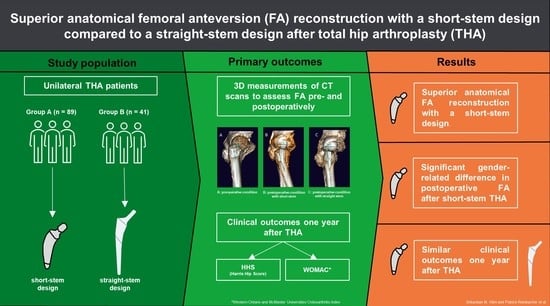
Femoral Anteversion in Total Hip Arthroplasty: Retrospective Comparison of Short- and Straight-Stem Models Using CT Scans
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kurtz, S.M.; Ong, K.L.; Lau, E.; Bozic, K.J. Impact of the Economic Downturn on Total Joint Replacement Demand in the United States: Updated Projections to 2021. J. Bone Joint Surg. Am. 2014, 96, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Sakalkale, D.P.; Sharkey, P.F.; Eng, K.; Hozack, W.J.; Rothman, R.H. Effect of Femoral Component Offset on Polyethylene Wear in Total Hip Arthroplasty. Clin. Orthop. Relat. Res. 2001, 388, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Karachalios, T.; Hartofilakidis, G.; Zacharakis, N.; Tsekoura, M. A 12- to 18-Year Radiographic Follow-up Study of Charnley Low-Friction Arthroplasty. The Role of the Center of Rotation. Clin. Orthop. Relat. Res. 1993, 296, 140–147. [Google Scholar]
- Bunyoz, K.I.; Malchau, E.; Malchau, H.; Troelsen, A. Has the Use of Fixation Techniques in THA Changed in This Decade? The Uncemented Paradox Revisited. Clin. Orthop. Relat. Res. 2020, 478, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, A.; Iannotti, F.; Proietti, L.; Massafra, C.; Speranza, A.; Laghi, A.; Iorio, R. The Accuracy of Patient-Specific Instrumentation with Laser Guidance in a Dynamic Total Hip Arthroplasty: A Radiological Evaluation. Sensors 2021, 21, 4232. [Google Scholar] [CrossRef]
- Bader, R.; Scholz, R.; Steinhauser, E.; Zimmermann, S.; Busch, R.; Mittelmeier, W. The Influence of Head and Neck Geometry on Stability of Total Hip Replacement: A Mechanical Test Study. Acta Orthop. Scand. 2004, 75, 415–421. [Google Scholar] [CrossRef]
- Stief, F.; van Drongelen, S.; Brenneis, M.; Tarhan, T.; Fey, B.; Meurer, A. Influence of Hip Geometry Reconstruction on Frontal Plane Hip and Knee Joint Moments during Walking Following Primary Total Hip Replacement. J. Arthroplasty 2019, 34, 3106–3113. [Google Scholar] [CrossRef]
- Flecher, X.; Ollivier, M.; Argenson, J.N. Lower Limb Length and Offset in Total Hip Arthroplasty. Orthop. Traumatol. Surg. Res. 2016, 102, S9–S20. [Google Scholar] [CrossRef]
- Archibeck, M.J.; Cummins, T.; Carothers, J.; Junick, D.W.; White, R.E. A Comparison of Two Implant Systems in Restoration of Hip Geometry in Arthroplasty. Clin. Orthop. Relat. Res. 2011, 469, 443–446. [Google Scholar] [CrossRef] [Green Version]
- Berend, K.R.; Sporer, S.M.; Sierra, R.J.; Glassman, A.H.; Morris, M.J. Achieving Stability and Lower-Limb Length in Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2010, 92, 2737–2752. [Google Scholar]
- Bourne, R.B.; Rorabeck, C.H. Soft Tissue Balancing: The Hip. J Arthroplastz 2002, 17, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Habor, J.; Fischer, M.C.M.; Tokunaga, K.; Okamoto, M.; Radermacher, K. The Patient-Specific Combined Target Zone for Morpho-Functional Planning of Total Hip Arthroplasty. J. Pers. Med. 2021, 11, 817. [Google Scholar] [CrossRef] [PubMed]
- Foissey, C.; Batailler, C.; Coulomb, R.; Giebaly, D.E.; Coulin, B.; Lustig, S.; Kouyoumdjian, P. Image-Based Robotic-Assisted Total Hip Arthroplasty through Direct Anterior Approach Allows a Better Orientation of the Acetabular Cup and a Better Restitution of the Centre of Rotation than a Conventional Procedure. Int. Orthop. (SICOT) 2023, 47, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Maurer-Ertl, W.; Friesenbichler, J.; Pfann, M.; Maier, M.; Reinbacher, P.; Leithner, A.; Smolle, M.A. Restoration of Hip Geometry after Total Hip Arthroplasty: Retrospective Comparison of Two Short Stems and One Straight Stem. BMC Musculoskelet. Disord. 2022, 23, 1035. [Google Scholar] [CrossRef]
- Karnezis, I.A. A Technique for Accurate Reproduction of the Femoral Anteversion during Primary Total Hip Arthroplasty. Arch. Orthop. Trauma Surg. 2001, 121, 343–345. [Google Scholar] [CrossRef]
- Renkawitz, T.; Haimerl, M.; Dohmen, L.; Gneiting, S.; Lechler, P.; Woerner, M.; Springorum, H.-R.; Weber, M.; Sussmann, P.; Sendtner, E.; et al. The Association between Femoral Tilt and Impingement-Free Range-of-Motion in Total Hip Arthroplasty. BMC Musculoskelet. Disord. 2012, 13, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zahar, A.; Rastogi, A.; Kendoff, D. Dislocation after Total Hip Arthroplasty. Curr. Rev. Musculoskelet. Med. 2013, 6, 350–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wines, A.P.; McNicol, D. Computed Tomography Measurement of the Accuracy of Component Version in Total Hip Arthroplasty. J. Arthroplasty 2006, 21, 696–701. [Google Scholar] [CrossRef]
- Dessyn, E.; Flecher, X.; Parratte, S.; Ollivier, M.; Argenson, J.-N. A 20-Year Follow-up Evaluation of Total Hip Arthroplasty in Patients Younger than 50 Using a Custom Cementless Stem. Hip Int. 2019, 29, 481–488. [Google Scholar] [CrossRef]
- Sariali, E.; Mouttet, A.; Flecher, X.; Argenson, J.N. Reproducing Proximal Femur Anatomy with Custom Stems. In Personalized Hip and Knee Joint Replacement; Rivière, C., Vendittoli, P.-A., Eds.; Springer: Cham, Switzerland, 2020; ISBN 978-3-030-24242-8. [Google Scholar]
- Jolles, B.M.; Zangger, P.; Leyvraz, P.-F. Factors Predisposing to Dislocation after Primary Total Hip Arthroplasty: A Multivariate Analysis. J. Arthroplasty 2002, 17, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Sariali, E.; Klouche, S.; Mamoudy, P. Ceramic-on-Ceramic Total Hip Arthroplasty: Is Squeaking Related to an Inaccurate Three-Dimensional Hip Anatomy Reconstruction? Orthop. Traumatol. Surg. Res. 2014, 100, 437–440. [Google Scholar] [CrossRef] [Green Version]
- Mitsutake, R.; Tanino, H.; Ito, H. The Effect of Range of Motion Simulated with a Patient-Specific Three-Dimensional Simulation Analysis on Dislocation after Total Hip Arthroplasty. Hip Int. 2023, 33, 313–322. [Google Scholar] [CrossRef]
- Zhang, T.; Jia, Z.; Han, W.; Wang, J.; Li, J.; Gong, M.; Jiang, X. Effectiveness and Accuracy of a Patient-Specific Instrumentation System for Total Hip Arthroplasty. Orthop. Surg. 2023, 15, 878–887. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Kurdi, O.; Tauviqirrahman, M.; Winarni, T.I.; Jamari, J. Tresca Stress Study of CoCrMo-on-CoCrMo Bearings Based on Body Mass Index Using 2D Computational Model. J. Tribol. 2022, 33, 31–38. [Google Scholar]
- Shah, M.; Vieira, A.; Mahajan, A.; Agrawal, L.; Shah, D.; Surme, S.; Velankar, A. Does Intra-Operative Fluoroscopy Significantly Improve Component Position in a Primary Total Hip Arthroplasty? Our Experience in a Tertiary Care Hospital. JOIO 2023, 57, 325–335. [Google Scholar] [CrossRef]
- Fischer, T.; Stern, C.; Fritz, B.; Zingg, P.O.; Pfirrmann, C.W.A.; Sutter, R. Impact of Stem Design and Cementation on Postoperative Femoral Antetorsion in 227 Patients with Total Hip Arthroplasty (THA). Skelet. Radiol. 2020, 49, 2001–2009. [Google Scholar] [CrossRef] [PubMed]
- Jamari, J.; Ammarullah, M.I.; Saad, A.P.M.; Syahrom, A.; Uddin, M.; van der Heide, E.; Basri, H. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. J. Funct. Biomater. 2021, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Driessen, A.; Colarossi, G.; El Mansy, Y.; Gatz, M.; Tingart, M.; Eschweiler, J. Short Stems for Total Hip Replacement among Middle-Aged Patients. Int. Orthop. 2020, 44, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, M.; Ettinger, P.; Lerch, M.; Radtke, K.; Budde, S.; Ezechieli, M.; Becher, C.; Thorey, F. The NANOS Short Stem in Total Hip Arthroplasty: A Mid Term Follow-Up. Hip Int. 2011, 21, 583–586. [Google Scholar] [CrossRef]
- Reinbacher, P.; Smolle, M.A.; Friesenbichler, J.; Draschl, A.; Leithner, A.; Maurer-Ertl, W. Three-Year Migration Analysis of a New Metaphyseal Anchoring Short Femoral Stem in THA Using EBRA-FCA. Sci. Rep. 2022, 12, 17173. [Google Scholar] [CrossRef] [PubMed]
- van Oldenrijk, J.; Molleman, J.; Klaver, M.; Poolman, R.W.; Haverkamp, D. Revision Rate after Short-Stem Total Hip Arthroplasty: A Systematic Review of 49 Studies. Acta Orthop. 2014, 85, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.-D.; Yang, W.-Y.; Pan, J.-K.; Huang, H.-T.; Luo, M.-H.; Zeng, L.-F.; Liu, J. Are Short-Stem Prostheses Superior to Conventional Stem Prostheses in Primary Total Hip Arthroplasty? A Systematic Review and Meta-Analysis of Randomised Controlled Trials. BMJ Open 2018, 8, e021649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, S.G.; Woiczinski, M.; Schmidutz, T.F.; Weber, P.; Paulus, A.C.; Steinbrück, A.; Jansson, V.; Schmidutz, F. Can the Metaphyseal Anchored Metha Short Stem Safely Be Revised with a Standard CLS Stem? A Biomechanical Analysis. Int. Orthop. 2017, 41, 2471–2477. [Google Scholar] [CrossRef] [PubMed]
- Bieger, R.; Ignatius, A.; Reichel, H.; Dürselen, L. Biomechanics of a Short Stem: In Vitro Primary Stability and Stress Shielding of a Conservative Cementless Hip Stem. J. Orthop. Res. 2013, 31, 1180–1186. [Google Scholar] [CrossRef] [PubMed]
- Salemyr, M.; Muren, O.; Ahl, T.; Bodén, H.; Eisler, T.; Stark, A.; Sköldenberg, O. Lower Periprosthetic Bone Loss and Good Fixation of an Ultra-Short Stem Compared to a Conventional Stem in Uncemented Total Hip Arthroplasty. Acta Orthop. 2015, 86, 659–666. [Google Scholar] [CrossRef]
- Hochreiter, J.; Böhm, G.; Fierlbeck, J.; Anderl, C.; Birke, M.; Münger, P.; Ortmaier, R. Femoral Antetorsion after Calcar-Guided Short-Stem Total Hip Arthroplasty: A Cadaver Study. J. Orthop. Res. 2022, 40, 2127–2132. [Google Scholar] [CrossRef]
- Sariali, E.; Pascal Moussellard, H. Higher Femoral Anteversion Restoration Accuracy after Total Hip Arthroplasty with a Proximally Fixed Anatomic Stem than with a Generic Straight Double-Tapered Stem. HIP Int. 2022, 112070002210789. [Google Scholar] [CrossRef] [PubMed]
- Watson-Jones, R. Fractures of the Neck of the Femur. Br. J. Surg. 1936, 23, 787–808. [Google Scholar] [CrossRef]
- Reinbacher, P.; Hecker, A.; Friesenbichler, J.; Smolle, M.; Leitner, L.; Klim, S.; Draschl, A.; Colovic, D.; Brunnader, K.; Leithner, A.; et al. Simultaneous Bilateral Total Hip Arthroplasty with Straight-Stems and Short-Stems: Does the Short One Do a Better Job? JCM 2023, 12, 1028. [Google Scholar] [CrossRef]
- Jarrett, D.Y.; Oliveira, A.M.; Zou, K.H.; Snyder, B.D.; Kleinman, P.K. Axial Oblique CT to Assess Femoral Anteversion. AJR Am. J. Roentgenol. 2010, 194, 1230–1233. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, P.; Attal, R.; Kammerer, M.; Thauerer, M.; Hamberger, L.; Mayr, R.; Schmoelz, W. Significant Differences in Femoral Torsion Values Depending on the CT Measurement Technique. Arch. Orthop. Trauma Surg. 2016, 136, 1259–1264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reinbacher, P.; Smolle, M.A.; Friesenbichler, J.; Draschl, A.; Leithner, A.; Maurer-Ertl, W. Pre-Operative Templating in THA Using a Short Stem System: Precision and Accuracy of 2D versus 3D Planning Method. J. Orthop. Traumatol. 2022, 23, 16. [Google Scholar] [CrossRef] [PubMed]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation Study of WOMAC: A Health Status Instrument for Measuring Clinically Important Patient Relevant Outcomes to Antirheumatic Drug Therapy in Patients with Osteoarthritis of the Hip or Knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Harris, W.H. Traumatic Arthritis of the Hip after Dislocation and Acetabular Fractures: Treatment by Mold Arthroplasty. An End-Result Study Using a New Method of Result Evaluation. J. Bone Jt. Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- Kutzner, K.P. Calcar-Guided Short-Stem Total Hip Arthroplasty: Will It Be the Future Standard? Review and Perspectives. World J. Orthop. 2021, 12, 534–547. [Google Scholar] [CrossRef]
- Kutzner, K.P.; Pfeil, J. Individualized Stem-Positioning in Calcar-Guided Short-Stem Total Hip Arthroplasty. J. Vis. Exp. JoVE 2018. [CrossRef] [Green Version]
- Maruyama, M.; Feinberg, J.R.; Capello, W.N.; D’Antonio, J.A. The Frank Stinchfield Award: Morphologic Features of the Acetabulum and Femur: Anteversion Angle and Implant Positioning. Clin. Orthop. Relat. Res. 2001, 393, 52–65. [Google Scholar] [CrossRef]
- Nakahara, I.; Takao, M.; Sakai, T.; Nishii, T.; Yoshikawa, H.; Sugano, N. Gender Differences in 3D Morphology and Bony Impingement of Human Hips. J. Orthop. Res. 2011, 29, 333–339. [Google Scholar] [CrossRef]
- Noble, P.C.; Alexander, J.W.; Lindahl, L.J.; Yew, D.T.; Granberry, W.M.; Tullos, H.S. The Anatomic Basis of Femoral Component Design. Clin. Orthop. Relat. Res. 1988, 235, 148–165. [Google Scholar] [CrossRef]
- Padgett, D.E.; Warashina, H. The Unstable Total Hip Replacement. Clin. Orthop. Relat. Res. 2004, 420, 72–79. [Google Scholar] [CrossRef]
- Coventry, M.B. Late Dislocations in Patients with Charnley Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 1985, 67, 832–841. [Google Scholar] [CrossRef]
- Woo, R.Y.; Morrey, B.F. Dislocations after Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 1982, 64, 1295–1306. [Google Scholar] [CrossRef]
- Hartel, M.J.; Petersik, A.; Schmidt, A.; Kendoff, D.; Nüchtern, J.; Rueger, J.M.; Lehmann, W.; Grossterlinden, L.G. Determination of Femoral Neck Angle and Torsion Angle Utilizing a Novel Three-Dimensional Modeling and Analytical Technology Based on CT Datasets. PLoS ONE 2016, 11, e0149480. [Google Scholar] [CrossRef]
- Yoon, J.Y.; Seo, W.Y.; Kim, H.J.; Yoo, J.J. The Relationship between Femoral Stem Tilt and Stem Length in Total Hip Arthroplasty: A Retrospective Case-Control Study. Clin. Orthop. Surg. 2022, 14, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Faizan, A.; Gerges, J.J.; Asencio, G.; Essig, J.; Munini, E.; Hozack, W.J. Changes in Femoral Version During Implantation of Anatomic Stems: Implications on Stem Design. J. Arthroplast. 2016, 31, 512–516. [Google Scholar] [CrossRef]
- Yu, H.; Liu, H.; Jia, M.; Hu, Y.; Zhang, Y. A Comparison of a Short versus a Conventional Femoral Cementless Stem in Total Hip Arthroplasty in Patients 70 Years and Older. J. Orthop. Surg. Res. 2016, 11, 33. [Google Scholar] [CrossRef] [Green Version]
- Huo, S.-C.; Wang, F.; Dong, L.-J.; Wei, W.; Zeng, J.-Q.; Huang, H.-X.; Han, Q.-M.; Duan, R.-Q. Short-Stem Prostheses in Primary Total Hip Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. Medicine 2016, 95, e5215. [Google Scholar] [CrossRef] [PubMed]
- Free, M.D.; Barnes, I.; Hutchinson, M.; Harvie, P. Preoperative Radiographs to Predict Component Malposition in Direct Anterior Approach Total Hip Arthroplasty. Hip Int. 2023, 33, 207–213. [Google Scholar] [CrossRef]

| Proxy (n = 89) N; % | Corail (n = 41) N; % | p-Value | ||
|---|---|---|---|---|
| Gender | Male | 51 (57.3) | 25 (61.0) | 0.693 |
| Female | 38 (42.7) | 16 (39.0) | ||
| Hip Type | Coxa vara (CCD < 125°) | 47 (52.8) | 0 (0.0) | <0.001 |
| Coxa norma (CCD 125–134.9°) | 33 (37.1) | 0 (0.0) | ||
| Coxa valga (CCD ≥ 135°) | 9 (10.1) | 41 (100.0) | ||
| Age at Surgery (in years; mean ± standard deviation) | 60.4 ± 4.5 | 63.9 ± 10.3 | 0.030 | |
| BMI (mean ± standard deviation) | 28.5 ± 4.8 | 28.2 ± 4.5 | 0.603 | |
| Preoperative Femoral Anteversion (mean ± standard deviation) | 22.4° ± 11.0° | N/A | N/A | |
| Postoperative Femoral Anteversion (mean ± standard deviation) | 23.4° ± 10.1° | 16.6° ± 1.3° | <0.001 | |
| HHS Score after 1 year (mean ± standard deviation) | 95.8 ± 8.0 | 93.5 ± 10.1 | 0.159 | |
| WOMAC Score after 1 year (mean ± standard deviation) | 10.5 ± 13.6 | 9.7 ± 14.4 | 0.758 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klim, S.M.; Reinbacher, P.; Smolle, M.A.; Hecker, A.; Maier, M.; Friesenbichler, J.; Leithner, A.; Leitner, L.; Draschl, A.; Lewis, J.; et al. Femoral Anteversion in Total Hip Arthroplasty: Retrospective Comparison of Short- and Straight-Stem Models Using CT Scans. J. Clin. Med. 2023, 12, 2391. https://doi.org/10.3390/jcm12062391
Klim SM, Reinbacher P, Smolle MA, Hecker A, Maier M, Friesenbichler J, Leithner A, Leitner L, Draschl A, Lewis J, et al. Femoral Anteversion in Total Hip Arthroplasty: Retrospective Comparison of Short- and Straight-Stem Models Using CT Scans. Journal of Clinical Medicine. 2023; 12(6):2391. https://doi.org/10.3390/jcm12062391
Chicago/Turabian StyleKlim, Sebastian Martin, Patrick Reinbacher, Maria Anna Smolle, Andrzej Hecker, Michael Maier, Joerg Friesenbichler, Andreas Leithner, Lukas Leitner, Alexander Draschl, Jan Lewis, and et al. 2023. "Femoral Anteversion in Total Hip Arthroplasty: Retrospective Comparison of Short- and Straight-Stem Models Using CT Scans" Journal of Clinical Medicine 12, no. 6: 2391. https://doi.org/10.3390/jcm12062391