Association of Antioxidants Use with All-Cause and Cause-Specific Mortality: A Prospective Study of the UK Biobank
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study and Participants
2.2. Exposure Assessment
2.3. Outcome Assessment
2.4. Statistical Analyses
3. Results
3.1. Baseline Characteristics of UK Biobank Participants
3.2. Antioxidants Use and All-Cause Mortality
3.3. Antioxidants Use and Cause-Specific Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dauchet, L.; Amouyel, P.; Hercberg, S.; Dallongeville, J. Fruit and vegetable consumption and risk fruit and vegetable consumption and risk of coronary heart disease: A meta-analysis of cohort studies. J. Nutr. 2006, 136, 2588–2593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Diet, Nutrition and the Prevention of Chronic Diseases; Technical Report Series 797; WHO: Geneva, Switzerland, 1990; Available online: https://www.who.int/nutrition/publications/obesity/WHO_TRS_797/en/ (accessed on 18 November 2020).
- NHS. Why 5 a Day? Available online: https://www.nhs.uk/live-well/eat-well/why-5-a-day/ (accessed on 5 November 2020).
- DGE. Fruit and Vegetables. It’s the Quantity. Available online: https://www.dge.de/wissenschaft/weitere-publikationen/fachinformationen/obst-und-gemuese-die-menge-machts/ (accessed on 5 November 2020).
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed. Available online: http://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 5 November 2020).
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—A systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ouyang, Y.; Liu, J.; Zhu, M.; Zhao, G.; Bao, W.; Hu, F.B. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 2014, 349, g4490. [Google Scholar] [CrossRef] [Green Version]
- Hertog, M.G.L.; Bueno-de-Mesquita, H.B.; Fehily, A.M.; Sweetman, P.M.; Elwood, P.C.; Kromhout, D. Fruit and vegetable consumption and cancer mortality in the caerphilly study. Cancer Epidemiol. Biomark. Prevent. 1996, 5, 673–677. [Google Scholar]
- Fortmann, S.P.; Burda, B.U.; Senger, C.A.; Lin, J.S.; Whitlock, E.P. Vitamin and mineral supplements in the primary prevention of vitamin and mineral supplements in the primary prevention of cardiovascular disease and cancer: An updated systematic evidence review for the U.S. preventive services task force. Ann. Intern. Med. 2013, 159, 824–834. [Google Scholar] [CrossRef] [PubMed]
- NHS. Supplements. Who Needs Them? A Behind the Headlines Report. Available online: https://www.nhs.uk/news/2011/05May/Documents/BtH_supplements.pdf (accessed on 18 October 2020).
- Marra, M.V.; Boyar, A.P. Position of the American Dietetic Association: Nutrient supplementation. J. Am. Diet. Assoc. 2009, 109, 2073–2085. [Google Scholar] [CrossRef]
- Bechthold, A.; Albrecht, V.; Leschik-Bonnet, E.; Heseker, H. DGE statement: Evaluation of vitamin supplies in Germany, part 2: Critical vitamins and vitamin supplies in special situations. Ernähr. Umsch. 2012, 59, 396–401. [Google Scholar] [CrossRef]
- Skeie, G.; Braaten, T.; Hjartåker, A.; Lentjes, M.; Amiano, P.; Jakszyn, P.; Pala, V.; Palanca, A.; Niekerk, E.M.; Verhagen, H.; et al. Use of dietary supplements in the European Prospective Investigation into cancer and nutrition calibration study. Eur. J. Clin. Nutr. 2009, 63 (Suppl. S4), S226–S238. [Google Scholar] [CrossRef]
- Food Standards Agency. Food Supplements Consumer Research. Available online: https://www.food.gov.uk/sites/default/files/media/document/food-supplements-consumer-research.pdf (accessed on 16 October 2020).
- Market Analysis Report. Dietary Supplements Market Size, Share & Trends Analysis Report by Ingredient (Vitamins, Minerals), by Form, by Application, by End User, by Distribution Channel, by Region, and Segment Forecasts, 2020–2027. Available online: https://www.grandviewresearch.com/industry-analysis/dietary-supplements-market (accessed on 4 November 2020).
- UK Biobank. Protocol for a Large-Scale Prospective Epidemiological Resource; UK Biobank Coordinating Centre: Stockport, UK; Available online: https://www.ukbiobank.ac.uk/wp-content/uploads/2011/11/UK-Biobank-Protocol.pdf (accessed on 2 May 2020).
- UK Biobank. Mortality Data: Linkage from National Death Registries; Version 2.0; UK Biobank: Stockport, UK; Available online: https://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/DeathLinkage.pdf (accessed on 5 November 2020).
- Behrendt, I.; Fasshauer, M.; Eichner, G. Gluten intake and all-cause and cause-specific mortality: Prospective findings from the UK Biobank. J. Nutr. 2020. [Google Scholar] [CrossRef]
- Behrendt, I.; Fasshauer, M.; Eichner, G. Gluten intake and metabolic health: Conflicting findings from the UK Biobank. Eur. J. Nutr. 2020. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org/ (accessed on 5 November 2020).
- Chen, F.; Du, M.; Blumberg, J.B.; Ho Chui, K.K.; Ruan, M.; Rogers, G.; Shan, Z.; Zeng, L.; Zhang, F.F. Association among dietary supplement use, nutrient intake, and mortality among U.S. adults: A cohort study. Ann. Intern. Med. 2019, 170, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Kaaks, R.; Linseisen, J.; Rohrmann, S. Vitamin/mineral supplementation and cancer, cardiovascular, and all-cause mortality in a German prospective cohort (EPIC-Heidelberg). Eur. J. Nutr. 2012, 51, 407–413. [Google Scholar] [CrossRef] [Green Version]
- Messerer, M.; Håkansson, N.; Wolk, A.; Akesson, A. Dietary supplement use and mortality in a cohort of Swedish men. Br. J. Nutr. 2008, 99, 626–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stampfer, M.J.; Hennekens, C.H.; Manson, J.E.; Colditz, G.A.; Rosner, B.; Willett, W.C. Vitamin E consumption and the risk of coronary disease in women. N. Engl. J. Med. 1993, 328, 1444–1449. [Google Scholar] [CrossRef] [PubMed]
- Pocobelli, G.; Peters, U.; Kristal, A.R.; White, E. Use of supplements of multivitamins, vitamin C, and vitamin E in relation to mortality. Am. J. Epidemiol. 2009, 170, 472–483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Losonczy, K.G.; Harris, T.B.; Havlik, R.J. Vitamin E and vitamin C supplement use and risk of all-cause and coronary heart disease mortality in older persons: The established populations for epidemilogic studies of their elderly. Am. J. Clin. Nutr. 1996, 64, 190–196. [Google Scholar] [CrossRef]
- Neuhouser, M.L.; Wassertheil-Smoller, S.; Thomson, C.; Aragaki, A.; Anderson, G.L.; Manson, J.E.; Patterson, R.E.; Rohan, T.E.; van Horn, L.; Shikany, J.M.; et al. Multivitamin use and risk of cancer and cardiovascular disease in the women’s health initiative cohorts. Arch. Intern. Med. 2009, 169, 294–304. [Google Scholar] [CrossRef]
- Mursu, J.; Robien, K.; Harnack, L.J.; Park, K.; Jacobs, D.R. Dietary supplements and mortality rate in older women: The Iowa women’s health study. Arch. Intern. Med. 2011, 171, 1625–1633. [Google Scholar] [CrossRef]
- Roswall, N.; Olsen, A.; Christensen, J.; Hansen, L.; Dragsted, L.O.; Overvad, K.; Tjønneland, A. Micronutrient intake in relation to all-cause mortality in a prospective Danish cohort. Food Nutr. Res. 2012, 56. [Google Scholar] [CrossRef] [Green Version]
- Brzozowska, A.; Kaluza, J.; Knoops, K.T.B.; de Groot, L.C.P.G.M. Supplement use and mortality: The SENECA study. Eur. J. Nutr. 2008, 47, 131–137. [Google Scholar] [CrossRef] [Green Version]
- Hayden, K.M.; Welsh-Bohmer, K.A.; Wengreen, H.J.; Zandi, P.P.; Lyketsos, C.G.; Breitner, J.C.S. Risk of mortality with vitamin E supplements: The Cache county study. Am. J. Med. 2007, 120, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Watkins, M.L.; Erickson, J.D.; Thu, M.J.; Mulinare, J.; Heath, C.W. Multivitamin use and mortality in a large prospective study. Am. J. Epidemiol. 2000, 152, 149–162. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.J.A.; Spence, J.D.; Giovannucci, E.L.; Kim, Y.-I.; Josse, R.; Vieth, R.; Blanco Mejia, S.; Viguiliouk, E.; Nishi, S.; Sahye-Pudaruth, S.; et al. Supplemental vitamins and minerals for CVD prevention and treatment. J. Am. Coll. Cardiol. 2018, 71, 2570–2584. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-Y.; Murphy, S.P.; Wilkens, L.R.; Henderson, B.E.; Kolonel, L.N. Multivitamin use and the risk of mortality and cancer incidence: The multiethnic cohort study. Am. J. Epidemiol. 2011, 173, 906–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Myung, S.-K.; Kim, Y.; Ju, W.; Choi, H.J.; Bae, W.K. Effects of antioxidant supplements on cancer prevention: Meta-analysis of randomized controlled trials. Ann. Oncol. 2010, 21, 166–179. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Boeing, H.; Stelmach-Mardas, M.; Gottschald, M.; Dietrich, S.; Hoffmann, G.; Chaimani, A. Dietary supplements and risk of cause-specific death, cardiovascular disease, and cancer: A systematic review and meta-analysis of primary prevention trials. Adv. Nutr. 2017, 8, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Muntwyler, J.; Hennekens, C.H.; Manson, J.E.; Buring, J.E.; Gaziano, M.J. Vitamin supplement use in a low-risk population of U.S. male physicians and subsequent cardiovascular mortality. Arch. Intern. Med. 2002, 162. [Google Scholar] [CrossRef]
- Adebamowo, S.N.; Feskanich, D.; Stampfer, M.; Rexrode, K.; Willett, W.C. Multivitamin use and risk of stroke incidence and mortality amongst women. Eur. J. Neurol. 2017, 24, 1266–1273. [Google Scholar] [CrossRef]
- Yochum, L.A.; Folsom, A.R.; Kushi, L.H. Intake of antioxidant vitamins and risk of death from stroke in postmenopausal women. Am. J. Clin. Nutr. 2000, 72, 476–483. [Google Scholar] [CrossRef] [Green Version]
- Kotsopoulos, J.; Narod, S.A. Towards a dietary prevention of hereditary breast cancer. Cancer Causes Control 2005, 16, 125–138. [Google Scholar] [CrossRef]
- Li, M.; Chen, Q.; Ma, T.; Yu, X. Targeting reactive nitrogen species suppresses hereditary pancreatic cancer. Proc. Natl. Acad. Sci. USA 2017, 114, 7106–7111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristics | Overall (n = 345,626) | Antioxidants Non-User (n = 244,467) | Antioxidants User (n = 101,159) | p-Value |
|---|---|---|---|---|
| Age (years) | 57 (49, 63) | 57 (49, 63) | 57 (50, 63) | <0.0001 |
| Female | 176,602 (51.1) | 118,746 (48.6) | 57,856 (57.2) | <0.0001 |
| Smoking status | - | - | - | <0.0001 |
| Never | 188,832 (54.6) | 133,514 (54.6) | 55,318 (54.7) | - |
| Previous | 121,388 (35.1) | 85,153 (34.8) | 36,235 (35.8) | - |
| Current | 35,406 (10.2) | 25,800 (10.6) | 9606 (9.5) | - |
| Alcohol intake | - | - | - | <0.0001 |
| Never | 23,705 (6.9) | 16,346 (6.7) | 7359 (7.3) | - |
| Special occasions only | 35,425 (10.3) | 24,314 (9.9) | 11,111 (11.0) | - |
| One to three times a month | 37,817 (10.9) | 26,472 (10.8) | 11,345 (11.2) | - |
| Once or twice a week | 88,607 (25.6) | 62,630 (25.6) | 25,977 (25.7) | - |
| Three to four times a week | 84,451 (24.4) | 60,319 (24.7) | 24,132 (23.9) | - |
| Daily or almost daily | 75,621 (21.9) | 54,386 (22.2) | 21,235 (21.0) | - |
| Total household income per year (£) | - | - | - | <0.0001 |
| <18,000 | 72,014 (20.8) | 51,015 (20.9) | 20,999 (20.8) | - |
| 18,000–30,999 | 86,006 (24.9) | 60,141 (24.6) | 25,865 (25.6) | - |
| 31,000–51,999 | 92,051 (26.6) | 65,120 (26.6) | 26,931 (26.6) | - |
| 52,000–99,999 | 74,984 (21.7) | 53,479 (21.9) | 21,505 (21.3) | - |
| ≥100,000 | 20,571 (6.0) | 14,712 (6.0) | 5859 (5.8) | - |
| Qualifications | - | - | - | <0.0001 |
| Other | 17,153 (5.0) | 12,022 (4.9) | 5131 (5.1) | - |
| NVQ or HND or HNC equivalent | 22,590 (6.5) | 16,261 (6.7) | 6329 (6.3) | - |
| CSEs or equivalent | 17,736 (5.1) | 13,031 (5.3) | 4705 (4.7) | - |
| O levels/GCSEs or equivalent | 73,121 (21.2) | 51,652 (21.1) | 21,469 (21.2) | - |
| A levels/AS levels or equivalent | 41,584 (12.0) | 28,744 (11.8) | 12,840 (12.7) | - |
| College or university degree | 128,271 (37.1) | 89,265 (36.5) | 39,006 (38.6) | - |
| Noa | 45,171 (13.1) | 33,492 (13.7) | 11,679 (11.5) | - |
| Ethnic background | - | - | - | <0.0001 |
| White | 329,823 (95.4) | 234,403 (95.9) | 95,420 (94.3) | - |
| Non-White | 15,803 (4.6) | 10,064 (4.1) | 5739 (5.7) | - |
| Total physical activity (MET-min/week) | 1760 (809, 3520) | 1710 (773, 3451) | 1878 (889, 3666) | <0.0001 |
| Percentage body fat | 30.3 (24.6, 36.9) | 30.0 (24.5, 36.7) | 30.8 (25.0, 37.3) | <0.0001 |
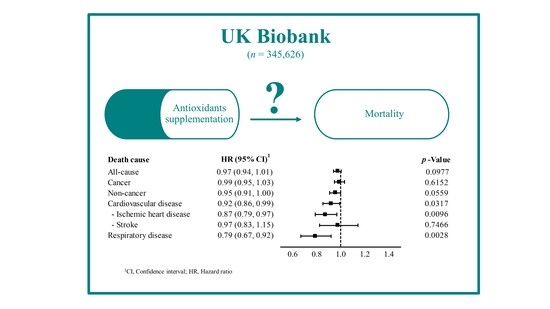
| Cause of Death | Events | HR | 95% CI | p-Value | Holm-Adjusted p-Value |
|---|---|---|---|---|---|
| Cancer | 10,780 | - | - | - | - |
| Non-users | 7706 | 1.00 | - | - | - |
| Users | 3074 | 0.99 | (0.95, 1.03) | 0.6152 | 1.0000 |
| Non-cancer | 8711 | - | - | - | - |
| Non-users | 6396 | 1.00 | - | - | - |
| Users | 2315 | 0.95 | (0.91, 1.00) | 0.0559 | 0.4471 |
| Cancer subtypes: | - | - | - | - | - |
| Colorectal | 1074 | - | - | - | - |
| Non-users | 793 | 1.00 | - | - | - |
| Users | 281 | 0.89 | (0.78, 1.02) | 0.0896 | 0.6269 |
| Bronchus and lung | 1726 | - | - | - | - |
| Non-users | 1275 | 1.00 | - | - | - |
| Users | 451 | 0.92 | (0.82, 1.02) | 0.1199 | 0.7197 |
| Female breast 2 | 828 | - | - | - | - |
| Non-users | 543 | 1.00 | - | - | - |
| Users | 285 | 1.07 | (0.92, 1.23) | 0.3848 | 1.0000 |
| Pancreatic | 783 | - | - | - | - |
| Non-users | 551 | 1.00 | - | - | - |
| Users | 232 | 1.04 | (0.89, 1.22) | 0.5950 | 1.0000 |
| Prostate 3 | 702 | - | - | - | - |
| Non-users | 503 | 1.00 | - | - | - |
| Users | 199 | 1.11 | (0.94, 1.31) | 0.2260 | 1.0000 |
| Non-cancer subtypes: | - | - | - | - | - |
| Cardiovascular disease | 3701 | - | - | - | - |
| Non-users | 2756 | 1.00 | - | - | - |
| Users | 945 | 0.92 | (0.86, 0.99) | 0.0317 | 0.2854 |
| Ischemic heart disease | 2076 | - | - | - | - |
| Non-Users | 1586 | 1.00 | - | - | - |
| Users | 490 | 0.87 | (0.79, 0.97) | 0.0096 | 0.0960 |
| Stroke | 729 | - | - | - | - |
| Non-users | 521 | 1.00 | - | - | - |
| Users | 208 | 0.97 | (0.83, 1.15) | 0.7466 | 1.0000 |
| Respiratory disease | 901 | - | - | - | - |
| Non-users | 697 | 1.00 | - | - | - |
| Users | 204 | 0.79 | (0.67, 0.92) | 0.0028 | 0.0310 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Behrendt, I.; Eichner, G.; Fasshauer, M. Association of Antioxidants Use with All-Cause and Cause-Specific Mortality: A Prospective Study of the UK Biobank. Antioxidants 2020, 9, 1287. https://doi.org/10.3390/antiox9121287
Behrendt I, Eichner G, Fasshauer M. Association of Antioxidants Use with All-Cause and Cause-Specific Mortality: A Prospective Study of the UK Biobank. Antioxidants. 2020; 9(12):1287. https://doi.org/10.3390/antiox9121287
Chicago/Turabian StyleBehrendt, Inken, Gerrit Eichner, and Mathias Fasshauer. 2020. "Association of Antioxidants Use with All-Cause and Cause-Specific Mortality: A Prospective Study of the UK Biobank" Antioxidants 9, no. 12: 1287. https://doi.org/10.3390/antiox9121287