Google Scholar] [CrossRef]
- Jeanbat-Mimaud, V.; Barbaud, C.; Caruelle, J.-P.; Barritault, D.; Cammas-Marion, S.; Guérin, P. Functionalized Polymers of Malic Acid Stimulate Tissue Repair Presumably by Regulating Heparin Growth Factors Bioavailability. In Biomedical Polymers and Polymer Therapeutics; Springer: Berlin/Heidelberg, Germany, 2002; pp. 243–251. [Google Scholar]
- Cattaneo, F.; De Marino, S.; Parisi, M.; Festa, C.; Castaldo, M.; Finamore, C.; Duraturo, F.; Zollo, C.; Ammendola, R.; Zollo, F. Wound Healing Activity and Phytochemical Screening of Purified Fractions of Sempervivum Tectorum L. Leaves on HCT 116. Phytochem. Anal. 2019, 30, 524–534. [Google Scholar] [CrossRef]
- Pereira, M.P.; Tavano, O.L. Use of Different Spices as Potential Natural Antioxidant Additives on Cooked Beans (Phaseolus Vulgaris). Increase of DPPH Radical Scavenging Activity and Total Phenolic Content. Plant Foods Hum. Nutr. 2014, 69, 337–343. [Google Scholar] [CrossRef]
- Marinova, D.; Ribarova, F.; Atanassova, M. Total phenolics and total flavonoids in bulgarian fruits and vegetables. JU Chem. Metal 2005, 40, 255–260. [Google Scholar]
- Papuc, C.; Predescu, C.; Nicorescu, V.; Stefan, G.; Nicorescu, I. Antioxidant Properties of a Parsley (Petroselinum crispum) Juice Rich in Polyphenols and Nitrites. Curr. Res. Nutr. Food Sci. J. 2016, 4, 114–118. [Google Scholar] [CrossRef]
- Lafraxo, H.; Bakour, M.; Laaroussi, H.; El Ghouizi, A.; Ousaaid, D.; Aboulghazi, A.; Lyoussi, B. The Synergistic Beneficial Effect of Thyme Honey and Olive Oil against Diabetes and Its Complications Induced by Alloxan in Wistar Rats. Evid. Based Complement. Alternat. Med. 2021, 2021. [Google Scholar] [CrossRef]
- Lee, C.E.; Petersen, C.H. Effects of Developmental Acclimation on Adult Salinity Tolerance in the Freshwater-Invading Copepod Eurytemora Affinis. Physiol. Biochem. Zool. 2003, 76, 296–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanachi, P.; Golkho, S.H. Using HPLC to Determination the Composition and Antioxidant Activity of Berberis Vulgaris. Eur. J. Sci. Res. 2009, 29, 47–54. [Google Scholar]
- Kazemi, M.; Hadavi, E.; Hekmati, J. Effect of Salicylic Acid, Malic Acid, Citric Acid and Sucrose on Antioxidant Activity, Membrane Stability and ACC-Oxidase Activity in Relation to Vase Life of Carnation Cut Flowers. J. Plant Sci. 2012, 7, 78–84. [Google Scholar] [CrossRef]
- Al-Juhaimi, F.; Ghafoor, K. Total Phenols and Antioxidant Activities of Leaf and Stem Extracts from Coriander, Mint and Parsley Grown in Saudi Arabia. Pak J Bot 2011, 43, 2235–2237. [Google Scholar]
- Wong, P.Y.Y.; Kitts, D.D. Studies on the Dual Antioxidant and Antibacterial Properties of Parsley (Petroselinum Crispum) and Cilantro (Coriandrum Sativum) Extracts. Food Chem. 2006, 97, 505–515. [Google Scholar] [CrossRef]
- Agyare, C.; Appiah, T.; Boakye, Y.D.; Apenteng, J.A. Chapter 25 - Petroselinum Crispum: A Review. In Medicinal Spices and Vegetables from Africa; Kuete, V., Ed.; Academic Press: Cambridge, MA, USA, 2017; pp. 527–547. ISBN 978-0-12-809286-6. [Google Scholar]
- Marín, I.; Sayas-Barberá, E.; Viuda-Martos, M.; Navarro, C.; Sendra, E. Chemical Composition, Antioxidant and Antimicrobial Activity of Essential Oils from Organic Fennel, Parsley, and Lavender from Spain. Foods 2016, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Herken, E.N.; Guzel, S. Total Antioxidant Capacity and Total Phenol Contents of Selected Commercial Fruit Juices in Turkey. Int. J. Food Prop. 2010, 13, 1373–1379. [Google Scholar] [CrossRef]
- Atef, N.M.; Shanab, S.M.; Negm, S.I.; Abbas, Y.A. Evaluation of Antimicrobial Activity of Some Plant Extracts against Antibiotic Susceptible and Resistant Bacterial Strains Causing Wound Infection. Bull. Natl. Res. Cent. 2019, 43, 144. [Google Scholar] [CrossRef]
- Keita, K.; Darkoh, C.; Okafor, F. Secondary Plant Metabolites as Potent Drug Candidates against Antimicrobial-Resistant Pathogens. SN Appl. Sci. 2022, 4, 1–10. [Google Scholar] [CrossRef]
- Chaillot, J.; Tebbji, F.; Remmal, A.; Boone, C.; Brown, G.W.; Bellaoui, M.; Sellam, A. The Monoterpene Carvacrol Generates Endoplasmic Reticulum Stress in the Pathogenic Fungus Candida Albicans. Antimicrob. Agents Chemother. 2015, 59, 4584–4592. [Google Scholar] [CrossRef]
- Lv, F.; Liang, H.; Yuan, Q.; Li, C. In Vitro Antimicrobial Effects and Mechanism of Action of Selected Plant Essential Oil Combinations against Four Food-Related Microorganisms. Food Res. Int. 2011, 44, 3057–3064. [Google Scholar] [CrossRef]
- Moussii, I.M.; Nayme, K.; Timinouni, M.; Jamaleddine, J.; Filali, H.; Hakkou, F. Synergistic Antibacterial Effects of Moroccan Artemisia Herba Alba, Lavandula Angustifolia and Rosmarinus Officinalis Essential Oils. Synergy 2020, 10, 100057. [Google Scholar] [CrossRef]
- Viuda-Martos, M.; Mohamady, M.A.; Fernández-López, J.; Abd ElRazik, K.A.; Omer, E.A.; Pérez-Alvarez, J.A.; Sendra, E. In Vitro Antioxidant and Antibacterial Activities of Essentials Oils Obtained from Egyptian Aromatic Plants. Food Control 2011, 22, 1715–1722. [Google Scholar] [CrossRef]
- Mostafa, I.; Abbas, H.A.; Ashour, M.L.; Yasri, A.; El-Shazly, A.M.; Wink, M.; Sobeh, M. Polyphenols from Salix Tetrasperma Impair Virulence and Inhibit Quorum Sensing of Pseudomonas Aeruginosa. Molecules 2020, 25, 1341. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Peak | Molecules | Formula | Rt (min) | [M-H]- (m/z) | SI | Typical MS/MS | Area under Curve |
|---|---|---|---|---|---|---|---|
| 1 | Naringin | C27H32O14 | 1.108 | 579.00 | 579.2 → 124.89 | 271 | 27,397,987 |
| 2 | Oleuropein | C25H32O13 | 1.115 | 539.00 | 539 → 179 | 307 | 56,757,543 |
| 3 | Myricetin | C15H10O8 | 1.384 | 317.00 | 317 →150.8 | 287 | 3,417,929 |
| 4 | Arbutin | C12H16O7 | 1.939 | 271.20 | 271.2 →144.9 | 162 | 28,442,471 |
| Peak | Name | Formula | Rt (min) | Area % |
|---|---|---|---|---|
| 1 | l-Alanine, N-(trimethylsilyl) | C9H23NO2Si2 | 7.430 | 0.51 |
| 2 | Cyclotetrasiloxane, octamethyl | C8H24O4Si4 | 8.148 | 1.60 |
| 3 | Propanedioic acid, bis(trimethylsilyl) | C9H20O4Si2 | 8.417 | 1.08 |
| 4 | L-Valine, N-trimethylsilyl | C11H27NO2Si2 | 8.558 | 0.72 |
| 5 | Propanephosphonic acid, bis(trimethylsilyl) | C9H25O3PSi2 | 9.088 | 12.57 |
| 6 | L-Isoleucine, N-(trimethylsilyl) | C12H29NO2Si2 | 9.248 | 0.62 |
| 7 | Butanedioic acid, bis(trimethylsilyl) | C10H22O4Si2 | 9.317 | 0.75 |
| 8 | L-Proline, 1-(trimethylsilyl) | C11H25NO2Si2 | 9.361 | 0.98 |
| 9 | Benzonitrile | C18H18N2 | 9.594 | 0.62 |
| 10 | Malic acid, tris(trimethylsilyl) ester | C13H30O5Si3 | 10.730 | 13.52 |
| 11 | 2,3,4-Trihydroxybutyric acid tetraTMS | C16H40O5Si4 | 11.260 | 0.56 |
| 12 | D-Ribofuranose, 1,2,3,5-tetrakis-O-(trimethylsilyl) | C17H42O5Si4 | 12.918 | 5.62 |
| 13 | β-D-Galactofuranoside, ethyl 2,3,5,6-tetrakis-O-(trimethylsilyl) | C20H48O6Si4 | 13.019 | 13.29 |
| 14 | 9H-Carbazole, 9-phenyl- alcaloide | C18H13N | 13.220 | 3.04 |
| 15 | Talose, 2,3,4,5,6-pentakis-O-(trimethylsilyl) | C21H52O6Si5 | 13.400 | 9.75 |
| 16 | D-Mannitol, 1,2,3,4,5,6-hexakis-O-(trimethylsilyl) | C24H62O6Si6 | 13.653 | 10.95 |
| 17 | D-Glucose, 2,3,4,5,6-pentakis-O-(trimethylsilyl) | C21H52O6Si5 | 13.782 | 13.52 |
| 18 | D-gluconic acid 6TMS | C24H60O7Si6 | 14.071 | 1.31 |
| 19 | Myo-Inositol, 1,2,3,4,5,6-hexakis-O-(trimethylsilyl) | C24H60O6Si6 | 14.549 | 1.19 |
| 20 | Mannoonic acid, 2,3,5,6-tetrakis-O-(trimethylsilyl) | C18H42O6Si4 | 18.050 | 7.70 |
| Total | 99.9 | |||
| Extract | DPPH | FRAP |
|---|---|---|
| IC50 (µg/mL) | EC50 (mg/mL) | |
| Hydro-ethanolic extract | 19.38 ± 0.15 | 5.34 ± 0.40 |
| Polyphenols | 40.36 ± 1.47 | 4.91 ± 0.40 |
| BHT | 01.97 ± 0.10 | – |
| Ascorbic acid | – | 1.43 ± 0.02 |
| Inhibition Zone Diameter in mm | |||
|---|---|---|---|
| Fractions | Gram-Negative Bacteria | Gram-Positive Bacteria | Fungi |
| P. aeruginosa | S. aureus | C. albicans | |
| Hydro-ethanolic extract | 12.33 ± 0.33 a | 0.00 ± 0.00 b | 9.33 ± 0.33 ab |
| Polyphenols | 14.00 ± 0.33 a | 9 ± 0.16 a | 13 ± 0.57 a |
| Streptomycin (1 mg/mL) | 14.67 ± 0.17 a | 16 ± 0.57 a | __ |
| Fluconazole (5 mg/mL) | __ | __ | 21 ± 1.2 a |
| Minimum Inhibitory Concentration (MIC) in mg/mL | |||
|---|---|---|---|
| Fractions | Gram-Negative Bacteria | Gram-Positive Bacteria | Fungi |
| P. aeruginosa | S. aureus | C. albicans | |
| Hydro-ethanolic extract | 12.5 | Resistant | 6.25 |
| Polyphenols | 6.25 | 3.125 | 6.25 |
| Streptomycin | 0.625 | 0.15 | __ |
| Fluconazole | __ | __ | 0.31 |
| Treatment | Dose (mg/kg) | Number of Writes |
|---|---|---|
| Control | 65.00 ± 2.88 c | |
| Tramadol | 10 | 17.33 ± 1.45 a |
| Hydro-ethanolic extract | 500 | 50.00 ± 0.57 bc |
| 1000 | 39.67 ± 0.88 b | |
| Polyphenols | 200 | 46.00 ± 3.05 b |
| Treatment | Dose (mg/kg) | Licking Time (s) | |
|---|---|---|---|
| First Phase (0–5 min) | Second Phase (15–30 min) | ||
| Control | 58.00 ± 0.5 c | 30.33 ± 2.5 c | |
| Tramadol | 10 | 10.33 ± 0.8 a | 4.33 ± 1.7 a |
| Hydro-ethanolic extract | 500 | 49.67 ± 1.4 b | 21.67 ± 2.1 b |
| 1000 | 38.67 ± 1.7 b | 19.00 ± 1.1 b | |
| Polyphenols | 200 | 43.00 ± 1.1 bc | 21.00 ± 0.5 b |
| Wound Size in cm2 | ||||||
|---|---|---|---|---|---|---|
| Treatments | Day 1 | Day 5 | Day 10 | Day 15 | Day 20 | Day 25 |
| Negative Control | 1.91 ± 0.15 a | 1.70 ± 0.18 a | 1.26 ± 0.03 a | 0.62 ± 0.05 a | 0.46 ± 0.03 a | 0.37 ± 0.06 a |
| Madecassol® (1%) | 2.27 ± 0.12 a | 1.59 ± 0.09 a | 1.14 ± 0.11 a | 0.46 ± 0.10 a | 0.37 ± 0.04 a | 0.13 ± 0.03 b |
| Hydro-ethanolic extract (10%) | 2.83 ± 0.03 a | 1.52 ± 0.06 a | 0.49 ± 0.10 b | 0.36 ± 0.05 a | 0.23 ± 0.05 a | 0.08 ± 0.02 b |
| Polyphenolic extract | 2.79 ± 0.46 a | 1.71 ± 0.23 a | 0.83 ± 0.15 ab | 0.58 ± 0.19 a | 0.36 ± 0.13 a | 0.14 ± 0.03 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Slighoua, M.; Mahdi, I.; Moussaid, F.Z.; Kamaly, O.A.; Amrati, F.E.-z.; Conte, R.; Drioiche, A.; Saleh, A.; Housseini, A.I.; Bari, A.; et al. LC-MS/MS and GC/MS Profiling of Petroselinum sativum Hoffm. and Its Topical Application on Burn Wound Healing and Related Analgesic Potential in Rats. Metabolites 2023, 13, 260. https://doi.org/10.3390/metabo13020260
Slighoua M, Mahdi I, Moussaid FZ, Kamaly OA, Amrati FE-z, Conte R, Drioiche A, Saleh A, Housseini AI, Bari A, et al. LC-MS/MS and GC/MS Profiling of Petroselinum sativum Hoffm. and Its Topical Application on Burn Wound Healing and Related Analgesic Potential in Rats. Metabolites. 2023; 13(2):260. https://doi.org/10.3390/metabo13020260
Chicago/Turabian StyleSlighoua, Meryem, Ismail Mahdi, Fatima Zahrae Moussaid, Omkulthom Al Kamaly, Fatima Ez-zahra Amrati, Raffaele Conte, Aziz Drioiche, Asmaa Saleh, Abdelilah Iraqi Housseini, Amina Bari, and et al. 2023. "LC-MS/MS and GC/MS Profiling of Petroselinum sativum Hoffm. and Its Topical Application on Burn Wound Healing and Related Analgesic Potential in Rats" Metabolites 13, no. 2: 260. https://doi.org/10.3390/metabo13020260