Albuminuria Is Associated with Hepatic Iron Load in Patients with Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome
Abstract
:1. Introduction
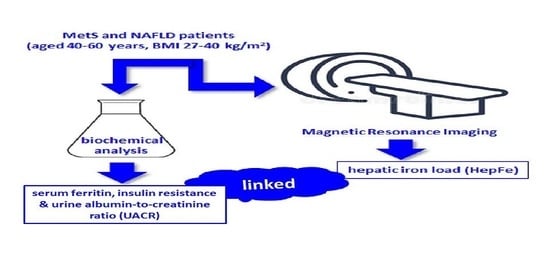
2. Methods
2.1. Subjects
2.2. Ethics
2.3. General Data
2.4. Anthropometric Measurements
2.5. Adherence to the Mediterranean Diet
2.6. Blood and Urine Sample Collection
2.7. Blood and Urine Sample Analysis
2.8. Diagnosis of NAFLD
2.9. Statistical Analysis
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Clinical Trials Registration
References
- Younossi, Z.M. Non-alcoholic fatty liver disease—A global public health perspective. J. Hepatol. 2019, 70, 531–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jézéquel, C.; Lainé, F.; Laviolle, B.; Kiani, A.; Bardou-Jacquet, E.; Deugnier, Y. Both hepatic and body iron stores are increased in dysmetabolic iron overload syndrome. A case-control study. PLoS ONE 2015, 10, e0128530. [Google Scholar] [CrossRef]
- Deugnier, Y.; Bardou-Jacquet, É.; Lainé, F. Dysmetabolic iron overload syndrome (DIOS). Presse Med. 2017, 46 Pt 2, e306–e311. [Google Scholar] [CrossRef]
- Bugianesi, E.; Moscatiello, S.; Ciaravella, M.F.; Marchesini, G. Insulin resistance in nonalcoholic fatty liver disease. Curr. Pharm. Des. 2010, 16, 1941–1951. [Google Scholar] [CrossRef] [PubMed]
- Trombini, P.; Piperno, A. Ferritin, metabolic syndrome and NAFLD: Elective attractions and dangerous liaisons. J. Hepatol. 2007, 46, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Haap, M.; Fritsche, A.; Mensing, H.J.; Häring, H.U.; Stumvoll, M. Association of high serum ferritin concentration with glucose intolerance and insulin resistance in healthy people. Ann. Intern. Med. 2003, 139, 869–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sivasankari, J.; Thiruchelvan, V. Serum Ferritin: An Early Marker of Insulin Resistance in Metabolic Syndrome. Int. J. Sci. 2017, 5, 59–64. [Google Scholar]
- Kim, B.J.; Kim, B.S.; Kang, J.H. The association between serum ferritin level, microalbuminuria and non-alcoholic fatty liver disease in non-diabetic, non-hypertensive men. Clin. Exp. Hypertens 2014, 36, 380–385. [Google Scholar] [CrossRef]
- Amin, R.F.; El Bendary, A.S.; Ezzat, S.E.; Mohamed, W.S. Serum Ferritin level, microalbuminuria and non-alcoholic fatty liver disease in type 2 diabetic patients. Diabetes Metab. Syndr. 2019, 13, 2226–2229. [Google Scholar] [CrossRef]
- Hwang, S.T.; Cho, Y.K.; Yun, J.W.; Park, J.H.; Kim, H.J.; Park, D.I.; Sohn, C.I.; Jeon, W.K.; Kim, B.I.; Rhee, E.J.; et al. Impact of nonalcoholic fatty liver disease on microalbuminuria in patients with prediabetes and diabetes. Intern. Med. J. 2010, 40, 437–442. [Google Scholar] [CrossRef]
- Tuttle, K.R. Renal manifestations of the metabolic syndrome. Nephrol. Dial. Transplant. 2005, 20, 861–864. [Google Scholar] [CrossRef] [Green Version]
- Arnlöv, J.; Evans, J.C.; Meigs, J.B.; Wang, T.J.; Fox, C.S.; Levy, D.; Benjamin, E.J.; D’Agostino, R.B.; Vasan, R.S. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: The Framingham Heart Study. Circulation 2005, 112, 969–975. [Google Scholar] [CrossRef] [Green Version]
- Gerstein, H.C.; Mann, J.F.E.; Yi, O.; Zinman, B.; Dinneen, S.F.; Hoogwerf, B.; Hallé, J.P.; Young, J.; Rashkow, A.; Joyce, C.; et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 2001, 286, 421–426. [Google Scholar] [CrossRef] [Green Version]
- Wachtell, K.; Ibsen, H.; Olsen, M.H.; Borch-Johnsen, K.; Lindholm, L.H.; Mogensen, C.E.; Dahlöf, B.; Devereux, R.B.; Beevers, G.; de Faire, U.; et al. Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: The LIFE study. Ann. Intern. Med. 2003, 139, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Klausen, K.; Borch-Johnsen, K.; Feldt-Rasmussen, B.; Jensen, G.; Clausen, P.; Scharling, H.; Appleyard, M.; Jensen, J.S. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation 2004, 110, 32–35. [Google Scholar] [CrossRef] [Green Version]
- Jessani, S.; Levey, A.S.; Chaturvedi, N.; Jafar, T.H. High normal levels of albuminuria and risk of hypertension in Indo-Asian population. Nephrol. Dial. Transplant. 2012, 27 (Suppl. S3), iii58–iii64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wijarnpreecha, K.; Thongprayoon, C.; Boonpheng, B.; Panjawatanan, P.; Sharma, K.; Ungprasert, P.; Pungpapong, S.; Cheungpasitporn, W. Nonalcoholic fatty liver disease and albuminuria: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2018, 30, 986–994. [Google Scholar] [CrossRef]
- Abd El-Kader, S.M.; El-Den Ashmawy, E.M. Non-alcoholic fatty liver disease: The diagnosis and management. World J. Hepatol. 2015, 7, 846–858. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Diehl, A.M.; Brunt, E.M.; Cusi, K.; Charlton, M.; Sanyal, A.J. The diagnosis and management of non-alcoholic fatty liver disease: Practice Guideline by the American AssociationAmerican Association for the Study of Liver Diseases, American College of Gastroenterology, and the Americanthe American Gastroenterological Association. Hepatology 2012, 55, 2005–2023. [Google Scholar] [PubMed]
- Younes, R.; Bugianesi, E. The Impact of Metabolic Syndrome on the Outcome of NASH: Cirrhosis, Hepatocellular Carcinoma, and Mortality. Curr. Hepatol. Rep. 2018, 17, 336–344. [Google Scholar] [CrossRef]
- Lainé, F.; Bendavid, C.; Moirand, R.; Tessier, S.; Perrin, M.; Guillygomarc’h, A.; Guyader, D.; Calon, E.; Renault, A.; Brissot, P.; et al. Prediction of liver fibrosis in patients with features of the metabolic syndrome regardless of alcohol consumption. Hepatology 2004, 39, 1639–1646. [Google Scholar] [CrossRef] [PubMed]
- The International Diabetic Federation (IDF). The IDF Consensus Worldwide De-Finition of Definition of the Metabolic Syndrome. Available online: http://www.idf.org/webdata/docs/IDF_Meta_def_final.pdf (accessed on 11 April 2020).
- Elosua, R.; García, M.; Aguilar, A.; Molina, L.; Covas, M.I.; Marrugat, J. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish Women. Med. Sci. Sports Exerc. 2000, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Elosua, R.; Marrugat, J.; Molina, L.; Pons, S.; Pujol, E. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish Men. Am. J. Epidemiol. 1994, 139, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Schroder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [Green Version]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Levey, A.S.; Coresh, J.; Greene, T.; Stevens, L.A.; Zhang, Y.L.; Hendriksen, S.; Kusek, J.W.; Van Lente, F. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006, 145, 247–254. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro 3rd, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Tang, A.; Tan, J.; Sun, M.; Hamilton, G.; Bydder, M.; Wolfson, T.; Gamst, A.C.; Middleton, M.; Brunt, E.M.; Loomba, R.; et al. Nonalcoholic fatty liver disease: MR imaging of liver proton density fat fraction to assess hepatic steatosis. Radiology 2013, 267, 422–431. [Google Scholar] [CrossRef] [Green Version]
- Chandarana, H.; Lim, R.P.; Jensen, J.H.; Hajdu, C.H.; Losada, M.; Babb, J.S.; Huffman, S.; Taouli, B. Hepatic Iron Deposition in Patients With Liver Disease: Preliminary Experience With Breath-Hold Multiecho T2*-Weighted Sequence. Am. J. Roentgenol. 2009, 193, 1261–1267. [Google Scholar] [CrossRef]
- The French METAVIR Cooperative Study Group. Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. Hepatology 1994, 20, 15–20. [Google Scholar] [CrossRef]
- Ferraioli, G.; Maiocchi, L.; Lissandrin, R.; De Silvestri, A.; Tinelli, C.; Filice, C. Non-Invasive Staging of Liver Fibrosis in Patients with Chronic Viral Hepatitis: Performance of a Shear Wave Measurement Method. Poster No.: B-1248. ECR Congress 2017. Available online: https://epos.myesr.org/poster/esr/ecr2017/B-1248 (accessed on 30 April 2021).
- De la Iglesia, R.; Lopez-Legarrea, P.; Abete, I.; Bondia-Pons, I.; Navas-Carretero, S.; Forga, L.; Martinez, J.A.; Zulet, M.A. A new dietary strategy for long-term treatment of the metabolic syndrome is compared with the American Heart Association (AHA) guidelines: The MEtabolic Syndrome REduction in NAvarra (RESMENA) project. Br. J. Nutr. 2014, 111, 643–652. [Google Scholar] [CrossRef] [Green Version]
- Rubio Herrera, M.A. Evidence-based medicine: Nutrition in obesity. Endocrinol. Nutr. 2005, 52 (Suppl. S2), 102–109. [Google Scholar] [CrossRef]
- Mendler, M.H.; Turlin, B.; Moirand, R.; Jouanolle, A.M.; Sapey, T.; Guyader, D.; Le Gall, J.Y.; Brissot, P.; David, V.; Deugnier, Y. Insulin resistance-associated hepatic iron overload. Gastroenterology 1999, 117, 1155–1163. [Google Scholar] [CrossRef]
- Ryan, J.D.; Armitage, A.E.; Cobbold, J.F.; Banerjee, R.; Borsani, O.; Dongiovanni, P.; Neubauer, S.; Morovat, R.; Wang, L.M.; Pasricha, S.R.; et al. Hepatic iron is the major determinant of serum ferritin in NAFLD patients. Liver Int. 2017, 38, 164–173. [Google Scholar] [CrossRef]
- Dongiovanni, P.; Fracanzani, A.L.; Fargion, S.; Valenti, L. Iron in fatty liver and in the metabolic syndrome: A promising therapeutic target. J. Hepatol. 2011, 55, 920–932. [Google Scholar] [CrossRef] [PubMed]
- Buzzetti, E.; Petta, S.; Manuguerra, R.; Luong, T.V.; Cabibi, D.; Corradini, E.; Craxì, A.; Pinzani, M.; Tsochatzis, E.; Pietrangelo, A. Evaluating the association of serum ferritin and hepatic iron with disease severity in non-alcoholic fatty liver disease. Liver Int. 2019, 39, 1325–1334. [Google Scholar] [CrossRef] [PubMed]
- Fumeron, F.; Péan, F.; Driss, F.; Balkau, B.; Tichet, J.; Marre, M.; Grandchamp, B.; Insulin Resistance Syndrome (DESIR) Study Group. Ferritin and transferrin are both predictive of the onset of hyperglycemia in men and women over 3 years: The data from an epidemiological study on the Insulin Resistance Syndrome (DESIR) study. Diabetes Care 2006, 29, 2090–2094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryoo, J.H.; Park, S.K.; Jung, J.Y. Elevated Fasting Insulin Level Significantly Increases the Risk of Microalbuminuria. Circ. J. 2015, 79, 210–215. [Google Scholar] [CrossRef] [Green Version]
- Loebstein, R.; Lehotay, D.C.; Luo, X.; Bartfay, W.; Tyler, B.; Sher, G.D. Diabetic nephropathy in hypertransfused patients with beta-thalassemia. The role of oxidative stress. Diabetes Care 1998, 21, 1306–1309. [Google Scholar] [CrossRef]
- Vaziri, N.D. Safety Issues in Iron Treatment in CKD. Semin. Nephrol. 2016, 36, 112–118. [Google Scholar] [CrossRef] [Green Version]
- Ikeda, Y.; Enomoto, H.; Tajima, S.; Izawa-Ishizawa, Y.; Kihira, Y.; Ishizawa, K.; Tomita, S.; Tsuchiya, K.; Tamaki, T. Dietary iron restriction inhibits progression of diabetic nephropathy in db/db mice. Am. J. Physiol.-Renal Physiol. 2013, 304, F1028–F1036. [Google Scholar] [CrossRef]
- Rajapurkar, M.M.; Hegde, U.; Bhattacharya, A.; Alam, M.G.; Shah, S.V. Effect of deferiprone, an oral iron chelator, in diabetic and non-diabetic glomerular disease. Toxicol. Mech. Methods 2013, 23, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Chartampilas, E. Imaging of nonalcoholic fatty liver disease and its clinical utility. Hormones 2018, 17, 69–81. [Google Scholar] [CrossRef] [Green Version]
- Groop, P.H.; Forsblom, C.; Thomas, M.C. Mechanisms of disease: Pathway-selective insulin resistance and microvascular complications of diabetes. Nat. Clin. Pract. Endocrinol. Metab. 2005, 1, 100–110. [Google Scholar] [CrossRef] [PubMed]
- Rashidbeygi, E.; Safabakhsh, M.; Delshad Aghdam, S.; Mohammed, S.H.; Alizadeh, S. Metabolic syndrome and its components are related to a higher risk for albuminuria and proteinuria: Evidence from a meta-analysis on 10,603,067 subjects from 57 studies. Diabetes Metab. Syndr. 2019, 13, 830–843. [Google Scholar] [CrossRef]
- Singh, B.; Saxena, A. Surrogate markers of insulin resistance: A review. World J. Diabetes 2010, 1, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Nestler, J.E.; Barlascini, C.O.; Tetrault, G.A.; Fratkin, M.J.; Clore, J.N.; Blackard, W.G. Increased transcapillary escape rate of albumin in nondiabetic men in response to hyperinsulinemia. Diabetes 1990, 39, 1212–1217. [Google Scholar] [CrossRef] [PubMed]
- Redon, J.; Miralles, A.; Pascual, J.M.; Baldó, E.; Garcia Robles, R.; Carmena, R. Hyperinsulinemia as a determinant of microalbuminuria in essential hypertension. J. Hypertens. 1997, 15, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Gordeuk, V.R.; Reboussin, D.M.; McLaren, C.E.; Barton, J.C.; Acton, R.T.; McLaren, G.D.; Harris, E.L.; Reiss, J.A.; Adams, P.C.; Speechley, M.; et al. Serum ferritin concentrations and body iron stores in a multicenter, multiethnic primary-care population. Am. J. Hematol. 2008, 83, 618–626. [Google Scholar] [CrossRef] [Green Version]
- Jehn, M.; Clark, J.M.; Guallar, E. Serum ferritin and risk of the metabolic syndrome in U.S. adults. Diabetes Care 2004, 27, 2422–2428. [Google Scholar] [CrossRef] [Green Version]
- Branten, A.J.; Swinkels, D.W.; Klasen, I.S.; Wetzels, J.F. Serum ferritin levels are increased in patients with glomerular diseases and proteinuria. Nephrol. Dial. Transplant. 2004, 19, 2754–2760. [Google Scholar] [CrossRef] [PubMed]
- De Mello, V.D.; Zelmanovitz, T.; Perassolo, M.S.; Azevedo, M.J.; Gross, J.L. Withdrawal of red meat from the usual diet reduces albuminuria and improves serum fatty acid profile in type 2 diabetes patients with macroalbuminuria. Am. J. Clin. Nutr. 2006, 83, 1032–1038. [Google Scholar] [CrossRef] [Green Version]
- Facchini, F.S.; Hua, N.W.; Stoohs, R.A. Effect of iron depletion in carbohydrate-intolerant patients with clinical evidence of nonalcoholic fatty liver disease. Gastroenterology 2002, 122, 931–939. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Real, J.M.; Peñarroja, G.; Castro, A.; García-Bragado, F.; Hernández-Aguado, I.; Ricart, W. Blood letting in high-ferritin type 2 diabetes: Effects on insulin sensitivity and beta-cell function. Diabetes 2002, 51, 1000–1004. [Google Scholar] [CrossRef] [Green Version]
- Yoneda, M.; Fujii, H.; Sumida, Y.; Hyogo, H.; Itoh, Y.; Ono, M.; Eguchi, Y.; Suzuki, Y.; Aoki, N.; Kanemasa, K.; et al. Platelet count for predicting fibrosis in nonalcoholic fatty liver disease. J. Gastroenterol. 2011, 46, 1300–1306. [Google Scholar] [CrossRef]
- Milovanovic Alempijevic, T.; Stojkovic Lalosevic, M.; Dumic, I.; Jocic, N.; Pavlovic Markovic, A.; Dragasevic, S.; Jovicic, I.; Lukic, S.; Popovic, D.; Milosavljevic, T. Diagnostic Accuracy of Platelet Count and Platelet Indices in Noninvasive Assessment of Fibrosis in Nonalcoholic Fatty Liver Disease Patients. Can. J. Gastroenterol. Hepatol. 2017, 2017, 6070135. [Google Scholar] [CrossRef] [Green Version]
- Angulo, P.; Hui, J.M.; Marchesini, G.; Bugianesi, E.; George, J.; Farrell, G.C.; Enders, F.; Saksena, S.; Burt, A.D.; Bida, J.P.; et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007, 45, 846–854. [Google Scholar] [CrossRef]
- Ünübol, M.; Ayhan, M.; Güney, E. The relationship between mean platelet volume with microalbuminuria and glycemic control in patients with type II diabetes mellitus. Platelets 2012, 23, 475–480. [Google Scholar] [CrossRef]
- Papanas, N.; Symeonidis, G.; Maltezos, E.; Mavridis, G.; Karavageli, E.; Vosnakidis, T.; Lakasas, G. Mean platelet volume in patients with type 2 diabetes mellitus. Platelets 2004, 15, 475–478. [Google Scholar] [CrossRef] [PubMed]
- Hamilos, M.; Petousis, S.; Parthenakis, F. Interaction between platelets and endothelium: From pathophysiology to new therapeutic options. Cardiovasc. Diagn. Ther. 2018, 8, 568–580. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A. Coagulation activation in diabetes mellitus: The role of hyperglycaemia and therapeutic prospects. Diabetologia 1993, 36, 1119–1125. [Google Scholar] [CrossRef]
- Ferreira, D.; Severo, M.; Araújo, J.; Barros, H.; Guimarães, J.T.; Ramos, E. Association between insulin resistance and haematological parameters: A cohort study from adolescence to adulthood. Diabetes Metab. Res. Rev. 2019, 35, e3194. [Google Scholar] [CrossRef]
- Abdel-Moneim, A.; Mahmoud, B.; Sultan, E.A.; Mahmoud, R. Relationship of leukocytes, platelet indices and adipocytokines in metabolic syndrome patients. Diabetes Metab. Syndr. 2019, 13, 874–880. [Google Scholar] [CrossRef]
- Zhao, F.; Yan, Z.; Meng, Z.; Li, X.; Liu, M.; Ren, X.; Zhu, M.; He, Q.; Zhang, Q.; Song, K.; et al. Relationship between mean platelet volume and metabolic syndrome in Chinese patients. Sci. Rep. 2018, 8, 14574. [Google Scholar] [CrossRef] [Green Version]
- Nelson, J.E.; Klintworth, H.; Kowdley, K.V. Iron metabolism in Nonalcoholic Fatty Liver Disease. Curr. Gastroenterol. Rep. 2012, 14, 8–16. [Google Scholar] [CrossRef]
- Ko, C.; Siddaiah, N.; Berger, J.; Gish, R.; Brandhagen, D.; Sterling, R.K.; Cotler, S.J.; Fontana, R.J.; McCashland, T.M.; Han, S.H.; et al. Prevalence of hepatic iron overload and association with hepatocellular cancer in end-stage liver disease: Results from the National Hemochromatosis Transplant Registry. Liver Int. 2007, 27, 1394–1401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marchesini, G.; Brizi, M.; Morselli Labate, A.M.; Bianchi, G.; Bugianesi, G.; McCullough, A.J.; Forlani, G.; Melchionda, N. Association of non-alcoholic fatty liver disease to insulin resistance. Am. J. Med. 1999, 107, 450–455. [Google Scholar] [CrossRef]
- Marchesini, G.; Brizi, M.; Bianchi, G.; Tomassetti, S.; Bugianesi, E.; Lenzi, M.; McCullough, A.J.; Natale, S.; Forlani, G.; Melchionda, N. Nonalcoholic fatty liver disease: A feature of the metabolic syndrome. Diabetes 2001, 50, 1844–1850. [Google Scholar] [CrossRef] [Green Version]
- Sanyal, A.J.; Campbell-Sargent, C.; Mirshahi, F.; Rizzo, W.B.; Contos, M.J.; Sterling, R.K.; Luketic, V.A.; Shiffman, M.L.; Clore, J.N. Nonalcoholic steatohepatitis: Association of insulin resistance and mitochondrial abnormalities. Gastroenterology 2001, 120, 1183–1192. [Google Scholar] [CrossRef] [PubMed]
- Yki-Järvinen, H. Liver fat in the pathogenesis of insulin resistance and type 2 diabetes. Dig. Dis. 2010, 28, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Fabbrini, E.; Magkos, F.; Mohammed, B.S.; Pietka, T.; Abumrad, N.A.; Patterson, B.W.; Okunade, A.; Klein, S. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc. Natl. Acad. Sci. USA 2009, 106, 15430–15435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bugianesi, E.; Gastaldelli, A.; Vanni, E.; Gambino, R.; Cassader, M.; Baldi, S.; Ponti, V.; Pagano, G.; Ferrannini, E.; Rizzetto, M. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: Sites and mechanisms. Diabetologia 2005, 48, 634–642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musso, G.; Gambino, R.; Tabibian, J.H.; Ekstedt, M.; Kechagias, S.; Hamaguchi, M.; Hultcrantz, R.; Hagström, H.; Yoon, S.K.; Charatcharoenwitthaya, P.; et al. Association of non-alcoholic fatty liver disease with chronic kidney disease: A systematic review and meta-analysis. PLoS Med. 2014, 11, e1001680. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slee, A.D. Exploring metabolic dysfunction in chronic kidney disease. Nutr. Metab. 2012, 9, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tripepi, G.; Jager, K.J.; Dekker, F.W.; Zoccali, C. Selection Bias and Information Bias in Clinical Research. Nephron Clin. Pract. 2010, 115, c94–c99. [Google Scholar] [CrossRef] [PubMed]


| Female | 30 (40.0%) |
|---|---|
| Who were having menopause | 19 (25.3%) |
| Age (y) (mean ± SD) | 52.7 ± 6.7 (6.86) |
| Currently smoking | 6 (8.0%) |
| Alcohol ≥7 drinks/week | 12 (16.0%) |
| Regular physical activity | |
| None | 34 (45.3%) |
| Light | 27 (36.0%) |
| Moderate | 12 (16.0%) |
| Heavy | 2 (2.7%) |
| Type 2 diabetes | 20 (26.7%) |
| Hypertension | 43 (57.3%) |
| Concomitant medications | |
| Hypoglycemic agents | |
| Oral hypoglycemic agents alone | 18 (24.0%) |
| Antihypertensive agents | |
| Any | 31 (41.3%) |
| Diuretics | 12 (16.0%) |
| μ-blockers | 5 (6.7%) |
| Calcium-channel blockers | 4 (5.3%) |
| ACE inhibitors, ARBs | 28 (37.3%) |
| Lipid-lowering agents | |
| Any | 23 (30.7%) |
| Statins alone | 14 (18.7%) |
| Fibrate alone | 6 (8.0%) |
| Statins and fibrate | 3 (4.0%) |
| Antiplatelet agents | 3 (4.0%) |
| Concomitant medications—other | |
| Any | 49 (65.3%) |
| Thyroid medications | 6 (8%) |
| Depression/anxiety/insomnia | 14 (18.7%) |
| Gout medications | 9 (12.0%) |
| Mean ± SD | Median (IQR) | |
|---|---|---|
| Anthropometric variables | ||
| Weight (kg) | 94.1 ± 13.7 | 92.2 (18.6) |
| BMI (kg/m2) | 33.6 ± 4.0 | 32.6 (6.0) |
| Waist circumference (cm) | 112.9 ± 8.8 | 111.3 (14.6) |
| Total body fat (kg) | 32.7 ± 8.0 | 30.3 (9.2) |
| Total body fat (%) | 34.7 ± 6.7 | 33.4 (11.4) |
| Clinical parameters | ||
| Systolic BP (mmHg) | 137.3 ± 16.8 | 136.3 (20.2) |
| Diastolic BP (mmHg) | 82.6 ± 9.3 | 80.7 (13.4) |
| MAP (mmHg) | 100.9 ± 11.1 | 99.0 (13.6) |
| HR (bpm) | 70.6 ± 10.8 | 70.2 (14.1) |
| Metabolic variables | ||
| Glycemia (mg/dL) | 114.1 ± 44.1 | 105.0 (23.0) |
| HbA1c (%) | 6.0 ± 1.2 | 5.7 (0.6) |
| Fasting insulin (µIU/L) | 19.5 ± 9.5 | 17.8 (12.7) |
| HOMA-IR | 5.6 ± 3.4 | 5.1 (4.5) |
| Blood lipids | ||
| Total cholesterol (mg/dL) | 210.0 ± 41.5 | 210.0 (58.0) |
| HDL cholesterol (mg/dL) | 42.4 ± 8.7 | 41.0 (9.0) |
| LDL cholesterol (mg/dL) | 128.1 ± 32.5 | 127.0 (44.7) |
| VLDL cholesterol (mg/dL) | 41.0 ± 30.7 | 35.0 (17.0) |
| Triglycerides (mg/dL) | 203.4 ± 152.1 | 175.0 (86.0) |
| Physical Activity | ||
| METs (min/week) | 3072.2 ± 3641.2 | 1920.0 (2680.2) |
| Mediterranean Diet Adherence | 8.1 ± 2.7 | 8.0 (4.0) |
| Other variables | ||
| Uric acid (mg/dL) | 6.3 ± 1.5 | 6.3 (1.8) |
| Serum Ferritin (ng/mL) | 155.5 ± 156.6 | 98.0 (138.0) |
| Transferrin (mg/dL) | 271.5 ± 38.0 | 268.5 (42.7) |
| CK (U/L) | 149.9 ± 161.4 | 120.0 (91.0) |
| PCR (mg/dL) | 0.5 ± 0.6 | 0.3 (0.5) |
| TSH (mUI/L) | 2.02± 1.1 | 1.8 (1.3) |
| Mean ± SD | Median (IQR) | |
|---|---|---|
| Hepatic variables | ||
| Stages of NAFLD | ||
| 1: Mild (6.4%–17.4%) | 49 (65.3%) | |
| 2: Moderate (17.4%–22.1%) | 9 (12.0%) | |
| 3: Severe (>22.1%) | 17 (22.7%) | |
| NAFLD—Mean liver fat % | 15.9 ± 9.9 | 12.4 (11.3) |
| Stages of HepFe (ms) | ||
| 0: Normal (>20 ms) | 68 (90.7%) | |
| 1: Mild/moderate (10–20 ms) | 5 (6.7%) | |
| 2: Severe (<10 ms) | 2 (2.7%) | |
| Hepatic iron load (mg/g) | 1.2 ± 0.3 | 1.1 (0.3) |
| Hepatic iron load (ms) | 27.0 ± 5.5 | 26.9 (7.1) |
| Stages of fibrosis | ||
| F0–F1: Normal (<6.44 kPa) | 55 (73.3%) | |
| F2: Mild (6.44–7.81 kPa) | 7 (9.3%) | |
| F3: Moderate (7.82–8.39 kPa) | 1 (1.3%) | |
| F4: Severe (>8.39 kPa) | 4 (5.3%) | |
| Fibrosis (kPa) | 5.2 ± 1.5 | 4.90 (1.80) |
| Liver function test | ||
| AST (IU/L) | 27.1 ± 14.6 | 23.0 (11.50) |
| ALT (IU/L) | 38.4 ± 34.7 | 31.0 (25.0) |
| GGT (IU/L) | 58.4 ± 71.5 | 38.0 (28.0) |
| Total bilirubin (mg/dL) | 0.71± 0.4 | 0.60 (0.35) |
| Platelets (103/uL) | 238.4 ± 46.8 | 240.0 (63.0) |
| Kidney function | ||
| MDRD (ml/min/1.73 m2) | 91.7 ± 14.2 | 94.4 (18.9) |
| CKD-EPI (ml/min/1.73 m2) | 92.3 ± 17.9 | 98.8 (16.7) |
| Serum albumin (g/L) | 4.4 ± 0.4 | 4.4 (0.3) |
| Serum creatinine (mg/dL) | 0.8 ± 0.2 | 0.8 (0.1) |
| Urea (mg/dL) | 37.3 ± 10.6 | 34.0 (15.0) |
| Urine albumin (mg/L) | 13.4 ± 21.4 | 6.0 (11.5) |
| Urine creatinine (mg/L) | 121.7 ± 48.5 | 116.9 (64.8) |
| UACR (mg/g) | 11.3 ± 17.5 | 5.6 (7.75) |
| Albuminuria high normal (10–29 mg/g) | 20 (26.0%) | |
| Increased albuminuria (>30 mg/g) | 6 (8.0%) |
| b (95%CI) | Std. Error | β | p | |
|---|---|---|---|---|
| Model 1—Variables | ||||
| (Constant) | −1.48 (−2.63–(−0.32)) | 0.58 | 0.010 | |
| NAFLD—Mean liver fat % | 0.00 (−0.01–0.01) | 0.01 | −0.09 | 0.490 |
| Triglycerides (mg/dL) | 0.00 (0.00–0.00) | 0.00 | 0.04 | 0.740 |
| Hepatic iron load (mg/g) | 0.43 (0.02–0.84) | 0.20 | 0.30 | 0.040 |
| Serum Ferritin (ng/mL) | 0.00 (0.00–0.00) | 0.00 | 0.33 | 0.020 |
| Fasting insulin (µIU/L) # | 1.00 (−0.01–2.01) | 0.51 | 0.55 | 0.050 |
| HOMA-IR # | −0.60 (−1.46–0.26) | 0.43 | −0.40 | 0.170 |
| Platelets (103/uL) | 0.00 (0.00–0.01) | 0.00 | 0.48 | < 0.001 |
| Model 2—Variables | ||||
| (Constant) | −4.26 (−7.95–(−0.58)) | 1.84 | 0.020 | |
| NAFLD—Mean liver fat % | 0.00 (−0.02–0.02) | 0.01 | 0.11 | 0.660 |
| Triglycerides (mg/dL) | 0.00 (0.00–0.00) | 0.00 | 0.01 | 0.920 |
| Hepatic iron load (mg/g) | 0.54 (0.08–1.00) | 0.23 | 0.38 | 0.020 |
| Serum Ferritin (ng/mL) | 0.00 (0.00–0.00) | 0.00 | 0.34 | 0.040 |
| Fasting insulin (µIU/L) # | 2.60 (0.01–5.18) | 1.29 | 1.43 | 0.049 |
| HOMA-IR # | −2.10 (−4.53–0.33) | 1.21 | −1.41 | 0.090 |
| Platelets (103/µL) | 0.00 (0.00–0.01) | 0.00 | 0.39 | 0.009 |
| Gender (m/f) | 0.05 (−0.16–0.26) | 0.10 | 0.07 | 0.620 |
| Age (y) | 0.01 (−0.01–0.03) | 0.01 | 0.17 | 0.230 |
| eGFR (ml/min/1.73 m2) | 0.00 (0.00–0.01) | 0.00 | 0.20 | 0.150 |
| HbA1c (%) | 0.16 (−0.05–0.37) | 0.11 | 0.51 | 0.140 |
| T2DM (y/n) | −0.10 (−0.36–0.16) | 0.13 | −0.12 | 0.430 |
| Stage of NAFLD (1/2/3) | −0.08 (−0.31–0.15) | 0.11 | −0.18 | 0.480 |
| Liver fibrosis (y/n) | −0.01 (−0.25–0.23) | 0.12 | −0.01 | 0.920 |
| Stage 0 (n = 68) | Stage 1–2 (n = 7) | ||
|---|---|---|---|
| Mean ± SD | Mean ± SD | p | |
| Weight (kg) | 93.5 ± 13.5 | 101.0 ± 15.3 | 0.290 |
| BMI (kg/m2) | 33.4 ± 4.0 | 34.7 ± 3.5 | 0.440 |
| Waist circumference (cm) | 112.6 ± 8.7 | 115.8 ± 9.9 | 0.480 |
| Systolic BP (mmHg) | 136.2 ± 16.6 | 149.7 ± 15.8 | 0.090 |
| Diastolic BP (mmHg) | 81.7 ± 8.7 | 92.0 ± 10.4 | 0.060 |
| MAP (mmHg) | 99.9 ± 10.6 | 111.2± 11.8 | 0.070 |
| HR (bpm) | 70.1 ± 10.0 | 75.5 ± 17.5 | 0.490 |
| Blood glucose (mg/dL) | 112.2 ± 44.2 | 132.3 ± 41.6 | 0.260 |
| HbA1c (%) | 6.0 ± 1.3 | 6.1 ± 1.1 | 0.910 |
| Fasting insulin (µIU/L)# | 19.0 ± 9.4 | 25.6 ± 9.2 | 0.130 |
| HOMA-IR # | 5.3 ± 3.1 | 9.5 ± 5.4 | 0.040 |
| Serum ferritin (ng/mL) | 125.1 ± 114.4 | 495.0 ± 172.1 | 0.003 |
| HDL-cholesterol (mg/dL) | 42.6 ± 9.0 | 40.1 ± 3.3 | 0.160 |
| Triglycerides (mg/dL) | 187.9 ± 97.7 | 353.1 ± 387.1 | 0.300 |
| NAFLD (mean fat %) | 14.2 ± 7.5 | 31.8 ± 16.2 | 0.030 |
| Fibrosis (kPa) | 5.1 ± 1.5 | 5.7 ± 1.0 | 0.200 |
| HepFe (mg/g) | 1.1 ± 0.1 | 1.8 ± 0.5 | 0.007 |
| Platelets (103/uL) | 240.5 ± 45.7 | 218.7 ± 56.8 | 0.360 |
| MDRD (ml/min/1.73 m2) | 92.2 ± 13.7 | 86.2 ± 19.0 | 0.440 |
| CKD-EPI (ml/min/1.73 m2) | 92.9 ± 16.9 | 86.5 ± 26.8 | 0.560 |
| UACR (mg/g) # | 8.2 ± 8.5 | 40.0 ± 42.1 | 0.020 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbate, M.; Montemayor, S.; Mascaró, C.M.; Casares, M.; Gómez, C.; Ugarriza, L.; Tejada, S.; Abete, I.; Zulet, M.Á.; Sureda, A.; et al. Albuminuria Is Associated with Hepatic Iron Load in Patients with Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome. J. Clin. Med. 2021, 10, 3187. https://doi.org/10.3390/jcm10143187
Abbate M, Montemayor S, Mascaró CM, Casares M, Gómez C, Ugarriza L, Tejada S, Abete I, Zulet MÁ, Sureda A, et al. Albuminuria Is Associated with Hepatic Iron Load in Patients with Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome. Journal of Clinical Medicine. 2021; 10(14):3187. https://doi.org/10.3390/jcm10143187
Chicago/Turabian StyleAbbate, Manuela, Sofía Montemayor, Catalina M. Mascaró, Miguel Casares, Cristina Gómez, Lucía Ugarriza, Silvia Tejada, Itziar Abete, M. Ángeles Zulet, Antoni Sureda, and et al. 2021. "Albuminuria Is Associated with Hepatic Iron Load in Patients with Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome" Journal of Clinical Medicine 10, no. 14: 3187. https://doi.org/10.3390/jcm10143187