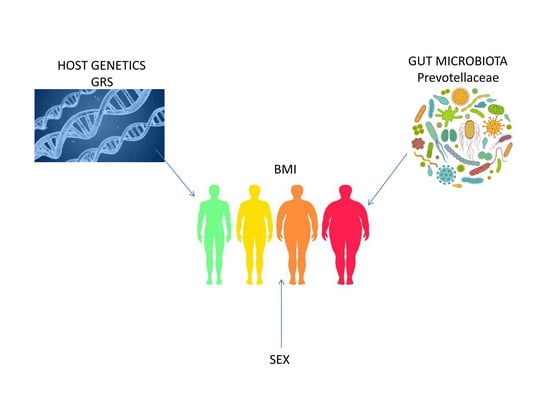
Sex-Specific Associations between Gut Prevotellaceae and Host Genetics on Adiposity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Anthropometric Measurements
2.3. Habitual Dietary Intake and Physical Activity
2.4. Biochemical Measurements
2.5. Fecal Sample Collection and Metagenomic Data
2.6. SNP Selection and Genotyping
2.7. Genetic Risk Score (GRS)
2.8. Statistical Analyses
3. Results
3.1. Baseline Characteristics of the Study Population
3.2. Genetic Risk Score (GRS)
3.3. Relationship between BMI, GRS and Gut Microbiome.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mcallister, E.J.; Dhurandhar, N.V.; Keith, S.W.; Aronne, L.J.; Barger, J.; Baskin, M.; Benca, R.M.; Biggio, J.; Boggiano, M.M.; Eisenmann, J.C.; et al. Ten Putative Contributors to the Obesity Epidemic. Crit. Rev. Food Sci. Nutr. 2009, 49, 868–913. [Google Scholar] [CrossRef] [Green Version]
- Kelly, T.; Yang, W.; Chen, C.S.; Reynolds, K.; He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ley, R.E.; Backhed, F.; Turnbaugh, P.; Lozupone, C.A.; Knight, R.D.; Gordon, J.I. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA 2005, 102, 11070–11075. [Google Scholar] [CrossRef] [Green Version]
- Speliotes, E.K.; Willer, C.J.; Berndt, S.I.; Monda, K.L.; Thorleifsson, G.; Jackson, A.U.; Lango-Allen, H.; Lindgren, C.M.; Luan, J.; Mägi, R.; et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat. Genet. 2010, 42, 937–948. [Google Scholar] [CrossRef] [Green Version]
- Xia, Q.; Grant, S.F. The genetics of human obesity. Ann. N. Y. Acad. Sci. 2013, 1281, 178–190. [Google Scholar] [CrossRef]
- Tims, S.; Derom, C.; Jonkers, D.M.; Vlietinck, R.; Saris, W.H.; Kleerebezem, M.; de Vos, W.M.; Zoetendal, E.G. Microbiota conservation and BMI signatures in adult monozygotic twins. ISME J. 2013, 7, 707–717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yatsumenko, T.; Rey, F.E.; Manary, M.J.; Trehan, I.; Dominguez-Bello, M.G.; Contreras, M.; Magria, M.; Hidalgo, G.; Baldassano, R.N.; Anokhin, A.P.; et al. Human gut microbiome viewed across age and geography. Clin. Exp. Rheumatol. 2010, 28, 222–227. [Google Scholar]
- Cani, P.D.; Bibiloni, R.; Knauf, C.; Neyrinck, A.M.; Delzenne, N.M. Changes in gut microbiota control metabolic diet–induced obesity and diabetes in mice. Diabetes 2008, 57, 1470–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vijay-kumar, M.; Aitken, J.D.; Carvalho, F.A.; Cullender, T.C.; Mwangi, S.; Srinivasa, S.; Sitaraman, S.V.; Knight, R.; Ley, R.E.; Gewirtz, A.T. Metabolic Syndrome and Altered Gut Microbiota in Mice Lacking Toll-Like Receptor 5. Science 2010, 328, 228–231. [Google Scholar] [CrossRef] [Green Version]
- Goodrich, J.K.; Davenport, E.R.; Beaumont, M.; Jackson, M.A.; Knight, R.; Ober, C.; Spector, T.D.; Bell, J.T.; Clark, A.G.; Ley, R.E. Genetic Determinants of the Gut Microbiome in UK Twins Genus Heritability. Cell Host Microbe. 2016, 19, 731–743. [Google Scholar] [CrossRef] [Green Version]
- Bonder, M.J.; Kurilshikov, A.; Tigchelaar, E.F.; Mujagic, Z.; Imhann, F.; Vila, A.V.; Deelen, P.; Vatanen, T.; Schirmer, M.; Smeekens, S.P.; et al. The effect of host genetics on the gut microbiome. Nat. Genet. 2016, 48, 1407–1412. [Google Scholar] [CrossRef]
- Davenport, E.R.; Cusanovich, D.A.; Michelini, K.; Barreiro, L.B.; Ober, C.; Gilad, Y. Genome-wide association studies of the human gut microbiota. PLoS ONE 2015, 10, 1–22. [Google Scholar] [CrossRef]
- Santos-Marcos, J.A.; Haro, C.; Vega-Rojas, A.; Alcala-Diaz, J.F.; Molina-Abril, H.; Leon-Acuña, A.; Lopez-Moreno, J.; Landa, B.B.; Tena-Sempere, M.; Perez-Martinez, P.; et al. Sex differences in the gut microbiota as potential determinants of gender predisposition to disease. Mol. Nutr. Food Res. 2019, 63, 1800870. [Google Scholar] [CrossRef] [PubMed]
- Dominianni, C.; Sinha, R.; Goedert, J.J.; Pei, Z.; Yang, L.; Hayes, R.B.; Ahn, J. Sex, body mass index, and dietary fiber intake influence the human gut microbiome. PLoS ONE 2015, 10, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haro, C.; Rangel-Zúñiga, O.A.; Alcalá-díaz, J.F.; Gómez-Delgado, F.; Pérez-Martínez, P.; Delgado-Lista, J.; Quintana-Navarro, G.M.; Landa, B.B.; Navas-Cortés, J.A.; Tena-Sempere, M.; et al. Intestinal Microbiota Is Influenced by Gender and Body Mass Index. PLoS ONE 2016, 11, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, C.; Yin, A.; Li, H.; Wang, R.; Wu, G.; Shen, J.; Zhang, M.; Wang, L.; Hou, Y.; Ouyang, H.; et al. Dietary Modulation of Gut Microbiota Contributes to Alleviation of Both Genetic and Simple Obesity in Children. EBioMedicine 2015, 2, 968–984. [Google Scholar] [CrossRef] [PubMed]
- Bashiardes, S.; Godneva, A.; Elinav, E.; Segal, E. Towards utilization of the human genome and microbiome for personalized nutrition. Curr. Opin. Biotechnol. 2018, 51, 57–63. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. Clin. R Educ. 2013, 310, 2191–2194. [Google Scholar]
- Lopez-Legarrea, P.; de la Iglesia, R.; Abete, I.; Bondia-Pons, I.; Navas-Carretero, S.; Forga, L.; Martínez, J.A.; Zulet, M.A. Short-term role of the dietary total antioxidant capacity in two hypocaloric regimes on obese with metabolic syndrome symptoms: The RESMENA randomized controlled trial. Nutr. Metab. 2013, 10, 22. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Obesity and Overweight criteria. WHO 2016. Available online: https://www.who.int/features/factfiles/obesity/facts/es/ (accessed on 26 May 2020).
- Whitworth, J.A.; Chalmers, J. World Health Organisation-International Society of Hypertension (WHO/ISH) hypertension guidelines. Clin. Exp. Hypertens. 2004, 26, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Martin-moreno, J.M.; Boyle, P.; Gorgojo, L.; Maisonneuve, P.; Fernandez-Rodriguez, J.C.; Salvini, S.; Willett, W.C. Development and Validation of a Food Frequency Questionnaire in Spain. Int. J. Epidemiol. 1993, 22, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Moreiras, O.; Carbajal, A.; Cabrera, L.; Cuadrado, C. Tablas De Composicion De Alimentos, 16th ed.; Ediciones Piramide: Madrid, Spain, 2009; p. 296. [Google Scholar]
- Martínez-González, M.A.; López-Fontana, C.; Varo, J.J.; Sánchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005, 8, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Basterra-Gortari, F.J.; Bes-Rastrollo, M.; Pardo-Fernández, M.; Forga, L.; Martinez, J.A.; Martínez-González, M.A. Changes in weight and physical activity over two years in spanish alumni. Med. Sci. Sports Exerc. 2009, 41, 516–522. [Google Scholar] [CrossRef] [Green Version]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, Whithout Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Hildebrand, F.; Tadeo, R.; Voigt, A.Y.; Bork, P.; Raes, J. LotuS: An efficient and user-friendly OTU processing pipeline. Microbiome 2014, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Edgar, R.C. UPARSE: Highly accurate OTU sequences from microbial amplicon reads. Nat. Methods 2013, 10. [Google Scholar] [CrossRef]
- Edgar, R.C. UCHIME2: Improved chimera prediction for amplicon sequencing. bioRxiv 2016. [Google Scholar] [CrossRef] [Green Version]
- Rideout, J.R.; He, Y.; Navas-Molina, J.A.; Walters, W.A.; Ursell, L.K.; Gibbons, S.M.; Chase, J.; McDonald, D.; Gonzalez, A.; Robbins-Pianka, A.; et al. Subsampled open-reference clustering creates consistent, comprehensive OTU definitions and scales to billions of sequences. PeerJ 2014, 2, 545. [Google Scholar] [CrossRef] [Green Version]
- Ritari, J.; Salojärvi, J.; Lahti, L.; de Vos, W.M. Improved taxonomic assignment of human intestinal 16S rRNA sequences by a dedicated reference database. BMC Genom. 2015, 16, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMurdie, P.J.; Holmes, S. Phyloseq: An R Package for Reproducible Interactive Analysis and Graphics of Microbiome Census Data. PLoS ONE 2013, 8, e61217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gentleman, R.C.; Carey, V.J.; Bates, D.M.; Bolstad, B.; Dettling, M.; Dudoit, S.; Ellis, B.; Gautier, L.; Ge, Y.; Gentry, J.; et al. Bioconductor: Open software development for computational biology and bioinformatics. Genome Biol. 2004, 10, R80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goni, L.; Cuervo, M.; Milagro, I.; Martinez, J.A. Future Perspectives of Personalized Weight Loss Interventions Based on Nutrigenetic. J. Nutr. 2016, 146, 905S–912S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramos-Lopez, O.; Milagro, F.I.; Allayee, H.; Chmurzynska, A.; Choi, M.S.; Curi, R.; De Caterina, R.; Ferguson, L.R.; Goni, L.; Kang, J.X.; et al. Guide for current nutrigenetic, nutrigenomic, and nutriepigenetic approaches for precision nutrition involving the prevention and management of chronic diseases associated with obesity. J. Nutrigenet. Nutrigenom. 2017, 10, 43–62. [Google Scholar] [CrossRef]
- Goni, L.; Milagro, F.I.; Cuervo, M.; Martínez, J.A. Single-nucleotide polymorphisms and DNA methylation markers associated with central obesity and regulation of body weight. Nutr. Rev. 2014, 72, 673–690. [Google Scholar] [CrossRef]
- Heianza, Y.; Qi, L. Gene-diet interaction and precision nutrition in obesity. Int. J. Mol. Sci. 2017, 18. [Google Scholar] [CrossRef] [Green Version]
- Guo, F.; Zhou, Y.; Song, H.; Zhao, J.; Shen, H.; Zhao, B.; Liu, F.; Jiang, X. Forensic Science International: Genetics Next generation sequencing of SNPs using the HID-Ion AmpliSeq TM Identity Panel on the Ion Torrent PGM TM platform. Forensic Sci. Int. Genet. 2016, 25, 73–84. [Google Scholar] [CrossRef]
- Ramos-Lopez, O.; Riezu-Boj, J.I.; Milagro, F.I.; Goni, L.; Cuervo, M.; Martinez, J.A. Association of the Gly482Ser PPARGC1A gene variant with different cholesterol outcomes in response to two energy-restricted diets in subjects with excessive weight. Nutrition 2018, 47, 83–89. [Google Scholar] [CrossRef]
- Ramos-lopez, O.; Riezu-boj, J.I.; Milagro, F.I.; Goni, L.; Cuervo, M.; Martinez, J.A. Nutrition, Metabolism & Cardiovascular Diseases Differential lipid metabolism outcomes associated with ADRB2 gene polymorphisms in response to two dietary interventions in overweight / obese subjects. Nutr. Metab. Cardiovasc. Dis. 2017, 28, 165–172. [Google Scholar]
- Ramos-Lopez, O.; Cuervo, M.; Goni, L.; Milagro, F.I.; Riezu-Boj, J.I.; Martinez, J.A. Modeling of an integrative prototype based on genetic, phenotypic, and environmental information for personalized prescription of energy-restricted diets in overweight/obese subjects. Am. J. Clin. Nutr. 2020, 111, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Ramos-lopez, O.; Riezu-boj, J.I.; Milagro, F.I.; Cuervo, M.; Goni, L.; Martinez, J.A. Interplay of an Obesity-Based Genetic Risk Score with Dietary and Endocrine Factors on Insulin Resistance. Nutrients 2019, 12, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sing, T.; Sander, O.; Beerenwinkel, N.; Lengauer, T. ROCR: Visualizing classifier performance in R. Bioinformatics 2005, 20, 3940–3941. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.D. The gut microbiome and its role in obesity. Nutr. Today 2014, 4, 139–148. [Google Scholar] [CrossRef] [Green Version]
- Falony, G.; Joossens, M.; Vieira-Silva, S.; Wang, J.; Darzi, Y.; Faust, K.; Kurilshikov, A.; Bonder, M.J.; Valles-Colomer, M.; Vandeputte, D.; et al. Population-level analysis of gut microbiome variation. Science 2016, 352, 560–564. [Google Scholar] [CrossRef]
- Farooqi, I.S.; Rahilly, S.O. Genetic factors in human obesity. Obes. Rev. 2007, 8, 37–40. [Google Scholar] [CrossRef]
- Hills, R.D.; Pontefract, B.A.; Mishcon, H.R.; Black, C.A.; Sutton, S.C.; Theberge, C.R. Gut Microbiome: Profound Implications for Diet and Disease. Nutrients 2019, 11, 1613. [Google Scholar] [CrossRef] [Green Version]
- Wright, S.M.; Aronne, L.J. Causes of obesity. Abdom. Imaging 2012, 37, 730–732. [Google Scholar] [CrossRef]
- Goodarzi, M.O. Genetics of obesity: What genetic association studies have taught us about the biology of obesity and its complications. Lancet Diabetes Endocrinol. 2018, 6, 223–236. [Google Scholar] [CrossRef]
- Erez, G.; Tirosh, A.; Rudich, A.; Meiner, V.; Schwarzfuchs, D.; Sharon, N.; Shpitzen, S.; Blüher, M.; Stumvoll, M.; Thiery, J.; et al. Phenotypic and genetic variation in leptin as determinants of weight regain. Int. J. Obes. 2011, 35, 785–792. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Wu, J.; Yu, L. Association of Gln27Glu and Arg16Gly Polymorphisms in Beta2-Adrenergic Receptor Gene with Obesity Susceptibility: A Meta-Analysis. PLoS ONE 2014, 9, e100489. [Google Scholar] [CrossRef] [PubMed]
- Soenen, S.; Mariman, E.C.; Vogels, N.; Bouwman, F.G.; den Hoed, M.; Brown, L.; Westerterp-Platenga, M.S. Physiology & Behavior Relationship between perilipin gene polymorphisms and body weight and body composition during weight loss and weight maintenance. Physiol. Behav. 2009, 96, 723–728. [Google Scholar] [PubMed]
- Mirzaei, K.; Xu, M.; Qi, Q.; de Jonge, L.; Bray, G.A.; Sacks, F.; Qi, L.; Trial, L. Variants in glucose- and circadian rhythm – related genes affect the response of energy expenditure to weight-loss diets: The POUNDS LOST Trial. Am. J. Clin. Nutr. 2014, 392–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fogelholm, M.; Valve, R.; Kukkonen-Harjula, K.; Uusitupa, M. Additive Effects of the Mutations in the 3 -Adrenergic Receptor and Uncoupling Protein-1 Genes on Weight Loss and Weight Maintenance in Finnish Women. J. Clin. Endocrinol. Metab. 1998, 83, 4246–4250. [Google Scholar]
- Haupt, A.; Thamer, C.; Heni, M.; Ketterer, C.; Machann, J.; Schick, F.; Machicao, F.; Stefan, N.; Claussen, D.; Haring, H.U.; et al. Gene Variants of TCF7L2 Influence Weight Loss and Body Composition During Lifestyle Intervention in a Population at Risk for Type 2 Diabetes. Diabetes 2010, 59, 747–750. [Google Scholar] [CrossRef] [Green Version]
- Dasgupta, S.; Salman, M.; Siddalingaiah, L.B.; Lakshmi, G.L.; Xaviour, D.; Sreenath, J. Genetic variants in leptin: Determinants of obesity and leptin levels in South Indian population. Adipocyte 2015, 4, 135–140. [Google Scholar] [CrossRef] [Green Version]
- Xu, M.; Qi, Q.; Liang, J.; Bray, G.A.; Hu, F.B.; Sacks, F.M.; Qi, L. Genetic determinant for amino acid metabolites and changes in body weight and insulin resistance in response to weight-loss diets: The Preventig Overweight Using Novel Dietary Stretegies (POUNDS LOST) trial. Circulation 2014, 127, 1283–1289. [Google Scholar] [CrossRef] [Green Version]
- Cha, M.H.; Shin, H.D.; Kim, K.S.; Lee, B.H.; Yoon, Y. The effects of uncoupling protein 3 haplotypes on obesity phenotypes and very low-energy diet – induced changes among overweight Korean female subjects. Metabolism 2006, 55, 578–586. [Google Scholar] [CrossRef]
- Janssens, A.C.; Aulchenko, Y.S.; Elefante, S.; Borsboom, G.J.; Steyerberg, E.W.; van Dujin, C.M. Predictive testing for complex diseases using multiple genes: Fact or fiction? Genet. Med. 2006, 8, 395–400. [Google Scholar] [CrossRef] [Green Version]
- Moonesinghe, R.; Liu, T.; Khoury, M.J. Evaluation of the discriminative accuracy of genomic profiling in the prediction of common complex diseases. Eur. J. Hum. Genet. 2010, 18, 485–489. [Google Scholar] [CrossRef]
- Goni, L.; Cuervo, M.; Milagro, F.I.; Martínez, J.A. A genetic risk tool for obesity predisposition assessment and personalized nutrition implementation based on macronutrient intake. Genes Nutr. 2015, 1, 445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hung, C.F.; Breen, G.; Czamara, D.; Corre, T.; Wolf, C.; Kloiber, S.; Bergmann, S.; Craddock, N.; Gill, M.; Holsboer, F.; et al. A genetic risk score combining 32 SNPs is associated with body mass index and improves obesity prediction in people with major depressive disorder. BMC Med. 2015, 13, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harakeh, S.M.; Khan, I.; Kumosani, T.; Barbour, E.; Almasaudi, S.B.; Bahijri, S.M.; Alfadul, S.M.; Ajabnoor, G.M.A.; Azhar, E.I. Gut Microbiota: A Contributing Factor to Obesity. Front. Cell. Infect. Microbiol. 2016, 6, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, H.; Park, S.; Jang, H.B.; Choi, M.; Park, K.H.; Kang, J.H.; Park, S.I.; Lee, H.J.; Seung-Hak, C. Obesity Alters the Microbial Community Profile in Korean Adolescents. PLoS ONE 2015, 10, e0138015. [Google Scholar] [CrossRef] [Green Version]
- Verdam, F.J.; Fuentes, S.; de Jonge, C.; Zoetendal, E.G.; Erbil, R.; Greve, J.W.; Burrman, W.A.; de Vos, W.M.; Rensen, S.S. Human Intestinal Microbiota Composition Is Associated with Local and Systemic Inflammation in Obesity. Obesity 2013, 21, 607–615. [Google Scholar] [CrossRef]
- Feng, J.; Tang, H.; Li, M.; Pang, X.; Wang, L.; Zhang, M.; Zhao, X.; Shen, J. The abundance of fecal Faecalibacterium prausnitzii in relation to obesity and gender in Chinese adults. Arch. Microbiol. 2014, 196, 73–77. [Google Scholar] [CrossRef]
- Delzenne, N.M.; Cani, P.D. Interaction Between Obesity and the Gut Microbiota: Relevance in Nutrition. Annu. Rev. Nutr. 2011, 31, 15–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serena, C.; Ceperuelo-Mallafré, V.; Keiran, N.; Queipo-Ortuño, M.I.; Bernal, R.; Gomez-Huelgas, R.; Urpi-Sarda, M.; Sabater, M.; Pérez-Brocal, V.; Andrés-Lacueva, C.; et al. Elevated circulating levels of succinate in human obesity are linked to specific gut microbiota. ISME J. 2018, 12, 1642–1657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, E.E.; Lozupone, C.A.; Rey, F.E.; Wu, M.; Guruge, J.L.; Narra, A.; Goodfellow, J.; Zaneveld, J.R.; McDonald, D.T.; Goodrich, J.A.; et al. Pan-genome of the dominant human gut-associated archaeon, Methanobrevibacter smithii, studied in twins. Proc. Natl. Acad. Sci. USA 2011, 108, 4599–4606. [Google Scholar] [CrossRef] [Green Version]
- Frank, D.N.; Robertson, C.E.; Hamm, C.M.; Zegbeh, K.; Zhang, T.; Chen, H.; Zhu, W.; Sartor, R.B.; Boedeker, E.C.; Harpaz, N.; et al. Disease phenotype and genotype are associated with shifts in Inflamm Bowel Diseases. Inflamm Bowel Dis. 2011, 17, 1–12. [Google Scholar] [CrossRef]
- Rausch, P.; Rehman, A.; Künzel, S.; Häsler, R.; Ott, S.J.; Schreiber, S.; Rosenstiel, P.; Franke, A.; Baines, J.F. Colonic mucosa-associated microbiota is influenced by an interaction of Crohn disease and FUT2 (Secretor) genotype. Proc. Natl. Acad. Sci. USA 2011, 108, 19030–19035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehman, A.; Sina, C.; Gavrilova, O.N.; Häsler, R.; Stephan, J.O.; Baines, J.F.; Schreiber, S.; Rosenstiel, P. Nod2 is essential for temporal development of intestinal microbial communities. Gut 2011, 60, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Goodrich, J.K.; Waters, J.L.; Poole, A.C.; Sutter, J.L.; Koren, O.; Blekhman, R.; Beaumont, M.; Van Treuren, W.; Knight, R.; Bell, J.T.; et al. Human genetics shape the gut microbiome. Cell 2014, 159, 789–799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Org, E.; Parks, B.W.; Joo, J.W.J.; Emert, B.; Schwartzman, W.; Kang, E.Y.; Mehrabian, M.; Pan, C.; Knight, R.; Gunsalus, R.; et al. Genetic and environmental control of host-gut microbiota interactions. Genome Res. 2015, 25, 1558–1569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- León-Mimila, P.; Villamil-Ramírez, H.; López-Contreras, B.E.; Morán-Ramos, S.; Macias-Kauffer, L.R.; Acuña-Alonzo, V.; Del Rio-Navarro, B.E.; Salmerón, J.; Velazquez-Cruz, R.; Villareal-Molina, T.; et al. Low Salivary Amylase Gene (AMY1) Copy Number Is Associated with Obesity and Gut Prevotella Abundance in Mexican Children and Adults. Nutrients 2018, 10, 1607. [Google Scholar] [CrossRef] [Green Version]
- Hall, A.B.; Tolonen, A.C.; Xavier, R.J. Human genetic variation and the gut microbiome in disease. Nat. Publ. Gr. 2017, 18, 690–699. [Google Scholar] [CrossRef]
- Wang, J.; Thingholm, L.B.; Skiecevičienė, J.; Rausch, P.; Kummen, M.; Hov, J.R.; Degenhardt, F.; Heinsen, F.A.; Rühlemann, M.C.; Szymczak, S.; et al. Genome-wide association analysis identifies variation in vitamin D receptor and other host factors influencing the gut microbiota. Nat. Genet. 2017, 48, 1396–1406. [Google Scholar] [CrossRef]
- Kolde, R.; Franzosa, E.A.; Rahnavard, G.; Brantley, A.; Vlamakis, H.; Stevens, C.; Daly, M.J.; Xavier, R.J.; Huttenhower, C. Host genetic variation and its microbiome interactions within the Human Microbiome Project. Genome Med. 2018, 10, 1–13. [Google Scholar] [CrossRef]
- Li, J.; Fu, R.; Yang, Y.; Horz, H.P.; Guan, Y.; Lu, Y.; Lou, H.; Tian, L.; Zheng, S.; Liu, H.; et al. A metagenomic approach to dissect the genetic composition of enterotypes in Han Chinese and two Muslim groups. Syst. Appl. Microbiol. 2018, 41, 1–12. [Google Scholar] [CrossRef]
- Rothschild, D.; Weissbrod, O.; Barkan, E.; Kurilshikov, A.; Korem, T.; Zeevi, D.; Costea, P.I.; Godneva, A.; Kalka, I.N.; Bar, N. Environment dominates over host genetics in shaping human gut microbiota. Nature 2018, 555, 210–215. [Google Scholar] [CrossRef]
- Li, M.; Wang, B.; Zhang, M.; Rantalainen, M.; Wang, S.; Zhou, H.; Zhang, Y.; Shen, J.; Pang, X.; Zhang, M. Symbiotic gut microbes modulate human metabolic phenotypes. Proc. Natl. Acad. Sci. USA 2008, 105, 2117–2122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borgo, F.; Garbossa, S.; Riva, A.; Severgnini, M.; Luigiano, C.; Benelti, A.; Pontiroli, A.E.; Morace, G.; Borghi, E. Body mass index and sex affect diverse microbial niches within the gut. Front. Microbiol. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, X.; Zhang, M.; Xue, J.; Huang, J.; Zhuang, R.; Zhou, X.; Zhang, H.; Fu, Q.; Hao, Y. Body mass index differences in the gut microbiota are gender specific. Front. Microbiol. 2018, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]






| Variables | All Population (n = 360) | BMI < 24.9 kg/m2 Women (n = 46) | BMI < 24.9 kg/m2 Men (n = 18) | p Value a | BMI > 25 kg/m2 Women (n = 205) | BMI ≥ 25 kg/m2 Men (n = 91) | p Value b |
|---|---|---|---|---|---|---|---|
| Age (y) | 44.8 ± 0.5 | 39.1 ± 1.3 | 41.5 ± 2.5 | 0.751 | 45.8 ± 0.7 | 46.3 ± 1.0 | 0.628 |
| Weight (kg) | 83.1 ± 0.8 | 57.8 ± 0.9 | 71.9 ± 1.9 | <0.001 | 83.6 ± 0.8 | 97.1 ± 1.2 | <0.001 |
| BMI (kg/m2) | 29.9 ± 0.2 | 21.7 ± 0.3 | 23.0 ± 0.3 | 0.009 | 31.6 ± 0.3 | 31.7 ± 0.3 | 0.694 |
| Waist circumference (cm) | 97.4 ± 0.8 | 73.1 ± 0.9 | 82.1 ± 1.4 | <0.001 | 99.5 ± 0.7 | 108.1 ± 0.9 | <0.001 |
| Hip circumference (cm) | 108.7 ± 0.6 | 94.3 ± 0.9 | 95.5 ± 1.2 | 0.497 | 113.4 ± 0.6 | 107.9 ± 0.7 | <0.001 |
| VAT (kg) | 1.3 ± 0.1 | 0.2 ± 0.03 | 0.4 ± 0.08 | 0.001 | 1.1± 0.04 | 2.3 ± 0.9 | <0.001 |
| SBP (mmHg) | 122 ± 1 | 104 ± 3 | 119 ± 3 | <0.001 | 122 ± 1 | 132 ± 3 | <0.001 |
| DBP (mmHg) | 76 ± 1 | 66 ± 1.9 | 73 ± 2.3 | 0.044 | 76 ± 1 | 80 ± 2 | 0.001 |
| Glucose (mg/dL) | 95 ± 1 | 83 ± 0.9 | 90 ± 1.3 | <0.001 | 95 ± 1 | 100 ± 1 | <0.001 |
| Total cholesterol (mg/dL) | 212 ± 2 | 191± 5.4 | 199 ± 6.2 | 0.381 | 215 ± 3 | 219 ± 4 | 0.407 |
| HDL-c (mg/dL) | 57 ± 1 | 64 ± 1.6 | 58 ± 2.6 | 0.052 | 59 ± 1 | 47 ± 1 | <0.001 |
| LDL-c (mg/dL) | 136 ± 2 | 113 ± 5 | 127 ± 6 | 0.035 | 137 ± 2 | 147 ± 4 | 0.018 |
| Triglycerides (mg/dL) | 98 ± 3 | 68 ± 5.5 | 68 ± 5.1 | 0.555 | 94 ± 3 | 125 ± 8 | <0.001 |
| ALT (U/L) | 22.6 ± 0.7 | 13 ± 0.4 | 24 ± 4.3 | <0.001 | 21 ± 1 | 31 ± 1 | <0.001 |
| AST (U/L) | 21.8 ± 0.4 | 18 ± 0.6 | 26 ± 1.6 | <0.001 | 21 ± 1 | 25 ± 1 | <0.001 |
| Uric acid (mg/dL) | 5.1 ± 0.1 | 3.9 ± 0.1 | 5.3 ± 0.2 | <0.001 | 4.7 ± 0.1 | 6.0 ± 0.1 | <0.001 |
| Adiponectin (µg/mL) | 11.9 ± 0.3 | 15.4 ± 0.7 | 9.6 ± 0.7 | <0.001 | 12.8 ± 0.4 | 8.4 ± 0.3 | <0.001 |
| Insulin (mU/L) | 7.1 ± 0.2 | 4.7 ± 0.3 | 3.5 ± 0.5 | 0.007 | 8.0 ± 0.3 | 8.7 ± 0.5 | 0.254 |
| Leptin (ng/mL) | 31.0 ± 1.6 | 14.2 ± 1.2 | 2.6 ± 0.3 | <0.001 | 48.1 ± 1.9 | 14.6 ± 0.9 | <0.001 |
| CRP (µg/mL) | 2.6 ± 0.2 | 1.5 ± 0.8 | 0.7 ± 0.4 | 0.519 | 2.1 ±0.2 | 3.2 ± 0.2 | 0.003 |
| TSH (mIU/L) | 1.3 ± 0.5 | 1.4 ± 0.1 | 1.3 ± 0.1 | 0.692 | 1.4 ± 0.1 | 1.2 ± 0.1 | 0.192 |
| TNFα (pg/mL) | 0.9 ± 0.1 | 0.8 ± 0.1 | 0.9 ± 0.1 | 0.221 | 1.0 ± 0.03 | 1.0 ± 0.03 | 0.258 |
| HOMA-IR | 1.7 ± 0.1 | 0.9 ± 0.1 | 0.8 ± 0.1 | 0.038 | 1.8 ± 0.1 | 2.2 ± 0.2 | 0.036 |
| Carbohydrate intake (%) | 41.1 ± 0.4 | 43.0 ± 1.0 | 44.9 ± 1.2 | 0.296 | 40.8 ± 0.5 | 40.4 ± 0.8 | 0.928 |
| Protein intake (%) | 16.9 ± 0.2 | 17.2 ± 0.4 | 15.7 ± 0.7 | 0.087 | 17.4 ± 0.2 | 16.0 ± 0.3 | <0.001 |
| Fat intake (%) | 40.1 ± 0.3 | 38.3 ± 0.9 | 37.5 ± 1.1 | 0.598 | 40.6 ± 0.4 | 40.1± 0.6 | 0.461 |
| Energy intake (kcal) | 2907 ± 48 | 2560 ± 106.2 | 2779 ± 149.9 | 0.271 | 2849 ± 63 | 3237 ± 104 | <0.001 |
| Physical activity (METs) | 25.3 ± 1.1 | 25.7 ± 2.8 | 47.8 ± 6.8 | 0.002 | 20.7 ± 1.2 | 30.9 ± 2.6 | <0.001 |
| SNP | Non-Risk Genotype | Risk Genotype | Non-Risk Group (n) | Risk Group (n) | Non-Risk Group Women BMI (kg/m2) | Non-Risk Group Men BMI (kg/m2) | Risk Group Women BMI (kg/m2) | Risk Group Men BMI (kg/m2) | p Value a | p Value b |
|---|---|---|---|---|---|---|---|---|---|---|
| rs4731426_LEP | GC | GG+CC | 168 | 191 | 29.0 ± 0.5 | 29.5 ± 0.6 | 30.4 ± 0.4 | 31.0 ± 0.6 | 0.032 | 0.069 |
| rs1800006_UCP3 | AG | GG+AA | 111 | 248 | 28.5 ± 0.5 | 29.8 ± 0.8 | 30.3 ± 0.4 | 30.4 ± 0.5 | 0.008 | 0.959 |
| rs1052700_PLIN1 | TT | AA+TA | 46 | 313 | 28.2±0.9 | 28.8 ± 1.2 | 30.0 ± 0.3 | 30.5 ± 0.4 | 0.089 | 0.096 |
| rs1042713_ADRB2 | AA+AG | GG | 230 | 129 | 29.5 ± 0.4 | 29.6 ± 0.5 | 30.3 ± 0.5 | 31.3 ± 0.7 | 0.217 | 0.034 |
| rs11605924_CRY2 | CC | AA+AC | 104 | 255 | 28.7 ± 0.6 | 29.8 ± 0.7 | 30.2 ± 0.4 | 30.4 ± 0.5 | 0.024 | 0.455 |
| rs1800592_UCP1 | CC+CT | CT | 246 | 113 | 29.3 ± 0.4 | 30.1 ± 0.5 | 30.7 ± 0.5 | 30.6 ± 0.8 | 0.092 | 0.321 |
| rs2734827_UCP3 | GG | AA+AG | 147 | 212 | 29.1 ± 0.4 | 30.1 ± 0.6 | 30.3 ± 0.4 | 30.3 ± 0.5 | 0.039 | 0.714 |
| rs1440581_PPM1K | CC | TT+TC | 78 | 281 | 28.7 ± 0.8 | 29.6 ± 0.8 | 30.1 ± 0.4 | 30.4 ± 0.5 | 0.122 | 0.410 |
| rs7799039_LEP | GA | GG+AA | 178 | 178 | 29.3 ± 0.5 | 29.8 ± 0.6 | 30.3 ± 0.5 | 30.7 ± 0.6 | 0.101 | 0.223 |
| rs12255372_TCF7L2 | TT | GG+GT | 51 | 308 | 28.7 ± 0.7 | 29.3 ± 1.1 | 29.9 ± 0.3 | 30.3 ± 0.4 | 0.097 | 0.400 |
| Model | Whole Population (n = 360) | Men (n = 109) | Women (n = 251) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| β ± SE | p Value | adjR2 | β ± SE | p Value | adjR2 | β ± SE | p Value | adjR2 | |
| Model A | <0.001 | 0.18 | 0.007 | 0.11 | <0.001 | 0.21 | |||
| Prevotellaceae | −0.27 ± 0.25 | 0.276 | 0.004 ± 0.38 | 0.992 | −0.44 ± 0.31 | 0.164 | |||
| GRS | 0.07 ± 0.50 | 0.887 | 0.70 ± 0.80 | 0.383 | −0.23 ± 0.63 | 0.713 | |||
| Prevotellaceae#GRS | 0.06 ± 0.04 | 0.098 | −0.006 ± 0.06 | 0.925 | 0.10 ± 0.05 | 0.039 | |||
| Model B | <0.001 | 0.18 | 0.003 | 0.13 | <0.001 | 0.19 | |||
| Leuconostocaceae | −1.37 ± 1.02 | 0.179 | −2.12 ± 1.75 | 0.228 | −0.17 ± 1.38 | 0.903 | |||
| GRS | 0.76 ± 0.16 | <0.001 | 0.51 ± 0.26 | 0.053 | 0.96 ± 0.21 | <0.001 | |||
| Leuconostocaceae#GRS | 0.23 ± 0.15 | 0.121 | 0.29 ± 0.28 | 0.305 | 0.08 ± 0.19 | 0.657 | |||
| Model C | <0.001 | 0.17 | 0.17 | 0.003 | <0.001 | 0.19 | |||
| Lactobacillaceae | 0.42 ± 0.35 | 0.231 | 0.48 ± 0.48 | 0.316 | 0.42 ± 0.48 | 0.382 | |||
| GRS | 0.99 ± 0.24 | <0.001 | 0.79 ± 0.36 | 0.032 | 1.15 ± 0.31 | <0.001 | |||
| Lactobacillaceae#GRS | −0.03 ± 0.05 | 0.506 | −0.05 ± 0.07 | 0.511 | −0.03 ± 0.07 | 0.648 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuevas-Sierra, A.; Riezu-Boj, J.I.; Guruceaga, E.; Milagro, F.I.; Martínez, J.A. Sex-Specific Associations between Gut Prevotellaceae and Host Genetics on Adiposity. Microorganisms 2020, 8, 938. https://doi.org/10.3390/microorganisms8060938
Cuevas-Sierra A, Riezu-Boj JI, Guruceaga E, Milagro FI, Martínez JA. Sex-Specific Associations between Gut Prevotellaceae and Host Genetics on Adiposity. Microorganisms. 2020; 8(6):938. https://doi.org/10.3390/microorganisms8060938
Chicago/Turabian StyleCuevas-Sierra, Amanda, José Ignacio Riezu-Boj, Elizabeth Guruceaga, Fermín Ignacio Milagro, and José Alfredo Martínez. 2020. "Sex-Specific Associations between Gut Prevotellaceae and Host Genetics on Adiposity" Microorganisms 8, no. 6: 938. https://doi.org/10.3390/microorganisms8060938