Longitudinal Analysis Evaluating Self-Reported CPAP Use for OSA during the COVID-19 Pandemic
Abstract
:1. Introduction
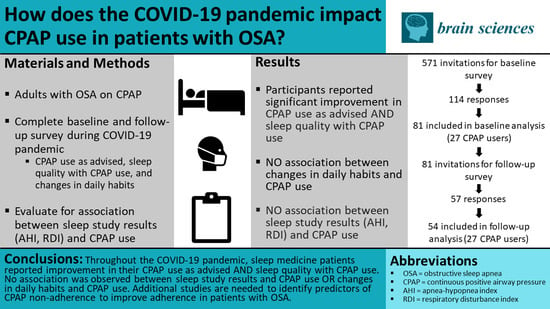
2. Materials and Methods
2.1. Participants
2.2. Data, Analysis, and Statistics
3. Results
3.1. Characteristics of Participants
3.2. Longitudial Analysis of CPAP Use during the COVID-19 Pandemic
3.3. Analysis of Sleep Study Results and CPAP Use during the COVID-19 Pandemic
3.4. Analysis of Changes in Daily Habits during the COVID-19 Pandemic and CPAP Use
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Young, T.; Peppard, P.E.; Gottlieb, D.J. Epidemiology of Obstructive Sleep Apnea: A population health perspective. Am. J. Respir. Crit. Care Med. 2002, 165, 1217–1239. [Google Scholar] [CrossRef] [PubMed]
- Marin, J.M.; Carrizo, S.J.; Vicente, E.; Agusti, A.G. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 2005, 365, 1046–1053. [Google Scholar] [CrossRef]
- Dhillon, S.; Chung, S.A.; Fargher, T.; Huterer, N.; Shapiro, C.M. Sleep Apnea, Hypertension, and the Effects of Continuous Positive Airway Pressure. Am. J. Hypertens. 2005, 18 Pt 1, 594–600. [Google Scholar] [CrossRef] [Green Version]
- Babu, A.R.; Herdegen, J.; Fogelfeld, L.; Shott, S.; Mazzone, T. Type 2 Diabetes, Glycemic Control, and Continuous Positive Airway Pressure in Obstructive Sleep Apnea. Arch. Intern. Med. 2005, 165, 447–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kribbs, N.B.; Pack, A.; Kline, L.R.; Smith, P.L.; Schwartz, A.R.; Schubert, N.M.; Redline, S.; Henry, J.N.; Getsy, J.E.; Dinges, D.F. Objective Measurement of Patterns of Nasal CPAP Use by Patients with Obstructive Sleep Apnea. Am. Rev. Respir. Dis. 1993, 147, 887–895. [Google Scholar] [CrossRef]
- Reeves-Hoché, M.K.; Meck, R.; Zwillich, C.W. Nasal CPAP: An objective evaluation of patient compliance. Am. J. Respir. Crit. Care Med. 1994, 149, 149–154. [Google Scholar] [CrossRef]
- Engleman, H.M.; Martin, S.E.; Douglas, N.J. Compliance with CPAP therapy in patients with the sleep apnoea/hypopnoea syndrome. Thorax 1994, 49, 263–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krieger, J. Long-Term Compliance With Nasal Continuous Positive Airway Pressure (CPAP) in Obstructive Sleep Apnea Patients and Nonapneic Snorers. Sleep 1992, 15 (Suppl. 6), S42–S46. [Google Scholar] [CrossRef] [Green Version]
- Sanders, M.H.; Gruendl, C.A.; Rogers, R.M. Patient Compliance with Nasal CPAP Therapy for Sleep Apnea. Chest 1986, 90, 330–333. [Google Scholar] [CrossRef]
- Weaver, T.E.; Kribbs, N.B.; Pack, A.; Kline, L.R.; Chugh, D.K.; Maislin, G.; Smith, P.L.; Schwartz, A.R.; Schubert, N.M.; Gillen, K.A.; et al. Night-To-Night Variability in CPAP Use Over the First Three Months of Treatment. Sleep 1997, 20, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.P.; Ayappa, I.A.; Caples, S.M.; Kimoff, R.J.; Patel, S.; Harrod, C.G. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2019, 15, 335–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sawyer, A.M.; Gooneratne, N.S.; Marcus, C.L.; Ofer, D.; Richards, K.C.; Weaver, T.E. A systematic review of CPAP adherence across age groups: Clinical and empiric insights for developing CPAP adherence interventions. Sleep Med. Rev. 2011, 15, 343–356. [Google Scholar] [CrossRef] [Green Version]
- Lai, A.Y.; Fong, D.Y.; Lam, J.C.; Weaver, T.E.; Ip, M.S. The Efficacy of a Brief Motivational Enhancement Education Program on CPAP Adherence in OSA. Chest 2014, 146, 600–610. [Google Scholar] [CrossRef]
- Chervin, R.D.; Theut, S.; Bassetti, C.; Aldrich, M.S. Compliance with Nasal CPAP Can Be Improved by Simple Interventions. Sleep 1997, 20, 284–289. [Google Scholar] [CrossRef] [Green Version]
- Demirovic, S.; Kalcina, L.L.; Dodig, I.P.; Pecotic, R.; Valic, M.; Ivkovic, N.; Dogas, Z. The COVID-19 Lockdown and CPAP Adherence: The More Vulnerable Ones Less Likely to Improve Adherence? Nat. Sci. Sleep 2021, 13, 1097–1108. [Google Scholar] [CrossRef]
- Barker, J.; Oyefeso, O.; Koeckerling, D.; Mudalige, N.L.; Pan, D. COVID-19: Community CPAP and NIV should be stopped unless medically necessary to support life. Thorax 2020, 75, 367. [Google Scholar] [CrossRef] [Green Version]
- Baker, J.G.; Sovani, M. Case for continuing community NIV and CPAP during the COVID-19 epidemic. Thorax 2020, 75, 368. [Google Scholar] [CrossRef] [Green Version]
- Johnston, K.L.; Lawrence, S.M.; Dodds, N.E.; Yu, L.; Daley, D.C.; Pilkonis, P.A. Evaluating PROMIS® instruments and methods for patient-centered outcomes research: Patient and provider voices in a substance use treatment setting. Qual. Life Res. 2015, 25, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Shadel, W.G.; Edelen, M.O.; Tucker, J.S.; Stucky, B.D.; Hansen, M.; Cai, L. Development of the PROMIS® Coping Expectancies of Smoking Item Banks. Nicotine Tob. Res. 2014, 16 (Suppl. 3), S202–S211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schalet, B.D.; Pilkonis, P.A.; Yu, L.; Dodds, N.; Johnston, K.L.; Yount, S.; Riley, W.; Cella, D. Clinical validity of PROMIS Depression, Anxiety, and Anger across diverse clinical samples. J. Clin. Epidemiol. 2016, 73, 119–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pilkonis, P.A.; Yu, L.; Dodds, N.E.; Johnston, K.L.; Lawrence, S.M.; Daley, D.C. Validation of the alcohol use item banks from the Patient-Reported Outcomes Measurement Information System (PROMIS®). Drug Alcohol Depend. 2016, 161, 316–322. [Google Scholar] [CrossRef]
- Yu, L.; Buysse, D.J.; Germain, A.; Moul, D.E.; Stover, A.; Dodds, N.E.; Johnston, K.L.; Pilkonis, P.A. Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behav. Sleep Med. 2012, 10, 6–24. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. Perceived stress scale. In Measuring Stress: A Guide for Health and Social Scientists; Oxford University Press: Oxford, UK, 1994; Volume 10, pp. 1–2. [Google Scholar]
- Carver, C.S. You want to measure coping but your protocol’too long: Consider the brief cope. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallieres, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Lee, S.A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020, 44, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare and Medicaid Services Website. Decision Memo for Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (CAG-00093N). 30 October 2001. Available online: https://www.cms.gov/medicare-coveragedatabase/details/nca-decision-memo.aspx?NCAId=19&fromdb=true (accessed on 2 January 2022).
- Attias, D.; Pepin, J.L.; Pathak, A. Impact of COVID-19 lockdown on adherence to continuous positive airway pressure by obstructive sleep apnoea patients. Eur. Respir. J. 2020, 56, 2001607. [Google Scholar] [CrossRef] [PubMed]
- Tepwimonpetkun, C.; Muntham, D.; Suppasawatgul, P.; Chirakalwasan, N. Positive airway pressure therapy adherence for obstructive sleep apnea during the COVID-19 pandemic. Sleep Breath 2021, 1–7. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8525851/ (accessed on 2 January 2022).
- Tracking Coronavirus in Texas: Latest Map and Case Count. The New York Times, 3 January 2022. Available online: https://www.nytimes.com/interactive/2021/us/texas-COVID-cases.html(accessed on 3 January 2022).

| Demographic Data | Participants in Baseline Survey, n = 81 | Participants in 6-Month Follow-Up Survey, n = 54 | Participants with CPAP Device, n = 27 |
|---|---|---|---|
| Age, years | 54.8 ± 15.9 | 55.2 ± 18.4 | 58 ± 18.2 |
| Sex | |||
| Female | 45 (55.6) | 33 (66.1) | 13 (48.2) |
| Male | 36 (44.4) | 21 (38.9) | 14 (51.8) |
| Race | |||
| Caucasian | 56 (69.1) | 38 (70.4) | 18 (66.7) |
| African American | 16 (19.8) | 12 (22.2) | 7 (25.9) |
| Asian | 4 (4.9) | 3 (5.6) | 1 (3.7) |
| Not reported | 5 (6.2) | 1 (1.9) | 1 (3.7) |
| α BMI, kg/m2 | 34.9 ± 12.4 | ||
| β AHI, events/hour | 8.2 ± 10.7 | ||
| Ω Current smoker | 1 (3.9) | ||
| ϕ Diabetes mellitus | 10 (38.5) | ||
| Self-reported CPAP usage per night, hours | |||
| 1–3 h | 1 (3.7) | ||
| ≥4 h | 26 (96.3) | ||
| Self-reported CPAP usage per week, nights | |||
| 1–3 nights | |||
| ≥4 nights | 27 (100) |
| Variable | Description | Participants in Baseline Survey, n (%) | Participants in 6-Month Follow-Up Survey, n (%) | p Value |
|---|---|---|---|---|
| CPAP use | Yes | 27 (33) | 27 (50) | - |
| No | 54 (67) | 27 (50) | ||
| Change in CPAP use | No change | 23 (85.2) | 24 (88.9) | |
| Use more | 3 (11.1) | 2 (7.4) | 0.166 | |
| Use less | 1 (3.7) | 1 (3.7) | ||
| Change in sleep quality with CPAP use | No change | 9 (33.3) | 7 (25.9) | |
| Better | 13 (48.2) | 19 (70.4) | 0.012 * | |
| Worse | 5 (18.5) | 1 (3.7) | ||
| Change in CPAP use as advised | Unsure | 6 (22.2) | 0 | |
| No | 4 (14.8) | 3 (11.1) | 0.003 * | |
| Yes | 17 (63.0) | 24 (88.9) |
| Sleep Study Results | Change in CPAP Use | Sleep Quality with CPAP Use | Change in CPAP Use as Advised |
|---|---|---|---|
| AHI | 1.02 (0.65) | 0.87 (0.13) | 1.03 (0.61) |
| RDI | 9.53 (0.75) | 0.11 (0.74) | 0.91 (0.51) |
| Daily Habit | Description | No Change in CPAP Use, n (%) | More CPAP Use, n (%) | Less CPAP Use, n (%) | p Value |
|---|---|---|---|---|---|
| Employment change | Yes | 4 (14.8) | - | - | 0.605 |
| No | 20 (74.1) | 2 (7.4) | 1 (3.7) | ||
| Healthcare change | Yes | 15 (55.6) | 2 (7.4) | - | 0.155 |
| No | 9 (33.3) | - | 1 (3.7) | ||
| Electronics | Less time | 1 (3.7) | - | - | 0.331 |
| More time | 16 (59.3) | 2 (7.4) | 1 (3.7) | ||
| No change | 7 (25.9) | - | - | ||
| Change in sleep medication | Yes | 1 (3.7) | - | - | 0.074 |
| No | 21 (91.3) | 1 (3.7) | - | ||
| No medications | 2 (7.4) | 1 (3.7) | 1 (3.7) | ||
| Exercise | Less time | 13 (48.2) | - | 1 (3.7) | 0.072 |
| More time | 3 (11.1) | - | - | ||
| No change | 8 (29.6) | 2 (7.4) | - | ||
| Sunlight exposure | Less time | 15 (55.6) | 1 (3.7) | 1 (3.7) | 0.124 |
| More time | 3 (11.1) | 1 (3.7) | - | ||
| No change | 6 (22.2) | - | - | ||
| Caffeine consumption | Less | - | - | - | 0.132 |
| More | 4 (14.8) | - | 1 (3.7) | ||
| No change | 20 (74.1) | 2 (7.4) | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teague, T.T.; Debian, A.; Kokonda, M.; Malhotra, S.; Arentson-Lantz, E.; Shaib, F.; Nowakowski, S. Longitudinal Analysis Evaluating Self-Reported CPAP Use for OSA during the COVID-19 Pandemic. Brain Sci. 2022, 12, 131. https://doi.org/10.3390/brainsci12020131
Teague TT, Debian A, Kokonda M, Malhotra S, Arentson-Lantz E, Shaib F, Nowakowski S. Longitudinal Analysis Evaluating Self-Reported CPAP Use for OSA during the COVID-19 Pandemic. Brain Sciences. 2022; 12(2):131. https://doi.org/10.3390/brainsci12020131
Chicago/Turabian StyleTeague, Taylor Torrence, Ahmad Debian, Manasa Kokonda, Sonal Malhotra, Emily Arentson-Lantz, Fidaa Shaib, and Sara Nowakowski. 2022. "Longitudinal Analysis Evaluating Self-Reported CPAP Use for OSA during the COVID-19 Pandemic" Brain Sciences 12, no. 2: 131. https://doi.org/10.3390/brainsci12020131