Melatonin as an Antitumor Agent against Liver Cancer: An Updated Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
- PubMed: (“melatonin” [All Fields]) AND (“liver cancer” [All Fields] OR “liver tumor” [All Fields] OR “hepatocarcinoma”[All Fields] OR “HCC”[All Fields] OR “hepatocellular carcinoma”[All Fields] OR “angiosarcoma”[All Fields] OR “cholangiocarcinoma”[All Fields] OR “hepatoblastoma”[All Fields]).
- Scopus: TITLE-ABS-KEY ((“melatonin”) AND (“liver cancer” OR “liver tumor” OR “hepatocarcinoma” OR “HCC” OR “hepatocellular carcinoma” OR “angiosarcoma” OR “cholangiocarcinoma” OR “hepatoblastoma”)).
- WOS: TS = ((“melatonin”) AND (“liver cancer” OR “liver tumor” OR “hepatocarcinoma” OR “HCC” OR “hepatocellular carcinoma” OR “angiosarcoma” OR “cholangiocarcinoma” OR “hepatoblastoma”)).
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Data Extraction
3. Results and Discussion
3.1. Study Selection and Characteristics
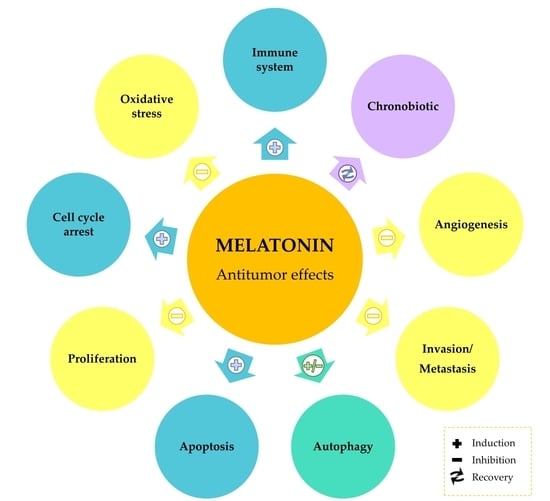
3.2. Melatonin as Antioxidant and Chronobiotic Agent in Liver Cancer
3.3. Cell Cycle Arrest by Melatonin in Liver Cancer
3.4. Modulation of Apoptosis by Melatonin in Liver Cancer
3.5. Modulation of Autophagy by Melatonin in Liver Cancer
3.6. Modulation of Angiogenesis and Invasion by Melatonin in Liver Cancer
3.7. Melatonin Immunomodulation in Liver Cancer
3.8. Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Sharma, R. Descriptive epidemiology of incidence and mortality of primary liver cancer in 185 countries: Evidence from GLOBOCAN 2018. Jpn. J. Clin. Oncol. 2020, 50, 1370–1379. [Google Scholar] [CrossRef]
- Marin, J.J.G.; Briz, O.; Herraez, E.; Lozano, E.; Asensio, M.; Di Giacomo, S.; Romero, M.R.; Osorio-Padilla, L.M.; Santos-Llamas, A.I.; Serrano, M.A.; et al. Molecular bases of the poor response of liver cancer to chemotherapy. Clin. Res. Hepatol. Gastroenterol. 2018, 42, 182–192. [Google Scholar] [CrossRef]
- Prieto-Domínguez, N.; Méndez-Blanco, C.; Carbajo-Pescador, S.; Fondevila, F.; García-Palomo, A.; González-Gallego, J.; Mauriz, J.L. Melatonin enhances sorafenib actions in human hepatocarcinoma cells by inhibiting mTORC1/p70S6K/HIF-1α and hypoxia-mediated mitophagy. Oncotarget 2017, 8, 91402–91414. [Google Scholar] [CrossRef]
- Wang, G.; Wang, Q.; Liang, N.; Xue, H.; Yang, T.; Chen, X.; Qiu, Z.; Zeng, C.; Sun, T.; Yuan, W.; et al. Oncogenic driver genes and tumor microenvironment determine the type of liver cancer. Cell Death Dis. 2020, 11, 313. [Google Scholar] [CrossRef]
- Mauriz, J.L.; Collado, P.S.; Veneroso, C.; Reiter, R.J.; González-Gallego, J. A review of the molecular aspects of melatonin’s anti-inflammatory actions: Recent insights and new perspectives. J. Pineal Res. 2013, 54, 1–14. [Google Scholar] [CrossRef]
- Sánchez-Hidalgo, M.; Guerrero, J.M.; Villegas, I.; Packham, G.; de la Lastra, C.A. Melatonin, a natural programmed cell death inducer in cancer. Curr. Med. Chem. 2012, 19, 3805–3821. [Google Scholar] [CrossRef]
- Reiter, R.J.; Rosales-Corral, S.A.; Tan, D.X.; Acuña-Castroviejo, D.; Qin, L.; Yang, S.F.; Xu, K. Melatonin, a full service anti-cancer agent: Inhibition of initiation, progression and metastasis. Int. J. Mol. Sci. 2017, 18, 843. [Google Scholar] [CrossRef]
- Li, Y.; Li, S.; Zhou, Y.; Meng, X.; Zhang, J.-J.; Xu, D.-P.; Li, H.-B. Melatonin for the prevention and treatment of cancer. Oncotarget 2017, 8, 39896–39921. [Google Scholar] [CrossRef] [Green Version]
- Martín-Renedo, J.; Mauriz, J.L.; Jorquera, F.; Ruiz-Andrés, O.; González, P.; González-Gallego, J. Melatonin induces cell cycle arrest and apoptosis in hepatocarcinoma HepG2 cell line. J. Pineal Res. 2008, 45, 532–540. [Google Scholar] [CrossRef]
- Carbajo-Pescador, S.; Martín-Renedo, J.; García-Palomo, A.; Tuñón, M.J.; Mauriz, J.L.; González-Gallego, J. Changes in the expression of melatonin receptors induced by melatonin treatment in hepatocarcinoma HepG2 cells. J. Pineal Res. 2009, 47, 330–338. [Google Scholar] [CrossRef]
- Carbajo-Pescador, S.; García-Palomo, A.; Martín-Renedo, J.; Piva, M.; González-Gallego, J.; Mauriz, J.L. Melatonin modulation of intracellular signaling pathways in hepatocarcinoma HepG2 cell line: Role of the MT1 receptor. J. Pineal Res. 2011, 51, 463–471. [Google Scholar] [CrossRef]
- Carbajo-Pescador, S.; Ordoñez, R.; Benet, M.; Jover, R.; García-Palomo, A.; Mauriz, J.L.; González-Gallego, J. Inhibition of VEGF expression through blockade of Hif1α and STAT3 signalling mediates the anti-angiogenic effect of melatonin in HepG2 liver cancer cells. Br. J. Cancer 2013, 109, 83–91. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, D.I.; González-Fernández, B.; Crespo, I.; San-Miguel, B.; Álvarez, M.; González-Gallego, J.; Tuñón, M.J. Melatonin modulates dysregulated circadian clocks in mice with diethylnitrosamine-induced hepatocellular carcinoma. J. Pineal Res. 2018, 65, e12506. [Google Scholar] [CrossRef]
- Ordoñez, R.; Carbajo-Pescador, S.; Prieto-Dominguez, N.; García-Palomo, A.; González-Gallego, J.; Mauriz, J.L. Inhibition of matrix metalloproteinase-9 and nuclear factor kappa B contribute to melatonin prevention of motility and invasiveness in HepG2 liver cancer cells. J. Pineal Res. 2014, 56, 20–30. [Google Scholar] [CrossRef]
- Ordoñez, R.; Fernández, A.; Prieto-Domínguez, N.; Martínez, L.; García-Ruiz, C.; Fernández-Checa, J.C.; Mauriz, J.L.; González-Gallego, J. Ceramide metabolism regulates autophagy and apoptotic cell death induced by melatonin in liver cancer cells. J. Pineal Res. 2015, 59, 178–189. [Google Scholar] [CrossRef]
- Moreira, A.J.; Ordoñez, R.; Cerski, C.T.; Picada, J.N.; García-Palomo, A.; Marroni, N.P.; Mauriz, J.L.; González-Gallego, J. Melatonin activates endoplasmic reticulum stress and apoptosis in rats with diethylnitrosamine-induced hepatocarcinogenesis. PLoS ONE 2015, 10, e0144517. [Google Scholar] [CrossRef]
- Prieto-Domínguez, N.; Ordóñez, R.; Fernández, A.; Méndez-Blanco, C.; Baulies, A.; Garcia-Ruiz, C.; Fernández-Checa, J.C.; Mauriz, J.L.; González-Gallego, J. Melatonin-induced increase in sensitivity of human hepatocellular carcinoma cells to sorafenib is associated with reactive oxygen species production and mitophagy. J. Pineal Res. 2016, 61, 396–407. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Dakshayani, K.B.; Subramanian, P.; Manivasagam, T.; Mohamed Essa, M.; Manoharan, S. Melatonin modulates the oxidant-antioxidant imbalance during N-nitrosodiethylamine induced hepatocarcinogenensis in rats. J. Pharm. Pharm. Sci. 2005, 8, 316–321. [Google Scholar]
- Dakshayani, K.B.; Subramanian, P.; Essa, M.M. Effect of melatonin on N-nitrosodiethylamine-induced hepatocarcinogenesis in rats with reference to biochemical circadian rhythms. Toxicol. Mech. Methods 2007, 17, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, P.; Mirunalini, S.; Dakshayani, K.B.; Pandi-Perumal, S.R.; Trakht, I.; Cardinali, D.P. Prevention by melatonin of hepatocarcinogenesis in rats injected with N-nitrosodiethylamine. J. Pineal Res. 2007, 43, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, P.; Dakshayani, K.B.; Pandi-Perumal, S.R.; Trakht, I.; Cardinali, D.P. 24-hour rhythms in oxidative stress during hepatocarcinogenesis in rats: Effect of melatonin or α-ketoglutarate. Redox Rep. 2008, 13, 78–86. [Google Scholar] [CrossRef]
- Ozdemir, F.; Deniz, O.; Kaynar, K.; Arslan, M.; Kavgaci, H.; Yildiz, B.; Aydin, F. The effects of melatonin on human hepatoma (Hep G2) cell line. Bratislava Med. J. 2009, 110, 276–279. [Google Scholar]
- Fan, L.-L.; Sun, G.-P.; Wei, W.; Wang, Z.-G.; Ge, L.; Fu, W.-Z.; Wang, H. Melatonin and Doxorubicin synergistically induce cell apoptosis in human hepatoma cell lines. World J. Gastroenterol. 2010, 16, 1473–1481. [Google Scholar] [CrossRef]
- Laothong, U.; Pinlaor, P.; Hiraku, Y.; Boonsiri, P.; Prakobwong, S.; Khoontawad, J.; Pinlaor, S. Protective effect of melatonin against Opisthorchis viverrini-induced oxidative and nitrosative DNA damage and liver injury in hamsters. J. Pineal Res. 2010, 49, 271–282. [Google Scholar] [CrossRef]
- Lin, Z.Y.; Chuang, W.L. Pharmacologic concentrations of melatonin have diverse influence on differential expressions of angiogenic chemokine genes in different hepatocellular carcinoma cell lines. Biomed. Pharmacother. 2010, 64, 659–662. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; DeMorrow, S.; Invernizzi, P.; Jing, Q.; Glaser, S.; Renzi, A.; Meng, F.; Venter, J.; Bernuzzi, F.; White, M.; et al. Melatonin exerts by an autocrine loop antiproliferative effects in cholangiocarcinoma; its synthesis is reduced favoring cholangiocarcinoma growth. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 301, 623–633. [Google Scholar] [CrossRef]
- Carbajo-Pescador, S.; Steinmetz, C.; Kashyap, A.; Lorenz, S.; Mauriz, J.L.; Heise, M.; Galle, P.R.; González-Gallego, J.; Strand, S. Melatonin induces transcriptional regulation of Bim by FoxO3a in HepG2 cells. Br. J. Cancer 2013, 108, 442–449. [Google Scholar] [CrossRef] [Green Version]
- Cid, M.A.; Úbeda, A.; Hernández-Bule, M.L.; Martínez, M.A.; Trillo, M.Á. Antagonistic effects of a 50 Hz magnetic field and melatonin in the proliferation and differentiation of hepatocarcinoma cells. Cell. Physiol. Biochem. 2012, 30, 1502–1516. [Google Scholar] [CrossRef]
- Liu, C.; Jia, Z.; Zhang, X.; Hou, J.; Wang, L.; Hao, S.; Ruan, X.; Yu, Z.; Zheng, Y. Involvement of melatonin in autophagy-mediated mouse hepatoma H22 cell survival. Int. Immunopharmacol. 2012, 12, 394–401. [Google Scholar] [CrossRef]
- Zha, L.; Fan, L.; Sun, G.; Wang, H.; Ma, T.; Zhong, F.; Wei, W. Melatonin sensitizes human hepatoma cells to endoplasmic reticulum stress-induced apoptosis. J. Pineal Res. 2012, 52, 322–331. [Google Scholar] [CrossRef]
- Fan, L.; Sun, G.; Ma, T.; Zhong, F.; Lei, Y.; Li, X.; Wei, W. Melatonin reverses tunicamycin-induced endoplasmic reticulum stress in human hepatocellular carcinoma cells and improves cytotoxic response to doxorubicin by increasing CHOP and decreasing Survivin. J. Pineal Res. 2013, 55, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.; Sun, G.; Ma, T.; Zhong, F.; Wei, W. Melatonin overcomes apoptosis resistance in human hepatocellular carcinoma by targeting Survivin and XIAP. J. Pineal Res. 2013, 55, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Laothong, U.; Pinlaor, P.; Boonsiri, P.; Pairojkul, C.; Priprem, A.; Johns, N.P.; Charoensuk, L.; Intuyod, K.; Pinlaor, S. Melatonin inhibits cholangiocarcinoma and reduces liver injury in Opisthorchis viverrini-infected and N-nitrosodimethylamine-treated hamsters. J. Pineal Res. 2013, 55, 257–266. [Google Scholar] [CrossRef]
- Tomov, B.; Popov, D.; Tomova, R.; Vladov, N.; Den Otter, W.; Krastev, Z. Therapeutic response of untreatable hepatocellular carcinoma after application of the immune modulators IL-2, BCG and melatonin. Anticancer Res. 2013, 33, 4531–4536. [Google Scholar]
- Bennukul, K.; Numkliang, S.; Leardkamolkarn, V. Melatonin attenuates cisplatin-induced HepG2 cell death via the regulation of mTOR and ERCC1 expressions. World J. Hepatol. 2014, 6, 230–242. [Google Scholar] [CrossRef]
- Verma, D.; Hashim, O.; Jayapalan, J.; Subramanian, P. Effect of melatonin on antioxidant status and circadian activity rhythm during hepatocarcinogenesis in mice. J. Cancer Res. Ther. 2014, 10, 1040–1044. [Google Scholar] [CrossRef]
- Laothong, U.; Hiraku, Y.; Oikawa, S.; Intuyod, K.; Murata, M.; Pinlaor, S. Melatonin induces apoptosis in cholangiocarcinoma cell lines by activating the reactive oxygen species-mediated mitochondrial pathway. Oncol. Rep. 2015, 33, 1443–1449. [Google Scholar] [CrossRef] [Green Version]
- Colombo, J.; Wolf Maciel, J.M.; Ferreira, L.C.; Da Silva, R.F.; Pires De Campos Zuccari, D.A. Effects of melatonin on HIF-1α and VEGF expression and on the invasive properties of hepatocarcinoma cells. Oncol. Lett. 2016, 12, 231–237. [Google Scholar] [CrossRef] [Green Version]
- Bu, L.-J.; Yu, H.-Q.; Fan, L.-L.; Li, X.-Q.; Wang, F.; Liu, J.-T.; Zhong, F.; Zhang, C.-J.; Wei, W.; Wang, H.; et al. Melatonin, a novel selective ATF-6 inhibitor, induces human hepatoma cell apoptosis through COX-2 downregulation. World J. Gastroenterol. 2017, 23, 986–998. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Liu, J.; Liu, Q.; Liu, Y.; Fan, L.; Wang, F.; Yu, H.; Li, Y.; Bu, L.; Li, X.; et al. Exosomes from melatonin treated hepatocellularcarcinoma cells alter the immunosupression status through STAT3 pathway in macrophages. Int. J. Biol. Sci. 2017, 13, 723–734. [Google Scholar] [CrossRef] [Green Version]
- Hao, J.; Li, Z.; Zhang, C.; Yu, W.; Tang, Z.; Li, Y.; Feng, X.; Gao, Y.; Liu, Q.; Huang, W.; et al. Targeting NF-κB/AP-2β signaling to enhance antitumor activity of cisplatin by melatonin in hepatocellular carcinoma cells. Am. J. Cancer Res. 2017, 7, 13–27. [Google Scholar]
- Lin, S.; Hoffmann, K.; Gao, C.; Petrulionis, M.; Herr, I.; Schemmer, P. Melatonin promotes sorafenib-induced apoptosis through synergistic activation of JNK/c-jun pathway in human hepatocellular carcinoma. J. Pineal Res. 2017, 62, e12398. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, J.; Cheng, L.; Fan, L.; Wang, F.; Yu, H.; Liu, Q.; Li, Y.; Bu, L.; Li, X.; et al. Melatonin increases the anti-tumor effects of sorafenib on human hepatoma cell lines via down-regulating autophagy. Int. J. Clin. Exp. Med. 2017, 10, 14109–14120. [Google Scholar]
- Long, F.; Dong, C.; Jiang, K.; Xu, Y.; Chi, X.; Sun, D.; Liang, R.; Gao, Z.; Shao, S.; Wang, L. Melatonin enhances the anti-tumor effect of sorafenib via AKT/p27-mediated cell cycle arrest in hepatocarcinoma cell lines. RSC Adv. 2017, 7, 21342–21351. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, D.I.; González-Fernández, B.; San-Miguel, B.; de Urbina, J.O.; Crespo, I.; González-Gallego, J.; Tuñón, M.J. Melatonin prevents deregulation of the sphingosine kinase/sphingosine 1-phosphate signaling pathway in a mouse model of diethylnitrosamine-induced hepatocellular carcinoma. J. Pineal Res. 2017, 62, e12369. [Google Scholar] [CrossRef]
- Wang, T.-H.; Wu, C.-H.; Yeh, C.-T.; Su, S.-C.; Hsia, S.-M.; Liang, K.-H.; Chen, C.-C.; Hsueh, C.; Chen, C.-Y. Melatonin suppresses hepatocellular carcinoma progression via lncRNA-CPS1-IT-mediated HIF-1α inactivation. Oncotarget 2017, 8, 82280–82293. [Google Scholar] [CrossRef]
- Wongsena, W.; Charoensuk, L.; Dangtakot, R.; Pinlaor, P.; Intuyod, K.; Pinlaor, S. Melatonin suppresses eosinophils and Th17 cells in hamsters treated with a combination of human liver fluke infection and a chemical carcinogen. Pharmacol. Rep. 2018, 70, 98–105. [Google Scholar] [CrossRef]
- Chen, C.-C.; Chen, C.-Y.; Wang, S.-H.; Yeh, C.-T.; Su, S.C.; Ueng, S.-H.; Chuang, W.-Y.; Hsueh, C.; Wang, T.-H. Melatonin sensitizes hepatocellular carcinoma cells to chemotherapy through long non-coding RNA RAD51-AS1-mediated suppression of DNA repair. Cancers (Basel) 2018, 10, 320. [Google Scholar] [CrossRef] [Green Version]
- Colombo, J.; Jardim-Perassi, B.V.; Ferreira, J.P.S.; Braga, C.Z.; Sonehara, N.M.; Júnior, R.P.; Moschetta, M.G.; Girol, A.P.; Zuccari, D.A.P.C. Melatonin differentially modulates NF-кB expression in breast and liver cancer cells. Anticancer Agents Med. Chem. 2018, 18, 1688–1694. [Google Scholar] [CrossRef]
- Dauchy, R.T.; Wren-Dail, M.A.; Dupepe, L.M.; Hill, S.M.; Xiang, S.; Anbalagan, M.; Belancio, V.P.; Dauchy, E.M.; Blask, D.E. Effect of daytime blue-enriched LED light on the nighttime circadian melatonin inhibition of hepatoma 7288CTC Warburg effect and progression. Comp. Med. 2018, 68, 269–279. [Google Scholar] [CrossRef]
- Wang, T.H.; Hsueh, C.; Chen, C.C.; Li, W.S.; Yeh, C.T.; Lian, J.H.; Chang, J.L.; Chen, C.Y. Melatonin inhibits the progression of hepatocellular carcinoma through microRNA let7i-3p mediated RAF1 reduction. Int. J. Mol. Sci. 2018, 19, 2687. [Google Scholar] [CrossRef] [Green Version]
- El-Magd, M.A.; Mohamed, Y.; El-Shetry, E.S.; Elsayed, S.A.; Abo Gazia, M.; Abdel-Aleem, G.A.; Shafik, N.M.; Abdo, W.S.; El-Desouki, N.I.; Basyony, M.A. Melatonin maximizes the therapeutic potential of non-preconditioned MSCs in a DEN-induced rat model of HCC. Biomed. Pharmacother. 2019, 114, 108732. [Google Scholar] [CrossRef]
- Mohamed, Y.; Basyony, M.A.; El-Desouki, N.I.; Abdo, W.S.; El-Magd, M.A. The potential therapeutic effect for melatonin and mesenchymal stem cells on hepatocellular carcinoma. BioMedicine 2019, 9, 23–29. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; He, Y.; Wu, X.; Zhao, G.; Zhang, K.; Yang, C.S.; Reiter, R.J.; Zhang, J. Melatonin and (−)-epigallocatechin-3-Gallate: Partners in fighting cancer. Cells 2019, 8, 745. [Google Scholar] [CrossRef] [Green Version]
- Zhou, B.; Lu, Q.; Liu, J.; Fan, L.; Wang, Y.; Wei, W.; Wang, H.; Sun, G. Melatonin increases the sensitivity of hepatocellular carcinoma to sorafenib through the PERK-ATf4-Beclin1 pathway. Int. J. Biol. Sci. 2019, 15, 1905–1920. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ao, L.; Li, L.; Sun, H.; Chen, H.; Li, Y.; Huang, H.; Wang, X.; Guo, Z.; Zhou, R. Transcriptomic analysis on the effects of melatonin in gastrointestinal carcinomas. BMC Gastroenterol. 2020, 20, 233. [Google Scholar] [CrossRef]
- Mi, L.; Kuang, H. Melatonin regulates cisplatin resistance and glucose metabolism through hippo signaling in hepatocellular carcinoma cells. Cancer Manag. Res. 2020, 12, 1863–1874. [Google Scholar] [CrossRef] [Green Version]
- Wang, R.; Liu, Y.; Mi, X.; Chen, Q.; Jiang, P.; Hou, J.; Lin, Y.; Li, S.; Ji, B.; Fang, Y. Sirt3 promotes hepatocellular carcinoma cells sensitivity to regorafenib through the acceleration of mitochondrial dysfunction. Arch. Biochem. Biophys. 2020, 689, 108415. [Google Scholar] [CrossRef] [PubMed]
- Moreira, A.J.; Rodrigues, G.; Bona, S.; Cerski, C.T.; Marroni, C.A.; Mauriz, J.L.; González-Gallego, J.; Marroni, N.P. Oxidative stress and cell damage in a model of precancerous lesions and advanced hepatocellular carcinoma in rats. Toxicol. Rep. 2015, 2, 333–340. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Palanca, P.; Fondevila, F.; Méndez-Blanco, C.; Tuñón, M.J.; González-Gallego, J.; Mauriz, J.L. Antitumor effects of quercetin in hepatocarcinoma in vitro and in vivo models: A systematic review. Nutrients 2019, 11, 2875. [Google Scholar] [CrossRef] [Green Version]
- Pourhanifeh, M.H.; Mehrzadi, S.; Kamali, M.; Hosseinzadeh, A. Melatonin and gastrointestinal cancers: Current evidence based on underlying signaling pathways. Eur. J. Pharmacol. 2020, 886, 173471. [Google Scholar] [CrossRef]
- González-Fernández, B.; Sánchez, D.I.; Crespo, I.; San-Miguel, B.; De Urbina, J.O.; González-Gallego, J.; Tuñón, M.J. Melatonin attenuates dysregulation of the circadian clock pathway in mice with CCl4-induced fibrosis and human hepatic stellate cells. Front. Pharmacol. 2018, 9, 556. [Google Scholar] [CrossRef] [PubMed]
- Crespo, I.; Fernández-Palanca, P.; San-Miguel, B.; Álvarez, M.; González-Gallego, J.; Tuñón, M.J. Melatonin modulates mitophagy, innate immunity and circadian clocks in a model of viral-induced fulminant hepatic failure. J. Cell. Mol. Med. 2020, 24, 7625–7636. [Google Scholar] [CrossRef] [PubMed]
- Filipski, E.; Subramanian, P.; Carrière, J.; Guettier, C.; Barbason, H.; Lévi, F. Circadian disruption accelerates liver carcinogenesis in mice. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2009, 680, 95–105. [Google Scholar] [CrossRef]
- Pfeffer, C.M.; Singh, A.T.K. Apoptosis: A target for anticancer therapy. Int. J. Mol. Sci. 2018, 19, 448. [Google Scholar] [CrossRef] [Green Version]
- Kim, B.-J.; Ryu, S.-W.; Song, B.-J. JNK- and p38 kinase-mediated phosphorylation of Bax leads to its activation and mitochondrial translocation and to apoptosis of human hepatoma HepG2 cells. J. Biol. Chem. 2006, 281, 21256–21265. [Google Scholar] [CrossRef] [Green Version]
- Méndez-Blanco, C.; Fondevila, F.; García-Palomo, A.; González-Gallego, J.; Mauriz, J.L. Sorafenib resistance in hepatocarcinoma: Role of hypoxia-inducible factors. Exp. Mol. Med. 2018, 50, 134. [Google Scholar] [CrossRef] [Green Version]
- Fondevila, F.; Méndez-Blanco, C.; Fernández-Palanca, P.; González-Gallego, J.; Mauriz, J.L. Anti-tumoral activity of single and combined regorafenib treatments in preclinical models of liver and gastrointestinal cancers. Exp. Mol. Med. 2019, 51, 109. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.; Yang, L.; Li, X.; Li, B.; Li, Y.; Zhang, X.; Ma, Y.; Peng, X.; Jin, H.; Li, H. New insights into autophagy in hepatocellular carcinoma: Mechanisms and therapeutic strategies. Am. J. Cancer Res. 2019, 9, 1329–1353. [Google Scholar] [PubMed]
- Morales, A.; Lee, H.; Goñi, F.M.; Kolesnick, R.; Fernandez-Checa, J.C. Sphingolipids and cell death. Apoptosis 2007, 12, 923–939. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Domínguez, N.; Ordóñez, R.; Fernández, A.; García-Palomo, A.; Muntané, J.; González-Gallego, J.; Mauriz, J.L. Modulation of autophagy by sorafenib: Effects on treatment response. Front. Pharmacol. 2016, 7, 151. [Google Scholar] [CrossRef] [Green Version]
- Méndez-Blanco, C.; Fondevila, F.; Fernández-Palanca, P.; García-Palomo, A.; van Pelt, J.; Verslype, C.; González-Gallego, J.; Mauriz, J.L. Stabilization of hypoxia-inducible factors and BNIP3 promoter methylation contribute to acquired sorafenib resistance in human hepatocarcinoma cells. Cancers 2019, 11, 1984. [Google Scholar] [CrossRef] [Green Version]
- Mauriz, J.L.; González-Gallego, J. Antiangiogenic drugs: Current knowledge and new approaches to cancer therapy. J. Pharm. Sci. 2008, 97, 4129–4154. [Google Scholar] [CrossRef]
- Morse, M.A.; Sun, W.; Kim, R.; He, A.R.; Abada, P.B.; Mynderse, M.; Finn, R.S. The role of angiogenesis in hepatocellular carcinoma. Clin. Cancer Res. 2019, 25, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Mancinelli, R.; Mammola, C.L.; Sferra, R.; Pompili, S.; Vetuschi, A.; Pannarale, L. Role of the angiogenic factors in cholangiocarcinoma. Appl. Sci. 2019, 9, 1393. [Google Scholar] [CrossRef] [Green Version]
- Jung, J.E.; Lee, H.; Cho, I.; Chung, D.H.; Yoon, S.; Yang, Y.M.; Lee, J.W.; Choi, S.; Park, J.; Ye, S.; et al. STAT3 is a potential modulator of HIF-1-mediated VEGF expression in human renal carcinoma cells. FASEB J. 2005, 19, 1296–1298. [Google Scholar] [CrossRef]
- Yu, H.; Pan, C.; Zhao, S.; Wang, Z.; Zhang, H.; Wu, W. Resveratrol inhibits tumor necrosis factor-α-mediated matrix metalloproteinase-9 expression and invasion of human hepatocellular carcinoma cells. Biomed. Pharmacother. 2008, 62, 366–372. [Google Scholar] [CrossRef]
- Scheau, C.; Badarau, I.A.; Costache, R.; Caruntu, C.; Mihai, G.L.; Didilescu, A.C.; Constantin, C.; Neagu, M. The role of matrix metalloproteinases in the epithelial-mesenchymal transition of hepatocellular carcinoma. Anal. Cell. Pathol. 2019, 2019, 9423907. [Google Scholar] [CrossRef] [Green Version]
- Reiter, R.J.; Sharma, R.; Ma, Q. Switching diseased cells from cytosolic aerobic glycolysis to mitochondrial oxidative phosphorylation: A metabolic rhythm regulated by melatonin? J. Pineal Res. 2021, 70, e12677. [Google Scholar] [CrossRef] [PubMed]
- Bizarri, M.; Proietti, S.; Cucina, A.; Reiter, R.J. Molecular mechanisms of the pro-apoptotic actions of melatonin in cancer: A review. Expert Opin. Ther. Targets 2013, 17, 1483–1496. [Google Scholar] [CrossRef] [PubMed]



| First Author, Publication Year, [Reference] | Country | Liver Tumor | Experimental Model (n, Sample Size per Group) | Administration Strategy | Treatment Regimen | Process Alteration |
|---|---|---|---|---|---|---|
| Dakshayani et al. 2005 [20] | India | HCC | In vivo Adult male Wistar rats Intraperitoneal injection of DEN followed by subcutaneous CCl4 (n = 6) | Intraperitoneal melatonin | 5 mg/kg 20 weeks | Antioxidant and hepatoprotective activity |
| Dakshayani et al. 2007 [21] | India | HCC | In vivo Adult male Wistar rats Intraperitoneal injection of DEN followed by subcutaneous CCl4 (n = 6) | Intraperitoneal melatonin | 5 mg/kg Thrice a week 20 weeks | Chronobiotic effect Antioxidant effect |
| Subramanian et al. 2007 [22] | India | HCC | In vivo 3-months-old male Wistar rats Intraperitoneal injection of DEN followed by subcutaneous of CCl4 (n = 6) | Intraperitoneal melatonin | 5 mg/kg Daily 20 weeks | Tumor growth inhibition Antioxidant activity |
| Martín-Renedo et al. 2008 [10] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin | 0.1–10 mM 4, 6, 8 and 10 days | Proliferation inhibition Apoptosis induction Cell cycle arrest |
| Subramanian et al. 2008 [23] | India | HCC | In vivo 3-months-old male Wistar rats Intraperitoneal injection of DEN followed by subcutaneous injection of CCl4 (n = 6) | Intraperitoneal melatonin | 5 mg/kg Daily 20 weeks | Chronobiotic effect Antioxidant effect |
| Carbajo-Pescador et al. 2009 [11] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin | 1–2.5 mM 2, 4 and 6 days | Proliferation inhibition Cell cycle arrest |
| Ozdemir et al. 2009 [24] | Turkey | HCC | In vitro Human HepG2 cell line | Melatonin | 0.05–1 mM 72 h | Cell cycle arrest |
| Fan et al. 2010 [25] | China | HCC | In vitro Human HepG2 and Bel-7402 cell lines | Melatonin + Doxorubicin | 0.01–10 µM 48 h | Proliferation inhibition Apoptosis induction |
| Laothong et al. 2010 [26] | Thailand | CCA | In vivo Male Syrian golden hamsters Oral inoculation of 50 metacercariae of Opisthorchis viverrini (n = 5) | Oral melatonin | 5, 10, 20 mg/kg Daily 30 days | Antioxidant and protective activity |
| Lin and Chuang 2010 [27] | Taiwan | HCC | In vitro Human HCC cell lines: HCC24/KMUH (resistant to AmB-induced oxidative stress) and HCC38/KMUH: (susceptible to AmB-induced oxidative stress) | Melatonin | 1 and 100 µM 24 h | Proliferation increase |
| Melatonin + AmB | 1 and 100 µM 24 h | Antiangiogenic effect | ||||
| Carbajo-Pescador et al. 2011 [12] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin | 1–2.5 mM 12, 24 and 48 h | Proliferation inhibition |
| Han et al. 2011 [28] | New York | CCA | In vivo 6-weeks-old male BALB/c nude mice Subcutaneous injection of Mz-ChA-1 cells (n = 4) | Intraperitoneal melatonin | 4 mg/kg Thrice a week 43 days | Proliferation inhibition |
| Carbajo-Pescador et al. 2012 [29] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin | 50–2000 µM 1, 6, 24 and 48 h | Apoptosis induction |
| Cid et al. 2012 [30] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin + MF exposure | 0.01–1000 nM 4, 5 and 7 days | Proliferation inhibition |
| Liu et al. 2012 [31] | China | HCC | In vitro Mouse hepatoma cell line H22 | Melatonin | 100 µM 24 h | Apoptosis induction |
| Melatonin + Beclin-1 RNAi Melatonin + 3-MA | 100 µM 24 h | Autophagy blockade Apoptosis induction | ||||
| In vivo 8-weeks-old female BALB/c mice Subcutaneous injection of H22 cells (n = 10) | Intraperitoneal melatonin | 10 or 20 mg/kg Daily 14 days | Autophagy induction | |||
| Zha et al. 2012 [32] | China | HCC | In vitro Human HCC HepG2 cell line Human hepatocyte HL-7702 cell line | Melatonin + Tunicamycin | 10−7 µM 24 h | Proliferation inhibition Apoptosis induction |
| Carbajo-Pescador et al. 2013 [13] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin | 1 nM and 1 mM 2, 4, 6, 8, 12 and 24 h or 24 h | Hypoxia-dependent angiogenesis |
| Fan et al. 2013 [33] | China | HCC | In vitro Human HepG2 and SMMC-7721 cell lines | Melatonin + Doxorubicin | 1 mM 24 h | Apoptosis induction |
| Melatonin + Doxorubicin + Tunicamycin | 0.1–1000 µM 24 h | Proliferation inhibition Apoptosis induction | ||||
| Fan et al. 2013b [34] | China | HCC | In vitro Human HepG2 and SMMC-7721 cell lines | Melatonin | 0.001–1000 µM 24 and 48 h | Proliferation inhibition Apoptosis induction |
| Laothong et al. 2013 [35] | Thailand | CCA | In vivo 4-to-6-weeks-old male Syrian golden hamsters Oral inoculation of 50 metacercariae of Opisthorchis viverrini and 12.5 ppm DEN (n = 15) | Oral melatonin | 10 or 50 mg/kg Daily 120 days | Apoptosis induction |
| Tomov et al. 2013 [36] | Bulgaria | HCC | Case report 67-years-old female | Intermittent administration of IL-2, BCG and oral melatonin | 20 mg Daily | Immunomodulation |
| Bennukul et al. 2014 [37] | Thailand | HCC | In vitro Human HepG2 cell line | Melatonin | 0.5–5 mM 24 and 48 h | Autophagy induction |
| Melatonin + Cisplatin | ||||||
| Ordóñez et al. 2014 [15] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin | 1 mM 24 h | Angiogenesis and invasion inhibition |
| Melatonin + IL-1β | ||||||
| Verma et al. 2014 [38] | Malaysia | HCC | In vivo Adult male mice Intraperitoneal injection of DEN (n = 6) | Intraperitoneal melatonin | 0.5 mg/kg Thrice a week 10 weeks | Antioxidant activity Modulation of circadian rhythms |
| Laothong et al. 2015 [39] | Thailand | CCA | In vitro Human KKU-M055 and KKU-M214 cell lines | Melatonin | 0.5, 1 and 2 mM 48 h | Oxidative stress activity Apoptosis induction |
| Moreira et al. 2015 [17] | Brazil | HCC | In vivo Male Wistar rats Intraperitoneal injection of DEN and 2-AAF administration at week 4 (n = 12) | Oral melatonin | 1 mg/kg Daily 45 and 90 days | Apoptosis induction |
| Ordóñez et al. 2015 [16] | Spain | HCC | In vitro Human HepG2 cell line | Melatonin | 2 mM 0.5–48 h | Apoptosis induction Autophagy induction |
| Colombo et al. 2016 [40] | Brazil | HCC | In vitro Human HepG2 cell line | Melatonin | 1–106 nM 24 h | Proliferation inhibition |
| 1 mM 24 h | Inhibition of hypoxia-derived invasion | |||||
| Prieto-Domínguez et al. 2016 [18] | Spain | HCC | In vitro Human HepG2, HuH7 and Hep3B cell lines | Melatonin | 0.1–2 mM | Proliferation inhibition Pro-oxidant activity Mitophagy induction Apoptosis induction |
| Melatonin + Sorafenib | ||||||
| Bu et al. 2017 [41] | China | HCC | In vitro Human HepG2 cell line | Melatonin + Tunicamycin | 10−6 –1 mM | Apoptosis induction and ER stress |
| Cheng et al. 2017 [42] | China | HCC | In vitro Human HepG2 and Bel-7402 cell lines | Melatonin | 0.1 mM | Immunomodulation |
| In vivo 6-weeks-old female BALB/c nude mice Injected with Exo-con or Exo-MT (0.1 mM melatonin) | Exo-MT | 100 µL Daily 10 days | ||||
| Hao et al. 2017 [43] | China | HCC | In vitro Human Bel-7402, SNU-449, HepG2 and Hep3B 2.1-7 cell line | Melatonin | 1 mM 48 h | Proliferation inhibition Inhibition of cell migration ability Apoptosis induction |
| Melatonin + CDDP | ||||||
| Lin et al. 2017 [44] | China | HCC | In vitro Human HuH7 cell line | Melatonin | 1–5 mM 48 h | Proliferation inhibition Apoptosis induction |
| Melatonin + Sorafenib | ||||||
| Liu et al. 2017 [45] | China | HCC | In vitro Human HepG2 and Bel-7402 cell lines | Melatonin | 10 µM 48 h | Apoptosis induction |
| Melatonin + Sorafenib | 1–100 µM 48 h | Proliferation inhibition | ||||
| 10 µM 48 h | Apoptosis induction Autophagy blockage | |||||
| Long et al. 2017 [46] | China | HCC | In vitro Human Bel-7402, SMMC-7721 HCC cell lines Human normal liver L02 cell line | Melatonin | 0.2–2 mM 48–72 h | Proliferation inhibition |
| Melatonin + Sorafenib | 1 mM 48 h 2 weeks | Proliferation inhibition Cell cycle arrest | ||||
| In vivo 4-weeks-old female BALB/c nude mice Subcutaneous injection of SMMC-7721 cells (n = 4) | Intraperitoneal melatonin | 25 mg/kg Daily 18 days | Tumor growth inhibition | |||
| Intraperitoneal melatonin + sorafenib | ||||||
| Prieto-Domínguez et al. 2017 [4] | Spain | HCC | In vitro Human Hep3B cell line | Melatonin | 1 or 2 mM 24 or 48 h | Pro-oxidant activity Proliferation inhibition |
| Melatonin + Sorafenib | Proliferation inhibition Blockade of sorafenib-induced mitophagy | |||||
| Sánchez et al. 2017 [47] | Spain | HCC | In vivo 6-weeks-old male ICR mice Intraperitoneal injection of DEN | Intraperitoneal melatonin | 5 or 10 mg/kg Daily 10, 20, 30, 40 weeks | Cell cycle arrest Modulation of sphingolipid metabolism |
| Wang et al. 2017 [48] | Taiwan | HCC | In vitro Human HepG2 and HuH7 cell lines | Melatonin | 1 mM 12, 24, 36, 48, 60 and 72 h | Proliferation inhibition |
| 1 mM 24, 48 and 72 h | Suppression of cell migration ability | |||||
| 1 mM 24 h | EMT inhibition | |||||
| In vivo 6-to-8-weeks-old male BALB/c nude mice Subcutaneous injection of HuH7 cells (n = 10) | Intraperitoneal melatonin | 40 mg/kg Five days per week | Tumor growth inhibition EMT suppression | |||
| Wongsena et al. 2017 [49] | Thailand | CCA | In vivo 6-to-8-weeks-old male Syrian golden hamsters Oral infection with 50 metacercariae of Opisthorchis viverrini and oral administration with DEN (n = 7) | Oral melatonin | 50 mg/kg Daily 30 days | Immunomodulation |
| Chen et al. 2018 [50] | Taiwan | HCC | In vitro Human HuH7 and HepG2 cell lines | Melatonin | 1 mM 12, 24, 36, 48, 60 and 72 h | Proliferation inhibition |
| 1 mM 24, 48 and 72 h | Suppression of migration and invasion abilities | |||||
| Melatonin + Etoposide | 1 mM 12, 24, 36, 48, 60, and 72 h | Proliferation inhibition Apoptosis induction | ||||
| Melatonin + Camptothecin | 1 mM 24 h | |||||
| Chen et al. 2018 [50] | Taiwan | HCC | In vivo 6-weeks-old male BALB/c nude mice Subcutaneous injection of HuH7 cells (n = 6) | Intraperitoneal melatonin | 40 mg/kg Five days/week 25 days | Tumor growth inhibition Apoptosis induction |
| Intraperitoneal melatonin + etoposide | ||||||
| Colombo et al. 2018 [51] | Brazil | HCC | In vitro Human HepG2 cell line | Melatonin | 1 mM 24 h | Increase of NF-κB protein expression |
| Dauchy et al. 2018 [52] | USA | HCC | In vivo Male Buffalo rats Implantation of Morris 7288CTC hepatomas (control: n = 6; experimental: n = 9) | Endogenous melatonin | Increase of endogenous melatonin levels | Tumor growth inhibition |
| Sánchez et al. 2018 [14] | Spain | HCC | In vitro Human Hep3B cell line | Melatonin | 0.5 or 1 mM 1 h | Proliferation inhibition Apoptosis induction |
| Melatonin + SR9009 | Proliferation inhibition | |||||
| Melatonin + Bmal1 siRNA | 0.5 or 1 mM 24 h | Proliferation inhibition Apoptosis induction | ||||
| In vivo 6-weeks-old male ICR mice Intraperitoneal injection of DEN (n = 4–8) | Intraperitoneal melatonin | 5 or 10 mg/kg Daily 10, 20, 30, 40 weeks | Circadian clock modulation Cell cycle arrest Apoptosis induction | |||
| Wang et al. 2018 [53] | Taiwan | HCC | In vitro Human HepG2 and HuH7 cell lines | Melatonin | 1 and 2 mM 12, 24, 36, 48, 60 and 72 h | Proliferation inhibition |
| 1 and 2 mM 24, 48 and 72 h | Suppression of migration and invasion abilities | |||||
| Melatonin + let-7i-3p inhibitor | 1 and 2 mM 24 and 48 h | Proliferation inhibition Migration and invasion suppression | ||||
| In vivo 6–8-weeks-old male BALB/c nude mice Subcutaneous injection of HuH7 cells (n = 6) | Intraperitoneal melatonin | 40 mg/kg 5 days per week 35 days | Tumor growth inhibition | |||
| El-Magd et al. 2019 [54] | Egypt | HCC | In vivo Adult female rats Intraperitoneal injection of DEN and oral administration of 2-AAF at week 2 (n = 10) | Intraperitoneal melatonin | 20 mg/kg Twice a week 5 weeks | Apoptosis induction Antioxidant activity Reduction of angiogenesis and metastasis |
| Intraperitoneal melatonin + MSCs | ||||||
| Intraperitoneal injection of MSCs preincubated with melatonin | 5 µM 24 h | |||||
| Mohamed et al. 2019 [55] | Egypt | HCC | In vivo Adult female rats Intraperitoneal injection of DEN followed by oral administration of 2-AAF at week 2 (n = 10) | Intraperitoneal melatonin | 20 mg/kg Twice a week 5 weeks | Tumor growth inhibition Apoptosis induction |
| Intraperitoneal injection of MSCs preincubated with melatonin 5 µM for 24 h | ||||||
| Zhang et al. 2019 [56] | China | HCC | In vitro Human HepG2 cell line | Melatonin | 3 mM 48 h | Suppression of migration |
| 1 mM 14 days | Proliferation inhibition | |||||
| Melatonin + EGCG | 3 mM 48 h | Suppression of migration | ||||
| 1 mM 14 days | Proliferation inhibition | |||||
| Zhou et al. 2019 [57] | China | HCC | In vitro Human HepG2, 7721 and HuH7 HCC cell lines Human liver L02 cell line | Melatonin | 1–100 µM 48 h | Apoptosis induction |
| 10 µM 48 h | Autophagy inhibition | |||||
| Melatonin + Sorafenib | 1–100 µM 48 h | Proliferation inhibition Apoptosis induction | ||||
| 10 µM 48 h | Autophagy inhibition | |||||
| Ao et al. 2020 [58] | China | HCC | In vitro Human HepG2 and HuH7 cell lines | Melatonin | 2.5 mM 24 h | Apoptosis induction |
| Mi and Kuang 2020 [59] | China | HCC | In vitro Human HepG2 and Hep3B cell lines | Melatonin | 1 or 2 mM 24, 48, 72, 96 h | Proliferation inhibition |
| 1 or 2 mM 48 h | Cell cycle arrest | |||||
| Melatonin + Cisplatin | 1 or 2 mM 24 and 48 h | Proliferation inhibition Apoptosis induction | ||||
| Wang et al. 2020 [60] | China | HCC | In vitro Human SMMC-7721, cell line | Melatonin + Regorafenib | 50 µM 24 h | Antioxidant activity Apoptosis induction |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Palanca, P.; Méndez-Blanco, C.; Fondevila, F.; Tuñón, M.J.; Reiter, R.J.; Mauriz, J.L.; González-Gallego, J. Melatonin as an Antitumor Agent against Liver Cancer: An Updated Systematic Review. Antioxidants 2021, 10, 103. https://doi.org/10.3390/antiox10010103
Fernández-Palanca P, Méndez-Blanco C, Fondevila F, Tuñón MJ, Reiter RJ, Mauriz JL, González-Gallego J. Melatonin as an Antitumor Agent against Liver Cancer: An Updated Systematic Review. Antioxidants. 2021; 10(1):103. https://doi.org/10.3390/antiox10010103
Chicago/Turabian StyleFernández-Palanca, Paula, Carolina Méndez-Blanco, Flavia Fondevila, María J. Tuñón, Russel J. Reiter, José L. Mauriz, and Javier González-Gallego. 2021. "Melatonin as an Antitumor Agent against Liver Cancer: An Updated Systematic Review" Antioxidants 10, no. 1: 103. https://doi.org/10.3390/antiox10010103