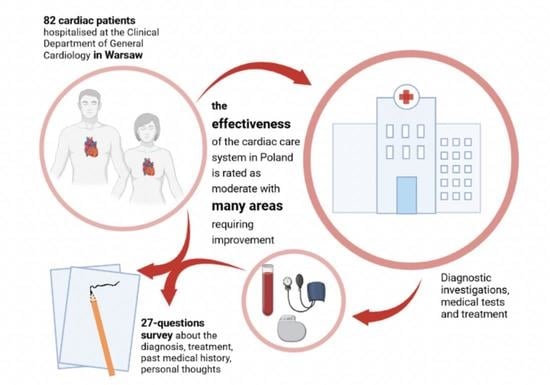
The Path of a Cardiac Patient—From the First Symptoms to Diagnosis to Treatment: Experiences from the Tertiary Care Center in Poland
Abstract
:1. Introduction
2. Materials and Methods
2.1. General Study Design and Data Collection Process
2.2. Construction of the Questionnaire
2.3. Data Analysis
3. Results
3.1. Study Group Characteristic
3.2. Clinical Characteristic
3.3. Open Questions
4. Discussion
4.1. Further Studies Directions
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019 Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Deaton, C.; Froelicher, E.S.; Wu, L.H.; Ho, C.; Shishani, K.; Jaarsma, T. The Global Burden of Cardiovascular Disease. Eur. J. Cardiovasc. Nurs. 2011, 10, S5–S13. [Google Scholar] [CrossRef]
- Nieuwlaat, R.; Schwalm, J.-D.; Khatib, R.; Yusuf, S. Why are we failing to implement effective therapies in cardiovascular disease? Eur. Heart J. 2013, 34, 1262–1269. [Google Scholar] [CrossRef] [PubMed]
- Morris, L.S.; Schulz, R.M. Patient Compliance—An Overview. J. Clin. Pharm. Ther. 1992, 17, 283–295. [Google Scholar] [CrossRef] [PubMed]
- Khera, A.; Baum, S.; Gluckman, T.J.; Gulati, M.; Martin, S.S.; Michos, E.D.; Navar, A.M.; Taub, P.R.; Toth, P.P.; Virani, S.S.; et al. Continuity of care and outpatient management for patients with and at high risk for cardiovascular disease during the COVID-19 pandemic: A scientific statement from the American Society for Preventive Cardiology. Am. J. Prev. Cardiol. 2020, 1, 100009. [Google Scholar] [CrossRef]
- Eraker, S.A.; Kirscht, J.P.; Becker, M.H. Understanding and Improving Patient Compliance. Ann. Intern. Med. 1984, 100, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Cameron, C. Patient compliance: Recognition of factors involved and suggestions for promoting compliance with therapeutic regimens. J. Adv. Nurs. 1996, 24, 244–250. [Google Scholar] [CrossRef] [PubMed]
- El-Haddad, C.; Hegazi, I.; Hu, W. Understanding Patient Expectations of Health Care: A Qualitative Study. J. Patient Exp. 2020, 7, 1724–1731. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Del Mar, C. Patients’ Expectations of the Benefits and Harms of Treatments, Screening, and Tests A Systematic Review. JAMA Intern. Med. 2015, 175, 274–286. [Google Scholar] [CrossRef] [PubMed]
- Casals, M.; Girabent-Farres, M.; Carrasco, J.L. Methodological Quality and Reporting of Generalized Linear Mixed Models in Clinical Medicine (2000–2012): A Systematic Review. PLoS ONE 2014, 9, e112653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, R. Plane Answers to Complex Questions: The Theory of Linear Models, 4th ed.; Springer: New York, NY, USA, 2011; pp. 1–482. [Google Scholar] [CrossRef]
- Weissgerber, T.L.; Garcia-Valencia, O.; Garovic, V.D.; Milic, N.M.; Winham, S.J. Why we need to report more than ‘Data were Analyzed by t-tests of ANOVA’. eLife 2018, 7, e36163. [Google Scholar] [CrossRef]
- O’Neill, D.E.; Forman, D.E. Cardiovascular care of older adults. BMJ 2021, 374, n1593. [Google Scholar] [CrossRef]
- Ballard, D.J. Indicators to improve clinical quality across an integrated health care system. Int. J. Qual. Health Care 2003, 15, I13–I23. [Google Scholar] [CrossRef] [PubMed]
- Koning, C.; Lock, A.; Bushe, J.; Guo, C. Patient Satisfaction with Heart Health Clinics in Fraser Health, Canada. J. Patient Exp. 2021, 8, 2374373520981475. [Google Scholar] [CrossRef]
- Soleimani, M.A.; Zarabadi-Pour, S.; Motalebi, S.A.; Allen, K.A. Predictors of Quality of Life in Patients with Heart Disease. J. Relig. Health 2020, 59, 2135–2148. [Google Scholar] [CrossRef] [PubMed]
- Chatzinikolaou, A.; Tzikas, S.; Lavdaniti, M. Assessment of Quality of Life in Patients with Cardiovascular Disease Using the SF-36, MacNew, and EQ-5D-5L Questionnaires. Cureus 2021, 13, e17982. [Google Scholar] [CrossRef]
- Reblin, M.; Uchino, B.N. Social and emotional support and its implication for health. Curr. Opin. Psychiatry 2008, 21, 201–205. [Google Scholar] [CrossRef]
- Pinckard, K.; Baskin, K.K.; Stanford, K.I. Effects of Exercise to Improve Cardiovascular Health. Front. Cardiovasc. Med. 2019, 6, 69. [Google Scholar] [CrossRef]
- Price, K.J.; Gordon, B.A.; Bird, S.R.; Benson, A.C. A review of guidelines for cardiac rehabilitation exercise programmes: Is there an international consensus? Eur. J. Prev. Cardiol. 2016, 23, 1715–1733. [Google Scholar] [CrossRef] [PubMed]
- Tian, D.Y.; Meng, J.Q. Exercise for Prevention and Relief of Cardiovascular Disease: Prognoses, Mechanisms, and Approaches. Oxidative Med. Cell. Longev. 2019, 2019, 3756750. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.G.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Mann, T.; Lamberts, R.P.; Lambert, M.I. Methods of Prescribing Relative Exercise Intensity: Physiological and Practical Considerations. Sports Med. 2013, 43, 613–625. [Google Scholar] [CrossRef]
- Wita, K.; Kulach, A.; Wita, M.; Wybraniec, M.T.; Wilkosz, K.; Polak, M.; Matla, M.; Maciejewski, L.; Fluder, J.; Kalanska-Lukasik, B.; et al. Managed Care after Acute Myocardial Infarction (KOS-zawal) reduces major adverse cardiovascular events by 45% in 3-month follow-up—Single-center results of Poland’s National Health Fund program of comprehensive post-myocardial infarction care. Arch. Med. Sci. 2020, 16, 551–558. [Google Scholar] [CrossRef]
- Pilarska, A.; Zimmermann, A.; Zdun-Ryzewska, A. Access to Health Information in the Polish Healthcare System-Survey Research. Int. J. Environ. Res. Public Health 2022, 19, 7320. [Google Scholar] [CrossRef] [PubMed]
- Sowada, C.; Sagan, A.; Kowalska-Bobko, I. Poland Health system review preface. In Poland: Health System Review; World Health Organization: Geneva, Switzerland, 2019; Volume 21. [Google Scholar]
- Masters, R.; Anwar, E.; Collins, B.; Cookson, R.; Capewell, S. Return on investment of public health interventions: A systematic review. J. Epidemiol. Community Health 2017, 71, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Boet, S.; Sharma, S.; Goldman, J.; Reeves, S. Review article: Medical education research: An overview of methods. Can. J. Anesth. 2012, 59, 159–170. [Google Scholar] [CrossRef]
- Mansouri, M.; Lockyer, J. A meta-analysis of Continuing Medical Education effectiveness. J. Contin. Educ. Health Prof. 2007, 27, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Ju, I.; Banks, E.; Calabria, B.; Ju, A.; Agostino, J.; Korda, R.J.; Usherwood, T.; Manera, K.; Hanson, C.S.; Craig, J.C.; et al. General practitioners’ perspectives on the prevention of cardiovascular disease: Systematic review and thematic synthesis of qualitative studies. BMJ Open 2018, 8, e021137. [Google Scholar] [CrossRef] [PubMed]
- Smeets, M.; Zervas, S.; Leben, H.; Vermandere, M.; Janssens, S.; Mullens, W.; Aertgeerts, B.; Vaes, B. General practitioners’ perceptions about their role in current and future heart failure care: An exploratory qualitative study. BMC Health Serv. Res. 2019, 19, 432. [Google Scholar] [CrossRef] [Green Version]
- Price, E.; Baker, R.; Krause, J.; Keen, C. Organisation of services for people with cardiovascular disorders in primary care: Transfer to primary care or to specialist-generalist multidisciplinary teams? BMC Fam. Pract. 2014, 15, 158. [Google Scholar] [CrossRef] [PubMed]
- Guadagnoli, E.; Normand, S.L.T.; DiSalvo, T.G.; Palmer, R.H.; McNeil, B.J. Effects of treatment recommendations and specialist intervention on care provided by primary care physicians to patients with myocardial infarction or heart failure. Am. J. Med. 2004, 117, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Dubas-Jakobczyk, K.; Domagala, A.; Mikos, M. Impact of the doctor deficit on hospital management in Poland: A mixed-method study. Int. J. Health Plan. Manag. 2019, 34, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Astin, J.A. Why patients use alternative medicine—Results of a national study. JAMA 1998, 279, 1548–1553. [Google Scholar] [CrossRef] [PubMed]
- The World Health Organization Quality of Life-100 Questionnaire. Available online: https://www.who.int/tools/whoqol/whoqol-100 (accessed on 18 August 2022).
- The World Health Organization Quality of Life Questionnaire-BREF. Available online: https://www.who.int/tools/whoqol/whoqol-bref (accessed on 18 August 2022).
- HCAHPS: Patients’ Perspectives of Care Survey. Available online: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS (accessed on 18 August 2022).
- Hermans, A.N.L.; Gawalko, M.; Hillmann, H.A.K.; Sohaib, A.; van der Velden, R.M.J.; Betz, K.; Verhaert, D.; Scherr, D.; Meier, J.; Sultan, A.; et al. Self-Reported Mobile Health-Based Risk Factor and CHA(2)DS(2)-VASc-Score Assessment in Patients with Atrial Fibrillation: TeleCheck-AF Results. Front. Cardiovasc. Med. 2022, 8, 757587. [Google Scholar] [CrossRef]


| Condition/Complex | Whole Population | 30–40 Years | 40–50 Years | 50–60 Years | >60 Years | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n of Patients | % of the Group | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | |
| Arrythmias | 43 | (52.44%) | 3 | (6.98%) | 4 | (9.30%) | 5 | (11.63%) | 31 | (72.09%) |
| Hypertension | 43 | (52.44%) | 3 | (6.98%) | 4 | (9.30%) | 8 | (18.60%) | 28 | (65.12%) |
| Overweight | 25 | (30.49%) | 1 | (4.00%) | 4 | (16.00%) | 6 | (24.00%) | 14 | (56.00%) |
| Type 2 diabetes mellitus | 24 | (29.27%) | 1 | (4.17%) | 2 | (8.33%) | 6 | (25.00%) | 15 | (62.50%) |
| Coronary artery disease | 23 | (28.05%) | 0 | (0.00%) | 0 | (0.00%) | 5 | (21.74%) | 18 | (78.26%) |
| Heart failure | 17 | (20.73%) | 2 | (11.76%) | 1 | (5.88%) | 3 | (17.65%) | 11 | (64.71%) |
| Hypercholesterolemia | 14 | (17.07%) | 0 | (0.00%) | 3 | (21.43%) | 2 | (14.29%) | 9 | (64.29%) |
| Chronic pulmonary disease | 13 | (15.85%) | 0 | (0.00%) | 2 | (15.38%) | 1 | −7.69% | 10 | −76.92% |
| Hypothyroidism | 13 | (15.85%) | 0 | (0.00%) | 3 | (23.08%) | 2 | (15.38%) | 8 | (61.54%) |
| Depression | 10 | (12.20%) | 2 | (20.00%) | 1 | (10.00%) | 2 | (20.00%) | 5 | (50.00%) |
| Atherosclerosis | 9 | (10.98%) | 0 | (0.00%) | 0 | (0.00%) | 0 | (0.00%) | 9 | (100.00%) |
| Valvular heart disease | 5 | (6.10%) | 0 | (0.00%) | 2 | (40.00%) | 1 | (20.00%) | 2 | (40.00%) |
| Symptom | Whole Population | 30–40 Years | 40–50 Years | 50–60 Years | >60 Years | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n of Patients | % of the Group | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | |
| Dyspnea | 26 | (31.71%) | 2 | (7.69%) | 2 | (7.69%) | 5 | (19.23%) | 17 | (65.38%) |
| Pain in the chest | 20 | (24.39%) | 1 | (5.00%) | 2 | (10.00%) | 2 | (10.00%) | 15 | (75.00%) |
| Exertion fatigue | 20 | (23.17%) | 3 | (15.00%) | 2 | (10.00%) | 2 | (10.00%) | 13 | (65.00%) |
| Palpitations | 19 | (20.73%) | 2 | (10.53%) | 1 | (5.26%) | 2 | (10.53%) | 14 | (73.68%) |
| Tiredness | 17 | (9.76%) | 1 | (5.88%) | 1 | (5.88%) | 2 | (11.76%) | 13 | (76.47%) |
| Fainting | 8 | (3.66%) | 1 | (12.50%) | 2 | (25.00%) | 2 | (25.00%) | 3 | (37.50%) |
| Edema | 3 | (3.66%) | 0 | (0.00%) | 2 | (66.67%) | 0 | (0.00%) | 1 | (33.33%) |
| Cough | 3 | (31.71%) | 1 | (33.33%) | 0 | (0.00%) | 0 | (0.00%) | 2 | (66.67%) |
| First Diagnostic Step | Whole Population | 30–40 Years | 40–50 Years | 50–60 Years | >60 Years | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n of Patients | % of the Group | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | n of Patients | % of the Subgroup | |
| Reimbursed examination by the GP | 45 | (54.88%) | 3 | (6.67%) | 5 | (11.11%) | 6 | (13.33%) | 31 | (68.89%) |
| Examination by the cardiologist | 18 | (21.95%) | 2 | (11.11%) | 2 | (11.11%) | 2 | (11.11%) | 12 | (66.67%) |
| Calling an ambulance | 9 | (10.98%) | 0 | (0.00%) | 0 | (0.00%) | 2 | (22.22%) | 7 | (77.78%) |
| Appointment at the hospital | 6 | (7.32%) | 0 | (0.00%) | 1 | (16.67%) | 1 | (16.67%) | 4 | (66.67%) |
| Paid examination by the GP | 4 | (4.88%) | 0 | (0.00%) | 0 | (0.00%) | 1 | (25.00%) | 3 | (75.00%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kasiak, P.S.; Buchalska, B.; Kowalczyk, W.; Wyszomirski, K.; Krzowski, B.; Grabowski, M.; Balsam, P. The Path of a Cardiac Patient—From the First Symptoms to Diagnosis to Treatment: Experiences from the Tertiary Care Center in Poland. J. Clin. Med. 2022, 11, 5276. https://doi.org/10.3390/jcm11185276
Kasiak PS, Buchalska B, Kowalczyk W, Wyszomirski K, Krzowski B, Grabowski M, Balsam P. The Path of a Cardiac Patient—From the First Symptoms to Diagnosis to Treatment: Experiences from the Tertiary Care Center in Poland. Journal of Clinical Medicine. 2022; 11(18):5276. https://doi.org/10.3390/jcm11185276
Chicago/Turabian StyleKasiak, Przemysław Seweryn, Barbara Buchalska, Weronika Kowalczyk, Krzysztof Wyszomirski, Bartosz Krzowski, Marcin Grabowski, and Paweł Balsam. 2022. "The Path of a Cardiac Patient—From the First Symptoms to Diagnosis to Treatment: Experiences from the Tertiary Care Center in Poland" Journal of Clinical Medicine 11, no. 18: 5276. https://doi.org/10.3390/jcm11185276