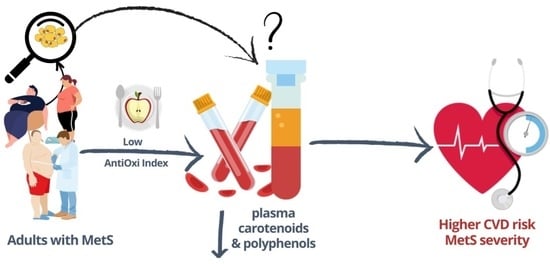
Plasma Carotenoids and Polyphenols and Their Association with MetS: The Need for Nutritional Interventions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Approval
2.2. Study Design and Participants
2.3. Data Collection
2.3.1. Socio-Demographics and Lifestyle Data
2.3.2. Dietary AntiOxi Index
2.3.3. Anthropometry Measurements
2.3.4. Blood Pressure
2.3.5. Blood Sample
2.3.6. Biochemical Analysis
2.3.7. Diagnosis of Metabolic Syndrome and MetS Severity
2.4. Study Group Characteristics
2.5. Statistical Analysis
3. Results
3.1. Effect of MetS and Inflammation on Plasma Bioactive Compounds
3.1.1. Plasma Carotenoids and Number of MetS Components
3.1.2. Plasma Polyphenols and Number of MetS Components
3.2. Correlation between AntiOxi Index and Plasma Antioxidants and MetS Severity
3.3. Association between Plasma Bioactive Compounds and MetS Severity, Individual MetS Components and CRP
3.3.1. Plasma Carotenoids
3.3.2. Polyphenols
4. Discussion
Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guo, Q.; Li, F.; Duan, Y.; Wen, C.; Wang, W.; Zhang, L.; Huang, R.; Yin, Y. Oxidative stress, nutritional antioxidants and beyond. Sci. China Life Sci. 2020, 63, 866–874. [Google Scholar] [CrossRef] [PubMed]
- Di Lorenzo, C.; Colombo, F.; Biella, S.; Stockley, C.; Restani, P. Polyphenols and Human Health: The Role of Bioavailability. Nutrients 2021, 13, 273. [Google Scholar] [CrossRef] [PubMed]
- Bohn, T.; Bonet, M.; Borel, P.; Keijer, J.; Landrier, J.; Milisav, I.; Ribot, J.; Riso, P.; Winklhofer-Roob, B.; Sharoni, Y. Mechanistic aspects of carotenoid health benefits—Where are we now? Nutr. Res. Rev. 2021, 34, 276–302. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.V.; Rao, L.G. Carotenoids and human health. Pharmacol. Res. 2007, 55, 207–216. [Google Scholar] [CrossRef]
- Eggersdorfer, M.; Wyss, A. Carotenoids in human nutrition and health. Arch. Biochem. Biophys. 2018, 15, 18–26. [Google Scholar] [CrossRef]
- Beydoun, M.A.; Chen, X.; Jha, K.; Beydoun, H.A.; Zonderman, A.B.; Canas, J.A. Carotenoids, vitamin A, and their association with the metabolic syndrome: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 32–45. [Google Scholar] [CrossRef]
- Harari, A.; Coster, A.C.F.; Jenkins, A.; Xu, A.; Greenfield, J.R.; Harats, D.; Shaish, A.; Samocha-Bonet, D. Obesity and Insulin Resistance Are Inversely Associated with Serum and Adipose Tissue Carotenoid Concentrations in Adults. J. Nutr. 2020, 150, 38–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Sesso, H.D. Flavonoid consumption and cardiometabolic health: Potential benefits due to foods, supplements, or biomarkers? Am. J. Clin. Nutr. 2021, 114, 9–11. [Google Scholar] [CrossRef]
- Aloo, S.-O.; Ofosu, F.K.; Kim, N.-H.; Kilonzi, S.M.; Oh, D.-H. Insights on Dietary Polyphenols as Agents against Metabolic Disorders: Obesity as a Target Disease. Antioxidants 2023, 12, 416. [Google Scholar] [CrossRef]
- Shen, N.; Wang, T.; Gan, Q.; Liu, S.; Wang, L.; Jin, B. Plant flavonoids: Classification, distribution, biosynthesis, and antioxidant activity. Food Chem. 2022, 383, 132531. [Google Scholar] [CrossRef]
- Rana, A.; Samtiya, M.; Dhewa, T.; Mishra, V.; Aluko, R.E. Health benefits of polyphenols: A concise review. J. Food Biochem. 2022, 46, e14264. [Google Scholar] [CrossRef] [PubMed]
- Rani, V.; Deep, G.; Singh, R.K.; Palle, K.; Yadav, U.C. Oxidative stress and metabolic disorders: Pathogenesis and therapeutic strategies. Life Sci. 2016, 148, 183–193. [Google Scholar] [CrossRef]
- Arfaoui, L. Dietary Plant Polyphenols: Effects of Food Processing on Their Content and Bioavailability. Molecules 2021, 26, 2959. [Google Scholar] [CrossRef] [PubMed]
- Lee, C. Effects of dietary vitamins on obesity-related metabolic parameters. J. Nutr. Sci. 2023, 12, E47. [Google Scholar] [CrossRef]
- Bohn, T. Carotenoids and Markers of Oxidative Stress in Human Observational Studies and Intervention Trials: Implications for Chronic Diseases. Antioxidants 2019, 8, 179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sies, H. Oxidative Stress: Concept and Some Practical Aspects. Antioxidants 2020, 9, 852. [Google Scholar] [CrossRef] [PubMed]
- Marseglia, L.; Manti, S.; D’Angelo, G.; Nicotera, A.; Parisi, E.; Di Rosa, G.; Gitto, E.; Arrigo, T. Oxidative Stress in Obesity: A Critical Component in Human Diseases. Int. J. Mol. Sci. 2015, 16, 378–400. [Google Scholar] [CrossRef] [Green Version]
- Masenga, S.K.; Kabwe, L.S.; Chakulya, M.; Kirabo, A. Mechanisms of Oxidative Stress in Metabolic Syndrome. Int. J. Mol. Sci. 2023, 24, 7898. [Google Scholar] [CrossRef]
- Cojocaru, K.-A.; Luchian, I.; Goriuc, A.; Antoci, L.-M.; Ciobanu, C.-G.; Popescu, R.; Vlad, C.-E.; Blaj, M.; Foia, L.G. Mitochondrial Dysfunction, Oxidative Stress, and Therapeutic Strategies in Diabetes, Obesity, and Cardiovascular Disease. Antioxidants 2023, 12, 658. [Google Scholar] [CrossRef]
- Xu, H.; Li, X.; Adams, H.; Kubena, K.; Guo, S. Etiology of Metabolic Syndrome and Dietary Intervention. Int. J. Mol. Sci. 2019, 20, 128. [Google Scholar] [CrossRef] [Green Version]
- Ambroselli, D.; Masciulli, F.; Romano, E.; Catanzaro, G.; Besharat, Z.M.; Massari, M.C.; Ferretti, E.; Migliaccio, S.; Izzo, L.; Ritieni, A.; et al. New Advances in Metabolic Syndrome, from Prevention to Treatment: The Role of Diet and Food. Nutrients 2023, 15, 640. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grosso, G.; Stepaniak, U.; Micek, A.; Stefler, D.; Bobak, M.; Pająk, A. Dietary polyphenols are inversely associated with metabolic syndrome in Polish adults of the HAPIEE study. Eur. J. Nutr. 2017, 56, 1409–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Martínez, P.; Mikhailidis, D.P.; Athyros, V.G.; Bullo, M.; Couture, P.; Covas, M.I.; de Koning, L.; Delgado-Lista, J.; Díaz-López, A.; Drevon, C.A.; et al. Lifestyle recommendations for the prevention and management of metabolic syndrome: An international panel recommendation. Nutr. Rev. 2017, 75, 307–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Białkowska, A.; Górnicka, M.; Zielinska-Pukos, M.A.; Hamulka, J. Associations between Dietary Patterns, Anthropometric and Cardiometabolic Indices and the Number of MetS Components in Polish Adults with Metabolic Disorders. Nutrients 2023, 15, 2237. [Google Scholar] [CrossRef]
- Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data (in Polish: KomPAN Kwestionariusz do Badania Poglądów i Zwyczajów Żywieniowych oraz Procedura Opracowania Danych (KomPAN®). Committee of Human Nutrition Science. Polish Academy of Science. Warsaw. 2014. Available online: http://www.knozc.pan.pl/ (accessed on 23 January 2017).
- Kowalkowska, J.; Wadolowska, L.; Czarnocinska, J.; Czlapka-Matyasik, M.; Galinski, G.; Jezewska-Zychowicz, M.; Bronkowska, M.; Dlugosz, A.; Loboda, D.; Wyka, J. Reproducibility of a Questionnaire for Dietary Habits, Lifestyle and Nutrition Knowledge Assessment (KomPAN) in Polish Adolescents and Adults. Nutrients 2018, 10, 1845. [Google Scholar] [CrossRef] [Green Version]
- National Institute for Health and Care Excellence (NICE) Hypertension in Adults: Diagnosis and Management. Available online: https://www.nice.org.uk/guidance/ng136 (accessed on 19 March 2023).
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Myers, G.L.; Rifai, N.; Tracy, R.P.; Roberts, W.L.; Alexander, R.W.; Biasucci, L.M.; Catravas, J.D.; Cole, T.G.; Cooper, G.R.; Khan, B.V.; et al. CDC/AHA Workshop on Markers of Inflammation and Cardiovascular Disease: Application to Clinical and Public Health Practice: Report from the laboratory science discussion group. Circulation 2004, 110, e545–e549. [Google Scholar] [CrossRef] [Green Version]
- Wu, K.; Schwartz, S.J.; Platz, E.A.; Clinton, S.K.; Erdman, J.W.J.r.; Ferruzzi, M.G.; Willett, W.C.; Giovannucci, E.L. Variations in plasma lycopene and specific isomers over time in a cohort of U.S. men. J. Nutr. 2003, 133, 1930–1936. [Google Scholar] [CrossRef] [Green Version]
- Su, Q.; Rowley, K.G.; Balazs, N.D. Carotenoids: Separation methods applicable to biological samples. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2002, 781, 393–418. [Google Scholar] [CrossRef]
- Sholola, M.J.; Cooperstone, J.L. Carotenoid extraction and analysis from blood plasma/serum. Methods Enzymol. 2022, 670, 423–457. [Google Scholar] [CrossRef] [PubMed]
- Radtke, J.; Linseisen, J.; Wolfram, G. Fasting plasma concentrations of selected flavonoids as markers of their ordinary dietary intake. Eur. J. Nutr. 2002, 41, 203–209. [Google Scholar] [CrossRef] [PubMed]
- DeBoer, M.D.; Gurka, M.J. Clinical utility of metabolic syndrome severity scores: Considerations for practitioners. Diabetes Metab. Syndr. Obes. 2017, 10, 65–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toh, D.W.K.; Loh, W.W.; Sutanto, C.N.; Yao, Y.; Kim, J.E. Skin Carotenoid Status and Plasma Carotenoids: Biomarkers of Dietary Carotenoids, Fruits and Vegetables for Middle-Aged and Older Singaporean Adults. Br. J. Nutr. 2021, 126, 1398–1407. [Google Scholar] [CrossRef] [PubMed]
- Nagao, A.; Kotake-Nara, E.; Hase, M. Effects of Fats and Oils on the Bioaccessibility of Carotenoids and Vitamin E in Vegetables. Biosci. Biotechnol. Biochem. 2013, 77, 1055–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molteni, C.; la Motta, C.; Valoppi, F. Improving the Bioaccessibility and Bioavailability of Carotenoids by Means of Nanostructured Delivery Systems: A Comprehensive Review. Antioxidants 2022, 11, 1931. [Google Scholar] [CrossRef]
- Böhm, V.; Lietz, G.; Olmedilla-Alonso, B.; Phelan, D.; Reboul, E.; Bánati, D.; Borel, P.; Corte-Real, J.; de Lera, A.R.; Desmarchelier, C.; et al. From carotenoid intake to carotenoid blood and tissue concentrations—Implications for dietary intake recommendations. Nutr. Rev. 2021, 79, 544–573. [Google Scholar] [CrossRef]
- Moran, N.E.; Mohn, E.S.; Hason, N.; Erdman, J.W., Jr.; Johnson, E.J. Intrinsic and Extrinsic Factors Impacting Absorption, Metabolism, and Health Effects of Dietary Carotenoids. Adv. Nutr. 2018, 9, 465–492. [Google Scholar] [CrossRef] [Green Version]
- Marhuenda-Muñoz, M.; Rinaldi de Alvarenga, J.F.; Hernáez, Á.; Tresserra-Rimbau, A.; Martínez-González, M.Á.; Salas-Salvadó, J.; Corella, D.; Malcampo, M.; Martínez, J.A.; Alonso-Gómez, Á.M.; et al. High Fruit and Vegetable Consumption and Moderate Fat Intake Are Associated with Higher Carotenoid Concentration in Human Plasma. Antioxidants 2021, 10, 473. [Google Scholar] [CrossRef]
- Hamułka, J.; Górnicka, M.; Sulich, A.; Frąckiewicz, J. Weight loss program is associated with decrease α-tocopherol status in obese adults. Clin. Nutr. 2019, 38, 1861–1870. [Google Scholar] [CrossRef]
- Umbreen, H.; Javid, M.; Riaz, M.; Mehar-un-Nisa. Metabolism of Carotenoids. In Carotenoids: Structure and Function in the Human Body; Zia-Ul-Haq, M., Dewanjee, S., Riaz, M., Eds.; Springer: Cham, Switzerland, 2021. [Google Scholar] [CrossRef]
- Jiang, Y.W.; Sun, Z.H.; Tong, W.W.; Yang, K.; Guo, K.Q.; Liu, G.; Pan, A. Dietary Intake and Circulating Concentrations of Carotenoids and Risk of Type 2 Diabetes: A Dose-Response Meta-Analysis of Prospective Observational Studies. Adv. Nutr. 2021, 12, 1723–1733. [Google Scholar] [CrossRef] [PubMed]
- McKay, G.J.; Lyner, N.; Linden, G.J.; Kee, F.; Moitry, M.; Biasch, K.; Amouyel, P.; Dallongeville, J.; Bongard, V.; Ferrières, J.; et al. Association of low plasma antioxidant levels with all-cause mortality and coronary events in healthy middle-aged men from France and Northern Ireland in the PRIME study. Eur. J. Nutr. 2021, 60, 2631–2641. [Google Scholar] [CrossRef] [PubMed]
- Harms, L.M.; Scalbert, A.; Zamora-Ros, R.; Rinaldi, S.; Jenab, M.; Murphy, N.; Achaintre, D.; Tjønneland, A.; Olsen, A.; Overvad, K.; et al. Plasma polyphenols associated with lower high-sensitivity C-reactive protein concentrations: A cross-sectional study within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Br. J. Nutr. 2020, 123, 198–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, K.; Liang, X.C.; Zhong, Y.L.; He, W.Y.; Wang, Z. 5-Caffeoylquinic Acid Decreases Diet-Induced Obesity in Rats by Modulating PPARα and LXRα Transcription. J. Sci. Food Agric. 2015, 95, 1903–1910. [Google Scholar] [CrossRef]
- Abdel-Moneim, A.; Abd El-Twab, S.M.; Yousef, A.I.; Ashour, M.B.; Reheim, E.S.A.; Hamed, M.A.A. New insights into the in vitro, in situ and in vivo antihyperglycemic mechanisms of gallic acid and p-coumaric acid. Arch. Physiol. Biochem. 2022, 128, 1188–1194. [Google Scholar] [CrossRef]
- Lu, H.; Tian, Z.; Cui, Y.; Liu, Z.; Ma, X. Chlorogenic acid: A comprehensive review of the dietary sources, processing effects, bioavailability, beneficial properties, mechanisms of action, and future directions. Compr. Rev. Food Sci. Food Saf. 2020, 19, 3130–3158. [Google Scholar] [CrossRef]
- Mubarak, A.; Bondonno, C.P.; Liu, A.H.; Considine, M.J.; Rich, L.; Mas, E.; Croft, K.D.; Hodgson, J.M. Acute effects of chlorogenic acid on nitric oxide status, endothelial function, and blood pressure in healthy volunteers: A randomized trial. J. Agric. Food Chem. 2012, 60, 9130–9136. [Google Scholar] [CrossRef]
- Noce, A.; Di Lauro, M.; Di Daniele, F.; Pietroboni Zaitseva, A.; Marrone, G.; Borboni, P.; Di Daniele, N. Natural Bioactive Compounds Useful in Clinical Management of Metabolic Syndrome. Nutrients 2021, 13, 630. [Google Scholar] [CrossRef]
- Schoeneck, M.; Iggman, D. The effects of foods on LDL cholesterol levels: A systematic review of the accumulated evidence from systematic reviews and meta-analyses of randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1325–1338. [Google Scholar] [CrossRef]
- Dabeek, W.M.; Marra, M.V. Dietary Quercetin and Kaempferol: Bioavailability and Potential Cardiovascular-Related Bioactivity in Humans. Nutrients 2019, 25, 2288. [Google Scholar] [CrossRef] [Green Version]
- Millar, C.L.; Duclos, Q.; Blesso, C.N. Effects of Dietary Flavonoids on Reverse Cholesterol Transport, HDL Metabolism, and HDL Function. Adv. Nutr. 2017, 15, 226–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, M.; Konigsberg, W.H.; Hao, C.; Pan, Y.; Sun, Y.; Wang, X. Bioactivity and mechanisms of flavonoids in decreasing insulin resistance. J. Enzym. Inhib. Med. Chem. 2023, 38, 1. [Google Scholar] [CrossRef]
- Koudoufio, M.; Desjardins, Y.; Feldman, F.; Spahis, S.; Delvin, E.; Levy, E. Insight into Polyphenol and Gut Microbiota Crosstalk: Are Their Metabolites the Key to Understand Protective Effects against Metabolic Disorders? Antioxidants 2020, 9, 982. [Google Scholar] [CrossRef] [PubMed]
- Neri-Numa, I.A.; Cazarin, C.B.B.; Ruiz, A.L.T.G.; Paulino, B.N.; Molina, G.; Pastore, G.M. Targeting flavonoids on modulation of metabolic syndrome. J. Funct. Foods 2020, 73, 10413. [Google Scholar] [CrossRef]
- Rocha, H.R.; Coelho, M.C.; Gomes, A.M.; Pintado, M.E. Carotenoids Diet: Digestion, Gut Microbiota Modulation, and Inflammatory Diseases. Nutrients 2023, 15, 2265. [Google Scholar] [CrossRef]
- Gasmi, A.; Mujawdiya, P.K.; Noor, S.; Lysiuk, R.; Darmohray, R.; Piscopo, S.; Lenchyk, L.; Antonyak, H.; Dehtiarova, K.; Shanaida, M.; et al. Polyphenols in Metabolic Diseases. Molecules 2022, 27, 6280. [Google Scholar] [CrossRef]
- Tresserra-Rimbau, A.; Castro-Barquero, S.; Becerra-Tomás, N.; Babio, N.; Martínez-González, M.Á.; Corella, D.; Fitó, M.; Romaguera, D.; Vioque, J.; Alonso-Gomez, A.M.; et al. Adopting a High-Polyphenolic Diet Is Associated with an Improved Glucose Profile: Prospective Analysis within the PREDIMED-Plus Trial. Antioxidants 2022, 11, 316. [Google Scholar] [CrossRef]
- Thomas, M.S.; Huang, L.; Garcia, C.; Sakaki, J.R.; Blesso, C.N.; Chun, O.K.; Fernandez, M.L. The Effects of Eggs in a Plant-Based Diet on Oxidative Stress and Inflammation in Metabolic Syndrome. Nutrients 2022, 14, 2548. [Google Scholar] [CrossRef]
- Tsitsimpikou, C.; Tsarouhas, K.; Kioukia-Fougia, N.; Skondra, C.; Fragkiadaki, P.; Papalexis, P.; Stamatopoulos, P.; Kaplanis, I.; Hayes, A.W.; Tsatsakis, A.; et al. Dietary supplementation with tomato-juice in patients with metabolic syndrome: A suggestion to alleviate detrimental clinical factors. Food Chem. Toxicol. 2014, 74, 9–13. [Google Scholar] [CrossRef]
- Habanova, M.; Holovicova, M.; Scepankova, H.; Lorkova, M.; Gazo, J.; Gazarova, M.; Pinto, C.A.; Saraiva, J.A.; Estevinho, L.M. Modulation of Lipid Profile and Lipoprotein Subfractions in Overweight/Obese Women at Risk of Cardiovascular Diseases through the Consumption of Apple/Berry Juice. Antioxidants 2022, 11, 2239. [Google Scholar] [CrossRef]
- Crowe-White, K.; Parrott, J.S.; Stote, K.S.; Gutschall, M.; Benson-Davies, S.; Droke, E.; O’Neil, C.E.; Wolfram, T.; Ziegler, P. Metabolic impact of 100% fruit juice consumption on antioxidant/oxidant status and lipid profiles of adults: An Evidence-Based review. Crit. Rev. Food Sci. Nutr. 2017, 57, 152–162. [Google Scholar] [CrossRef]
- Davis, D.W.; Navalta, J.W.; McGinnis, G.R.; Serafica, R.; Izuora, K.; Basu, A. Effects of Acute Dietary Polyphenols and Post-Meal Physical Activity on Postprandial Metabolism in Adults with Features of the Metabolic Syndrome. Nutrients 2020, 12, 1120. [Google Scholar] [CrossRef] [Green Version]
- Feldman, F.; Koudoufio, M.; Desjardins, Y.; Spahis, S.; Delvin, E.; Levy, E. Efficacy of Polyphenols in the Management of Dyslipidemia: A Focus on Clinical Studies. Nutrients 2021, 13, 672. [Google Scholar] [CrossRef]
- Javandoost, A.; Afshari, A.; Nikbakht-Jam, I.; Khademi, M.; Eslami, S.; Nosrati, M.; Foroutan-Tanha, M.; Sahebkar, A.; Tavalaie, S.; Ghayour-Mobarhan, M.; et al. Effect of crocin, a carotenoid from saffron, on plasma cholesteryl ester transfer protein and lipid profile in subjects with metabolic syndrome: A double blind randomized clinical trial. ARYA Atheroscler. 2017, 13, 245–252. [Google Scholar]
- Wang, Y.; Chung, S.J.; McCullough, M.L.; Song, W.O.; Fernandez, M.L.; Koo, S.I.; Chun, O.K. Dietary carotenoids are associated with cardiovascular disease risk biomarkers mediated by serum carotenoid concentrations. J. Nutr. 2014, 144, 1067–1074. [Google Scholar] [CrossRef] [Green Version]
- Yu, H.; Wen, Q.; Lv, J.; Sun, D.; Ma, Y.; Man, S.; Yin, J.; Tong, M.; Wang, B.; Yu, C.; et al. Association between Dietary Patterns Reflecting C-Reactive Protein and Metabolic Syndrome in the Chinese Population. Nutrients 2022, 14, 2566. [Google Scholar] [CrossRef] [PubMed]
- Chiva-Blanch, G.; Badimon, L. Effects of Polyphenol Intake on Metabolic Syndrome: Current Evidences from Human Trials. Oxidative Med. Cell. Longev. 2017, 2017, 5812401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willcox, D.C.; Scapagnini, G.; Willcox, B.J. Healthy aging diets other than the Mediterranean: A focus on the Okinawan diet. Mech. Ageing Dev. 2014, 136–137, 148–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Singh, R.B.; Fedacko, J.; Fatima, G.; Magomedova, A.; Watanabe, S.; Elkilany, G. Why and How the Indo-Mediterranean Diet May Be Superior to Other Diets: The Role of Antioxidants in the Diet. Nutrients 2022, 14, 898. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total Group (n = 275) |
|---|---|
| Sex (%): | |
| men | 42.5 (117) |
| women | 57.5 (158) |
| Age (years): | 53.9 ± 12.5 |
| Education (%): | |
| primary and vocational | 23.6 (65) |
| secondary | 43.4 (119) |
| university | 33.1 (91) |
| Physical activity (%): | |
| low | 74.9 (206) |
| moderate | 22.2 (61) |
| high | 2.9 (8) |
| Smoking status (%): | |
| current smokers | 25.1 (69) |
| former smokers | 32.7 (90) |
| never smoked | 42.2 (116) |
| AntiOxi Index (%) | 42.9 ± 13.3 |
| Anthropometrics | |
| BMI (kg/m2): | 30.8 ± 7.0 |
| men | 30.7 ± 5.8 |
| women | 30.8 ± 7.8 |
| WC (cm): | |
| men | 110.6 ± 15.7 |
| women | 100.1 ± 16.9 |
| WHtR: | 0.6 ± 0.1 |
| Fat mass (%): | |
| men | 27.1 ± 8.1 |
| women | 38.1 ± 9.1 |
| Biochemical markers and blood pressure | |
| Blood pressure (mmHg): | |
| systolic | 135.7 ± 17.9 |
| diastolic | 81.1 ± 12.0 |
| Cholesterol (mmol/L): | 5.0 ± 0.9 |
| Triglicerides (mmol/L): | 2.0 ± 0.7 |
| HDL cholesterol (mmol/L): | |
| men | 1.0 ± 0.3 |
| women | 1.2 ± 0.3 |
| LDL cholesterol (mmol/L): | 2.7 ± 0.8 |
| Fasting glucose (mmol/L): | 7.2 ± 3.3 |
| CRP (mg/L) | |
| men | 3.3 ± 5.3 |
| women | 2.3 ± 4.5 |
| Number of MetS-components: | |
| 3 | 54.2 (149) |
| 4 | 25.5 (70) |
| 5 | 20.4 (56) |
| MetS severity: | |
| men | 0.5 ± 1.2 |
| women | 0.8 ± 1.2 |
| Plasma Carotenoids (µmol/L) | Total Group (n = 275) | MetS Components | p-Value * | ||
|---|---|---|---|---|---|
| 3 (n = 149) | 4 (n = 70) | 5 (n = 56) | |||
| Mean (95% CI) Min–Max | |||||
| Lutein | 0.50 (0.46–0.54) 0.03–1.51 | 0.55 (0.49–0.60) a 0.07–1.51 | 0.51 (0.43–0.59) a 0.03–1.38 | 0.34 (0.28–0.40) b 0.06–0.89 | ≤0.001 |
| Zeaxanthin | 0.13 (0.12–0.14) 0.01–0.34 | 0.14 (0.13–0.16) a 0.01–0.34 | 0.13 (0.11–0.15) a 0.02–0.33 | 0.11 (0.09–0.13) b 0.02–0.31 | 0.008 |
| L + Z | 0.63 (0.59–0.67) 0.05–1.75 | 0.69 (0.63–0.75) a 0.14–1.75 | 0.64 (0.29–0.40) a 0.05–1.44 | 0.45 (0.39–0.51) b 0.08–0.96 | ≤0.001 |
| Lycopene | 0.30 (0.28–0.32) 0.02–0.75 | 0.29 (0.27–0.32) 0.02–0.72 | 0.30 (0.26–0.35) 0.03–0.75 | 0.29 (0.24–0.34) 0.08–0.71 | 0.844 |
| β-carotene | 0.30 (0.28–0.32) 0.05–0.74 | 0.29 (0.25–0.32) 0.05–0.74 | 0.29 (0.25–0.34) 0.08–0.72 | 0.34 (0.29–0.39) 0.08–0.73 | 0.143 |
| Total carotenoids | 1.22 (1.17–1.27) 0.38–2.58 | 1.27 (1.20–1.34) a 0.40–2.36 | 1.23 (1.12–1.35) a 0.38–2.58 | 1.08 (0.99–1.18) b 0.48–1.89 | 0.039 |
| Plasma Polyphenols (nmol/L) | Total Group (n = 275) | MetS Components | p-Value * | ||
|---|---|---|---|---|---|
| 3 (n = 149) | 4 (n = 70) | 5 (n = 56) | |||
| Mean (95% CI) Min–Max | |||||
| Gallic acid | 16.3 (15.3–17.3) 0.00–35.4 | 15.7 (14.4–17.0) 0.00–35.2 | 16.5 (14.4–18.6) 0.00–35.4 | 17.6 (15.3–19.8) 7.70–34.7 | 0.439 |
| Chlorogenic acid | 8.20 (7.70–8.60) 0.00–17.6 | 8.20 (7.60–8.80) 0.00–17.6 | 08.50 (7.50–9.60) 0.00–17.3 | 7.70 (6.70–8.60) 0.00–16.4 | 0.607 |
| Caffeic acid | 11.8 (11.2–12.4) 0.00–23.4 | 11.3 (10.5–12.1) 0.00–23.4 | 12.9 (11.5–14.2) 0.00–23.3 | 11.9 (10.5–13.0) 0.00–22.6 | 0.084 |
| p-Coumaric acid | 19.4 (17.6–21.2) 0.00–56.9 | 19.1 (16.7–21.6) 0.00–56.4 | 21.1 (17.1–25.1) 0.00–56.9 | 17.9 (14.3–21.5) 0.00–53.0 | 0.688 |
| Ferulic acid | 5.81 (5.20–6.32) 0.00–18.1 | 6.11 (5.41–6.93) 0.00–18.1 | 5.11 (4.10–6.22) 0.00–16.7 | 5.54 (4.22–6.80) 0.00–16.4 | 0.240 |
| Phenolic acids | 61.4 (58.9–63.9) 90.2–120.6 | 60.4 (57.0–63.9) 89.8–110.2 | 64.1 (58.5–69.7) 22.0–120.6 | 60.6 (55.5–65.8) 31.7–115.5 | 0.436 |
| Kaempferol | 3.5 (3.2–3.8) 0.00–0.93 | 3.7 (3.3–4.0) 0.00–9.3 | 3.3 (2.8–3.9) 0.00–8.5 | 3.3 (2.7–3.9) 0.00–8.2 | 0.389 |
| Quercetin | 14.4 (12.7–16.1) 0.00–48.6 | 14.9 (12.7–17.3) 0.00–45.7 | 12.2 (9.2–15.4) 0.00–44.6 | 15.6 (11.4–19.9) 0.00–48.6 | 0.338 |
| Flavonol derivatives | 17.9 (16.3–19.5) 0.00–57.7 | 18.6 (16.4–20.8) 0.00–54.3 | 15.6 (12.5–18.7) 0.00–52.4 | 18.9 (14.8–23.0) 0.00–57.0 | 0.323 |
| Total polyphenols | 79.3 (76.1–82.5) 12.7–162.5 | 79.0 (74.4–83.6) 12.7–162.5 | 79.7 (73.6–85.8) 22.1–137.9 | 79.5 (72.8–86.3) 33.8–148.6 | 0.732 |
| Variables | AntiOxi Index | p-Value * | |||
|---|---|---|---|---|---|
| Q1 (n = 68) | Q2 (n = 69) | Q3 (n = 70) | Q4 (n = 68) | ||
| AntiOxi Index [%] | 25.9 ± 6.5 27.0 | 38.9 ± 2.7 39.7 | 47.2 ± 2.6 46.8 | 59.1 ± 7.6 56.6 | 0.0001 |
| Plasma lycopene (µmol/L) | 0.28 ± 0.18 0.22 a | 0.27 ± 0.16 0.23 a | 0.28 ± 0.15 0.28 b | 0.35 ± 0.17 0.35 c | 0.0065 |
| Total plasma carotenoids (µmol/L) | 1.21 ± 0.42 1.17 | 1.13 ± 0.47 1.07 | 1.25 ± 0.48 1.21 | 1.30 ± 0.38 1.25 | 0.1008 |
| Total plasma polyphenols (nmol/L) | 79.7 ± 28.0 77.5 | 78.7 ± 24.6 74.9 | 77.5 ± 27.5 75.9 | 81.3 ± 27.9 83.6 | 0.7091 |
| MetS severity | 0.51 ± 0.98 | 0.70 ± 1.22 | 0.61 ± 1.37 | 0.84 ± 1.33 | 0.4285 |
| Plasma Carotenoids (µmol/L) | Multivariate Models β (95% CI) R2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MetS Severity | Fasting Glucose (mmol/L) | HDL (mmol/L) | LDL (mmol/L) | TG (mmol/L) | Cholesterol (mmol/L) | WC (cm) | SBP (mmHg) | DBP (mmHg) | CRP (mg/L) | |
| Lutein | −0.105 (−0.225–0.015) R2 = 0.08 *** | −0.126 (−0.249–−0.003) * R2 = 0.04 * | 0.088 (−0.028–0.204) R2 = 0.14 *** | 0.003 (−0.121–0.127) R2 = 0.02 | −0.011 (−0.134–0.113) R2 = 0.03 | −0.028 (−0.152–0.097) R2 = 0.01 | −0.079 (−0.152–−0.007) R2 = 0.66 *** | −0.089 (−0.214–0.036) R2 = 0.01 | 0.061 (−0.226–0.014) R2 = 0.08 | −0.083 (−0.206–0.040) R2 = 0.04 * |
| Zeaxanthin | 0.002 (−0.119–0.123) R2 = 0.07 ** | −0.044 (−0.168–0.080) R2 = 0.02 | 0.157 (0.042–0.272) ** R2 = 0.16 *** | 0.081 (−0.043–0.205) R2 = 0.03 | 0.047 (−0.077–0.171) R2 = 0.03 | 0.133 (0.009–0.257) * R2 = 0.02 | −0.053 (−0.126–0.020) R2 = 0.66 *** | −0.068 (−0.193–0.057) R2 = 0.01 | −0.076 (−0.197–0.045) R2 = 0.07 *** | −0.153 (−0.276–0.031) * R2 = 0.05 ** |
| L + Z | −0.102 (−0.033–0.204) R2 = 0.08 *** | −0.134 (−0.258–−0.010) * R2 = 0.04 * | 0.125 (0.008–0.241) * R2 = 0.14 *** | 0.023 (−0.102–0.148) R2 = 0.02 | 0.001 (−0.124–0.126) R2 = 0.03 | 0.006 (−0.120–0.132) R2 = 0.01 | −0.091 (−0.164–−0.017) R2 = 0.67 *** | −0.104 (−0.230–0.022) R2 = 0.01 | −0.122 (−0.243–−0.001) R2 = 0.07 *** | −0.119 (−0.243–0.005) R2 = 0.03 |
| Lycopene | 0.086 (−0.033–0.204) R2 = 0.08 *** | −0.048 (−0.171–0.074) R2 = 0.03 | 0.031 (−0.068–0.158) R2 = 0.14 *** | 0.066 (−0.056–0.188) R2 = 0.03 | 0.166 (0.046–0.286) ** R2 = 0.06 ** | 0.150 (0.029–0.272) * R2 = 0.03 * | 0.000 (−0.073–0.072) R2 = 0.66 *** | −0.068 (−0.191–0.055) R2 = 0.01 | −0.042 (−0.161–0.078) R2 = 0.07 *** | 0.025 (0.096–0.147) * R2 = 0.03 |
| β-carotene | −0.115 (−0.234–0.003) R2 = 0.08 *** | −0.061 (−0.183–0.061) R2 = 0.02 | 0.046 (−0.068–0.161) R2 = 0.14 *** | 0.009 (−0.113–0.131) R2 = 0.02 | 0.069 (−0.052–0.191) R2 = 0.05 * | 0.016 (−0.107–0.140) R2 = 0.01 | −0.019 (−0.096–0.058) R2 = 0.66 *** | 0.031 (−0.092–0.155) R2 = 0.00 | −0.031 (−0.150–0.088) R2 = 0.07 *** | −0.025 (−0.147–0.096) R2 = 0.03 |
| Total | −0.056 (−0.176–0.064) R2 = 0.08 *** | −0.148 (−0.271–−0.025) * R2 = 0.04 * | 0.128 (0.012–0.243) * R2 = 0.15 *** | 0.047 (−0.077–0.171) R2 = 0.02 | 0.096 (−0.027–0.219) R2 = 0.04 * | 0.070 (−0.055–0.195) R2 = 0.01 | −0.070 (−0.143–0.003) R2 = 0.66 *** | −0.092 (−0.217–0.033) R2 = 0.01 | −0.123 (−0.243–−0.003) R2 = 0.08 *** | −0.092 (−0.215–0.031) R2 = 0.04 * |
| Plasma Polyphenols (nmol/L) | Multivariate Models β (95% CI) R2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MetS Severity | Fasting Glucose (mmol/L) | HDL (mmol/L) | LDL (mmol/L) | TG (mmol/L) | Cholesterol (mmol/L) | WC (cm) | SBP (mmHg) | DBP (mmHg) | CRP (mg/L) | |
| Chlorogenic acid | −0.034 (−0.151–0.083) R2 = 0.05 ** | −0.065 (−0.184–0.053) R2 = 0.02 | 0.017 (−0.094–0.128) R2 = 0.14 *** | 0.138 (0.020–0.256) * R2 = 0.03 * | 0.002 (−0.115–0.120) R2 = 0.04 ** | 0.125 (0.005–0.245) R2 = 0.01 | 0.068 (−0.003–0.138) R2 = 0.66 *** | 0.042 (−0.079–0.164) R2 = 0.00 | 0.093 (−0.024–0.210) R2 = 0.08 *** | −0.116 (−0.235–0.003) R2 = 0.04 * |
| p-Coumaric acid | 0.036 (−0.083–0.155) R2 = 0.05 ** | −0.140 (−0.260–−0.021) * R2 = 0.04 * | 0.016 (−0.096–0.129) R2 = 0.15 *** | −0.021 (−0.143–0.100) R2 = 0.01 | −0.056 (−0.175–0.063) R2 = 0.04 * | 0.027 (−0.096–0.149) R2 = 0.01 | 0.052 (−0.021–0.124) R2 = 0.66 *** | 0.055 (−0.069–0.179) R2 = 0.00 | 0.096 (−0.024–0.215) R2 = 0.08 *** | −0.022 (−0.144–0.101) R2 = 0.03 |
| Kaempferol | −0.042 (−0.159–0.075) R2 = 0.07 ** | −0.017 (−0.136–0.102) R2 = 0.02 | 0.100 (−0.010–0.210) R2 = 0.16 *** | 0.098 (−0.020–0.217) R2 = 0.02 | 0.063 (−0.054–0.181) R2 = 0.05 * | 0.127 (0.008–0.247) * R2 = 0.01 * | −0.008 (−0.081–0.064) R2 = 0.66 *** | −0.031 (−0.154–0.092) R2 = 0.00 | −0.011 (−0.130–0.108) R2 = 0.07 ** | −0.075 (−0.196–0.046) R2 = 0.04 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Białkowska, A.; Górnicka, M.; Zielinska-Pukos, M.A.; Hallmann, E.; Hamulka, J. Plasma Carotenoids and Polyphenols and Their Association with MetS: The Need for Nutritional Interventions. Antioxidants 2023, 12, 1336. https://doi.org/10.3390/antiox12071336
Białkowska A, Górnicka M, Zielinska-Pukos MA, Hallmann E, Hamulka J. Plasma Carotenoids and Polyphenols and Their Association with MetS: The Need for Nutritional Interventions. Antioxidants. 2023; 12(7):1336. https://doi.org/10.3390/antiox12071336
Chicago/Turabian StyleBiałkowska, Agnieszka, Magdalena Górnicka, Monika A. Zielinska-Pukos, Ewelina Hallmann, and Jadwiga Hamulka. 2023. "Plasma Carotenoids and Polyphenols and Their Association with MetS: The Need for Nutritional Interventions" Antioxidants 12, no. 7: 1336. https://doi.org/10.3390/antiox12071336