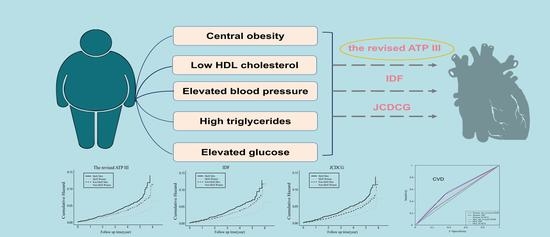
Comparison of the Three Most Commonly Used Metabolic Syndrome Definitions in the Chinese Population: A Prospective Study
Abstract
:1. Introduction
2. Results
2.1. Baseline Characteristics and Incidence of Cardiovascular Events
2.2. MetS Defined with Different Definitions and the Risk of CVD
2.3. ROC Analysis
3. Discussion
4. Materials and Methods
4.1. Design and Study Population
4.2. Data Collection
4.3. Ascertainment of Cardiovascular Outcomes
4.4. Statistical Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Guo, Z.; Wu, M.; Hu, X.; Xu, Y.; Zhou, Z. Interaction of smoking and metabolic syndrome on cardiovascular risk in a Chinese cohort. Int. J. Cardiol. 2013, 167, 250–253. [Google Scholar] [CrossRef]
- McNeill, A.M.; Rosamond, W.D.; Girman, C.J.; Golden, S.H.; Schmidt, M.I.; East, H.E.; Ballantyne, C.M.; Heiss, G. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care 2005, 28, 385–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, R.; Li, W.; Lun, Z.; Zhang, H.; Sun, Z.; Kanu, J.S.; Qiu, S.; Cheng, Y.; Liu, Y. Prevalence of metabolic syndrome in Mainland China: A meta-analysis of published studies. BMC Public Health 2016, 16, 296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. A J. Br. Diabet. Assoc. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Zimmet, P.; Shaw, J. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Zhu, J.; Gao, R.; Zhao, S.; Lu, G.; Zhao, D.; Li, J. Chinese guidelines on prevention and treatment of dyslipidemia in adults (2016 Revised Edition) Chin. Circ. J. 2016, 31, 937–953. [Google Scholar]
- Balkau, B.; Charles, M.A. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet Med. 1999, 16, 442–443. [Google Scholar] [CrossRef]
- Einhorn, D.; Reaven, G.M.; Cobin, R.H.; Ford, E.; Ganda, O.P.; Handelsman, Y.; Hellman, R.; Jellinger, P.S.; Kendall, D.; Krauss, R.M.; et al. American College of Endocrinology position statement on the insulin resistance syndrome. Endocr. Pract. 2003, 9, 237–252. [Google Scholar] [CrossRef] [PubMed]
- Asato, C.B.H.; Nelson-Hurwitz, D.C.; Lee, T.; Grandinetti, A. Comparative Analysis of Metabolic Syndrome Diagnostic Criteria and Its Effects on Prevalence in a Multiethnic Population. Metab. Syndr. Relat. Disord. 2021, 19, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Haverinen, E.; Paalanen, L.; Palmieri, L.; Padron-Monedero, A.; Noguer-Zambrano, I.; Sarmiento Suárez, R.; Tolonen, H. Comparison of metabolic syndrome prevalence using four different definitions—A population-based study in Finland. Arch. Public Health 2021, 79, 231. [Google Scholar] [CrossRef] [PubMed]
- Cissé, K.; Samadoulougou, D.R.S.; Bognini, J.D.; Kangoye, T.D.; Kirakoya-Samadoulougou, F. Using the first nationwide survey on non-communicable disease risk factors and different definitions to evaluate the prevalence of metabolic syndrome in Burkina Faso. PLoS ONE 2021, 16, e0255575. [Google Scholar] [CrossRef]
- Saukkonen, T.; Jokelainen, J.; Timonen, M.; Cederberg, H.; Laakso, M.; Härkönen, P.; Keinänen-Kiukaanniemi, S.; Rajala, U. Prevalence of metabolic syndrome components among the elderly using three different definitions: A cohort study in Finland. Scand. J. Prim. Health Care 2012, 30, 29–34. [Google Scholar] [CrossRef] [Green Version]
- Jiang, S.; Zhang, L.; Shao, L.; Yan, L.J.; Yldos, A.; Xie, Z.J. Epidemiological investigation and comparison of three different diagnostic criteria regarding metabolic syndrome among population age 30–80 in Xinjiang Uigur areas. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi 2011, 32, 756–759. [Google Scholar]
- Wen, J.; Yang, J.; Shi, Y.; Liang, Y.; Wang, F.; Duan, X.; Lu, X.; Tao, Q.; Lu, X.; Tian, Y.; et al. Comparisons of different metabolic syndrome definitions and associations with coronary heart disease, stroke, and peripheral arterial disease in a rural Chinese population. PLoS ONE 2015, 10, e0126832. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, L.; Wang, Z.; Wang, X.; Chen, Z.; Shao, L.; Tian, Y.; Zheng, C.; Chen, L.; Zhou, H.; et al. The prevalence and characteristics of metabolic syndrome according to different definitions in China: A nationwide cross-sectional study, 2012-2015. BMC Public Health 2022, 22, 1869. [Google Scholar] [CrossRef]
- Yu, S.; Guo, X.; Li, G.; Yang, H.; Zheng, L.; Sun, Y. Gender discrepancy in the predictive effect of metabolic syndrome and its components on newly onset cardiovascular disease in elderly from rural China. BMC Geriatr. 2021, 21, 505. [Google Scholar] [CrossRef]
- Wang, C.; Hou, X.; Bao, Y.; Pan, J.; Zuo, Y.; Zhong, W.; Jia, W.; Xiang, K. The metabolic syndrome increased risk of cardiovascular events in Chinese—A community based study. Int. J. Cardiol. 2010, 139, 159–165. [Google Scholar] [CrossRef]
- Liu, Q.; Li, Y.X.; Hu, Z.H.; Jiang, X.Y.; Li, S.J.; Wang, X.F. Comparing associations of different metabolic syndrome definitions with ischemic stroke in Chinese elderly population. Eur. J. Intern. Med. 2018, 47, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.L.; Wang, C.C.; Chiang, S.T.; Wang, Y.C.; Sun, Y.S.; Wu, W.T.; Liou, S.H. The impact of occupational psychological hazards and metabolic syndrome on the 8-year risk of cardiovascular diseases-A longitudinal study. PLoS ONE 2018, 13, e0202977. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Gao, B.; Wang, L.; Xing, Y.; Ming, J.; Zhou, J.; Fu, J.; Li, X.; Xu, S.; Liu, G.; et al. Agreement Between the JCDCG, Revised NCEP-ATPIII, and IDF Definitions of Metabolic Syndrome in a Northwestern Chinese Population. Diabetes Ther. Res. Treat. Educ. Diabetes Relat. Disord. 2018, 9, 1457–1468. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.; Lu, J.; Weng, J.; Ji, L.; Shan, Z.; Liu, J.; Tian, H.; Ji, Q.; Zhu, D.; Ge, J.; et al. Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in Chinese adults: A national diabetes and metabolic disorders survey. PLoS ONE 2013, 8, e57319. [Google Scholar] [CrossRef]
- Wu, L.T.; Shen, Y.F.; Hu, L.; Zhang, M.Y.; Lai, X.Y. Prevalence and associated factors of metabolic syndrome in adults: A population-based epidemiological survey in Jiangxi province, China. BMC Public Health 2020, 20, 133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ford, E.S.; Li, C.; Zhao, G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J. Diabetes 2010, 2, 180–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levesque, J.; Lamarche, B. The metabolic syndrome: Definitions, prevalence and management. J. Nutr. Nutr. 2008, 1, 100–108. [Google Scholar] [CrossRef]
- Khosravi-Boroujeni, H.; Ahmed, F.; Sadeghi, M.; Roohafza, H.; Talaei, M.; Dianatkhah, M.; Pourmogaddas, A.; Sarrafzadegan, N. Does the impact of metabolic syndrome on cardiovascular events vary by using different definitions? BMC Public Health 2015, 15, 1313. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Chair, S.Y.; Wong, E.M.; Li, X.; Liu, M.; Zhang, Y. Comparing the predictive abilities of different metabolic syndrome definitions for acute coronary syndrome: A case-control study in Chinese adults. Metab. Syndr. Relat. Disord. 2014, 12, 390–396. [Google Scholar] [CrossRef]
- Maruyama, K.; Uchiyama, S.; Iwata, M. Metabolic syndrome and its components as risk factors for first-ever acute ischemic noncardioembolic stroke. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2009, 18, 173–177. [Google Scholar] [CrossRef]
- Guembe, M.J.; Fernandez-Lazaro, C.I.; Sayon-Orea, C.; Toledo, E.; Moreno-Iribas, C. Risk for cardiovascular disease associated with metabolic syndrome and its components: A 13-year prospective study in the RIVANA cohort. Cardiovasc. Diabetol. 2020, 19, 195. [Google Scholar] [CrossRef] [PubMed]
- Lind, L.; Sundström, J.; Ärnlöv, J.; Risérus, U.; Lampa, E. A longitudinal study over 40 years to study the metabolic syndrome as a risk factor for cardiovascular diseases. Sci. Rep. 2021, 11, 2978. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Chen, Z.; Zhang, L.; Wang, X.; Hao, G.; Zhang, Z.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.; et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhang, L.; Chen, Z.; Wang, X.; Shao, L.; Guo, M.; Zhu, M.; Gao, R. Survey on prevalence of hypertension in China: Background, aim, method and design. Int. J. Cardiol. 2014, 174, 721–723. [Google Scholar] [CrossRef]
- Dong, Y.; Wang, Z.; Chen, Z.; Wang, X.; Zhang, L.; Nie, J.; Zheng, C.; Wang, J.; Shao, L.; Tian, Y.; et al. Comparison of visceral, body fat indices and anthropometric measures in relation to chronic kidney disease among Chinese adults from a large scale cross-sectional study. BMC Nephrol. 2018, 19, 40. [Google Scholar] [CrossRef] [Green Version]
- Zhou, X.-H.; A.Obuchowski, N.; McClish, D.K. Statistical Methods in Diagnostic Medicine, 2nd ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011; p. 51. [Google Scholar] [CrossRef]


| AHA/NHLBI, The Revised ATP III | IDF | JCDCG | |
|---|---|---|---|
| To be identified as MetS | Any 3 of the following features | Central obesity plus 2 more | Any 3 of the following features |
| Central obesity | WC ≥ 90 cm for men and WC ≥ 80 cm for women | WC ≥ 90 cm for men and WC ≥ 80 cm for women | WC ≥ 90 cm for men and WC ≥ 85 cm for women |
| High triglycerides | TG > 1.7 mmol/L or receipt of specific treatment for this lipid abnormality | >1.7 mmol/L or receipt of specific treatment for this lipid abnormality | ≥1.7 mmol/L or receipt of specific treatment for this lipid abnormality |
| Low HDL cholesterol | HDL-C < 40 mg/dL (1.03 mmol/L) in men, HDL-C < 50 mg/dL (1.3 mmol/L) in women, or receipt of drug treatment for reduced HDL-C | HDL-C < 40 mg/dL (1.03 mmol/L) in men, HDL-C < 50 mg/dL (1.29 mmol/L) in women, or specific treatment for this lipid abnormality | HDL-C < 1.0 mmol/l or specific treatment for this lipid abnormality |
| Elevated blood pressure | BP ≥ 130/85 mmHg or treatment of previously diagnosed hypertension | BP ≥ 130/85 mmHg or treatment of previously diagnosed hypertension | BP ≥ 130/85 mmHg or treatment of previously diagnosed hypertension |
| Elevated glucose | FPG ≥ 5.6 mmol/dL or drug treatment for elevated glucose | ≥5.6 mmol/L or previously diagnosed diabetes mellitus | ≥6.1 mmol/L or previously diagnosed diabetes mellitus |
| Overall (N = 20,888) | Men (N = 9713) | Women (N = 11,175) | p-Value | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age (years) | 56.3 ± 13.1 | 56.8 ± 13.3 | 55.9 ± 12.9 | <0.001 |
| Region (n%) | <0.001 | |||
| East | 8478 (40.6) | 3960 (40.8) | 4518 (40.4) | |
| Central | 8804 (42.1) | 4205 (43.3) | 4599 (41.2) | |
| West | 3606 (17.3) | 1548 (15.9) | 2058 (18.4) | |
| Area (n%) | <0.001 | |||
| Urban | 9347 (44.7) | 4469 (46.0) | 4878 (43.7) | |
| Rural | 11541 (55.3) | 5244 (54.0) | 6297 (56.3) | |
| Education level (n%) | <0.001 | |||
| Middle school or below | 16650 (79.7) | 7388 (76.1) | 9262 (82.9) | |
| High school or vocational school | 2922 (14.0) | 1567 (16.1) | 1355 (12.1) | |
| College and above | 1316 (6.3) | 758 (7.8) | 558 (5.0) | |
| Smoking status (n%) | 4828 (23.1) | 4461 (45.9) | 367 (3.3) | <0.001 |
| Alcohol consumption (n%) | 4131 (19.8) | 3722 (38.3) | 409 (3.7) | <0.001 |
| Statin use (n%) | 356 (1.7) | 158 (1.6) | 198 (1.8) | 0.450 |
| Waist circumference (cm) | 84.1 ± 10.1 | 85.8 ± 9.94 | 82.7 ± 10.1 | <0.001 |
| Total cholesterol (mmol/L) | 4.81 ± 0.971 | 4.73 ± 0.932 | 4.88 ± 0.998 | <0.001 |
| Triglycerides a (mmol/L) | 1.15 (0.820, 1.700) | 1.15 (0.810, 1.77) | 1.15 (0.830, 1.66) | 0.312 |
| HDL-C (mmol/L) | 1.35 ± 0.337 | 1.31 ± 0.339 | 1.39 ± 0.331 | <0.001 |
| LDL-C (mmol/L) | 2.82 ± 0.814 | 2.76 ± 0.789 | 2.86 ± 0.832 | <0.001 |
| Fasting glucose a (mmol/L) | 5.27 (4.87, 5.79) | 5.32 (4.89, 5.85) | 5.24 (4.86, 5.73) | <0.001 |
| Systolic BP (mmHg) | 133 ± 20.0 | 133 ± 19.0 | 132 ± 20.9 | <0.001 |
| Diastolic BP (mmHg) | 77.8 ± 11.0 | 79.8 ± 11.1 | 76.0 ± 10.7 | <0.001 |
| BMI (kg/m2) | 24.6 ± 3.48 | 24.5 ± 3.38 | 24.8 ± 3.57 | <0.001 |
| Family history of cardiovascular disease (n%) | 3130 (15.0) | 1288 (13.3) | 1842 (16.5) | <0.001 |
| MetS—Revised ATP III defined (n%) | 7131 (34.1) | 2741 (28.2) | 4390 (39.3) | <0.001 |
| MetS—IDF defined (n%) | 6058 (29.0) | 2125 (21.9) | 3933 (35.2) | <0.001 |
| MetS—JCDCG defined (n%) | 4633 (22.2) | 2275 (23.4) | 2358 (21.1) | <0.001 |
| Incidence of cardiovascular events | ||||
| Coronary heart disease (n%) | 275 (1.3) | 163 (1.7) | 112 (1.0) | <0.001 |
| Stroke (n%) | 560 (2.7) | 318 (3.3) | 242 (2.2) | <0.001 |
| Cardiovascular disease (n%) | 925 (4.4) | 530 (5.5) | 395 (3.5) | <0.001 |
| Cases/PYs (/1000) | HR (95% CI) | ||||
|---|---|---|---|---|---|
| MetS | Non-MetS | Crude Model | Model 1 | ||
| Revised ATP III | Cardiovascular disease | ||||
| Total | 12.11 | 8.26 | 1.47 (1.29, 1.67) *** | 1.36 (1.19, 1.56) *** | |
| Men | 14.20 | 10.91 | 1.31 (1.09, 1.57) ** | 1.33 (1.11, 1.60) ** | |
| Women | 10.81 | 5.55 | 1.94 (1.59, 2.37) *** | 1.37 (1.11, 1.67) ** | |
| Stroke | |||||
| Total | 7.46 | 4.87 | 1.53 (1.30, 1.81) *** | 1.44 (1.21, 1.71) *** | |
| Men | 8.78 | 6.35 | 1.39 (1.11, 1.75) ** | 1.46 (1.16, 1.85) ** | |
| Women | 6.63 | 3.35 | 1.97 (1.53, 2.54) *** | 1.37 (1.06, 1.78) * | |
| Coronary heart disease | |||||
| Total | 3.73 | 2.33 | 1.60 (1.26, 2.03) *** | 1.45 (1.13, 1.85) ** | |
| Men | 4.67 | 3.16 | 1.48 (1.08, 2.03) * | 1.36 (0.98, 1.88) | |
| Women | 3.1 | 1.48 | 2.12 (1.46, 3.08) *** | 1.43 (0.98, 2.11) | |
| IDF | Cardiovascular disease | ||||
| Total | 12.11 | 8.53 | 1.42 (1.24, 1.62) *** | 1.37 (1.19, 1.58) *** | |
| Men | 14.19 | 11.18 | 1.27 (1.05, 1.54) * | 1.33 (1.09, 1.62) ** | |
| Women | 10.99 | 5.79 | 1.90 (1.56, 2.31) *** | 1.37 (1.12, 1.68) ** | |
| Stroke | |||||
| Total | 7.43 | 5.06 | 1.47 (1.24, 1.74) *** | 1.43 (1.19, 1.71) *** | |
| Men | 8.68 | 6.57 | 1.32 (1.03, 1.69) * | 1.43 (1.11, 1.85) ** | |
| Women | 6.76 | 3.49 | 1.93 (1.50, 2.49) *** | 1.39 (1.07, 1.79) * | |
| Coronary heart disease | |||||
| Total | 3.69 | 2.45 | 1.50 (1.18, 1.92) *** | 1.42 (1.10, 1.82) ** | |
| Men | 4.50 | 3.33 | 1.35 (0.96, 1.90) | 1.26 (0.89, 1.79) | |
| Women | 3.25 | 1.53 | 1.93 (1.50, 2.49) *** | 1.48 (1.02, 2.17) * | |
| JCDCG | Cardiovascular disease | ||||
| Total | 13.40 | 8.49 | 1.59 (1.38, 1.83) *** | 1.36 (1.18, 1.57) *** | |
| Men | 14.81 | 10.94 | 1.36 (1.13, 1.64) ** | 1.38 (1.14, 1.67) ** | |
| Women | 12.05 | 6.45 | 1.88 (1.52, 2.32) *** | 1.30 (1.05, 1.61) * | |
| Stroke | |||||
| Total | 7.93 | 5.13 | 1.55 (1.30, 1.86) *** | 1.34 (1.12, 1.61) ** | |
| Men | 9.12 | 6.40 | 1.43 (1.13, 1.82) ** | 1.50 (1.18, 1.92) ** | |
| Women | 6.79 | 4.07 | 1.68 (1.28, 2.20) *** | 1.14 (0.86, 1.50) | |
| Coronary heart disease | |||||
| Total | 4.31 | 2.39 | 1.81 (1.41, 2.32) *** | 1.49 (1.15, 1.92) ** | |
| Men | 4.72 | 3.24 | 1.45 (1.04, 2.03) * | 1.32 (0.94, 1.85) | |
| Women | 3.92 | 1.66 | 2.35 (1.61, 3.45) *** | 1.59 (1.08, 2.35) * | |
| Total | Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| The Revised ATP III | IDF | JCDCG | The Revised ATP III | IDF | JCDCG | The Revised ATP III | IDF | JCDCG | |
| Cardiovascular disease | |||||||||
| Sensitivity | 43.14% | 36.65% | 30.70% | 33.77% | 26.23% | 29.06% | 55.70% | 50.63% | 32.91% |
| Specificity | 66.28% | 71.35% | 78.35% | 72.10% | 78.37% | 77.04% | 61.32% | 65.37% | 79.46% |
| Positive predictive value | 5.60% | 5.60% | 6.17% | 6.53% | 6.54% | 6.81% | 5.01% | 5.09% | 5.55% |
| Negative predictive value | 96.18% | 96.05% | 96.06% | 94.97% | 94.85% | 94.95% | 97.42% | 97.31% | 97.00% |
| ROC curve distance | 0.6611 | 0.6953 | 0.7260 | 0.7186 | 0.7688 | 0.7456 | 0.5881 | 0.603 | 0.7016 |
| Stroke | |||||||||
| Sensitivity | 44.29% | 37.50% | 30.36% | 35.22% | 27.04% | 30.19% | 56.20% | 51.24% | 30.58% |
| Specificity | 66.28% | 71.23% | 78.18% | 72.02% | 78.30% | 76.95% | 61.09% | 65.16% | 79.24% |
| Positive predictive value | 3.48% | 3.47% | 3.69% | 4.09% | 4.05% | 4.24% | 3.10% | 3.15% | 3.16% |
| Negative predictive value | 97.73% | 97.64% | 97.60% | 97.05% | 96.94% | 97.02% | 98.44% | 98.37% | 98.10% |
| ROC curve distance | 0.6513 | 0.6880 | 0.7298 | 0.7057 | 0.7612 | 0.7352 | 0.5859 | 0.5993 | 0.7246 |
| Coronary heart disease | |||||||||
| Sensitivity | 45.45% | 38.18% | 33.82% | 36.81% | 27.61% | 30.67% | 58.04% | 53.57% | 38.39% |
| Specificity | 66.01% | 71.12% | 78.11% | 71.93% | 78.22% | 76.84% | 60.91% | 64.99% | 79.20% |
| Positive predictive value | 1.75% | 1.73% | 2.02% | 2.19% | 2.12% | 2.21% | 1.48% | 1.53% | 1.83% |
| Negative predictive value | 98.91% | 98.85% | 98.88% | 98.52% | 98.44% | 98.48% | 99.31% | 99.28% | 99.22% |
| ROC curve distance | 0.6427 | 0.6823 | 0.6971 | 0.6915 | 0.7560 | 0.7309 | 0.5735 | 0.5815 | 0.6502 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.; Chen, Z.; Wang, X.; Zheng, C.; Shao, L.; Tian, Y.; Cao, X.; Tian, Y.; Gao, R.; Zhang, L.; et al. Comparison of the Three Most Commonly Used Metabolic Syndrome Definitions in the Chinese Population: A Prospective Study. Metabolites 2023, 13, 12. https://doi.org/10.3390/metabo13010012
Huang Y, Chen Z, Wang X, Zheng C, Shao L, Tian Y, Cao X, Tian Y, Gao R, Zhang L, et al. Comparison of the Three Most Commonly Used Metabolic Syndrome Definitions in the Chinese Population: A Prospective Study. Metabolites. 2023; 13(1):12. https://doi.org/10.3390/metabo13010012
Chicago/Turabian StyleHuang, Yilin, Zuo Chen, Xin Wang, Congying Zheng, Lan Shao, Ye Tian, Xue Cao, Yixin Tian, Runlin Gao, Linfeng Zhang, and et al. 2023. "Comparison of the Three Most Commonly Used Metabolic Syndrome Definitions in the Chinese Population: A Prospective Study" Metabolites 13, no. 1: 12. https://doi.org/10.3390/metabo13010012