Low-Frequency Noise and Its Main Effects on Human Health—A Review of the Literature between 2016 and 2019
Abstract
:1. Introduction
2. Materials and Methods
Database Collection
3. Results and Discussion
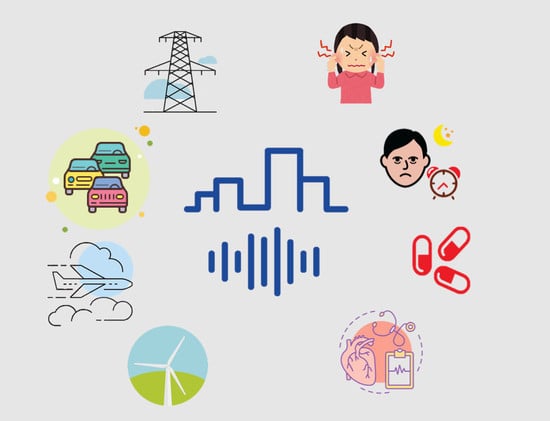
3.1. Low-Frequency Noise Exposure and Its Main Health Effects
3.2. Sleep Disturbance
3.3. Discomfort from, Sensitivity to, and Irritability from Noise
3.4. Annoyance
3.5. Hearing Loss
3.6. Cardiovascular Disease/Heart Rate
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Berglund, B.; Hassmén, P.; Job, R.F. Sources and effects of low-frequency noise. J. Acoust. Soc. Am. 1996, 99, 2985–3002. [Google Scholar] [CrossRef]
- Pawlaczyk-Łuszczyńska, M.; Dudarewicz, A.; Szymczak, W.; Sliwinska-Kowalska, M. Evaluation of annoyance from low frequency noise under laboratory conditions. Noise Health 2010, 12, 166–181. [Google Scholar] [CrossRef]
- Alves, J.A.; Silva, L.T.; Remoaldo, P.C. Impacts of low frequency noise exposure on well-being: A case-study from portugal. Noise Health 2018, 20, 131–145. [Google Scholar]
- Dart, E.E. Effects of high speed vibrating tools on operators engaged in airplane industry. Occup. Med. 1946, 1, 515–550. [Google Scholar]
- Rumancev, G.I. Investigations concerning the hygienic evaluation of vibration in factories producing reinforced concrete. Gig. Tr. Prof. Zabol 1961, 5, 6–12. [Google Scholar]
- Cohen, A. The influence of a company hearing conservation program on extra-auditory problems in workers. J. Saf. Res. 1976, 8, 146–162. [Google Scholar]
- Obata, J.; Morita, S.; Hirose, K.I.; Matsumoto, H. The effects of noise upon human efficiency. J. Acoust. Soc. Am. 1934, 5, 255–261. [Google Scholar] [CrossRef]
- Vasudevan, R.; Leventhall, H.G. Annoyance due to environmental low frequency noise and source location—A case study. J. Low Freq. Noise Vib. 1989, 8, 30–39. [Google Scholar] [CrossRef]
- Davis, A.C.; Lovell, E.A.; Smith, P.A.; Ferguson, M.A. The contribution of social noise to tinnitus in young people - a preliminary report. Noise Health 1998, 1, 40–46. [Google Scholar]
- Mirowska, M. An Investigation and Assessment of Annoyance of Low Frequency Noise in Dwellings. J. Low Freq. Noise Vib. 1998, 17, 119–126. [Google Scholar] [CrossRef]
- Rushforth, I.; Moorhouse, A.; Styles, P. A case study of low frequency noise assessed using DIN 45680 Criteria. J. Low Freq. Noise, Vib. Act. Control 2002, 21, 181–198. [Google Scholar] [CrossRef]
- Babisch, W.; Ising, H.; Gallacher, J.E.J.; Elwood, P.C. Traffic noise and cardiovascular risk: The Caerphilly study, first phase. Outdoor noise levels and risk factors. Arch. Environ. Health 1988, 43, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Bluhm, G.; Eriksson, C. Cardiovascular effects of environmental noise: Research in Sweden. Noise Health 2011, 13, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Lundquist, P.; Holmberg, K.; Landstrom, U. Annoyance and effects on work from environmental noise at school. Noise Health 2000, 2, 9–46. [Google Scholar]
- Mirowska, M. Evaluation of low frequency noise in dwellings. New Polish recommendations. J. Ofl Low Freq. Noise Vib. 2001, 20, 67–74. [Google Scholar] [CrossRef]
- Griefahn, B. Sleep disturbances related to environmental noise. Noise Health 2002, 4, 57–60. [Google Scholar]
- Rios, A.L.; Silva, G.A. Sleep quality in noise exposed Brazilian workers. Noise Health 2005, 7, 1–6. [Google Scholar]
- Murphy, E.; King, E.A. Scenario analysis and noise action planning: Modelling the impact of mitigation measures on population exposure. Appl. Acoust. 2011, 72, 487–494. [Google Scholar] [CrossRef]
- Schultz, T.J. Synthesis of social surveys on noise annoyance. J. Acoust. Soc. Am. 1978, 64, 377–405. [Google Scholar] [CrossRef] [Green Version]
- Paulsen, R.; Kastka, J. Effects of combined noise and vibration on annoynce. J. Sound Vib. 1995, 181, 295–314. [Google Scholar] [CrossRef]
- Karpova, N.I.; Alekseev, S.V.; Erokhin, V.N.; Kadyskina, E.N.; Reutov, O.V. Early response of the organism to low-frequency acoustical oscillations. Noise Vib. Bull. 1970, 11, 100–103. [Google Scholar]
- Silva, L.T.; Mendes, B.; Rodrigues, D.S.; Ribeiro, P.J.G.; Mendes, J.F.G. A Mobile Environmental Monitoring Station For Sustainable Cities. Int. J. Sustain. Dev. Plan. 2016, 11, 949–958. [Google Scholar] [CrossRef] [Green Version]
- Miedema, H.M.E.; Vos, H. Exposure-response relationships for transportation noise. J. Acoust. Soc. Am. 1998, 104, 3432–3445. [Google Scholar] [CrossRef]
- Babisch, W. Traffic noise and cardiovascular disease: Epidemiological review and synthesis. Noise Health 2000, 2, 9–32. [Google Scholar] [PubMed]
- Passchier-Vermeer, W.; Passchier, W.F. Noise Exposure and Public Health. Environ. Health Perspect. 2000, 108, 123–131. [Google Scholar] [PubMed] [Green Version]
- Ising, H.; Kruppa, B. Health effects caused by noise: Evidence in the literature from the past 25 years. Noise Health 2004, 6, 5–13. [Google Scholar]
- Bluhm, G.; Berglind, N.; Nordling, E.; Rosenlund, M. Road traffic noise and hypertension. Occup. Environ. Med. 2007, 64, 122–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavacas, M.A.; Tavares, V.; Oliveira, M.J.; Oliveira, P.; Sezinando, A.; Santos, J.M. Effects of industrial noise on circumpulpar dentin—A field emission scanning electron microscopy and energy dispersive spectroscopy analysis. Int. J. Clin. Exp. Pathol. 2013, 6, 2697–2702. [Google Scholar]
- Cavacas, M.A.; Tavares, V.; Borrecho, G.; Oliveira, M.J.; Oliveira, P.; Águas, A.; Santos, J.M. Industrial Noise and Tooth Wear – Experimental Study. Int. J. Med. Sci. 2015, 12, 3–8. [Google Scholar] [CrossRef] [Green Version]
- Waye, K.P.; Bengtsson, J.; Kjellberg, A.; Benton, S. Low frequency noise “pollution” interferes with performance. Noise Health 2001, 4, 33–49. [Google Scholar]
- Waye, K.P. On the Effects of Environmental Low Frequency Noise. Ph.D. Thesis, Goteborgs University, Gothenburg, Sweden, 1995. [Google Scholar]
- Pawlaczyk-Luszczyńska, M.; Szymczak, W.; Dudarewicz, A.; Sliwiñska-Kowalska, M. Proposed criteria for assessing low frequency noise annoyance in occupational settings. Int. J. Occup. Med. Environ. Health 2006, 19, 185–197. [Google Scholar] [CrossRef]
- Leventhall, H.G. Low frequency noise and annoyance. Noise Health 2004, 6, 59–72. [Google Scholar]
- Alves, J.A.; Silva, L.T.; Remoaldo, P.C. The influence of Low-frequency noise pollution on the quality of life and place in sustainable cities: A case study from Northern Portugal. Sustainability 2015, 7, 13920–13946. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Environmental Noise Guidelines for the European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2018. [Google Scholar]
- Laird, D.A. Experiments on the physiological cost of noise. J. Natl. Inst. Ind. Psychol. 1928, 4, 251–258. [Google Scholar]
- Vasudevan, R.N.; Gordon, C.G. Experimental study of annoyance due to low frequency environmental noise. Appl. Acoust. 1977, 10, 57–69. [Google Scholar] [CrossRef]
- Castelo Branco, N.A.A. A unique case of vibroacoustic disease. A tribute to an extraordinary patient. Aviat Space Env. Med. 1999, 70, A27–A31. [Google Scholar]
- Moorhouse, A.; Waddington, D.; Adams, M. Proposed Criteria for the Assessment of Low Frequency Noise Disturbance; DEFRA: University of Salford: Salford, UK, 2005. [Google Scholar]
- Van Kamp, I.; Breugelmans, O.; Van Poll, R.; Baliatsas, C.; Van Kempen, E. Determinants of annoyance from humming sound as indicator of low frequency noise. In Proceedings of ACOUSTICS 2017 Perth: Sound, Science and Society—2017 Annual Conference of the Australian Acoustical Society AAS, Perth, Australia, 19–22 November 2017; pp. 1–7. [Google Scholar]
- Abbasi, M.; Monazzam, M.R.; Zakerian, S.A.; Ebrahimi, M.H.; Dehghan, S.F.; Akbarzadeh, A. Assessment of noise effects of wind turbine on the general health of staff at wind farm of Manjil, Iran. J. Low Freq. Noise Vib. Act. Control. 2016, 35, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Morsing, J.A.; Smith, M.G.; Ögren, M.; Thorsson, P.; Pedersen, E.; Forssén, J.; Waye, K.P. Wind turbine noise and sleep: Pilot studies on the influence of noise characteristics. Int. J. Environ. Res. Public Health 2018, 15. [Google Scholar]
- Ishitake, T. Wind Turbine Noise and Health Effects. Nihon Eiseigaku Zasshi 2018, 73, 298–304. [Google Scholar] [CrossRef]
- Pohl, J.; Gabriel, J.; Hübner, G. Understanding stress effects of wind turbine noise—The integrated approach. Energy Policy 2018, 112, 119–128. [Google Scholar] [CrossRef]
- Poulsen, A.H.; Raaschou-Nielsen, O.; Peña, A.; Hahmann, A.N.; Nordsborg, R.B.; Ketzel, M.; Brandt, J.; Sørensen, M. Impact of Long-Term Exposure to Wind Turbine Noise on Redemption of Sleep Medication and Antidepressants: A Nationwide Cohort Study. Environ. Heal. Perspect. 2019, 127, 37005. [Google Scholar] [CrossRef] [PubMed]
- Blair, B.D.; Brindley, S.; Dinkeloo, E.; McKenzie, L.M.; Adgate, J.L. Residential noise from nearby oil and gas well construction and drilling. J. Expo. Sci. Environ. Epidemiol. 2018, 28, 538–547. [Google Scholar] [CrossRef]
- Smith, M.G.; Ögren, M.; Ageborg Morsing, J.; Persson Waye, K. Effects of ground-borne noise from railway tunnels on sleep: A polysomnographic study. Build. Environ. 2019, 149, 288–296. [Google Scholar] [CrossRef]
- Huang, B.; Pan, Z.; Liu, Z.; Hou, G.; Yang, H. Acoustic amenity analysis for high-rise building along urban expressway: Modeling traffic noise vertical propagation using neural networks. Transp. Res. Part. D Transp. Environ. 2017, 53, 63–77. [Google Scholar] [CrossRef]
- Suzuki, F.A.B.; Suzuki, F.A.; Onishi, E.T.; Penido, N.O. Psychoacoustic classification of persistent tinnitus. Braz. J. Otorhinolaryngol. 2018, 84, 583–590. [Google Scholar] [CrossRef]
- Lee, P.J.; Park, S.H.; Jeong, J.H.; Choung, T.; Kim, K.Y. Association between transportation noise and blood pressure in adults living in multi-storey residential buildings. Environ. Int. 2019, 132, 105101. [Google Scholar] [CrossRef] [PubMed]
- Tao, Z.; Wang, Y.; Zou, C.; Li, Q.; Luo, Y. Assessment of ventilation noise impact from metro depot with over-track platform structure on workers and nearby inhabitants. Environ. Sci. Pollut. Res. 2019, 26, 9203–9218. [Google Scholar] [CrossRef]
- Moradi, G.; Omidi, L.; Vosoughi, S.; Ebrahimi, H.; Alizadeh, A.; Alimohammadi, I. Effects of noise on selective attention: The role of introversion and extraversion. Appl. Acoust. 2019, 146, 213–217. [Google Scholar] [CrossRef]
- Alves, J.; Silva, L.T.; Remoaldo, P. How Can Low-Frequency Noise Exposure Interact with the Well-Being of a Population? Some Results from a Portuguese Municipality. Appl. Sci. 2019, 9, 5566. [Google Scholar] [CrossRef] [Green Version]
- Boyle, M.D.; Soneja, S.I.; Quirós-Alcalá, L.; Dalemarre, L.; Sapkota, A.R.; Sangaramoorthy, T.; Wilson, S.; Milton, D.; Sapkota, A. A pilot study to assess residential noise exposure near natural gas compressor stations. PLoS ONE 2017, 12, e0174310. [Google Scholar] [CrossRef]
- Hansen, K.L.; Nguyen, P.; Zajamšek, B.; Catcheside, P.; Hansen, C.H. Prevalence of wind farm amplitude modulation at long-range residential locations. J. Sound Vib. 2019, 455, 136–149. [Google Scholar] [CrossRef]
- Berglund, B.; Lindvall, T.; Schwela, D.H. Guidelines for Community Noise; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Hurtley, C. (Ed.) Night Noise Guidelines for Europe; WHO Regional Office Europe: Copenhagen, Denmark, 2009. [Google Scholar]
- Selander, J.; Albin, M.; Rosenhall, U.; Rylander, L.; Lewné, M.; Gustavsson, P. Maternal occupational exposure to noise during pregnancy and hearing dysfunction in children: A nationwide prospective cohort study in Sweden. Environ. Health Perspect. 2016, 124, 855–860. [Google Scholar] [CrossRef]
- Wang, V.-S.; Lo, E.-W.; Liang, C.-H.; Chao, K.-P.; Bao, B.-Y.; Chang, T.-Y. Temporal and spatial variations in road traffic noise for different frequency components in metropolitan Taichung, Taiwan. Environ. Pollut. 2016, 219, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Ohgami, N.; Oshino, R.; Ninomiya, H.; Li, X.; Kato, M. Impairments of Inner Ears Caused by Physical Environmental Stresses. Nihon Eiseigaku Zasshi. Jpn. J. Hyg. 2017, 72, 38–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venet, T.; Carreres-Pons, M.; Chalansonnet, M.; Thomas, A.; Merlen, L.; Nunge, H.; Bonfanti, E.; Cosnier, F.; Llorens, J.; Campo, P. Continuous exposure to low-frequency noise and carbon disulfide: Combined effects on hearing. NeuroToxicology 2017, 62, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Zhou, G.; Fu, W. Total serum bilirubin levels and sensorineural hearing loss in the US adolescents: NHANES 2007–2010. Int. J. Pediatric Otorhinolaryngol. 2018, 105, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Walker, E.D.; Brammer, A.; Cherniack, M.G.; Laden, F.; Cavallari, J.M. Cardiovascular and stress responses to short-term noise exposures—A panel study in healthy males. Environ. Res. 2016, 150, 391–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poulsen, A.H.; Raaschou-Nielsen, O.; Peña, A.; Hahmann, A.N.; Nordsborg, R.B.; Ketzel, M.; Brandt, J.; Sørensen, M. Long-Term Exposure to Wind Turbine Noise and Risk for Myocardial Infarction and Stroke: A Nationwide Cohort Study. Environ. Heal. Perspect. 2019, 2019, 37004. [Google Scholar] [CrossRef] [Green Version]
- Rossi, L.; Prato, A.; Lesina, L.; Schiavi, A. Effects of low-frequency noise on human cognitive performances in laboratory. Build. Acoust. 2018, 25, 17–33. [Google Scholar] [CrossRef]
- Zeitooni, M.; Mäki-Torkko, E.; Stenfelt, S. Binaural Hearing Ability with Bilateral Bone Conduction Stimulation in Subjects with Normal Hearing: Implications for Bone Conduction Hearing Aids. Ear Hear. 2016, 37, 690–702. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.S.; Young, L.H.; Yu, T.Y.; Bao, B.Y.; Chang, T.Y. Occupational noise frequencies and the incidence of hypertension in a retrospective cohort study. Am. J. Epidemiol. 2016, 184, 120–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vasilyeva, I.N.; Bespalov, V.G.; Semenov, A.L.; Baranenko, D.A.; Zinkin, V.N. The Effects of Low-Frequency Noise on Rats: Evidence of Chromosomal Aberrations in the Bone Marrow Cells and the Release of Low-Molecular-Weight DNA in the Blood Plasma. Noise Health 2017, 19, 79–83. [Google Scholar] [PubMed]
- Alimohammadi, I.; Ebrahimi, H. Comparison between effects of low and high frequency noise on mental performance. Appl. Acoust. 2017, 126, 131–135. [Google Scholar] [CrossRef]
- Mancera, K.F.; Lisle, A.; Allavena, R.; Phillips, C.J.C. The effects of mining machinery noise of different frequencies on the behaviour, faecal corticosterone and tissue morphology of wild mice (Mus musculus). Appl. Anim. Behav. Sci. 2017, 197, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Abbasi, A.M.; Motamedzade, M.; Aliabadi, M.; Golmohammadi, R.; Tapak, L. Study of the physiological and mental health effects caused by exposure to low-frequency noise in a simulated control room. Build. Acoust. 2018, 25, 233–248. [Google Scholar] [CrossRef]
- Ninomiya, H.; Ohgami, N.; Oshino, R.; Kato, M.; Ohgami, K.; Li, X.; Kato, M. Increased expression level of Hsp70 in the inner ears of mice by exposure to low frequency noise. Hear. Res. 2018, 363, 49–54. [Google Scholar] [CrossRef]
- Chalansonnet, M.; Carreres-Pons, M.; Venet, T.; Thomas, A.; Merlen, L.; Seidel, C.; Cosnier, F.; Nunge, H.; Pouyatos, B.; Llorens, J.; et al. Combined exposure to carbon disulfide and low-frequency noise reversibly affects vestibular function. NeuroToxicology 2018, 67, 270–278. [Google Scholar] [CrossRef]
- Min, J.Y.; Min, K. Cumulative exposure to nighttime environmental noise and the incidence of peptic ulcer. Environ. Int. 2018, 121, 1172–1178. [Google Scholar] [CrossRef]
- Wang, X.; Lai, Y.; Zhang, X.; Zhao, J. Effect of low-frequency but high-intensity noise exposure on swine brain blood barrier permeability and its mechanism of injury. Neuroscience Letters 2018, 662, 122–128. [Google Scholar] [CrossRef]
- Paunović, K.; Jakovljević, B.; Stojanov, V. The timeline of blood pressure changes and hemodynamic responses during an experimental noise exposure. Environ. Res. 2018, 163, 249–262. [Google Scholar] [CrossRef]
- Negishi-Oshino, R.; Ohgami, N.; He, T.; Li, X.; Kato, M.; Kobayashi, M.; Gu, Y.; Komuro, K.; Angelidis, C.E.; Kato, M. Heat shock protein 70 is a key molecule to rescue imbalance caused by low-frequency noise. Arch. Toxicol. 2019, 93, 3219–3228. [Google Scholar] [CrossRef] [PubMed]
- Scherer, R.W.; Formby, C. Effect of Tinnitus Retraining Therapy vs Standard of Care on Tinnitus-Related Quality of Life: A Randomized Clinical Trial. Jama Otolaryngol. Head Neck Surg. 2019, 145, 597–608. [Google Scholar] [PubMed]
- Phadke, K.V.; Abo-Hasseba, A.; Švec, J.G.; Geneid, A. Influence of Noise Resulting From the Location and Conditions of Classrooms and Schools in Upper Egypt on Teachers’ Voices. J. Voice 2019, 33, 802.e1–802.e9. [Google Scholar] [CrossRef] [PubMed]
- Zare, S.; Baneshi, M.R.; Hemmatjo, R.; Ahmadi, S.; Omidvar, M.; Dehaghi, B.F. The Effect of Occupational Noise Exposure on Serum Cortisol Concentration of Night-shift Industrial Workers: A Field Study. Saf. Health Work 2019, 10, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Licitra, G.; Fredianelli, L.; Petri, D.; Vigotti, M.A. Annoyance evaluation due to overall railway noise and vibration in Pisa urban areas. Sci. Total Environ. 2016, 568, 1315–1325. [Google Scholar] [CrossRef] [PubMed]
- Iannace, G.; Ciaburro, G.; Trematerra, A. Wind Turbine Noise Prediction Using Random Forest Regression. Machines 2019, 7, 69. [Google Scholar] [CrossRef] [Green Version]

| Year | Studies | Studies Evaluated | ||||
|---|---|---|---|---|---|---|
| Number of Participants/Sample | Main Human Health Effects | Methodology | Exposure | Outcomes | ||
| 2016 | Zeitooni, Mäki-Torkko and Stenfelt [66] | 27 | Binaural hearing capacity | Evaluation of binaural auditory capacity in adults with normal hearing when bone conduction stimulation is applied bilaterally in the bone conduction hearing aid implant position, as well as in the audiometric position in the mastoid. | Exposure to low-frequency noise (400 to 600 Hz) and high-frequency noise (3000 to 5000 Hz). | The results confirmed that the binaural auditory processing with bilateral bone conduction stimulation in the mastoid position is also present in the bone conduction hearing aid (BCHA) implant position. This indicates the capacity for binaural hearing in patients with good cochlear function when using bilateral BCHAs. |
| 2016 | Walker, Brammer, Cherniack, Laden and Cavallari [63] | 10 (male) | Heart rate variability and stress | The authors conducted a sound monitoring campaign between February 2015 and February 2016 across the city of Boston, MA. Boston occupies an area of 124 square kilometres with an estimated population of close to 700,000 individuals. To identify potential monitoring sites, the authors divided the city of Boston into 500 × 500 m grid cells using ArcGIS. They constructed a list of all accessible potential sites (n = 525), and 400 site locations were randomly selected for monitoring by time of day. Convenience sampling was also conducted in certain areas of the city to ensure adequate coverage of varied land use and urban activity. The participants underwent an outpatient electrocardiogram. Blood pressure measurements and saliva samples were collected before, during, and after exposure to noise. | Low-frequency noise (31.5 to 125 Hz at 75 dB (A)); high-frequency noise (500 to 2 kHz at 75 dB (A)); 50 dB (A) “noise-free” exposure. | During exposure to noise, reductions in heart rate variability of 19% (−35; −3.5) with low-frequency power and 9.1% (−17; −1.1) were observed according to the quadratic difference average between adjacent normal heartbeat intervals. During exposure to low-frequency noise, reductions in heart rate variability of 32% (- 57; −6.2) with high-frequency power, 34% (−52; −15) with low-frequency power and 16% (−26; - 6.1) according to the standard deviation of the adjacent normal heartbeat intervals. During exposure to high-frequency noise, reductions in heart rate variability of 21% (−39; −2.3) with low-frequency power compared to that with exposure to noise. |
| 2016 | Liu, Young, Yu, Bao and Chang [67] | 1002 | Hypertension and blood pressure | Personal noise measurements and environmental analysis of octave bands were carried out to divide workers into similar exposure groups based on the similarity and frequency of the tasks they performed in the company, thus creating a high exposure group (≥80 dBA), another of medium exposure (75–79 dBA), and another of low exposure (<75 dBA). | Noise at frequencies of 31.5 Hz, 63 Hz, 125 Hz, 250 Hz, 500 Hz, 1 kHz, 2 kHz, 4 kHz, and 8 kHz during the working period. | Participants exposed to ≥80 dBA for 8 years had a higher relative risk of hypertension (relative risk = 1.38, 95% confidence interval: 1.02, 1.85) than those exposed to <75 dBA. Significant exposure–response patterns were observed between incident hypertension and the stratum of exposure to noise at frequencies of 250 Hz, 1 kHz, 2 kHz, 4 kHz, and 8 kHz. The strongest effect was found at the frequency of 4 kHz, and a 20 dBA increase in noise exposure at 4 kHz was found to be associated with a 34% higher risk of hypertension (relative risk = 1.34, confidence interval of 95%: 1.01, 1.77). |
| 2016 | Selander et al. [58] | 1,422,333 | Hearing dysfunction in children due to noise during pregnancy | Occupational noise exposure during pregnancy, according to the prospective cohort study, FENIX (foetal noise exposure), based on births between 1986 and 2008. | Low-frequency noise (<75 dBA); high-frequency noise (≥85 dBA); medium-frequency noise (75–84 dBA). | In the sample, in a mixture of part-time and full-time workers during pregnancy, HR adjusted for hearing impairment associated with exposure to maternal occupational noise ≥85 vs. <75 dB LAeq, 8 h was 1.27 (95% CI: 0.99 1.64; 60 exposed cases). When restricted to children whose mothers worked full time and had less than 20 days of absence during pregnancy, the HR was 1.82 (95% CI: 1.08, 3.08; 14 exposed cases). |
| 2016 | Abbasi et al. [41] | 53 | General health; somatic symptoms; anxiety; insomnia; social dysfunction; depression | Study of the effect of wind turbine noise on the general health of employees at a wind farm, with workers divided into three groups: maintenance, security, and office workers. Equivalent sound levels were measured for each group. The individuals’ health data were assessed using a 28-item questionnaire. Pearson’s correlation, analysis of variance, and multiple regression tests were performed for data analysis using software. | In the maintenance team, an LAeq of 83 dBA was considered, an LAeq of 66 dBA was considered in the security team, and an LAeq of 60 dBA, in the administration team. | Exposure to noise is significantly correlated with all subscales of general health, except depression. The low-frequency noise from the turbines can cause harmful effects on the health of workers who are very close to the turbine and receive very intense noise. |
| 2016 | Wang et al. [59] | 2700 | Cardiovascular diseases; hearing loss. | The authors carried out the study in the metropolitan area of Taichung, Taiwan and set up 50 monitoring stations to collect related information on noise measurements, traffic flow rates, speed limits, and meteorological data. The 50 monitoring stations included 4 agricultural areas, 6 green-land areas (e.g., parks, forests, and mountains), 2 conservation areas, 8 culture-educational areas (i.e., schools, temples, and churches), 11 residential areas, 4 industrial areas, 1 stream-channel area (e.g., harbours), 7 commercial areas, 6 governmental areas (i.e., governmental agencies and institutes), and 1 recreational area. Determination of exposure to traffic noise by measuring the average equivalent noise levels A (LAeq, 24 h) in 50 monitoring stations (25 road traffic stations and 25 non-commercial ones) covering 10 different types of land use. | Equivalent continuous sound levels (Leq, 24 h) in the range of 30–130 dBA; noise levels with the time-weighted average (TWA) at frequencies of 31.5, 63, 125, 250, 500, 1000, 2000, 4000, and 8000 Hz. | The Leq annual average, 24 h in Taichung was 66.4 ± 4.7 dBA, exceeding the threshold for cardiovascular disease prevention. The mean annual Leq, 24 h in the flow and commercial channel areas was 71.2 ± 1.0 and 70.0 ± 2.6 dBA, respectively, revealing a potential risk of hearing loss among residents. The noise levels at 125 Hz had the highest correlation with total traffic and the highest forecast in multiple linear regression. |
| 2017 | Vasilyeva, Bespalov, Semenov, Baranenkoand Zinkin [68] | 96 rats | Frequency of chromosomal aberrations in bone marrow cells; levels of low molecular weight DNA (lmwDNA) in blood plasma. | Exposure to single or multiple LFN from male Wistar rats and their comparison with those in the control group. The control group rats were not subjected to any impact. Measurement of the frequency of chromosomal aberrations in bone marrow cells and the levels of lmwDNA in blood plasma. | Frequency below 250 Hz; simple LFN with sound pressure levels (SPL) of 120 dB; multiple LFN with 150 dB SPL. | Blood plasma lmwDNA levels measured the following day after a single exposure to LFN were significantly higher (7.7 and 7.6 times, respectively) than in the control group (11.0 ± 5.4 ng/mL), and these levels were higher (4.8 and 2.1 times, respectively) in the week after a single exposure of LFN to the SPL of 120 and 150 dB, respectively, than in the control group (18.8 ± 1.6 ng/mL). Similar results were obtained in the group with multiple exposures to LFN (36.4 and 22.4 times, respectively) compared to the control group (17.7 ± 1.7 ng/mL) and suggest an increase in cell apoptosis as a result of impact of the LFN. |
| 2017 | Boyle et al. [54] | 11 | Noise disturbance from natural gas compression stations. | Assessment of how A-weighted exposure levels differ indoors and outdoors in homes near the natural gas compressor station, where low-frequency noise was found. Measurement of noise levels defined in the A-weighted scale to filter out most of the low-frequency noise and in the C-weighted scale to identify the impulse noise. | - | Houses located close to a compressor station have higher average noise levels, both indoors and outdoors, than houses located more than 300 m away. Noise levels during the day were higher than at night. Residents of residences located less than 300 m from the station were exposed to low-frequency noise. The daytime and nighttime noise levels recommended for preventing hearing loss and annoyance were exceeded. |
| 2017 | Van Kamp, Breugelmans, Van Poll, Baliatsas and Van Kempen [40] | 3972 | Annoyance due to low-frequency noise | Survey of complaints due to low-frequency noise, based on analysis of existing data. Conducting a questionnaire with participants addressing aspects such as annoyance and sensitivity to noise, sources of emission, and residential satisfaction, among others. | - | The level of background noise, sensitivity to noise, and dissatisfaction with the residential situation were strongly associated with higher levels of annoyance. The lower the background noise levels, the greater the annoyance due to tinnitus. Low-frequency noise is particularly a problem in places with low levels of background noise. |
| 2017 | Ohgami, Oshino, Ninomiya, Li and Kato [60] | Rats | Hearing loss; imbalance | Conducting an experimental study in which wild type rats were exposed to similar low-frequency noise and the assessment of noise-induced hearing loss and determination of the rats’ imbalance. | Low-frequency noise (70 dB, 100 Hz) | The authors observed that a sound stimulation at 375 Hz at a frequency lower than the audible range of the rats causes a hearing reduction in wild type rats, and in rats with an abnormal otolytic morphology, this hearing loss was not observed. |
| 2017 | Venet et al. [61] | 117 rats | Effects on hearing | Evaluation of exposure to the combination of low-frequency noise and carbon disulfide. | Low-frequency noise, ranging from 0.5 to 2 kHz at an intensity of 106 dB SPL. | Exposure to CS2 (250 ppm or more) and noise increased the extent of the damaged frequency window, as a significant hearing deficit was measured at 9.6 kHz in these conditions; in addition, the significance at 9.6 kHz increased with solvent concentrations. Histological data showed that neither hair cells nor ganglion cells were damaged by CS2. |
| 2017 | Alimohammadi and Ebrahimi [69] | 89 | Mental performance | All participants underwent the Stroop and Cognitrone tests in silent conditions, after 30 min of exposure to LFN and HFN. The Cognitrone test assesses concentration and attention, and the Stroop interference test is a sensorimotor speed test that records the performance of reading speed. | Low-frequency and high-frequency noise at 50 and 70 dBA. | Both noises emitted (LFN and HFN) not only caused precision in scaling the response but also reduced the duration of the test run. It was concluded that, disregarding the distribution of energy frequencies, noise improved the task performance of participants. The results illustrated that individuals under LFN performed the Cognitrone test more quickly than individuals under HFN. |
| 2017 | Huang, Pan, Liu, Hou and Yang [48] | - | Noise disturbance | Analysis of acoustic comfort and development of a noise analysis model for a skyscraper, through the measurement of exterior noise, mainly road traffic noise. The selection of measuring points was made on the horizontal and vertical planes and strictly follows the guidelines (Chinese standard JTG B03–206 and HJ 2.4-2009). The noise measurement instruments were an AWA6270+B noise analyser, AWA6228 frequency analyser, and TES1350A sound level meter. | - | A higher capacity to respond to high-frequency than low-frequency mining noise (LF) was observed, which probably reflects the audibility of the two frequency spectra. |
| 2017 | Mancera, Lisle, Allavena and Phillips [70] | 57 rats | Effects on behaviour (stress), organ morphology, and faecal corticosterone. | Evaluation of the effects of noise from mining machines on the behaviour and physiological parameters (organ morphology and faecal corticosterone) of wild rats, when subjected to high- and low-frequency ranges, and comparison with a reference treatment without auditory stimuli. | High-frequency noise (>2 kHz); low-frequency noise (≤2 kHz). | The frequencies below and above 2 kHz had differential effects on male and female wild rats that can have important consequences for their well-being and survival. |
| 2018 | Morsing et al. [42] | 12 | Sleep effects | Evaluation of sleep effects, through polysomnography measurement and questionnaires, in 2 pilot studies, due to noise exposure from wind turbines. Six participants spent five consecutive nights in an ambient sound laboratory and, for three nights, were exposed to the noise of the wind turbine with the variation of some parameters. | High-frequency (>125 Hz) and low-frequency noise (125 Hz). Similar to a ventilation noise, a low background noise (18 dB LAeq) was used. | During nights with noise from the wind turbine, there were sleep disturbances compared to during control nights. Deeper sleep was negatively affected by higher rotational frequency and amplitude modulation, but light sleep increased with high rotational frequency and acoustic beat. |
| 2018 | Blair, Brindley, Dinkeloo, McKenzie and Adgate [46] | 4 (residences) | Annoyance, sleep disorders, and cardiovascular effects | Determination of noise levels in a well block of oil and gas operations of several wells during construction and drilling in a residential area in Colorado and the verification of impacts on human health. A (dBA) and C (dBC) weighted noise measurements were collected at four residences located between 320 (1049.9 ft) and 550 m (1804.5 ft) from the site during development over a three-month period (February to April 2017). | A and C weighted noise levels of 60.2 dBA and 80 dBC, respectively. | Proportionally, 41.1% of continuous daytime equivalent daytime measurements and 23.6% of 1 min dBA exceeded 50 dBA, and 97.5% of daytime and 98.3% of nighttime measurements exceeded 60 dBC. Average noise levels in an oil and gas well during construction and drilling exceed levels associated with annoyances, sleep disturbances, and cardiovascular health effects (greater than 50 dBA or 60 dBC) in studies involving noise sources such as traffic, airports, wind turbines, and rail-related noise pollution. |
| 2018 | A.M. Abbasi, Motamedzade, Aliabadi, Golmohammadi andTapak [71] | 35 | Physiological effects and mental health (fatigue) | Participants were exposed to low-frequency noise and were ultimately asked to determine their level of mental fatigue. A cognitive test was performed to assess working memory (low, medium, or high workload). Software was used to assess mental fatigue, visual fatigue analogue scale, and psychophysiological indexes. | Low-frequency noise levels of 55, 65, 70, and 74 dBA. | The results showed that mental fatigue significantly affected heart rate, low- to high-frequency rates, and electroencephalogram rates. The results confirmed that the mental fatigue caused by low-frequency noise significantly impacted the participants’ psychophysiological and working memory with exposure to noise levels of 65 to 75 dBA. |
| 2018 | Ninomiya et al. [72] | 44 rats | Stress | A comparison of auditory levels and levels of expression of the Hsp70 protein in the cochlea was performed between rats exposed and not exposed to LFN. | Low-frequency noise (100 Hz to 95 dB). | The results showed that the inner ear may be one of the organs negatively affected by the stress caused by the inaudible exposure to LFN. Exposure to LFN increases the level of Hsp70 expression via Cebpb in the inner ear. The levels of Hsp70 and Cebpb may be candidates for biomarkers of responses to exposure to LFN. |
| 2018 | Rossi, Prato, Lesina and Schiavi [65] | 25 (19 to 29 years) | Physiological effects (response time and heart rate) | The experiment involved 25 Italian volunteers (12 female and 13 male volunteers), aged 19–29 years. Before starting the test, each subject filled in a general questionnaire specifying age, occupation, musical experience, eyesight and hearing problems, and the presence of noise in their daily life. Measurement of changes in cognitive and physiological parameters in a sample of volunteers exposed to three types of noise in a hemi-anechoic room. Participants were involved in a cognitive task (Stroop effect) for 10 min in four different conditions: silence, multi-tonal broadband (BBN) stochastic noise, low and low-frequency stochastic noise (LFN1), and low-frequency stationary noise with regular amplitude modulation (LFN2). | Sounds reproduced with a sound pressure level equivalent to 93 dB; BBN noise based on frequencies between 315 and 2000 Hz; LFN1 with frequencies between 30 and 60 Hz; LFN2 with frequencies between 30 and 200 Hz. | In noise conditions, participants reduced their response times, that is, there was evidence of increasing stress. Dividing the participants into extroverts and introverts, it was demonstrated that LFN1 and LFN2 produced higher stress effects than BBN noise on cognitive performance and a physiological stress comparable to that produced by BBN noise. |
| 2018 | Zhou and Fu [62] | 1404 | Sensorineural hearing loss (SNHL); excess bilirubin (causes problems in the liver, spleen, kidneys, gallbladder). | Measurements of total serum bilirubin, tympanometry, and determination of the mean threshold of pure tones at low frequencies or high frequencies for a subset of adolescents, to assess levels of total serious bilirubin associated with different subtypes of sensorineural hearing loss. | Low-frequency noise (LPTA: 500, 1000, 2000 Hz); high-frequency noise (HPTA: 3000, 4000, 6000, and 8000 Hz). | Total serum bilirubin levels were associated with any high-frequency SNHL (HPTA > 15 dB in at least one ear) in adolescents in the USA; high-frequency SNHL with HPTA > 15 dB in both ears (bilateral) or with HPTA ≥ 25 dB in at least one ear had a stronger association with total serum bilirubin levels than HPTA > 15 dB in only one ear (unilateral) or HPTA = 15–25 dB in at least one ear. |
| 2018 | Ishitake [43] | 9000 (≥20 years) | Annoyance; sleep disorders | Conducting an environmental epidemiological study and assessing the effects on sleep disturbance due to low-frequency noise generated by wind power installations, based on residents living in areas close to the source. Assessment of sleep disorders using the Athens Insomnia Scale. Assessment of environmental noise in residential areas (50 community centres) close to the noise source by measuring infrared and low-frequency sound exposure levels. | Infrared, low-frequency (20 Hz) and infrasound (<20 Hz). | As for sleep disturbances caused by infrasound (20 Hz or less), the noise level of the wind turbine measured in the ultra-low-frequency range is below the human sensory threshold. Of the participants, 63% heard the noise when the distance was less than 1000 m. However, the hearing rate decreased significantly when the distance was increased to 5000 m, when only 2% of the participants heard the noise. Based on the Athens Insomnia Scale, 40% of participants had sleep disorders when the distance was less than 1000 m. However, the frequency of sleep disorders decreased to 22% with an increase in distance. Amplitude-modulated sounds and pure tones contained in the noise generated by wind power generation facilities tend to increase annoyance. |
| 2018 | Chalansonnet et al. [73] | 133 rats | Balance effects | Study of how exposure to low-frequency noise combined with 250 ppm CS2 affects rat balance. Vestibular function was tested based on post-rotational nystagmus recorded by a video-oculography system. These measurements were completed by behavioural tests and cerebellar analysis to measure levels of gene expression associated with neurotoxicity. | Low-frequency noise, ranging from 0.5 to 2 kHz at an intensity of 106 dB SPL. | Coexposure to CS-250 ppm and low-frequency noise reduced the number and duration of the withdrawals by 33% and 34%, respectively. It was observed that the effects of CS2 were due to reversible neurochemical disorders of the efferent pathways that manage post-rotational nystagmus. Since the nervous structures that involve vestibular function seem particularly sensitive to CS2, post-rotational nystagmus can be used as an early non-invasive measure to diagnose CS2 poisoning as part of an occupational conservation programme. |
| 2018 | Min and Min [74] | 466,822 (217,308 with gastric ulcer + 249,514 with duodenal ulcer) | Peptic ulcer (gastric and duodenal) | Investigation of the incidence of peptic ulcers in adults due to long-term exposure to environmental noise. The diagnosis of gastric and duodenal ulcers was made during an 8-year follow-up (2006–2013). Environmental noise data were obtained from the National Noise Information System, a national noise monitoring system. | The interquartile range (IQR) for nighttime noise exposure was 2.37 dB for gastric ulcers and 2.41 dB for duodenal ulcers. | Gastric ulcers occurred in 32.1% of individuals, and duodenal ulcers, in 10.7% of individuals. The diagnostic rate for gastric and duodenal ulcers increased with increasing cumulative mean levels of nighttime ambient noise. With increases in the IQR of nighttime noise, the risk rate increased significantly by 12% for gastric ulcers and 17% for duodenal ulcers, based on the fully adjusted model. |
| 2018 | Pohl, Gabriel and Hübner [44] | 212 (1st phase) and 133 (2nd phase) | General mental indisposition; reduced performance and work capacity; lack of concentration; fatigue; voltage; nervousness; dizziness; irritability; indisposition; reduced sleep quality; annoyance | A total of 212 persons participated in the first survey; nearly two-thirds (133 persons) remained in the second. Accordingly, a third dropped out (“dropouts”; 79 participants). Indeed, dropouts differed statistically from the other participants only in terms of education level and household size. The remaining participants had higher education levels and slightly larger households compared to the dropouts (small effect size for each). These socio-demographic variables had no significant influence on the central stress and attitude indicators; significant differences in the central attitude and annoyance assessments were not apparent. Longitudinal study, based on the methodology of stress psychology with noise measurements, in which residents of a wind farm in Lower Saxony were interviewed on two occasions (2012, 2014), using audio equipment to record irritating noises. Several residents complained of physical and psychological symptoms due to traffic noise (16%) and wind turbine noise (10%; two years later, 7%), which allowed the assessment of some symptoms caused by noise exposure. | Noise from low-frequency wind turbines (<100 Hz). | Participants reported more symptoms in 2012 than in 2014. From 2012 to 2014, sleep disorders decreased and symptoms of impaired performance were not repeated. Only a few participants showed evidence of low-frequency (<100 Hz) wind turbine (WT) noise effects: in 2012, 8.5% reported feelings of pressure related to wind farms and 6.1% experienced vibrations in the body. The annoyance experienced induced by feelings of pressure or vibrations was slightly greater in 2012. Symptoms of dizziness were not observed. The participants had more symptoms and greater irritation due to traffic noise than to wind noise. |
| 2018 | X. Wang, Lai, Zhang and Zhao [75] | 6 (3 exposed, 3 unexposed) Bama pigs | Effects on the blood–brain barrier (BBB) | Investigation of the effect of noise exposure on the blood–brain barrier (BBB). Healthy male Bama pigs were randomly divided into a noise exposure group and a control group (no noise) for 30 min. After exposure, brain imaging was performed using computed tomography and fluorescent images. | Low-frequency noise (50, 70, 100, and 120 Hz at 140 dB). | The BBB permeability test showed that 50, 70, and 100 Hz noise exposure at 140 dB increased the BBB permeability, and the BBB opening at 70 Hz was more severe and reversible. Tomographic images demonstrated that noise-induced opening of the BBB did not cause intracerebral haemorrhage. |
| 2018 | Suzuki, Suzuki, Onishi and Penido [49] | 110 | Tinnitus and LFN discomfort | Classification of persistent tinnitus and its comparison with pure tone or noise, high or low pitch, presented to the patient by the sounds of the audiometer. Participants were subject to inclusion and exclusion criteria. The following evaluations were performed on patients: otorhinolaryngological, audiological, Pitch Matching and Loudness, Visual Analogue Scale, Tinnitus Handicap Inventory, and Minimum Masking Level. | Three types of noise: white noise (WN), narrow band low frequency (LFNB) at 500 Hz, and narrow band high frequency (HFNB) at 6000 Hz. | A total of 181 tinnitus complaints were identified, in which the presence of pure tone type tinnitus was observed in 93 (51%) of the responses (4 from low pitch and 89 from high pitch) and from noise in 88 (49%) of the responses (15 low frequency and 73 high). For tinnitus with low-frequency sensation, 19 responses were determined, while for high-frequency sensation, 162 responses were determined. Visual Analogue Scale average of 5.47 for tinnitus similar to pure tone, and 6.66 for that similar to noise. Average Loudness for tinnitus similar to the pure tone of 12.31 dBNS, and for that similar to the noise of 10.54 dBNS. |
| 2018 | Paunović, Jakovljević and Stojanov [76] | 112 (82 women and 30 men, aged 19 to 32). | Blood pressure; haemodynamic events | Study divided into three 10-min phases: resting in quiet conditions before noise, exposure to traffic noise, and resting in quiet conditions after noise. Measurement of blood pressure, heart rate, and haemodynamic parameters (cardiac index and total peripheral resistance) with a chest bioimpedance device. Use of four statistical models to answer the study questions. | Exposure to noise: resting in quiet conditions before noise (Leq = 40 dBA); exposure to noise registered in traffic (Leq = 89 dBA); resting in quiet conditions after noise (Leq = 40 dBA). | Blood pressure decreased during the quiet phase before noise, increased in the first minute of exposure to noise, then gradually decreased at the end of exposure to noise, and continued to decrease to baseline values after exposure to noise. The cardiac index showed a gradual decrease throughout the experiment, while the total vascular resistance increased steadily during and after exposure to noise. |
| 2019 | Negishi-Oshino et al. [77] | Rats | Irreversible imbalance with structural damage to the otoconial membrane | Assessment of rats’ imbalance due to acute exposure to LFN. The exposed rats also showed decreased cervical vestibular evoked myogenic potential (cVEMP) with impaired vestibular hair cell activity. | LFN with a frequency of 100 Hz at 85, 90, or 95 dB. | The results of this study demonstrate that acute exposure to LFN at 100 Hz at 95 dB for just 1 h caused irreversible imbalance in rats with structural damage to the otoconial membrane, as the target region for the LFN-mediated imbalance, which could be rescued by Hsp70. |
| 2019 | Lee, Park, Jeong, Choung and Kim [50] | 400 | Discomfort and sensitivity to noise; blood pressure; annoyance due to noise | The study recruited healthy residents aged between 20 and 60 years. Effects of exposure to transport noise on blood pressure in adult residents of multi-storey residential buildings, modification of the effects of discomfort from and sensitivity to internal noise, and self-assessed associations between transport noise and blood pressure. Measurement of noise levels at the top of buildings for 24 h, forecasting the levels of each unit in the house for different sources and periods using noise maps. Conducting adjusted linear regression analyses to estimate associations between noise exposure levels and systolic blood pressure (SBP) and diastolic blood pressure (DBP). Conducting a questionnaire with questions about annoyance from and sensitivity to noise and sociodemographic variables. | Exposure to noise (Lden, LDay, and LNight). | General noise (road traffic and rail noise) and road traffic showed stronger associations with SBP than with DBP, while rail noise had similar associations with SBP and DBP. Stronger associations were estimated for participants who reported higher ratings of annoyance by internal noise. The results support the hypothesis that long-term exposure to transport noise is associated with higher blood pressure in adults living in multi-storey residential buildings. |
| 2019 | Scherer and Formby [78] | 151 | Tinnitus retraining therapy (TRT); sound therapy (ST); tinnitus-specific educational counselling (TC) | Comparison of the effectiveness of TRT and its components, ST and CT, with the standards of care (SoC) in reducing the negative effect of tinnitus on quality of life. Study carried out in 6 military hospitals, in the office and in a data coordination centre, among active, retired, and dependent military personnel with functionally adequate hearing sensitivity and moderate to severe subjective tinnitus, with the objective of treating the military. | LFN (tinnitus). | There were few differences between treatment groups. About half of the participants showed clinically significant reductions in the effect of tinnitus. |
| 2019 | Poulsen et al. [45] | Residences between 20 and 40 inhabitants | Annoyance; sleep disorders; depression | Evaluation of the evolution of medical prescriptions related to anxiolytics and antidepressants ingested by the populations that lived near the wind turbines, in an analysis that lasted two years (2012 to 2014). A total of 7256 wind turnines (WT) was considered in noise modelling. The authors collected information on model, type, height, and operational settings. Each WT was classified into to one of 99 noise spectra classes, with detailed information on the noise spectrum from 10–10,000 Hz in thirds of octaves for wind speeds of 4–25 m/s. | Exposure to outdoor wind turbine noise (WTN) at night (<24, 24 to <30, 30 to <36, 36 to <42, and ≥42 dB) and nighttime low frequency indoor WTN (<5, 5 to <10.10 and <15, and ≥15 dB). | High levels of outdoors WTN associated with use of anxiolytics and antidepressants among the elderly, suggesting that WTN may be potentially associated with sleep and mental health. |
| 2019 | Tao, Wang, Zou, Li and Luo [51] | 100 | Irritation and sensitivity to noise | Assessment of noise irritation in the metro deposit and the influence of noise in adjacent residential buildings. Conducting a questionnaire with people who worked at the metro station and made field measurements, both at the metro station and in the adjacent residential buildings. | LFN and HFN (31.5, 63, 125, 250, 500, 1000, 2000, 4000, 8000, and 16,000 Hz) | Of respondents, 96% are disturbed by the noise and 31% of them feel that the impact of the noise is serious. They found that there is a problem of annoyance due to low-frequency noise. The authors evaluated that the noise level caused by the fans decreases with the height of the floors and that the shorter the distance between the building’s fans and ventilation, the more severe the impact of the noise. They concluded that, with the increase in the distance to the noise source, the noise attenuation rate increases. |
| 2019 | Poulsen et al. [64] | 717.453 | Myocardial infarction (MI), stroke | The authors used the Danish Civil Registration System to identify the study cohort, defined as all adults (aged 25–84 years) who lived in one of these inclusion dwellings any time between five years before the erection of the first neighbouring WT and the end of 2013. Assessment of the impact of MI and stroke risk when there is long-term exposure to noise from wind turbines. Based on hospital and mortality records, an analysis was made of the number of cases of myocardial infarction and stroke that existed in homes located around wind turbines. | Exposure to wind turbine noise (WTN) at night outdoors (≥24 dB) and nighttime low frequency indoor WTN (≥5 dB; 10–160 Hz) | High long-term exposure to noise from wind turbines is associated with an increase in myocardial infarction and strokes. |
| 2019 | Hansen, Nguyen, Zajamšek, Catcheside and Hansen [55] | 9 (residences) A total of 8716 and 8972 10 min samples of outdoor and indoor data | Annoyance | The outdoor measurements carried out at 9 different residences located between 1 and 9 km from the nearest wind turbine of a South Australian wind farm (37 operational turbines), each with a rated power of 3 MW. The wind farm is positioned along the top of a ridge, and the wind turbine hub height relative to the residences varies between 85 and 240 m. At all residences, the indoor measurements were taken in a room that faced as closely as possible towards the wind farm and the windows were closed. The presence of amplitude modulation in the noise of wind farms results in increased annoyance and possible interruptions in sleep. The study investigated the prevalence of this characteristic present in homes close to the wind farm. | - | During the night, audible amplitude modulation occurred in homes located 3.5 km from the wind farm up to 22% of the time. This had important implications for possible sleep disruptions and annoyance due to the wind farm by audible amplitude modelling, particularly as ambient noise levels in rural South Australia can be as low as 15 and 5 dBA, outdoors and in closed areas, respectively. |
| 2019 | Phadke, Abo-Hasseba, Švec and Geneid [79] | 140 (between 21 and 56 years) | Voice disorders: dysphonia; neck pain; vocal effort | This study aimed to identify possible correlations between the vocal symptoms of teachers and their perception of noise, the locations of schools, as well as the locations and conditions of their classrooms. They carried out a questionnaire, whose answers were analysed statistically, with questions about the severity and frequency of their voice symptoms, noise perception, and the locations and conditions of their schools and classrooms. | - | Teachers experienced severe dysphonia, neck pain, and increased vocal effort with weekly or daily recurrence. Among the teachers who participated in the study, 24.2% felt that they were always in a noisy environment, with 51.4% of the total participants reporting having to raise their voices. The most common sources of noise were student activities and conversations in the teachers’ own classrooms (61.4%), noise from adjacent classrooms (52.9%), and road traffic (40.7%). |
| 2019 | Smith, Ögren, Ageborg Morsing and Persson Waye [47] | 23 | Disorders in physiological sleep; heart rate | The study volunteers slept for five nights in a sound environment laboratory, which was furnished like a typical apartment. The participants were instructed to start trying to fall asleep at 23:00 each evening and were woken with an alarm call at 07:00 each morning. Sleeping at times outside of this 8 h period was not permitted. Participants could follow their normal daytime routine but arrived at the laboratory by 20:00 each evening to allow time for relaxation and the setup of the sleep-measuring equipment. Caffeine was prohibited after 15:00 each day, and alcohol was prohibited at all times. Evaluation of the effects on physiological sleep resulting from the exposure of participants to railway noise for five consecutive nights, using polysomnography and questionnaires. Heart rate was measured by electrocardiography. | Frequencies of 35, 40, and 45 dB. | No significant differences were found in the overall structure of sleep disorders between the reference tests and the 35 dB night tests. Regarding cardiovascular diseases, they observed that the noise spectrum with amplitude frequencies greater than 100 Hz led to increases in heart rate for noise levels equal to or greater than 35 dB. |
| 2019 | Zare et al. [80] | 75 | Serum cortisol concentration | The study aimed to examine the effect of sound pressure level (SPL) on the serum concentration of cortisol at three different times during the night shift, in an industrial and mining company. Participants were divided into three groups (one control and two groups of cases, with 25 each). Dosimetry was adopted to evaluate SPL equivalents using a TES-1345 dosimeter. The serum cortisol concentration was measured using a radioimmunoassay (RIA) test in the laboratory. | Exposure levels of 67, 80, and 92 dB. | The results indicated a downward trend in the serum cortisol concentration of the three groups during the night shift. SPL and exposure time significantly affected cortisol concentration. Age and body mass index had no significant influence on the concentration of cortisol. It was concluded that an increase in SPL leads to an increase in serum cortisol concentration. |
| 2019 | Moradi et al. [52] | 28 (14 females and 14 males) | Stress; noise sensitivity; annoyance | The study was conducted on students at different levels of educational programmes in an acoustic room in the School of Public Health, Iran University of Medical Sciences, in 2016. The study subjects were comprised of 14 female and 14 male university students who met the following entrance criteria: normal sense of hearing (hearing loss less than 20 dB) and no sensitivity to noise. Study of the effects of noise on selective attention of university students. They carried out questionnaires to determine students’ personality traits (extroverted or introverted) and analyse their stability or instability. Evaluation of the level of sensitivity to noise, using the Weinstein sensitivity scale, and the level of selective attention, using the DUAF test. | 80 dBA noise at 4000 Hz frequency | Introverted participants are more sensitive to noise than extroverts. The most noise-sensitive participants showed greater stimulation during exposure to noise, which led to increases in incorrect responses and a decrease in mental performance. The participants’ personal traits are related to their annoyance due to noise. Stress due to noise improves selective attention in outgoing individuals. |
| 2019 | Alves, Silva and Remoaldo [53] | 200 questionnaires + 62 measurements of noise levels + 14 adapted audiometric tests | Annoyance from LFN; audibility threshold | Analysis of the effects of exposure to low-frequency noise pollution, emitted by poles and power lines, on the well-being of the population, based on a study of “exposed” and “unexposed” individuals in two areas. Conducting audiometric tests adapted to complement the analysis and determine the audibility threshold of the volunteers. Sound level measurement and sound recording (at a distance of 5 m from the source), as well as the adapted audiometric performance test. | Frequency range between 10 and 160 Hz | The “exposed” area has higher sound levels and, consequently, more welfare and health problems than the “unexposed” population. Audiometric tests also revealed that the “exposed” population appears to be less sensitive to low frequencies than the “unexposed” population. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araújo Alves, J.; Neto Paiva, F.; Torres Silva, L.; Remoaldo, P. Low-Frequency Noise and Its Main Effects on Human Health—A Review of the Literature between 2016 and 2019. Appl. Sci. 2020, 10, 5205. https://doi.org/10.3390/app10155205
Araújo Alves J, Neto Paiva F, Torres Silva L, Remoaldo P. Low-Frequency Noise and Its Main Effects on Human Health—A Review of the Literature between 2016 and 2019. Applied Sciences. 2020; 10(15):5205. https://doi.org/10.3390/app10155205
Chicago/Turabian StyleAraújo Alves, Juliana, Filipa Neto Paiva, Lígia Torres Silva, and Paula Remoaldo. 2020. "Low-Frequency Noise and Its Main Effects on Human Health—A Review of the Literature between 2016 and 2019" Applied Sciences 10, no. 15: 5205. https://doi.org/10.3390/app10155205