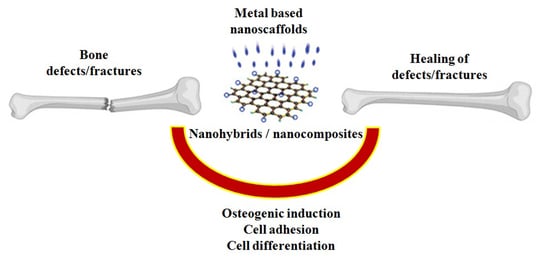
Metallic Nanoscaffolds as Osteogenic Promoters: Advances, Challenges and Scope
Abstract
:1. Introduction
2. Systematic Review of Literature
Literature Search
- Systematic reviews and research articles
- Including a quality evaluation of supportive experiments
- Published in a peer-reviewed, scientific journal
- Written in English
- Establishing the underlying mechanism of bioactivity
3. Data Extraction
4. Results
5. Copper
6. Gold
7. Magnetic Nanoparticles
8. Platinum and Palladium
9. Silver
10. Strontium
11. Titanium
12. Zinc
13. Discussion
14. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Nanoparticles | Size (nm) | Matrix | Functionalized Ligand | Cells | Reference |
|---|---|---|---|---|---|
| Copper nanoparticles | - | Chitosan | - | Rat calvarial defect | [39] |
| Graphene oxide-copper nanocomposites | 30 nm | Porous calcium phosphate | - | Rat bone marrow stem cells (BMSCs) | [40] |
| Copper ion | - | Mesoporous bioactive glasses | - | - | [42] |
| Gold nanoparticles | 80–110 nm | Mesoporous silica nanoparticles, chitosan | - | Preosteoblastic MC3T3 cells, critical-sized cranial defect site in rats | [46] |
| Gold nanoparticles | 10.76 ± 1.4 nm | - | - | MG63 osteoblast-like cells (human osteogenic sarcoma) | [47] |
| Gold nanoparticles | 20 nm | - | - | MSCs from Kunming mice | [48] |
| Gold nanoparticles | 5–45 nm | - | - | Human periodontal ligament progenitor cells (PDLPs) | [49] |
| Ferrofluid | 200 | Collagen | Hydroxyapatite | MSC from human bone marrow (hBMSC) | [54] |
| Iron oxide nanofiber | 600–1000 | Poly(L-lactide) | - | MC3T3-E1 | [55] |
| Fe powder | - | Hydroxypropylmethylcellulose | Hydroxyapatite | Rabbit bone marrowmesenchymal stem cells (rBMSCs) | [58] |
| Superparamagnetic iron oxide nanoparticles | 160 μm to 200 μm | Poly-lactic-co-glycolic acid | - | Murine bone BMSCs, rat femoral bone | [59] |
| Iron oxide nanoparticles | 7 | Polyglucose-sorbitol-carboxymethyether | - | MSC from human bone marrow (hBMSC) | [60] |
| Magnetic nanoparticles | - | Polycaprolactone | - | Mouse calvarial osteoblasts | [61] |
| Platinum nanoparticles | - | Calcium phosphate, poly vinyl alcohol | - | Human osteoblast cells | [65] |
| Platinum nanoparticles | 10–20 nm | Chitosan, poly (lactic acid) | Nanohydroxyapatite | Human osteosarcoma cell line MG-63 cells | [66] |
| Palladium nanoparticles | 2–5 nm | Reduced graphene oxide | Polypyrrole (PPy) | Osteosarcoma osteogenic cell line- ATCC HTB-85 (Saos-2) | [67] |
| Palladium nanoparticles, gold nanorods, maghemite nanoparticles | 15±5 nm, 3.4±1 nm and 10 nm | Type I collagen | Mg doped hydroxyapatite | Adipose-derived mesenchymal stem cells (hADSCs) | [68] |
| Palladium nanoparticles | 10 nm | Chitosan | Zinc oxide nanoparticles impregnated hydroxyapatite | Human dental pulp stem cells (hDPSCs) | [69] |
| Silver nanoparticles | 10–20 nm | Natural rubber latex | - | Mesenchymal stem cells of human deciduous dental pulp, bone defects in rat calvaria | [82] |
| Silver and gold nanoparticles | 12.7 to 69.1 nm, 9.3 to 54.7 nm | Silk fibroin | Hydroxyapatite | Osteoblast-like cells (MG63 cell line) | [83] |
| Silver nanoparticles | 5–15 nm | - | Collagen | Mouse mesenchymal stem cells (mMSC), mouse femoral fracture model | |
| Strontium and zinc | Ca–Si ceramic | Human bone derived cells (HOB), tibial bone defects in rats | [90] | ||
| Strontium | 70 nm × 1.3 µm | Titania nanotube arrays | Hydroxyapatite | Saos-2 cells | [91] |
| Titanium | 25 to 35 | - | - | Human periosteum-derived cells (hPDC), critical-size femoral bone defects in Wistar rats | [95] |
| Titania nanotubes | 25 and 80 nm (diameter), 5–10, 10–20 (width) | Mesenchymal stem cells derived from the bone marrow of Sprague Dawley rats | [96] | ||
| Titania | 3−4 µm (diameter) | - | Strontium-doped hydroxyapatite | hFOB1.19 cells (human fetal osteoblast cell line) | [97] |
| Titania | 32 nm | Poly-lactic-co-glycolic acid | - | Human osteoblast | [98] |
| Zinc silicate | - | Collagen | Nano hydroxyapatite | Rat BMSCs, monocytes, andaortic endothelial cells, rat critical-sized cranial defects | [103] |
References
- Cheng, H.; Chawla, A.; Yang, Y.; Li, Y.; Zhang, J.; Jang, H.L.; Khademhosseini, A. Development of nanomaterials for bone-targeted drug delivery. Drug Discov. Today 2017, 22, 1336–1350. [Google Scholar] [CrossRef]
- Jiang, W.; Kim, B.Y.S.; Rutka, J.T.; Chan, W.C.W. Nanoparticle-mediated cellular response is size-dependent. Nat. Nanotechnol. 2008, 3, 145–150. [Google Scholar] [CrossRef]
- Hubbell, J.A.; Chilkoti, A. Nanomaterials for drug delivery. Science 2012, 337, 303–305. [Google Scholar] [CrossRef]
- Hickey, D.J.; Ercan, B.; Sun, L.; Webster, T.J. Adding MgO nanoparticles to hydroxyapatite–PLLA nanocomposites for improved bone tissue engineering applications. Acta Biomater. 2015, 14, 175–184. [Google Scholar] [CrossRef]
- Kitture, R.; Ghosh, S. Hybrid nanostructures for in-vivo imaging. In Hybrid Nanostructures for Cancer Theranostics; Bohara, R.A., Thorat, N., Eds.; Elsevier Inc.: Amsterdam, The Netherlands, 2019; pp. 173–208. [Google Scholar]
- Liu, H.; Slamovich, E.B.; Webster, T.J. Less harmful acidic degradation of poly(lacticco-glycolic acid) bone tissue engineering scaffolds through titania nanoparticle addition. Int. J. Nanomedicine 2006, 1, 541–545. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, S. Mesoporous silica based nano drug delivery system synthesis, characterization and applications. In Nanocarriers for Drug Delivery; Mohapatra, S.S., Ranjan, S., Dasgupta, N., Mishra, R.K., Thomas, S., Eds.; Elsevier Inc.: Amsterdam, The Netherlands, 2019; pp. 285–317. [Google Scholar]
- Ghosh, S.; Patil, P.D.; Kitture, R.D. Physically responsive nanostructures in breast cancer theranostics. In External Field and Radiation Stimulated Breast Cancer Nanotheranostics; Thorat, N.D., Bauer, J., Eds.; IOP Publishing Ltd.: Bristol, UK, 2019; pp. 2-1–2-24. [Google Scholar]
- Ma, X.; Gong, N.; Zhong, L.; Sun, J.; Liang, X.-J. Future of nanotherapeutics: Targeting the cellular sub-organelles. Biomaterials 2016, 97, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.E.; Koo, H.; Sun, I.-C.; Hee Ryu, J.H.; Kim, K.; Kwon, I.C. Multifunctional nanoparticles for multimodal imaging and theragnosis. Chem. Soc. Rev. 2012, 41, 2656–2672. [Google Scholar] [CrossRef] [PubMed]
- Stocco, T.D.; Bassous, N.J.; Zhao, S.; Granato, A.E.C.; Webster, T.J.; Lobo, A.O. Nanofibrous scaffolds for biomedical applications. Nanoscale 2018, 10, 12228–12255. [Google Scholar] [CrossRef] [PubMed]
- Bassous, N.J.; Jones, C.L.; Webster, T.J. 3-D printed Ti-6Al-4V scaffolds for supporting osteoblast and restricting bacterial functions without using drugs: Predictive equations and experiments. Acta Biomater. 2019, 96, 662–673. [Google Scholar] [CrossRef]
- Jahangirian, H.; Azizi, S.; Rafiee-Moghaddam, R.; Baratvand, B.; Webster, T.J. Status of plant protein-based green scaffolds for regenerative medicine applications. Biomolecules 2019, 9, 619. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, I.C.P.; Woigt, L.F.; Pereira, K.D.; Luchessi, A.D.; Lopes, E.S.N.; Webster, T.J.; Gabriel, L.P. Low-cost hybrid scaffolds based on polyurethane and gelatine. J. Mater. Res. Technol. 2020, 9, 7777–7785. [Google Scholar] [CrossRef]
- Rodrigues, I.C.P.; Pereira, K.D.; Woigt, L.F.; Jardini, A.L.; Luchessi, A.D.; Lopes, E.S.N.; Webster, T.J.; Gabriel, L.P. A novel technique to produce tubular scaffolds based on collagen and elastin. Artif. Organs 2021, 45, E113–E122. [Google Scholar] [CrossRef]
- Mostafavi, A.; Abudula, T.; Russell, C.S.; Mostafavi, E.; Williams, T.J.; Salah, N.; Alshahrie, A.; Harris, S.; Basri, S.M.M.; Mishra, Y.K.; et al. In situ printing of scaffolds for reconstruction of bone defects. Acta Biomater. 2021, 127, 313–326. [Google Scholar] [CrossRef] [PubMed]
- Noori, A.; Ashrafi, S.J.; Vaez-Ghaemi, R.; Hatamian-Zaremi, A.; Webster, T.J. A review of fibrin and fibrin composites for bone tissue engineering. Int. J. Nanomedicine 2017, 12, 4937–4961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Rakotondradany, F.; Myles, A.J.; Fenniri, H.; Webster, T.J. Arginine-glycine-aspartic acid modified rosette nanotube–hydrogel composites for bone tissue engineering. Biomaterials 2009, 30, 1309–1320. [Google Scholar] [CrossRef]
- Brannigan, K.; Griffin, M. An update into the application of nanotechnology in bone healing. Open Orthop. J. 2016, 10, 808–823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neogi, T.; Zhang, Y. Epidemiology of osteoarthritis. Rheum. Dis. Clin. North Am. 2013, 39, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Wright, N.C.; Looker, A.C.; Saag, K.G.; Curtis, J.R.; Delzell, E.S.; Randall, S.; Dawson-Hughes, B. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J. Bone Miner. Res. 2014, 29, 2520–2526. [Google Scholar] [CrossRef] [Green Version]
- Hak, D.J.; Fitzpatrick, D.; Bishop, J.A.; Marsh, J.L.; Tilp, S.; Schnettler, R.; Simpson, H.; Alt, V. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury 2014, 45, S3–S7. [Google Scholar] [CrossRef]
- Rajani, R.; Schaefer, L.; Scarborough, M.T.; Gibbs, C.P. Giant cell tumors of the foot and ankle bones: High recurrence rates after surgical treatment. J. Foot Ankle Surg. 2015, 54, 1141–1145. [Google Scholar] [CrossRef]
- Nguyen, T.B.L.; Min, Y.K.; Lee, B.T. Nanoparticle biphasic calcium phosphate loading on gelatin-pectin scaffold for improved bone regeneration. Tissue Eng. Part A 2015, 21, 1376–1387. [Google Scholar] [CrossRef]
- Xing, Z.; Pedersen, T.O.; Wu, X.; Xue, Y.; Sun, Y.; Finne-Wistrand, A.; Kloss, F.R.; Waag, T.; Krueger, A.; Steinmüller-Nethl, D.; et al. Biological effects of functionalizing copolymer scaffolds with nanodiamond particles. Tissue Eng. Part A 2013, 19, 1783–1791. [Google Scholar] [CrossRef] [Green Version]
- Cross, L.M.; Thakur, A.; Jalili, N.A.; Detamore, M.; Gaharwar, A.K. Nanoengineered biomaterials for repair and regeneration of orthopedic tissue interfaces. Acta Biomater. 2016, 42, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Funda, G.; Taschieri, S.; Bruno, G.A.; Grecchi, E.; Paolo, S.; Girolamo, D.; Fabbro, M.D. Nanotechnology scaffolds for alveolar bone regeneration. Materials 2020, 13, 201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gong, T.; Xie, J.; Liao, J.; Zhang, T.; Lin, S.; Lin, Y. Nanomaterials and bone regeneration. Bone Res. 2015, 3, 15029. [Google Scholar] [CrossRef] [PubMed]
- Gorain, B.; Tekade, M.; Kesharwani, P.; Iyer, A.K.; Kalia, K.; Tekade, R.K. The use of nanoscaffolds and dendrimers in tissue engineering. Drug Discov. Today 2017, 22, 652–664. [Google Scholar] [CrossRef] [PubMed]
- Tschernitschek, H.; Borchers, L.; Geurtsen, W. Nonalloyed titanium as a bioinert metal—A review. Quintessence Int. 2005, 36, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Van den Bosch, M.; Sang, Å.O. Urban natural environments as nature-based solutions for improved public health—A systematic review of reviews. Env. Res. 2017, 158, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Smith, V.; Devane, D.; Begley, C.M.; Clarke, M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med. Res. Methodol. 2011, 11, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Shea, B.J.; Hamel, C.; Wells, G.A.; Bouter, L.M.; Kristjansson, E.; Grimshaw, J.; Henry, D.A.; Boers, M. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J. Clin. Epidemiol. 2009, 62, 1013–1020. [Google Scholar] [CrossRef] [Green Version]
- Brok, J.; Thorlund, K.; Gluud, C.; Wetterslev, J. Trial sequential analysis reveals insufficient information size and potentially false positive results in many metaanalyses. J. Clin. Epidemiol. 2008, 61, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Jamdade, D.A.; Rajpali, D.; Joshi, K.A.; Kitture, R.; Kulkarni, A.S.; Shinde, V.S.; Bellare, J.; Babiya, K.R.; Ghosh, S. Gnidia glauca and Plumbago zeylanica mediated synthesis of novel copper nanoparticles as promising antidiabetic agents. Adv. Pharmacol. Sci. 2019, 2019, 9080279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhagwat, T.R.; Joshi, K.A.; Parihar, V.S.; Asok, A.; Bellare, J.; Ghosh, S. Biogenic copper nanoparticles from medicinal plants as novel antidiabetic nanomedicine. World J. Pharm. Res. 2018, 7, 183–196. [Google Scholar]
- Ghosh, S.; More, P.; Nitnavare, R.; Jagtap, S.; Chippalkatti, R.; Derle, A.; Kitture, R.; Asok, A.; Kale, S.; Singh, S.; et al. Antidiabetic and antioxidant properties of copper nanoparticles synthesized by medicinal plant Dioscorea bulbifera. J. Nanomed. Nanotechnol. 2015, S6, 007. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, S. Copper and palladium nanostructures: A bacteriogenic approach. Appl. Microbiol. Biotechnol. 2018, 101, 7693–7701. [Google Scholar] [CrossRef] [PubMed]
- D’Mello, S.; Elangovan, S.; Hong, L.; Ross, R.D.; Sumner, D.R.; Salem, A.K. Incorporation of copper into chitosan scaffolds promotes bone regeneration in rat calvarial defects. J. Biomed. Mater. Res. Part B. 2015, 103B, 1044–1049. [Google Scholar] [CrossRef] [Green Version]
- Zhang, W.; Chang, Q.; Xu, L.; Li, G.; Yang, G.; Ding, X.; Wang, X.; Cui, D.; Jiang, X. Graphene oxide-copper nanocomposite-coated porous CaP scaffold for vascularized bone regeneration via activation of Hif-1α. Adv. Healthcare Mater. 2016, 5, 1299–1309. [Google Scholar] [CrossRef] [PubMed]
- Wan, C.; Shao, J.; Gilbert, S.R.; Riddle, R.C.; Long, F.; Johnson, R.S.; Schipani, E.; Clemens, T.L. Role of HIF-1α in skeletal development. Ann. N. Y. Acad. Sci. 2010, 1192, 322–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bari, A.; Bloise, N.; Fiorilli, S.; Novajra, G.; Vallet-Regí, M.; Bruni, G.; Torres-Pardo, A.; González-Calbet, J.M.; Visai, L.; Vitale-Brovarone, C. Copper-containing mesoporous bioactive glass nanoparticles as multifunctional agent for bone regeneration. Acta Biomater. 2017, 55, 493–504. [Google Scholar] [CrossRef]
- Ghosh, S.; Patil, S.; Chopade, N.B.; Luikham, S.; Kitture, R.; Gurav, D.D.; Patil, A.B.; Phadatare, S.D.; Sontakke, V.; Kale, S.; et al. Gnidia glauca leaf and stem extract mediated synthesis of gold nanocatalysts with free radical scavenging potential. J. Nanomed. Nanotechnol. 2016, 7, 358. [Google Scholar] [CrossRef] [Green Version]
- Shende, S.; Joshi, K.A.; Kulkarni, A.S.; Shinde, V.S.; Parihar, V.S.; Kitture, R.; Banerjee, K.; Kamble, N.; Bellare, J.; Ghosh, S. Litchi chinensis peel: A novel source for synthesis of gold and silver nanocatalysts. Glob. J. Nanomedicine 2017, 3, 555603. [Google Scholar]
- Ghosh, S.; Jagtap, S.; More, P.; Shete, U.J.; Maheshwari, N.O.; Rao, S.J.; Kitture, R.; Kale, S.; Bellare, J.; Patil, S.; et al. Dioscorea bulbifera mediated synthesis of novel AucoreAgshell nanoparticles with potent antibiofilm and antileishmanial activity. J. Nanomater. 2015, 2015, 562938. [Google Scholar] [CrossRef] [Green Version]
- Liang, H.; Jin, C.; Ma, L.; Feng, X.; Deng, X.; Wu, S.; Liu, X.; Yang, C. Accelerated bone regeneration by gold-nanoparticle-loaded mesoporous silica through stimulating immunomodulation. ACS Appl. Mater. Interfaces 2019, 11, 41758–41769. [Google Scholar] [CrossRef]
- Tsai, S.-W.; Liaw, J.-W.; Kao, Y.-C.; Huang, M.-Y.; Lee, C.-Y.; Rau, L.-R.; Huang, C.-Y.; Wei, K.-C.; Ye, T.-C. Internalized gold nanoparticles do not affect the osteogenesis and apoptosis of MG63 osteoblast-like cells: A quantitative, in vitro study. PLoS ONE 2013, 8, e76545. [Google Scholar] [CrossRef] [PubMed]
- Yi, C.; Liu, D.; Fong, C.-C.; Zhang, J.; Yang, M. Gold nanoparticles promote osteogenic differentiation of mesenchymal stem cells through p38 MAPK pathway. ACS Nano 2010, 4, 6439–6448. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kong, N.; Zhang, Y.; Yang, W.; Yan, F. Size-dependent effects of gold nanoparticles on osteogenic differentiation of human periodontal ligament progenitor cells. Theranostics 2017, 7, 1214–1224. [Google Scholar] [CrossRef]
- Zhang, X.; Cheng, G.; Xing, X.; Liu, J.; Cheng, Y.; Ye, T.; Wang, Q.; Xiao, X.; Li, Z.; Deng, H. Near-infrared light-triggered porous AuPd alloy nanoparticles to produce mild localized heat to accelerate bone regeneration. J. Phys. Chem. Lett. 2019, 10, 4185–4191. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, P.; Mao, H.; Zhang, Y.; Zheng, L.; Yu, P.; Guo, Z.; Li, L.; Jiang, Q. PEGylated gold nanoparticles promote osteogenic differentiation in in vitro and in vivo systems. Mater. Des. 2021, 197, 109231. [Google Scholar] [CrossRef]
- Ghosh, S.; Sanghavi, S.; Sancheti, P. Metallic biomaterial for bone support and replacement. In Fundamental Biomaterials: Metals; Balakrishnan, P., Sreekala, M.S., Thomas, S., Eds.; Woodhead Publishing Series in Biomaterials; Woodhead Publishing: Cambridge, UK, 2018; Volume 2, pp. 139–165. [Google Scholar]
- Ghosh, S.; More, P.; Derle, A.; Kitture, R.; Kale, T.; Gorain, M.; Avasthi, A.; Markad, P.; Kundu, G.C.; Kale, S.; et al. Diosgenin functionalized iron oxide nanoparticles as novel nanomaterial against breast cancer. J. Nanosci. Nanotechnol. 2015, 15, 9464–9472. [Google Scholar] [CrossRef] [PubMed]
- Bock, N.; Riminucci, A.; Dionigi, C.; Russo, A.; Tampieri, A.; Landi, E.; Goranov, V.A.; Marcacci, M.; Dediu, V. A novel route in bone tissue engineering: Magnetic biomimetic scaffolds. Acta Biomater. 2010, 6, 786–796. [Google Scholar] [CrossRef]
- Cai, Q.; Shi, Y.; Shan, D.; Jia, W.; Duan, S.; Deng, X.; Yang, X. Osteogenic differentiation of MC3T3-E1 cells on poly(L-lactide)/Fe3O4 nanofibers with static magnetic field exposure. Mater. Sci. Eng. C 2015, 55, 166–173. [Google Scholar] [CrossRef]
- Rajesh, R.; Ravichandran, Y.D. Development of a new carbon nanotube–alginate–hydroxyapatite tricomponent composite scaffold for application in bone tissue engineering. Int. J. Nanomed. 2015, 10, 7–15. [Google Scholar]
- Yang, L.; Webster, T.J. Nanotechnology controlled drug delivery for treating bone diseases. Expert Opin. Drug Deliv. 2009, 6, 851–864. [Google Scholar] [CrossRef]
- Yang, C.; Huan, Z.; Wang, X.; Wu, C.; Chang, J. 3D printed Fe scaffolds with HA nanocoating for bone regeneration. ACS Biomater. Sci. Eng. 2018, 4, 608–616. [Google Scholar] [CrossRef]
- Zhao, Y.-Z.; Chen, R.; Xue, P.-P.; Luo, L.-Z.; Zhong, B.; Tong, M.-Q.; Chen, B.; Yao, Q.; Yuan, J.-D.; Xu, H.-L. Magnetic PLGA microspheres loaded with SPIONs promoted the reconstruction of bone defects through regulating the bone mesenchymal stem cells under an external magnetic field. Mater. Sci. Eng. C 2021, 122, 111877. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Chen, B.; Cao, M.; Sun, J.; Wu, H.; Zhao, P.; Xing, J.; Yang, Y.; Zhang, X.; Ji, M.; et al. Response of MAPK pathway to iron oxide nanoparticles in vitro treatment promotes osteogenic differentiation of hBMSCs. Biomaterials 2016, 86, 11–20. [Google Scholar] [CrossRef]
- Yun, H.-M.; Ahn, S.-J.; Park, K.-R.; Kim, M.-J.; Kim, J.-J.; Jin, G.-Z.; Kim, H.-W.; Kim, E.-C. Magnetic nanocomposite scaffolds combined with static magnetic field in the stimulation of osteoblastic differentiation and bone formation. Biomaterials 2016, 85, 88–98. [Google Scholar] [CrossRef]
- Rokade, S.; Joshi, K.; Mahajan, K.; Patil, S.; Tomar, G.; Dubal, D.; Parihar, V.S.; Kitture, R.; Bellare, J.R.; Ghosh, S. Gloriosa superba mediated synthesis of platinum and palladium nanoparticles for induction of apoptosis in breast cancer. Bioinorg. Chem. Appl. 2018, 2018, 4924186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rokade, S.S.; Joshi, K.A.; Mahajan, K.; Tomar, G.; Dubal, D.S.; Parihar, V.S.; Kitture, R.; Bellare, J.; Ghosh, S. Novel anticancer platinum and palladium nanoparticles from Barleria prionitis. Glob. J. Nanomedicine 2017, 2, 555600. [Google Scholar]
- Ghosh, S.; Nitnavare, R.; Dewle, A.; Tomar, G.B.; Chippalkatti, R.; More, P.; Kitture, R.; Kale, S.; Bellare, J.; Chopade, B.A. Novel platinum-palladium bimetallic nanoparticles synthesized by Dioscorea bulbifera: Anticancer and antioxidant activities. Int. J. Nanomedicine. 2015, 10, 7477–7490. [Google Scholar]
- Eid, K.; Eldesouky, A.; Fahmy, A.; Shahat, A.; Elaal, R.A. Calcium phosphate scaffold loaded with platinum nanoparticles for bone allograft. Am. J. Biomed. Sci. 2013, 5, 242–249. [Google Scholar] [CrossRef]
- Radwan-Pragłowska, J.; Janus, Ł.; Piatkowski, M.; Bogdał, D.; Matysek, D. 3D hierarchical, nanostructured chitosan/PLA/HA scaffolds doped with TiO2/Au/Pt NPs with tunable properties for guided bone tissue engineering. Polymers 2020, 12, 792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balaji, M.; Nithya, P.; Mayakrishnan, A.; Jegatheeswaran, S.; Selvam, S.; Cai, Y.; Yao, J.; Sundrarajan, M. Fabrication of palladium nanoparticles anchored polypyrrole functionalized reduced graphene oxide nanocomposite for antibiofilm associated orthopedic tissue engineering. Appl. Surf. Sci. 2020, 510, 145403. [Google Scholar]
- Calabrese, G.; Petralia, S.; Fabbi, C.; Forte, S.; Franco, D.; Guglielmino, S.; Esposito, E.; Cuzzocrea, S.; Traina, F.; Conoci, S. Au, Pd and maghemite nanofunctionalized hydroxyapatite scaffolds for bone regeneration. Regen. Biomater. 2020, 7, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Heidari, F.; Tabatabaei, F.S.; Razavi, M.; Lari, R.B.; Tavangar, M.; Romanos, G.E.; Vashaee, D.; Tayebi, L. 3D construct of hydroxyapatite/zinc oxide/palladium nanocomposite scaffold for bone tissue engineering. J. Mater. Sci. Mater. Med. 2020, 31, 85. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Harke, A.N.; Chacko, M.J.; Gurav, S.P.; Joshi, K.A.; Dhepe, A.; Dewle, A.; Tomar, G.B.; Kitture, R.; Parihar, V.S.; et al. Gloriosa superba mediated synthesis of silver and gold nanoparticles for anticancer applications. J. Nanomed. Nanotechnol. 2016, 7. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, S.; Chacko, M.J.; Harke, A.N.; Gurav, S.P.; Joshi, K.A.; Dhepe, A.; Kulkarni, A.S.; Shinde, V.S.; Parihar, V.S.; Asok, A.; et al. Barleria prionitis leaf mediated synthesis of silver and gold nanocatalysts. J. Nanomed. Nanotechnol. 2016, 7. [Google Scholar] [CrossRef]
- Shende, S.; Joshi, K.A.; Kulkarni, A.S.; Charolkar, C.; Shinde, V.S.; Parihar, V.S.; Kitture, R.; Banerjee, K.; Kamble, N.; Bellare, J.; et al. Platanus orientalis leaf mediated rapid synthesis of catalytic gold and silver nanoparticles. J. Nanomed. Nanotechnol. 2018, 9, 2. [Google Scholar] [CrossRef]
- Shinde, S.S.; Joshi, K.A.; Patil, S.; Singh, S.; Kitture, R.; Bellare, J.; Ghosh, S. Green synthesis of silver nanoparticles using Gnidia glauca and computational evaluation of synergistic potential with antimicrobial drugs. World J. Pharm. Res. 2018, 7, 156–171. [Google Scholar]
- Joshi, K.A.; Ghosh, S.; Dhepe, A. Green synthesis of antimicrobial nanosilver using in-vitro cultured Dioscorea bulbifera. Asian J. Org. Med. Chem. 2019, 4, 222–227. [Google Scholar] [CrossRef]
- Sant, D.G.; Gujarathi, T.R.; Harne, S.R.; Ghosh, S.; Kitture, R.; Kale, S.; Chopade, B.A.; Pardesi, K.R. Adiantum philippense L. frond assisted rapid green synthesis of gold and silver nanoparticles. J. Nanoparticles 2013, 2013, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Salunke, G.R.; Ghosh, S.; Santosh, R.J.; Khade, S.; Vashisth, P.; Kale, T.; Chopade, S.; Pruthi, V.; Kundu, G.; Bellare, J.R.; et al. Rapid efficient synthesis and characterization of AgNPs, AuNPs and AgAuNPs from a medicinal plant, Plumbago zeylanica and their application in biofilm control. Int. J. Nanomedicine 2014, 9, 2635–2653. [Google Scholar] [PubMed] [Green Version]
- Ranpariya, B.; Salunke, G.; Karmakar, S.; Babiya, K.; Sutar, S.; Kadoo, N.; Kumbhakar, P.; Ghosh, S. Antimicrobial synergy of silver-platinum nanohybrids with antibiotics. Front. Microbiol. 2021, 11, 610968. [Google Scholar] [CrossRef]
- Cao, H.; Zhang, W.; Meng, F.; Guo, J.; Wang, D.; Qian, S.; Jiang, X.; Liu, X.; Chu, P.K. Osteogenesis catalyzed by titanium-supported silver nanoparticles. ACS Appl. Mater. Interfaces 2017, 9, 5149–5157. [Google Scholar] [CrossRef]
- Castiglioni, S.; Cazzaniga, A.; Locatelli, L.; Maier, J.A.M. Silver nanoparticles in orthopedic applications: New insights on their effects on osteogenic cells. Nanomaterials 2017, 7, 124. [Google Scholar] [CrossRef] [Green Version]
- Jiang, J.; Li, L.; Li, K.; Li, G.; You, F.; Zuo, Y.; Li, Y.; Li, J. Antibacterial nanohydroxyapatite/polyurethane composite scaffolds with silver phosphate particles for bone regeneration. J. Biomater. Sci. Polym. Ed. 2016, 27, 1584–1598. [Google Scholar] [CrossRef]
- Jin, S.; Li, J.; Wang, J.; Jiang, J.; Zuo, Y.; Li, Y.; Yang, F. Electrospun silver ion-loaded calcium phosphate/chitosan antibacterial composite fibrous membranes for guided bone regeneration. Int. J. Nanomedicine 2018, 13, 4591–4605. [Google Scholar] [CrossRef] [Green Version]
- Marques, L.; Martinez, G.; Guidelli, E.; Tamashiro, J.; Segato, R.; Payão, S.L.M.; Baa, O.; Kinoshita, A. Performance on bone regeneration of a silver nanoparticle delivery system based on natural rubber membrane NRL-AgNP. Coatings 2020, 10, 323. [Google Scholar] [CrossRef] [Green Version]
- Ribeiro, M.; Ferraz, M.P.; Monteiro, F.J.; Fernandes, M.H.; Beppu, M.M.; Mantione, D.; Sardon, H. Antibacterial silk fibroin/nanohydroxyapatite hydrogels with silver and gold nanoparticles for bone regeneration. Nanomedicine 2017, 13, 231–239. [Google Scholar] [CrossRef]
- Zhang, R.; Lee, P.; Lui, V.C.H.; Chen, Y.; Liu, X.; Lok, C.N.; To, M.; Yeung, K.W.K.; Wong, K.K.Y. Silver nanoparticles promote osteogenesis of mesenchymal stem cells and improve bone fracture healing in osteogenesis mechanism mouse model. Nanomedicine 2015, 11, 1949–1959. [Google Scholar] [CrossRef]
- Marie, P.J. Strontium ranelate: A novel mode of action optimizing bone formation and resorption. Osteoporos. Int. 2005, 16, S7–S10. [Google Scholar] [CrossRef] [PubMed]
- Ammann, P. Strontium ranelate: A novel mode of action leading to renewed bone quality. Osteoporos. Int. 2005, 16, S11–S15. [Google Scholar] [CrossRef]
- Marie, P.J. Strontium ranelate: New insights into its dual mode of action. Bone 2007, 4, S5–S8. [Google Scholar] [CrossRef]
- Ghosh, S.; Webster, T.J. Mesoporous silica based nanostructures for bone tissue regeneration. Front. Mater. 2021, 8, 692309. [Google Scholar] [CrossRef]
- Katagiri, T.; Takahashi, N. Regulatory mechanisms of osteoblast and osteoclast differentiation. Oral Dis. 2002, 8, 147–159. [Google Scholar] [CrossRef]
- Zreiqat, H.; Ramaswamy, Y.; Wu, C.; Paschalidis, A.; Lu, Z.; James, B.; Birke, O.; McDonald, M.; Little, D.; Dunstan, C.R. The incorporation of strontium and zinc into a calcium–silicon ceramic for bone tissue engineering. Biomaterials 2010, 31, 3175–3184. [Google Scholar] [CrossRef]
- Xin, Y.; Jiang, J.; Huo, K.; Hu, T.; Chu, P.K. Bioactive SrTiO3 nanotube arrays: Strontium delivery platform on Ti-based osteoporotic bone implants. ACS Nano 2009, 3, 3228–3234. [Google Scholar] [CrossRef]
- Brammer, K.S.; Oh, S.H.; Gallagher, J.O.; Jin, S.H. Enhanced cellular mobility guided by TiO2 nanotube surfaces. Nano. Lett. 2008, 8, 786–793. [Google Scholar] [CrossRef]
- Macak, J.M.; Tsuchiya, H.; Ghicov, A.; Yasuda, K.; Hahn, R.; Bauer, S.; Schmuki, P. TiO2 nanotubes: Self-organized electrochemical formation, properties and applications. Curr. Opin. Solid State Mater. Sci. 2007, 11, 3–18. [Google Scholar] [CrossRef]
- Ghicov, A.; Schmuki, P. Self-ordering electrochemistry: A review on growth and functionality of TiO2 nanotubes and other self-aligned MOx structures. Chem. Commun. 2009, 2791–2808. [Google Scholar] [CrossRef] [PubMed]
- Yavari, S.A.; van der Stok, J.; Chai, Y.C.; Wauthle, R.; Birgani, Z.T.; Habibovic, P.; Mulier, M.; Schrooten, J.; Weinans, H.; Zadpoor, A.A. Bone regeneration performance of surface-treated porous titanium. Biomaterials 2014, 35, 6172–6181. [Google Scholar] [CrossRef]
- Zhao, L.; Liu, l.; Wu, Z.; Zhang, y.; Chu, P.K. Effects of micropitted/nanotubular titania topographies on bone mesenchymal stem cell osteogenic differentiation. Biomaterials 2012, 33, 2629–2641. [Google Scholar] [CrossRef]
- Zhou, J.; Li, B.; Lu, S.; Zhang, L.; Han, Y. Regulation of osteoblast proliferation and differentiation by interrod spacing of Sr-HA nanorods on microporous titania coatings. ACS Appl. Mater. Interfaces 2013, 5, 5358–5365. [Google Scholar] [CrossRef]
- Palin, E.; Liu, H.; Webster, T.J. Mimicking the nanofeatures of bone increases bone-forming cell adhesion and proliferation. Nanotechnology 2005, 16, 1828–1835. [Google Scholar] [CrossRef]
- Adersh, A.; Kulkarni, A.R.; Ghosh, S.; More, P.; Chopade, B.A.; Gandhi, M.N. Surface defect rich ZnO quantum dots as antioxidant inhibiting α-amylase and α-glucosidase: A potential anti-diabetic nanomedicine. J. Mater. Chem. B. 2015, 3, 4597–4606. [Google Scholar]
- Robkhob, P.; Ghosh, S.; Bellare, J.; Jamdade, D.; Tang, I.M.; Thongmee, S. Effect of silver doping on antidiabetic and antioxidant potential of ZnO nanorods. J. Trace Elem. Med. Biol. 2020, 58, 126448. [Google Scholar] [CrossRef] [PubMed]
- Kitture, R.; Chordiya, K.; Gaware, S.; Ghosh, S.; More, P.A.; Kulkarni, P.; Chopade, B.A.; Kale, S.N. ZnO nanoparticles-red sandalwood conjugate: A promising anti-diabetic agent. J. Nanosci. Nanotechnol. 2015, 15, 4046–4051. [Google Scholar] [CrossRef]
- Karmakar, S.; Ghosh, S.; Kumbhakar, P. Enhanced sunlight driven photocatalytic and antibacterial activity of flower-like ZnO@MoS2 nanocomposite. J. Nanopart. Res. 2020, 22, 11. [Google Scholar] [CrossRef]
- Song, Y.; Wu, H.; Gao, Y.; Li, J.; Lin, K.; Liu, B.; Lei, X.; Cheng, P.; Zhang, S.; Wang, Y.; et al. Zinc silicate/nano-hydroxyapatite/collagen scaffolds promote angiogenesis and bone regeneration via the p38 MAPK pathway in activated monocytes. ACS Appl. Mater. Interfaces 2020, 12, 16058–16075. [Google Scholar] [CrossRef] [PubMed]
- Mehta, M.; Schmidt-Bleek, K.; Duda, G.N.; Mooney, D.J. Biomaterial delivery of morphogens to mimic the natural healing cascade in bone. Adv. Drug Deliv. Rev. 2012, 64, 1257–1276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kane, R.; Ma, P.X. Mimicking the nanostructure of bone matrix to regenerate bone. Mater. Today 2013, 16, 418–423. [Google Scholar] [CrossRef]
- Marrella, A.; Lee, T.Y.; Lee, D.H.; Karuthedom, S.; Syla, D.; Chawla, A.; Khademhosseini, A.; Jang, H.L. Engineering vascularized and innervated bone biomaterials for improved skeletal tissue regeneration. Mater. Today 2018, 21, 362–376. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Mostafavi, E.; Thorat, N.; Webster, T.J. Nanobiomaterials for three-dimensional bioprinting. In Nanotechnology in Medicine and Biology; Liu, H., Shokuhfar, T., Ghosh, S., Eds.; Elsevier: Amsterdam, The Netherlands, 2021. (In press) [Google Scholar]
- Monteiro, N.; Martins, A.; Reis, R.L.; Neves, N.M. Nanoparticle-based bioactive agent release systems for bone and cartilage tissue engineering. Regen. Ther. 2015, 1, 109–118. [Google Scholar] [CrossRef] [Green Version]
- Vo, T.N.; Kasper, F.K.; Mikos, A.G. Strategies for controlled delivery of growth factors and cells for bone regeneration. Adv. Drug Deliv. Rev. 2012, 64, 1292–1309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gogolewski, S.; Jovanovic, M.; Perren, S.M.; Dillon, J.G.; Hughes, M.K. Tissue response and in vivo degradation of selected polyhydroxyacids: Polylactides (PLA), poly(3-hydroxybutyrate) (PHB), and poly(3-hydroxybutyrate-co-3-hydroxyvalerate) (PHB/VA). J. Biomed. Mater. Res. 1993, 27, 1135–1148. [Google Scholar] [CrossRef] [PubMed]
- Freiberg, S.; Zhu, X.X. Polymer microspheres for controlled drug release. Int. J. Pharm. 2004, 282, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Witte, F.; Fischer, J.; Nellesen, J.; Crostack, H.A.; Kaese, V.; Pisch, A.; Beckmann, F.; Windhagen, H. In vitro and in vivo corrosion measurements of magnesium alloys. Biomaterials 2006, 27, 1013–1018. [Google Scholar] [CrossRef]
- Bohner, M. Resorbable biomaterials as bone graft substitutes. Mater. Today 2010, 13, 24–30. [Google Scholar] [CrossRef]
- Ghosh, S.; Webster, T.J. Nanobiotechnology: Microbes and Plant Assisted Aynthesis of Nanoparticles, Mechanisms and Applications; Elsevier Inc.: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Ning, C.; Zhou, L.; Tan, G. Fourth-generation biomedical materials. Mater. Today 2016, 19, 1–3. [Google Scholar] [CrossRef]











Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghosh, S.; Webster, T.J. Metallic Nanoscaffolds as Osteogenic Promoters: Advances, Challenges and Scope. Metals 2021, 11, 1356. https://doi.org/10.3390/met11091356
Ghosh S, Webster TJ. Metallic Nanoscaffolds as Osteogenic Promoters: Advances, Challenges and Scope. Metals. 2021; 11(9):1356. https://doi.org/10.3390/met11091356
Chicago/Turabian StyleGhosh, Sougata, and Thomas Jay Webster. 2021. "Metallic Nanoscaffolds as Osteogenic Promoters: Advances, Challenges and Scope" Metals 11, no. 9: 1356. https://doi.org/10.3390/met11091356