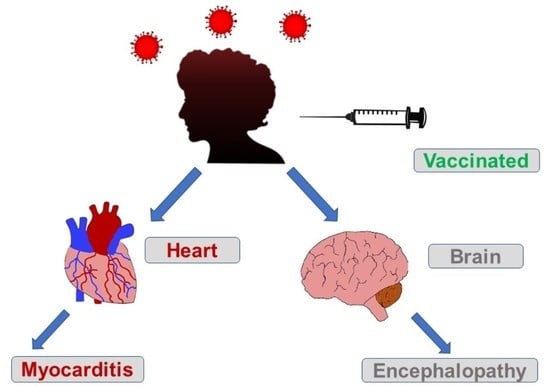
A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously
Abstract
:1. Introduction
2. Case Presentation
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lakhanpal, M.; Sarkar, D.; Kumar, R.; Yadav, I. Reduction in the Rate of Mortality of Moderate to Severe COVID 19 Infected Patients with the use of Remdesivir—A Tertiary Care Hospital-Based Retrospective Observational Study. Anesth. Essays Res. 2022, 16, 296–300. [Google Scholar] [CrossRef]
- Fiolet, T.; Kherabi, Y.; MacDonald, C.J.; Ghosn, J.; Peiffer-Smadja, N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: A narrative review. Clin. Microbiol. Infect. 2022, 28, 202–221. [Google Scholar] [CrossRef] [PubMed]
- Ferdinands, J.M.; Rao, S.; Dixon, B.E.; Mitchell, P.K.; DeSilva, M.B.; Irving, S.A.; Lewis, N.; Natarajan, K.; Stenehjem, E.; Grannis, S.J.; et al. Waning 2-Dose and 3-Dose Effectiveness of MRNA Vaccines Against COVID-19–Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance—VISION Network, 10 States, August 2021–January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Annavajhala, M.K.; Mohri, H.; Wang, P.; Nair, M.; Zucker, J.E.; Sheng, Z.; Gomez-Simmonds, A.; Kelley, A.L.; Tagliavia, M.; Huang, Y.; et al. Emergence and expansion of SARS-CoV-2 B.1.526 after identification in New York. Nature 2021, 597, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Rodríguez-Jiménez, J.; Cancela-Cilleruelo, I.; Guerrero-Peral, A.; Martín-Guerrero, J.D.; García-Azorín, D.; Cornejo-Mazzuchelli, A.; Hernández-Barrera, V.; Pellicer-Valero, O.J. Post-COVID-19 Symptoms 2 Years After SARS-CoV-2 Infection Among Hospitalized vs Nonhospitalized Patients. JAMA Netw. Open 2022, 5, 2242106. [Google Scholar] [CrossRef] [PubMed]
- Inciardi, R.M.; Lupi, L.; Zaccone, G.; Italia, L.; Raffo, M.; Tomasoni, D.; Cani, D.S.; Cerini, M.; Farina, D.; Gavazzi, E.; et al. Cardiac Involvement in a Patient with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 819–824. [Google Scholar] [CrossRef] [Green Version]
- Ebinger, J.E.; Driver, M.; Joung, S.; Tran, T.; Barajas, D.; Wu, M.; Botting, P.G.; Navarrette, J.; Sun, N.; Cheng, S. Hypertension and Excess Risk for Severe COVID-19 Illness Despite Booster Vaccination. Hypertension 2022, 79, e132–e134. [Google Scholar] [CrossRef]
- Xiong, T.Y.; Redwood, S.; Prendergast, B.; Chen, M. Coronaviruses and the cardiovascular system: Acute and long-term implications. Eur. Heart J. 2020, 41, 1798–1800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atri, D.; Siddiqi, H.K.; Lang, J.P.; Nauffal, V.; Morrow, D.A.; Bohula, E.A. COVID-19 for the Cardiologist: Basic Virology, Epidemiology, Cardiac Manifestations, and Potential Therapeutic Strategies. JACC Basic Transl. Sci. 2020, 5, 518–536. [Google Scholar] [CrossRef]
- Nasab, E.M.; Aghajani, H.; Makoei, R.H.; Athari, S.S. COVID-19′s Immuno-Pathology and Cardiovascular Diseases. J. Investig. Med. 2023, 71, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Deng, Q.; Hu, B.; Zhang, Y.; Wang, H.; Zhou, X.; Hu, W.; Cheng, Y.; Yan, J.; Ping, H.; Zhou, Q. Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. Int. J. Cardiol. 2020, 311, 116–121. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683–690. [Google Scholar] [CrossRef] [Green Version]
- Marra, D.E.; Busl, K.M.; Robinson, C.P.; Bruzzone, M.J.; Miller, A.H.; Chen, Z.; Guo, Y.; Lyu, T.; Bian, J.; Smith, G.E. Examination of Early CNS Symptoms and Severe Coronavirus Disease 2019: A Multicenter Observational Case Series. Crit. Care Explor. 2021, 3, e0456. [Google Scholar] [CrossRef]
- Ghannam, M.; Alshaer, Q.; Al-Chalabi, M.; Zakarna, L.; Robertson, J.; Manousakis, G. Neurological involvement of coronavirus disease 2019: A systematic review. J. Neurol. 2020, 267, 3135–3153. [Google Scholar] [CrossRef]
- Siahaan, Y.M.T.; Puspitasari, V.; Pangestu, A. COVID-19-Associated Encephalopathy: Systematic Review of Case Reports. J. Clin. Neurol. 2022, 18, 194–206. [Google Scholar] [CrossRef]
- Baig, A.M.; Khaleeq, A.; Ali, U.; Syeda, H. Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem. Neurosci. 2020, 11, 995–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaudhuri, A.; Kennedy, P.G. Diagnosis and treatment of viral encephalitis. Postgrad. Med. J. 2002, 78, 575–583. [Google Scholar] [CrossRef] [Green Version]
- Pizzato Tondo, L.; Beck Paglioli Neto, E.; Arpini, S.; Passos, G.; Becker, J. Encephalopathy Due to COVID-19 With Great Response to Glucocorticoids. Cureus 2021, 13, e17845. [Google Scholar] [CrossRef] [PubMed]
- Michael, B.D.; Walton, D.; Westenberg, E.; García-Azorín, D.; Singh, B.; Tamborska, A.A.; Netravathi, M.; Chomba, M.; Wood, G.K.; Easton, A.; et al. Consensus Clinical Guidance for Diagnosis and Management of Adult COVID-19 Encephalopathy Patients. J. Neuropsychiatry Clin. Neurosci. 2023, 35, 12–27. [Google Scholar] [CrossRef] [PubMed]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahman, S.; Montero, M.T.V.; Rowe, K.; Kirton, R.; Kunik, F., Jr. Epidemiology, pathogenesis, clinical presentations, diagnosis and treatment of COVID-19: A review of current evidence. Expert Rev. Clin. Pharmacol. 2021, 14, 601–621. [Google Scholar] [CrossRef] [PubMed]
- Scialo, F.; Daniele, A.; Amato, F.; Pastore, L.; Matera, M.G.; Cazzola, M.; Castaldo, G.; Bianco, A. ACE2: The Major Cell Entry Receptor for SARS-CoV-2. Lung 2020, 198, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Rat, P.; Olivier, E.; Dutot, M. SARS-CoV-2 vs. SARS-CoV-1 management: Antibiotics and inflammasome modulators potential. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7880–7885. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Chen, K.; Zou, J.; Han, P.; Hao, J.; Han, Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. 2020, 14, 185–192. [Google Scholar] [CrossRef] [Green Version]
- Zheng, Z.; Peng, F.; Xu, B.; Zhao, J.; Liu, H.; Peng, J.; Li, Q.; Jiang, C.; Zhou, Y.; Liu, S.; et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020, 81, e16–e25. [Google Scholar] [CrossRef]
- Haussner, W.; DeRosa, A.P.; Haussner, D.; Tran, J.; Torres-Lavoro, J.; Kamler, J.; Shah, K. COVID-19 associated myocarditis: A systematic review. Am. J. Emerg. Med. 2022, 51, 150–155. [Google Scholar] [CrossRef]
- Michard, F.; Vieillard-Baron, A. Critically ill patients with COVID-19: Are they hemodynamically unstable and do we know why? Intensive Care Med. 2021, 47, 254–255. [Google Scholar] [CrossRef] [PubMed]
- Purdy, A.; Ido, F.; Sterner, S.; Tesoriero, E.; Matthews, T.; Singh, A. Myocarditis in COVID-19 presenting with cardiogenic shock: A case series. Eur. Heart J. Case Rep. 2021, 5, ytab028. [Google Scholar] [CrossRef]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on etiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef]
- Assad, J.; Femia, G.; Pender, P.; Badie, T.; Rajaratnam, R. Takotsubo Syndrome: A Review of Presentation, Diagnosis and Management. Clin. Med. Insights Cardiol. 2022, 16, 11795468211065782. [Google Scholar] [CrossRef] [PubMed]
- Oster, M.E.; Shay, D.K.; Su, J.R.; Gee, J.; Creech, C.B.; Broder, K.R.; Edwards, K.; Soslow, J.H.; Dendy, J.M.; Schlaudecker, E.; et al. Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021. JAMA 2022, 327, 331–340. [Google Scholar] [CrossRef]
- Park, D.Y.; An, S.; Kaur, A.; Malhotra, S.; Vij, A. Myocarditis after COVID-19 mRNA vaccination: A systematic review of case reports and case series. Clin. Cardiol. 2022, 45, 691–700. [Google Scholar] [CrossRef]
- Lane, S.; Yeomans, A.; Shakir, S. Systematic review of spontaneous reports of myocarditis and pericarditis in transplant recipients and immunocompromised patients following COVID-19 mRNA vaccination. BMJ Open 2022, 12, e060425. [Google Scholar] [CrossRef]
- Liotta, E.M.; Batra, A.; Clark, J.R.; Shlobin, N.A.; Hoffman, S.C.; Orban, Z.S.; Koralnik, I.J. Frequent Neurologic Manifestations and Encephalopathy-Associated Morbidity in COVID-19 Patients. Ann. Clin. Transl. Neurol. 2020, 7, 2221–2230. [Google Scholar] [CrossRef] [PubMed]
- Mavroudis, I.; Kazis, D.; Chowdhury, R.; Petridis, F.; Costa, V.; Balmus, I.-M.; Ciobica, A.; Luca, A.-C.; Radu, I.; Dobrin, R.P.; et al. Post-Concussion Syndrome and Chronic Traumatic Encephalopathy: Narrative Review on the Neuropathology, Neuroimaging and Fluid Biomarkers. Diagnostics 2022, 12, 740. [Google Scholar] [CrossRef] [PubMed]
- Psimaras, D.; Carpentier, A.F.; Rossi, C.; Euronetwork, P.N.S. Cerebrospinal fluid study in paraneoplastic syndromes. J. Neurol. Neurosurg. Psychiatry 2010, 8, 42–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agrawal, K.; Agrawal, N. A Rare Case of Paraneoplastic Encephalitis in Association with Breast Cancer. J. Med. Cases 2018, 9, 296–302. [Google Scholar] [CrossRef]
- Zhang, R.; Sun, C.; Chen, X.; Han, Y.; Zang, W.; Jiang, C.; Wang, J.; Wang, J. COVID-19-Related Brain Injury: The Potential Role of Ferroptosis. J. Inflamm. Res. 2022, 15, 2181–2198. [Google Scholar] [CrossRef]
- Hoerger, M.; Gerhart, J.; Swartz, M.C. Variability in COVID-19 Vaccine Response Among People with Cancer: What Health Care Strategy Best Protects the Vulnerable? JAMA Oncol. 2022. [Google Scholar] [CrossRef]
- Bergler-Klein, J.; Rainer, P.P.; Wallner, M.; Zaruba, M.M.; Dörler, J.; Böhmer, A.; Buchacher, T.; Frey, M.; Adlbrecht, C.; Bartsch, R.; et al. Cardio-oncology in Austria: Cardiotoxicity and surveillance of anti-cancer therapies: Position paper of the Heart Failure Working Group of the Austrian Society of Cardiology. Wien. Klin. Wochenschr. 2022, 134, 654–674. [Google Scholar] [CrossRef] [PubMed]



| Lab | Date | Value | Normal Value |
|---|---|---|---|
| Troponin T | 23 October 2022 | 42 ng/L | <14 ng/L |
| 27 October 2022 | 27 ng/L | ||
| CA 15-3 | 24 October 2022 | 16.8 U/mL | <30 U/mL |
| CA 19-9 | 24 October 2022 | 7 U/mL | <35 U/mL |
| CA 27.29 | 24 October 2022 | 21.9 U/mL | <38.6 U/mL |
| CEA | 24 October 2022 | 1.5 ng/mL | <3.4 ng/mL |
| proBNP | 27 October 2022 | 7616 pg/mL | <125 pg/mL |
| Anatomy | Label | Value | Normal Value |
|---|---|---|---|
| Interventricular Septum | IVSd | 0.8 cm | (0.6–0.9 cm) |
| Left Atrium | LADs | 2.3 cm | (2.7–3.9 cm) |
| Left Ventricle | LVOTd | 1.7 cm | (1.8–2 cm) |
| Left Ventricle | LVDd | 3.3 cm | (3.8–5.2 cm) |
| Left Ventricle | LVEF, MOD4 | 37% | (54–74%) |
| Left Ventricle | LVEF, MOD2 | 25% | (54–74%) |
| Left Ventricle | LV Mass Index | 41.5 g/m2 | (43–95 g/m2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saeedullah, U.; Abbas, A.M.; Ward, C.; Bayya, M.; Bhandari, J.; Abbas, A.M.; DeLeon, J.; Reiss, A.B. A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously. Vaccines 2023, 11, 541. https://doi.org/10.3390/vaccines11030541
Saeedullah U, Abbas AM, Ward C, Bayya M, Bhandari J, Abbas AM, DeLeon J, Reiss AB. A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously. Vaccines. 2023; 11(3):541. https://doi.org/10.3390/vaccines11030541
Chicago/Turabian StyleSaeedullah, Usman, Anas M. Abbas, Caitlin Ward, Maha Bayya, Jenish Bhandari, Araf M. Abbas, Joshua DeLeon, and Allison B. Reiss. 2023. "A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously" Vaccines 11, no. 3: 541. https://doi.org/10.3390/vaccines11030541