Artificial Intelligence Supports Decision Making during Open-Chest Surgery of Rare Congenital Heart Defects
Abstract
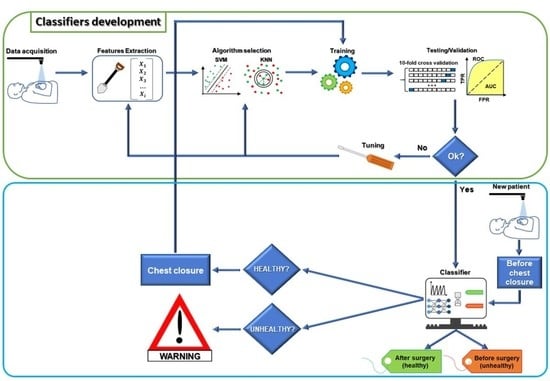
:1. Introduction
2. Materials and Methods
2.1. Surgical Methods
2.2. Right Ventricle Video Recording
- Maximum contraction velocity: estimates the instantaneous maximal velocity of the cardiac tissue during systole;
- Force: estimates the instantaneous acceleration;
- Energy: estimates the kinetic energy during cardiac cycles;
- Perimeter: estimates the ventricular compliance.
2.3. Features/Predictors
2.4. Models’ Training and Optimization
- Optimizable KNN (k-nearest neighbor classifier), via the “fitcknn” function (https://it.mathworks.com/help/stats/fitcknn.html, accessed on 1 August 2021) with a total of 100 optimization iterations and no standardization of the input features;
- Optimizable SVM (support vector machine classifier), via the “fitcsvm” function (https://it.mathworks.com/help/stats/fitcsvm.html, accessed on 1 August 2021) with a total of 100 optimization iterations and no standardization of the input features.
2.5. Decision Surface
2.6. Statistical Analysis
3. Results
3.1. Selected Models
3.2. Optimized Model Training
- The MATLAB®’s script of the optimized model;
- The MATLAB®’s optimized model (as a saved workspace structure array) to employ in the operating room to classify the current patient’s heart movement as unhealthy or healthy.
3.3. Classifiers’ Prediction Ability Tested via Two Additional Patients with Different Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Foresti, R.; Rossi, S.; Magnani, M.; Lo Bianco, C.G.; Delmonte, N. Smart Society and Artificial Intelligence: Big Data Scheduling and the Global Standard Method Applied to Smart Maintenance. Engineering 2020, 6, 835–846. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Khan, I.H. Holography applications toward medical field: An overview. Indian J. Radiol. Imaging 2020, 30, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, P.P.; Forkan, A.R.M.; Morshed, A.; Haghighi, P.D.; Kang, Y.-B. Healthcare 4.0: A review of frontiers in digital health. WIREs Data Min. Knowl. Discov. 2020, 10, e1350. [Google Scholar] [CrossRef]
- Poli, R.; Obrst, L. The Interplay Between Ontology as Categorial Analysis and Ontology as Technology. In Theory and Applications of Ontology: Computer Applications; Poli, R., Healy, M., Kameas, A., Eds.; Springer: Dordrecht, The Netherlands, 2010; pp. 1–26. [Google Scholar]
- Bal, M.; Amasyali, M.F.; Sever, H.; Kose, G.; Demirhan, A. Performance evaluation of the machine learning algorithms used in inference mechanism of a medical decision support system. Sci. World J. 2014, 2014, 137896. [Google Scholar] [CrossRef]
- Chen, Y.; McElvain, L.E.; Tolpygo, A.S.; Ferrante, D.; Friedman, B.; Mitra, P.P.; Karten, H.J.; Freund, Y.; Kleinfeld, D. An active texture-based digital atlas enables automated mapping of structures and markers across brains. Nat. Methods 2019, 16, 341–350. [Google Scholar] [CrossRef]
- Feeny, A.K.; Chung, M.K.; Madabhushi, A.; Attia, Z.I.; Cikes, M.; Firouznia, M.; Friedman, P.A.; Kalscheur, M.M.; Kapa, S.; Narayan, S.M.; et al. Artificial Intelligence and Machine Learning in Arrhythmias and Cardiac Electrophysiology. Circ. Arrhythm. Electrophysiol. 2020, 13, e007952. [Google Scholar] [CrossRef]
- Oikonomou, E.K.; Siddique, M.; Antoniades, C. Artificial intelligence in medical imaging: A radiomic guide to precision phenotyping of cardiovascular disease. Cardiovasc. Res. 2020, 116, 2040–2054. [Google Scholar] [CrossRef] [Green Version]
- Knott, K.D.; Seraphim, A.; Augusto, J.B.; Xue, H.; Chacko, L.; Aung, N.; Petersen, S.E.; Cooper, J.A.; Manisty, C.; Bhuva, A.N.; et al. The Prognostic Significance of Quantitative Myocardial Perfusion An Artificial Intelligence-Based Approach Using Perfusion Mapping. Circulation 2020, 141, 1282–1291. [Google Scholar] [CrossRef]
- Dawes, T.J.W.; de Marvao, A.; Shi, W.; Fletcher, T.; Watson, G.M.J.; Wharton, J.; Rhodes, C.J.; Howard, L.; Gibbs, J.S.R.; Rueckert, D.; et al. Machine Learning of Three-dimensional Right Ventricular Motion Enables Outcome Prediction in Pulmonary Hypertension: A Cardiac MR Imaging Study. Radiology 2017, 283, 381–390. [Google Scholar] [CrossRef] [Green Version]
- Genovese, D.; Rashedi, N.; Weinert, L.; Narang, A.; Addetia, K.; Patel, A.R.; Prater, D.; Goncalves, A.; Mor-Avi, V.; Lang, R.M. Machine Learning-Based Three-Dimensional Echocardiographic Quantification of Right Ventricular Size and Function: Validation Against Cardiac Magnetic Resonance. J. Am. Soc. Echocardiogr. 2019, 32, 969–977. [Google Scholar] [CrossRef]
- Deo, R.C. Machine Learning in Medicine. Circulation 2015, 132, 1920–1930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fralick, M.; Colak, E.; Mamdani, M. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 2588–2589. [Google Scholar] [CrossRef] [Green Version]
- Mukherjee, P.; Cintra, M.; Huang, C.; Zhou, M.; Zhu, S.; Colevas, A.D.; Fischbein, N.; Gevaert, O. CT-based Radiomic Signatures for Predicting Histopathologic Features in Head and Neck Squamous Cell Carcinoma. Radiol. Imaging Cancer 2020, 2, e190039. [Google Scholar] [CrossRef]
- Fassina, L.; Faragli, A.; Lo Muzio, F.P.; Kelle, S.; Campana, C.; Pieske, B.; Edelmann, F.; Alogna, A. A Random Shuffle Method to Expand a Narrow Dataset and Overcome the Associated Challenges in a Clinical Study: A Heart Failure Cohort Example. Front. Cardiovasc. Med. 2020, 7, 599923. [Google Scholar] [CrossRef]
- Rockowitz, S.; LeCompte, N.; Carmack, M.; Quitadamo, A.; Wang, L.; Park, M.; Knight, D.; Sexton, E.; Smith, L.; Sheidley, B.; et al. Children’s rare disease cohorts: An integrative research and clinical genomics initiative. NPJ Genom. Med. 2020, 5, 29. [Google Scholar] [CrossRef]
- Guthridge, J.M.; Lu, R.; Tran, L.T.; Arriens, C.; Aberle, T.; Kamp, S.; Munroe, M.E.; Dominguez, N.; Gross, T.; DeJager, W.; et al. Adults with systemic lupus exhibit distinct molecular phenotypes in a cross-sectional study. EClinicalMedicine 2020, 20, 100291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, A.M.; Chamberlin, S.; Deloughery, T.; Nguyen, M.; Bedrick, S.; Meninger, S.; Ko, J.J.; Amin, J.J.; Wei, A.H.; Hersh, W. Detecting rare diseases in electronic health records using machine learning and knowledge engineering: Case study of acute hepatic porphyria (vol 15, e0235574, 2020). PLoS ONE 2020, 15, e0238277. [Google Scholar] [CrossRef]
- Hinton, R.B.; Ware, S.M. Heart Failure in Pediatric Patients With Congenital Heart Disease. Circ. Res. 2017, 120, 978–994. [Google Scholar] [CrossRef] [Green Version]
- Fassina, L.; Rozzi, G.; Rossi, S.; Scacchi, S.; Galetti, M.; Lo Muzio, F.P.; Del Bianco, F.; Colli Franzone, P.; Petrilli, G.; Faggian, G.; et al. Cardiac kinematic parameters computed from video of in situ beating heart. Sci. Rep. 2017, 7, 46143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozzi, G.; Lo Muzio, F.P.; Sandrini, C.; Rossi, S.; Fassina, L.; Faggian, G.; Miragoli, M.; Luciani, G.B. Real-time video kinematic evaluation of the in situ beating right ventricle after pulmonary valve replacement in patients with tetralogy of Fallot: A pilot study. Interact. Cardiovasc. Thorac. Surg. 2019, 29, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Rozzi, G.; Lo Muzio, F.P.; Fassina, L.; Rossi, S.; Statello, R.; Sandrini, C.; Laricchiuta, M.; Faggian, G.; Miragoli, M.; Luciani, G.B. Right ventricular functional recovery depends on timing of pulmonary valve replacement in tetralogy of Fallot: A video kinematic study. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2021, 59, 1329–1336. [Google Scholar] [CrossRef]
- Villafane, J.; Feinstein, J.A.; Jenkins, K.J.; Vincent, R.N.; Walsh, E.P.; Dubin, A.M.; Geva, T.; Towbin, J.A.; Cohen, M.S.; Fraser, C.; et al. Hot topics in tetralogy of Fallot. J. Am. Coll. Cardiol. 2013, 62, 2155–2166. [Google Scholar] [CrossRef] [Green Version]
- Sevakula, R.K.; Au-Yeung, W.M.; Singh, J.P.; Heist, E.K.; Isselbacher, E.M.; Armoundas, A.A. State-of-the-Art Machine Learning Techniques Aiming to Improve Patient Outcomes Pertaining to the Cardiovascular System. J. Am. Heart Assoc. 2020, 9, e013924. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H. Frequency-domain features for ECG beat discrimination using grey relational analysis-based classifier. Comput. Math. Appl. 2008, 55, 680–690. [Google Scholar] [CrossRef] [Green Version]
- Kinoshita, O.; Fontaine, G.; Rosas, F.; Elias, J.; Iwa, T.; Tonet, J.; Lascault, G.; Frank, R. Time-Domain and Frequency-Domain Analyses of the Signal-Averaged Ecg in Patients with Arrhythmogenic Right-Ventricular Dysplasia. Circulation 1995, 91, 715–721. [Google Scholar] [CrossRef]
- Taye, G.T.; Hwang, H.J.; Lim, K.M. Application of a convolutional neural network for predicting the occurrence of ventricular tachyarrhythmia using heart rate variability features (vol 10, 6769, 2020). Sci. Rep. 2020, 10, 6769. [Google Scholar] [CrossRef] [Green Version]
- Armitage, P.B.G.; Berry, G.; Matthews, J.N.S. Clinical Trials. In Statistical Methods in Medical Research; Wiley Blackwell: Hoboken, NJ, USA, 2002; pp. 591–647. [Google Scholar]
- Liu, Y.; Chen, S.; Zuhlke, L.; Black, G.C.; Choy, M.K.; Li, N.; Keavney, B.D. Global birth prevalence of congenital heart defects 1970-2017: Updated systematic review and meta-analysis of 260 studies. Int. J. Epidemiol. 2019, 48, 455–463. [Google Scholar] [CrossRef]
- Gould, K.A. The Elements of Statistical Learning (2nd edition): Data Mining, Inference, and Prediction. Dimens Crit. Care Nur. 2016, 35, 52. [Google Scholar]
- Freund, Y.; Schapire, R.E. A decision-theoretic generalization of on-line learning and an application to boosting. J. Comput. Syst. Sci. 1997, 55, 119–139. [Google Scholar] [CrossRef] [Green Version]
- Seiffert, C.; Khoshgoftaar, T.M.; Van Hulse, J.; Napolitano, A. RUSBoost: Improving Classification Performance when Training Data is Skewed. In Proceedings of the 2008 19th International Conference on Pattern Recognition, Tampa, FL, USA, 8–11 December 2008; pp. 3650–3653. [Google Scholar]
- Melillo, P.; Fusco, R.; Sansone, M.; Bracale, M.; Pecchia, L. Discrimination power of long-term heart rate variability measures for chronic heart failure detection. Med. Biol. Eng. Comput. 2011, 49, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Melillo, P.; Izzo, R.; Orrico, A.; Scala, P.; Attanasio, M.; Mirra, M.; De Luca, N.; Pecchia, L. Automatic Prediction of Cardiovascular and Cerebrovascular Events Using Heart Rate Variability Analysis. PLoS ONE 2015, 10, e0118504. [Google Scholar] [CrossRef]
- Ali, L.; Khan, S.U.; Golilarz, N.A.; Yakubu, I.; Qasim, I.; Noor, A.; Nour, R. A Feature-Driven Decision Support System for Heart Failure Prediction Based on chi 2 Statistical Model and Gaussian Naive Bayes. Comput. Math. Methods Med. 2019, 2019, 6314328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dutta, S.; Chatterjee, A.; Munshi, S. Correlation technique and least square support vector machine combine for frequency domain based ECG beat classification. Med. Eng. Phys. 2010, 32, 1161–1169. [Google Scholar] [CrossRef]
- Liu, G.Z.; Wang, L.; Wang, Q.; Zhou, G.M.; Wang, Y.; Jiang, Q. A New Approach to Detect Congestive Heart Failure Using Short-Term Heart Rate Variability Measures. PLoS ONE 2014, 9, e93399. [Google Scholar] [CrossRef]
- Frigiola, A.; Tsang, V.; Bull, C.; Coats, L.; Khambadkone, S.; Derrick, G.; Mist, B.; Walker, F.; van Doorn, C.; Bonhoeffer, P.; et al. Biventricular response after pulmonary valve replacement for right ventricular outflow tract dysfunction: Is age a predictor of outcome? Circulation 2008, 118, S182–S190. [Google Scholar] [CrossRef] [Green Version]
- Mercer-Rosa, L.; Yang, W.; Kutty, S.; Rychik, J.; Fogel, M.; Goldmuntz, E. Quantifying pulmonary regurgitation and right ventricular function in surgically repaired tetralogy of Fallot: A comparative analysis of echocardiography and magnetic resonance imaging. Circ. Cardiovasc. Imaging 2012, 5, 637–643. [Google Scholar] [CrossRef] [Green Version]
- Pedrotti, P.; Peritore, A.; Cereda, A.; Giannattasio, C.; Imazio, M. Total pericardial agenesis mimicking arrhythmogenic right ventricular dysplasia. J. Cardiovasc. Med. 2016, 17, e216–e217. [Google Scholar] [CrossRef]
- Bokma, J.P.; Geva, T.; Sleeper, L.A.; Babu Narayan, S.V.; Wald, R.; Hickey, K.; Jansen, K.; Wassall, R.; Lu, M.; Gatzoulis, M.A.; et al. A propensity score-adjusted analysis of clinical outcomes after pulmonary valve replacement in tetralogy of Fallot. Heart 2018, 104, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Lo Muzio, F.P.; Rozzi, G.; Rossi, S.; Gerboles, A.G.; Fassina, L.; Pela, G.; Luciani, G.B.; Miragoli, M. In-situ optical assessment of rat epicardial kinematic parameters reveals frequency-dependent mechanic heterogeneity related to gender. Prog. Biophys. Mol. Biol. 2020, 154, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Saini, I.; Singh, D.; Khosla, A. QRS detection using K-Nearest Neighbor algorithm (KNN) and evaluation on standard ECG databases. J. Adv. Res. 2013, 4, 331–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alshakhs, F.; Alharthi, H.; Aslam, N.; Khan, I.U.; Elasheri, M. Predicting Postoperative Length of Stay for Isolated Coronary Artery Bypass Graft Patients Using Machine Learning. Int. J. Gen. Med. 2020, 13, 751–762. [Google Scholar] [CrossRef]
- Tseng, P.Y.; Chen, Y.T.; Wang, C.H.; Chiu, K.M.; Peng, Y.S.; Hsu, S.P.; Chen, K.L.; Yang, C.Y.; Lee, O.K. Prediction of the development of acute kidney injury following cardiac surgery by machine learning. Crit. Care 2020, 24, 478. [Google Scholar] [CrossRef]
- Fernandes, M.P.B.; Armengol de la Hoz, M.; Rangasamy, V.; Subramaniam, B. Machine Learning Models with Preoperative Risk Factors and Intraoperative Hypotension Parameters Predict Mortality After Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2021, 35, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Moghaddasi, H.; Nourian, S. Automatic assessment of mitral regurgitation severity based on extensive textural features on 2D echocardiography videos. Comput. Biol. Med. 2016, 73, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Bellini, V.; Guzzon, M.; Bigliardi, B.; Mordonini, M.; Filippelli, S.; Bignami, E. Artificial Intelligence: A New Tool in Operating Room Management. Role of Machine Learning Models in Operating Room Optimization. J. Med. Syst. 2019, 44, 20. [Google Scholar] [CrossRef] [PubMed]
- Bartek, M.A.; Saxena, R.C.; Solomon, S.; Fong, C.T.; Behara, L.D.; Venigandla, R.; Velagapudi, K.; Lang, J.D.; Nair, B.G. Improving Operating Room Efficiency: Machine Learning Approach to Predict Case-Time Duration. J. Am. Coll. Surg. 2019, 229, 346–354.e3. [Google Scholar] [CrossRef]







| Feature/Predictor | MATLAB® Function |
|---|---|
| Band power [pixel]: it returns the ‘average power’ or average l2 norm (average Euclidean norm) of the input signal [pixel] | bandpower https://it.mathworks.com/help/signal/ref/bandpower.html |
| Power bandwidth [Hz]: it returns the 3 dB (half-power) bandwidth of the input signal | powerbw https://it.mathworks.com/help/signal/ref/powerbw.html |
| Occupied bandwidth [Hz]: it returns the 99% occupied bandwidth of the input signal | obw https://it.mathworks.com/help/signal/ref/obw.html |
| Spurious free dynamic range [dB]: it returns the SFDR of the real sinusoidal-like input signal | sfdr https://it.mathworks.com/help/signal/ref/sfdr.html |
| Signal to noise and distortion ratio [dB]: it returns the SINAD of the real sinusoidal-like input signal | sinad https://it.mathworks.com/help/signal/ref/sinad.html |
| Signal to noise ratio [dB]: it returns the SNR of the input signal | SNR https://it.mathworks.com/help/signal/ref/snr.html |
| Spectral entropy (information content) of the input signal | pentropy https://it.mathworks.com/help/signal/ref/pentropy.html |
| Classifier | Accuracy (%) |
|---|---|
| Boosted trees (ensemble of trees using the AdaBoost (Adaptive Boosting) algorithm) [32] | 46.5 |
| RUSBoosted trees (ensemble of trees using the RUSBoost (Random Undersampling Boosting) algorithm) [33] | 46.5 |
| Linear discriminant [34] | 66.3 |
| Kernel naïve Bayes [35] | 68.6 |
| Gaussian naïve Bayes [36] | 69.8 |
| Fine Gaussian (Radial Basis) support vector machine (SVM) [37] | 79.1 |
| Fine k-nearest neighbor (KNN) [38] | 86.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo Muzio, F.P.; Rozzi, G.; Rossi, S.; Luciani, G.B.; Foresti, R.; Cabassi, A.; Fassina, L.; Miragoli, M. Artificial Intelligence Supports Decision Making during Open-Chest Surgery of Rare Congenital Heart Defects. J. Clin. Med. 2021, 10, 5330. https://doi.org/10.3390/jcm10225330
Lo Muzio FP, Rozzi G, Rossi S, Luciani GB, Foresti R, Cabassi A, Fassina L, Miragoli M. Artificial Intelligence Supports Decision Making during Open-Chest Surgery of Rare Congenital Heart Defects. Journal of Clinical Medicine. 2021; 10(22):5330. https://doi.org/10.3390/jcm10225330
Chicago/Turabian StyleLo Muzio, Francesco Paolo, Giacomo Rozzi, Stefano Rossi, Giovanni Battista Luciani, Ruben Foresti, Aderville Cabassi, Lorenzo Fassina, and Michele Miragoli. 2021. "Artificial Intelligence Supports Decision Making during Open-Chest Surgery of Rare Congenital Heart Defects" Journal of Clinical Medicine 10, no. 22: 5330. https://doi.org/10.3390/jcm10225330