Prevalence of Neural Autoantibodies in Epilepsy of Unknown Etiology: Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Identification and Selection
2.2. Data Extraction and Bias Evaluation
2.3. Data Synthesis and Analysis
3. Results
3.1. Search
3.2. Characteristics of the Included Studies for Qualitative Synthesis
3.3. Neural Autoantibodies Pooled Prevalence
3.4. Heterogeneity and Publication Bias Assessment
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Spatola, M.; Novy, J.; Du Pasquier, R.; Dalmau, J.; Rossetti, A.O. Status epilepticus of inflammatory etiology. Neurology 2015, 85, 464–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geis, C.; Planagumà, J.; Carreño, M.; Graus, F.; Dalmau, J. Autoimmune seizures and epilepsy. J. Clin. Investig. 2019, 129, 926–940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheffer, I.E.; Berkovic, S.; Capovilla, G.; Connolly, M.B.; French, J.; Guilhoto, L.; Hirsch, E.; Jain, S.; Mathern, G.W.; Moshé, S.L.; et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017, 58, 512–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Husari, K.S.; Dubey, D. Autoimmune Epilepsy. Neurother. J. Am. Soc. Exp. Neurother. 2019, 16, 685–702. [Google Scholar]
- Fisher, R.S.; Acevedo, C.; Arzimanoglou, A.; Bogacz, A.; Cross, J.H.; Elger, C.E.; Engel, J.; Forsgren, L.; French, J.A.; Glynn, M.; et al. ILAE Official Report: A practical clinical definition of epilepsy. Epilepsia 2014, 55, 475–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steriade, C.; Britton, J.; Dale, R.C.; Gadoth, A.; Irani, S.R.; Linnoila, J.; McKeon, A.; Shao, X.; Venegas, V.; Bien, C.G. Acute symptomatic seizures secondary to autoimmune encephalitis and autoimmune-associated epilepsy: Conceptual definitions. Epilepsia 2020, 61, 1341–1351. [Google Scholar] [CrossRef]
- Rada, A.; Birnbacher, R.; Gobbi, C.; Kurthen, M.; Ludolph, A.; Naumann, M.; Neirich, U.; von Oertzen, T.J.; Ransmayr, G.; Riepe, M.; et al. Seizures associated with antibodies against cell surface antigens are acute symptomatic and not indicative of epilepsy: Insights from long-term data. J. Neurol. 2021, 268, 1059–1069. [Google Scholar] [CrossRef] [PubMed]
- Hansen, N.; Ernst, L.; Rüber, T.; Widman, G.; Becker, A.J.; Elger, C.E.; Helmstaedter, C. Pre- and long-term postoperative courses of hippocampus-associated memory impairment in epilepsy patients with antibody-associated limbic encephalitis and selective amygdalohippocampectomy. Epilepsy Behav. 2018, 79, 93–99. [Google Scholar] [CrossRef]
- McGinty, R.N.; Handel, A.; Moloney, T.; Ramesh, A.; Fower, A.; Torzillo, E.; Kramer, H.; Howell, S.; Waters, P.; Adcock, J.; et al. Clinical features which predict neuronal surface autoantibodies in new-onset focal epilepsy: Implications for immunotherapies. J. Neurol. Neurosurg. Psychiatry 2021, 92, 291–294. [Google Scholar] [CrossRef]
- Ansari, B.; Etemadifar, M.; Najafi, M.; Nasri, M.; Meamar, R. Neuronal autoantibodies in focal epilepsy with or without mesial temporal sclerosis. Iran. J. Neurol. 2019, 18, 13–18. [Google Scholar] [CrossRef] [Green Version]
- Iorio, R.; Assenza, G.; Tombini, M.; Colicchio, G.; Della Marca, G.; Benvenga, A.; Damato, V.; Rossini, P.M.; Vollono, C.; Plantone, D.; et al. The detection of neural autoantibodies in patients with antiepileptic-drug-resistant epilepsy predicts response to immunotherapy. Eur. J. Neurol. 2015, 22, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Brenner, T.; Sills, G.J.; Hart, Y.; Howell, S.; Waters, P.; Brodie, M.J.; Vincent, A.; Lang, B. Prevalence of neurologic autoantibodies in cohorts of patients with new and established epilepsy. Epilepsia 2013, 54, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Liimatainen, S.; Peltola, M.; Sabater, L.; Fallah, M.; Kharazmi, E.; Haapala, A.-M.; Dastidar, P.; Knip, M.; Saiz, A.; Peltola, J. Clinical significance of glutamic acid decarboxylase antibodies in patients with epilepsy. Epilepsia 2010, 51, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Tecellioglu, M.; Kamisli, O.; Kamisli, S.; Yucel, F.E.; Ozcan, C. Neurological autoantibodies in drug-resistant epilepsy of unknown cause. Ir. J. Med. Sci. 2018, 187, 1057–1063. [Google Scholar] [CrossRef]
- Gozubatik-Celik, G.; Ozkara, C.; Ulusoy, C.; Gunduz, A.; Delil, S.; Yeni, N.; Tuzun, E. Anti-Neuronal Autoantibodies in Both Drug Responsive and Resistant Focal Seizures with Unknown Cause. Epilepsy Res. 2017, 135, 131–136. [Google Scholar] [CrossRef]
- Ekizoglu, E.; Tuzun, E.; Woodhall, M.; Lang, B.; Jacobson, L.; Icoz, S.; Bebek, N.; Gurses, C.; Gokyigit, A.; Waters, P.; et al. Investigation of neuronal autoantibodies in two different focal epilepsy syndromes. Epilepsia 2014, 55, 414–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falip, M.; Carreno, M.; Miró, J.; Saiz, A.; Villanueva, V.; Quílez, A.; Molins, A.; Barceló, I.; Sierra, A.; Graus, F. Prevalence and immunological spectrum of temporal lobe epilepsy with glutamic acid decarboxylase antibodies. Eur. J. Neurol. 2012, 19, 827–833. [Google Scholar] [CrossRef]
- Dubey, D.; Alqallaf, A.; Hays, R.; Freeman, M.; Chen, K.; Ding, K.; Agostini, M.; Vernino, S. Neurological Autoantibody Prevalence in Epilepsy of Unknown Etiology. JAMA Neurol. 2017, 74, 397–402. [Google Scholar] [CrossRef]
- De Bruijn, M.A.; Bastiaansen, A.E.; Mojzisova, H.; van Sonderen, A.; Thijs, R.D.; Majoie, M.J.; Rouhl, R.P.; van Coevorden-Hameete, M.H.; de Vries, J.M.; Lopetegi, A.M.; et al. The Antibodies Contributing to focal Epilepsy Signs and symptoms (ACES) score. Ann. Neurol. 2021. [Google Scholar] [CrossRef]
- Li, Y.; Tymchuk, S.; Barry, J.; Muppidi, S.; Le, S. Antibody Prevalence in Epilepsy before Surgery (APES) in drug-resistant focal epilepsy. Epilepsia 2021, 1–9. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pleasure, D. Diagnostic and Pathogenic Significance of Glutamate Receptor Autoantibodies. Arch. Neurol. 2008, 65, 589–592. [Google Scholar] [CrossRef] [Green Version]
- Michael, S.; Waters, P.; Irani, S.R. Stop testing for autoantibodies to the VGKC-complex: Only request LGI1 and CASPR2. Pract. Neurol. 2020, 20, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Lopetegi, A.; de Bruijn, M.A.; Boukhrissi, S.; Bastiaansen, A.E.; Nagtzaam, M.M.; Hulsenboom, E.S.; Boon, A.J.; Neuteboom, R.F.; de Vries, J.M.; Smitt, P.A.S.; et al. Neurologic syndromes related to anti-GAD65: Clinical and serologic response to treatment. Neurol. Neuroimmunol. Neuroinflammat. 2020, 7, e696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graus, F.; Saiz, A.; Dalmau, J. GAD antibodies in neurological disorders—Insights and challenges. Nat. Rev. Neurol. 2020, 16, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Miller, J. The Scottish Intercollegiate Guidelines Network (SIGN). Br. J. Diabetes Vasc. Dis. 2002, 2, 47–49. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions; The Cochrane Database of Systematic Reviews; John Wiley & Sons: Oxford, UK, 2019; Volume 10, p. ED000142. [Google Scholar]
- Yeshokumar, A.K.; Coughlin, A.; Fastman, J.; Psaila, K.; Harmon, M.; Randell, T.; Schorr, E.M.; Han, H.; Hoang, H.; Soudant, C.; et al. Seizures in autoimmune encephalitis—A systematic review and quantitative synthesis. Epilepsia 2021, 62, 397–407. [Google Scholar] [CrossRef]
- Stanojevic, M.; Savin, S.; Cvejiċ, D.; Djukic, A.; Jeremic, M.; Simonovic, S.Z. Comparison of the influence of thyroglobulin antibodies on serum thyroglobulin values from two different immunoassays in post surgical differentiated thyroid carcinoma patients. J. Clin. Lab. Anal. 2009, 23, 341–346. [Google Scholar] [CrossRef]
- Vogrig, A.; Joubert, B.; André-Obadia, N.; Gigli, G.L.; Rheims, S.; Honnorat, J. Seizure specificities in patients with antibody-mediated autoimmune encephalitis. Epilepsia 2019, 60, 1508–1525. [Google Scholar] [CrossRef]
- Kuehn, J.C.; Meschede, C.; Helmstaedter, C.; Surges, R.; Von Wrede, R.; Hattingen, E.; Vatter, H.; Elger, C.E.; Schoch, S.; Becker, A.J.; et al. Adult-onset temporal lobe epilepsy suspicious for autoimmune pathogenesis: Autoantibody prevalence and clinical correlates. PLoS ONE 2020, 29, e0241289. [Google Scholar] [CrossRef]
- Bozzetti, S.; Rossini, F.; Ferrari, S.; Delogu, R.; Cantalupo, G.; Marchioretto, F.; Zanette, G.; Zanoni, T.; Turatti, M.; Vitale, G.; et al. Epileptic seizures of suspected autoimmune origin: A multicentre retrospective study. J. Neurol. Neurosurg. Psychiatry 2020, 91, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Graus, F.; Titulaer, M.J.; Balu, R.; Benseler, S.; Bien, C.G.; Cellucci, T.; Cortese, I.; Dale, R.C.; Gelfand, J.M.; Geschwind, M.; et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016, 15, 391–404. [Google Scholar] [CrossRef] [Green Version]
- Déchelotte, B.; Muñiz-Castrillo, S.; Joubert, B.; Vogrig, A.; Picard, G.; Rogemond, V.; Pinto, A.-L.; Lombard, C.; Desestret, V.; Fabien, N.; et al. Diagnostic yield of commercial immunodots to diagnose paraneoplastic neurologic syndromes. Neurol. Neuroimmunol. Neuroinflamm. 2020, 7, e701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, N.; Fotedar, N.; Abboud, H. Confounders in the Interpretation of Paraneoplastic and Neuronal Autoantibody Panels. Clin. Lab. Med. 2020, 40, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Ricken, G.; Schwaiger, C.; De Simoni, D.; Pichler, V.; Lang, J.; Glatter, S.; Macher, S.; Rommer, P.S.; Scholze, P.; Kubista, H.; et al. Detection Methods for Autoantibodies in Suspected Autoimmune Encephalitis. Front. Neurol. 2018, 9, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Rüegg, S. Antineuronal antibodies and epilepsy: Treat the patient, not the lab. J. Neurol. Neurosurg. Psychiatry 2021, 92, 230. [Google Scholar] [CrossRef]
- Ekizoglu, E.; Baykan, B.; Sezgin, M.; Erdag, E.; Gundogdu-Unverengil, G.; Vanlı-Yavuz, E.N.; Tekturk, P.; Yılmaz, E.; Bebek, N.; Tuzun, E. Follow-up of patients with epilepsy harboring antiglycine receptor antibodies. Epilepsy Behav. 2019, 92, 103–107. [Google Scholar] [CrossRef]
- Cabezudo-García, P.; Mena-Vázquez, N.; Villagrán-García, M.; Serrano-Castro, P.J. Efficacy of antiepileptic drugs in autoimmune epilepsy: A systematic review. Seizure 2018, 59, 72–76. [Google Scholar] [CrossRef] [Green Version]
- Swayne, A.; Tjoa, L.; Broadley, S.; Dionisio, S.; Gillis, D.; Jacobson, L.; Woodhall, M.R.; McNabb, A.; Schweitzer, D.; Tsang, B.; et al. Antiglycine receptor antibody related disease: A case series and literature review. Eur. J. Neurol. 2018, 25, 1290–1298. [Google Scholar] [CrossRef] [Green Version]
- Dalmau, J.; Graus, F. Antibody-Mediated Encephalitis. N. Engl. J. Med. 2018, 378, 840–851. [Google Scholar] [CrossRef] [Green Version]
- Titulaer, M.J.; McCracken, L.; Gabilondo, I.; Armangué, T.; Glaser, C.; Iizuka, T.; Honig, L.S.; Benseler, S.M.; Kawachi, I.; Martinez-Hernandez, E.; et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: An observational cohort study. Lancet Neurol. 2013, 12, 157–165. [Google Scholar] [CrossRef] [Green Version]
- Gresa-Arribas, N.; Titulaer, M.J.; Torrents, A.; Aguilar, E.; McCracken, L.; Leypoldt, F.; Gleichman, A.J.; Balice-Gordon, R.; Rosenfeld, M.R.; Lynch, D.; et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: A retrospective study. Lancet Neurol. 2014, 13, 167–177. [Google Scholar] [CrossRef] [Green Version]
- Van Sonderen, A.; Thijs, R.D.; Coenders, E.C.; Jiskoot, L.C.; Sanchez, E.; De Bruijn, M.A.; van Coevorden-Hameete, M.H.; Wirtz, P.W.; Schreurs, M.W.; Smitt, P.A.S.; et al. Anti-LGI1 encephalitis: Clinical syndrome and long-term follow-up. Neurology 2016, 84, 1449–1456. [Google Scholar] [CrossRef] [PubMed]
- Sen, A.; Wang, J.; Laue-Gizzi, H.; Lee, T.; Ghougassian, D.; Somerville, E.R. Pathognomonic seizures in limbic encephalitis associated with anti-LGI1 antibodies. Lancet 2014, 383, 2018. [Google Scholar] [CrossRef]
- Hansen, N.; Malchow, B.; Zerr, I.; Stöcker, W.; Wiltfang, J.; Timäus, C. Neural cell-surface and intracellular autoantibodies in patients with cognitive impairment from a memory clinic cohort. J. Neural Transm. 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hansen, N. Long-Term Memory Dysfunction in Limbic Encephalitis. Front. Neurol. 2019, 10, 1–5. [Google Scholar] [CrossRef] [PubMed]

| Reference | n Patients Included for Meta-Analysis | Anti-GAD | Neural Surface Autoantibodies | Onconeuronal | Level of Evidence |
|---|---|---|---|---|---|
| Ansari B. et al., 2019 [10] * | N = 33 Control group: No | IF (CBA) | IF (CBA): NDMAR, AMPAR, LGI1, CASPR2, GABAB, GlyR | IF (CBA) | 2− |
| Iorio R. et al., 2015 [11] | N = 42 Control group: N = 75 | RIA | IF (IHC). Confirmed by CBA NMDAR, AMPAR, LGI1, CASPR2, GABAB, | IF (IHC). Confirmed by immunoblot | 2+ |
| Brenner T. et al., 2013 [12] | N = 176 Control group: N = 148 | RIA | IF (CBA) NDMAR, LGI1, CASPR2, GLYR | - | 2+ |
| Liimatainen S. et al., 2010 [13] | N = 73 Control group: N = 200 | RIA. Confirmation by IF/immunoblot | - | - | 2++ |
| Teceilloglu M. et al., 2018 [14] | N = 77 Control group: No | IRMA | - | Immunoblot | 2+ |
| Gozubatik-Celik G. et al., 2017 [15] | N = 94 Control group: N = 50 | RIA | IF (CBA): NMDAR, AMPAR, LGI1, CASPR2, GABAB, | - | 2+ |
| Ekizoglu E. et al., 2014 [16] | N = 81 Control group: N = 30 | IPA | IF (CBA): NMDAR, AMPAR, LGI1, CASPR2, GlyR | - | 2++ |
| Falip M. et al., 2012 [17] | N = 23 Control group: No | IF (IHC) and RIA | - | - | 2+ |
| Dubey D. et al., 2017 [18] | N = 112 Control group: No | RIA | Method not specified: NMDAR, AMPAR, LGI1, GABAB | Method not specified | 2+ |
| de Bruijn MAAM et al., 2021 [19] | N = 582 Control group: No | IF (IHC). Confirmation by CBA and ELISA | IF (IHC). Confirmation and GlyR by CBA NMDAR, AMPAR, LGI1, CASPR2, GABAB, GABAA, GlyR | IF (IHC). Confirmation by immunoblot | 2++ |
| Li Y. et al., 2021 [20] | N = 42 Control group: No | IF (IHC or CBA). Confirmation by other techniques | IF (IHC or CBA). Confirmation by other techniques NMDAR, AMPAR, LGI1, CASPR2, GABAB | IF (IHC or CBA). Confirmation by other techniques | 2+ |
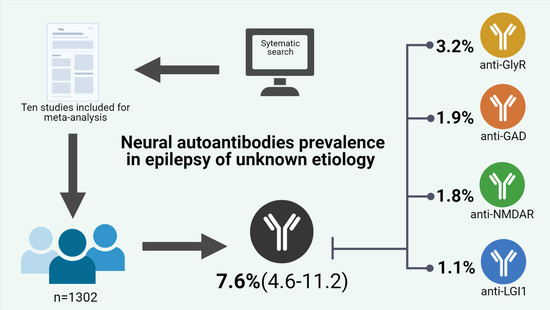
| Neural Autoantibody | n, Studies Determined | n, Subjects Determined | Pooled Prevalence | CI Lower | CI Upper | I-Squared | p-Value Egger’s Test | p-Value Begg’s Test |
|---|---|---|---|---|---|---|---|---|
| Total | 11 | 1302 | 7.6% | 4.6% | 11.2% | 75% | 0.11 | 0.58 |
| GlyR | 3 | 839 | 3.2% | 0.1% | 9.8% | 91% | 0.20 | 0.60 |
| GAD | 9 | 1260 | 1.9% | 0.6% | 3.8% | 70% | 0.76 | 0.14 |
| NMDAR | 7 | 1129 | 1.8% | 0.6% | 3.7% | 66% | 0.08 | 0.75 |
| LGI1 | 6 | 1087 | 1.0% | 0.2% | 2.7% | 68% | 0.36 | 0.09 |
| CASPR2 | 6 | 1017 | 0.6% | 0.2% | 1.3% | 47% | 0.65 | 0.22 |
| Onconeuronal | 5 | 855 | 0.2% | 0.1% | 0.8% | 38% | 0.10 | 0.78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabezudo-García, P.; Mena-Vázquez, N.; Ciano-Petersen, N.L.; García-Martín, G.; Estivill-Torrús, G.; Serrano-Castro, P.J. Prevalence of Neural Autoantibodies in Epilepsy of Unknown Etiology: Systematic Review and Meta-Analysis. Brain Sci. 2021, 11, 392. https://doi.org/10.3390/brainsci11030392
Cabezudo-García P, Mena-Vázquez N, Ciano-Petersen NL, García-Martín G, Estivill-Torrús G, Serrano-Castro PJ. Prevalence of Neural Autoantibodies in Epilepsy of Unknown Etiology: Systematic Review and Meta-Analysis. Brain Sciences. 2021; 11(3):392. https://doi.org/10.3390/brainsci11030392
Chicago/Turabian StyleCabezudo-García, Pablo, Natalia Mena-Vázquez, Nicolás L. Ciano-Petersen, Guillermina García-Martín, Guillermo Estivill-Torrús, and Pedro J. Serrano-Castro. 2021. "Prevalence of Neural Autoantibodies in Epilepsy of Unknown Etiology: Systematic Review and Meta-Analysis" Brain Sciences 11, no. 3: 392. https://doi.org/10.3390/brainsci11030392