Evaluating the Impact of Telehealth-Based, Diabetes Medication Training for Community Health Workers on Glycemic Control
Abstract
:1. Introduction
2. Methods
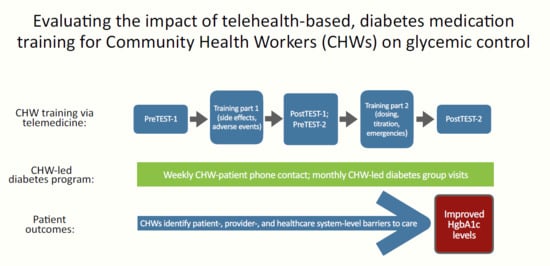
2.1. Study Design
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Clinical Outcomes
3.2. Community Health Worker Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Community Health Worker TEST-1 and TEST-2. Correct Answers Are Bolded
- The most common side effect of metformin is:
- Weight loss
- Weight gain
- Stomach upset
- Low blood sugar
- What diabetes medication(s) are FOUR dollars at CVS or Walmart?
- Actos
- Metformin
- The “g” drugs e.g., glimepiride, glyburide, glipizide
- B and C
- All of the above
- What medication class end in “pril” or “artan” i.e., lisinopril, losartan?
- Cholesterol medications
- Diabetes medications
- Weight loss medications
- Blood Pressure medications
- The most common side effect of the “prils”is:
- Cough
- Diarrhea
- Stomach upset
- Leg cramps
- What medication class end in “statin”?
- Cholesterol medications
- Diabetes medications
- Weight loss medications
- Blood Pressure medications
- The most common side effect of the “statins” is:
- Leg cramps
- Stomach upset
- Weight loss
- Cough
- A concerning side effect of Actos (pioglitazone) is:
- A rash
- Headache
- Blurry vision
- Leg swelling
- Actos was once taken off the market in other countries since some thought it increased the chances of:
- Skin infection
- Bladder cancer
- Amputation
- Kidney failure
- The most common medication used for diabetes care is:
- The “g” drugs e.g., glimepiride, glyburide, glipizide
- Actos (pioglitazone)
- Metformin
- Insulin
- What is NOT common with patients taking metformin?
- Weight loss
- Stomach upset
- Diarrhea
- Swelling of the legs
- What does insulin do to blood sugar?
- Increases blood sugar
- Does not change blood sugar
- Decreases blood sugar
- What does orange juice do to blood sugar?
- Increases blood sugar
- Does not change blood sugar
- Decreases blood sugar
- What US pharmacy sells some insulin for $25 per bottle?
- CVS
- Walmart
- Kroger
- Walgreens
- What cholesterol pill is the strongest to decrease triglycerides?
- Simvastatin
- Glimepiride
- Lisinopril
- Fenofibrate
- What is the maximum dose of metformin per day?
- 500
- 1000
- 1500
- 2000
- What medication(s) is often prescribed after a heart attack and/or stroke?
- A “statin”
- Aspirin
- Plavix
- All of the above
- Which medication(s) may cause patients to GAIN weight?
- Actos/pioglitazone
- The “g” drugs e.g., glimepiride, glyburide, glipizide
- Metformin
- Insulin
- A, B, and D
- Which medication should be stored in the refrigerator?
- Insulin
- Enalapril
- Metformin
- Actos/pioglitazone
- the “g” drugs e.g., glimepiride, glyburide, glipizide
- Which medication must be taken with food?
- Atorvastatin
- Lisinopril
- The “g” drugs e.g., glimepiride, glyburide, glipizide
- Actos/pioglitazone
- Which is NOT correct?
- Novolog insulin works fast (short-acting)
- Humalog insulin works “in the middle” (intermediate)
- NPH insulin works “in the middle” (intermediate)
- Lantus insulin works for a long time (long-acting)
Appendix B. Community Health Worker TEST-1 and TEST-2. Correct Answers Are Bolded
- How often should patients take metformin “IR”?
- Once daily
- Twice daily
- Three times daily
- Four times daily
- How often should patients take metformin “XL”?
- Once daily
- Twice daily
- Three times daily
- Four times daily
- How is metformin IR started?
- 250mg daily
- 500mg daily
- 1000mg daily
- 1500mg daily
- How much is metformin IR/XL increased each week?
- 250mg
- 500mg
- 1500mg
- 2000mg
- What medication is the most effective to decrease blood sugar?
- Metformin(a) IR
- Metformin(a) XL
- They are the same
- Less than ______ is “severe” low blood sugar.
- 20
- 30
- 40
- 50
- A patient’s blood sugar is 62. He drank a cup of orange juice. After how many minutes should he recheck his blood sugar?
- 5
- 15
- 45
- 60
- 90
- A patient’s medication is expired. Now, the medication may:
- Be stronger than before
- Be weaker than before
- Not change at all
- All of the above
- What is NOT a symptom of high blood sugar?
- Increased urination
- Increased thirst
- Increased constipation
- Increased hunger
- Your patient tells you that her blood sugar is 425. What should you do?
- Tell her to drink more non-sugary liquids
- Tell her to recheck it and make sure the number is right
- Ask her if she took her medications as prescribed today
- Tell her to continue monitoring until it goes down and if not, call her doctor
- All of the above
- What is “sliding scale insulin”?
- A type of short-acting insulin
- A type of long-acting insulin
- Taking a certain amount of insulin based on blood sugar
- Decreasing the amount of insulin the patient takes over time
- What is a reasonable way to increase the amount of insulin used if fasting and afternoon/evening sugars are high?
- Increased by 3 units every 3 days
- Increased by 5 units every day
- Increase by 10 units every 10 days
- Increase by 7 units every day
- Where is the preferred place to inject insulin?
- Upper arm
- Stomach
- Thigh
- Buttocks
- What is the starting dose for glimepiride?
- 2 mg/day
- 4 mg/day
- 5 mg/day
- 15 mg/day
- What is the maximum dose for glimepiride?
- 2 mg/day
- 5 mg/day
- 8 mg/day
- 45 mg/day
- What is the starting dose for Actos?
- 2 mg/day
- 4 mg/day
- 5 mg/day
- 15 mg/day
- What is the maximum dose for Actos?
- 2 mg/day
- 5 mg/day
- 8 mg/day
- 45 mg/day
- What medication can NOT be started in kidney failure (end stage)?
- Glimepiride
- Insulin
- Actos
- Metformin
- A patient’s bottle of medicine is empty. She has 2 refills, expiration 1/1/2019. What should she do?
- Call the clinic (pharmacy) to fill for refills
- Call the clinic to make an appointment with her doctor
- Wait until her appointment next month and ask her doctor.
References
- International Diabetes Federation. International Diabetes Atlas-9th Edition. Available online: https://www.idf.org/e-library/epidemiology-research/diabetes-atlas (accessed on 4 September 2020).
- Centers for Disease Control and Prevention; US Department of Health and Human Services. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States; CDC: Atlanta, GA, USA, 2017.
- Chow, E.A.; Foster, H.; Gonzalez, V.; Mclver, L. The Disparate Impact of Diabetes on Racial/Ethnic Minority Populations. Clin. Diabetes 2012, 30, 130–133. [Google Scholar] [CrossRef] [Green Version]
- Polonsky, W.H.; Henry, R.R. Poor medication adherence in type 2 diabetes: Recognizing the scope of the problem and its key contributors. Patient Prefer Adherence 2016, 10, 1299–1307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kane, E.P.; Collinsworth, A.W.; Schmidt, K.L.; Brown, R.M.; Snead, C.A.; Barnes, S.A.; Fleming, N.S.; Walton, J.W. Improving diabetes care and outcomes with community health workers. Fam. Pract. 2016, 33, 523–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.T.; Bussell, J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [Green Version]
- Babamoto, K.S.; Sey, K.A.; Camilleri, A.J.; Karlan, V.J.; Catalasan, J.; Morisky, D.E. Improving diabetes care and health measures among hispanics using community health workers: Results from a randomized controlled trial. Health Educ. Behav. 2009, 36, 113–126. [Google Scholar] [CrossRef]
- Bhaumik, S.; Moola, S.; Tyagi, J.; Nambiar, D.; Kakoti, M. Community health workers for pandemic response: A rapid evidence synthesis. BMJ Glob. Health 2020, 5. [Google Scholar] [CrossRef]
- Egbujie, B.A.; Delobelle, P.A.; Levitt, N.; Puoane, T.; Sanders, D.; van Wyk, B. Role of community health workers in type 2 diabetes mellitus self-management: A scoping review. PLoS ONE 2018, 13, e0198424. [Google Scholar] [CrossRef]
- Katigbak, C.; Van Devanter, N.; Islam, N.; Trinh-Shevrin, C. Partners in health: A conceptual framework for the role of community health workers in facilitating patients’ adoption of healthy behaviors. Am. J. Public Health 2015, 105, 872–880. [Google Scholar] [CrossRef]
- Hill-Briggs, F.; Batts-Turner, M.; Gary, T.L.; Brancati, F.L.; Hill, M.; Levine, D.M.; Bone, L. Training community health workers as diabetes educators for urban African Americans: Value added using participatory methods. Prog. Community Health Partnersh. 2007, 1, 185–194. [Google Scholar] [CrossRef]
- Swider, S.M.; Martin, M.; Lynas, C.; Rothschild, S. Project MATCH: Training for a promotora intervention. Diabetes Educ. 2010, 36, 98–108. [Google Scholar] [CrossRef]
- Vaughan, E.M.; Naik, A.D.; Lewis, C.M.; Foreyt, J.P.; Samson, S.L.; Hyman, D.J. Telemedicine Training and Support for Community Health Workers: Improving Knowledge of Diabetes. Telemed J. E Health 2020, 26, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Perez-Escamilla, R.; Damio, G.; Chhabra, J.; Fernandez, M.L.; Segura-Perez, S.; Vega-Lopez, S.; Kollannor-Samuel, G.; Calle, M.; Shebl, F.M.; D’Agostino, D. Impact of a community health workers-led structured program on blood glucose control among latinos with type 2 diabetes: The DIALBEST trial. Diabetes Care 2015, 38, 197–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silverman, J.; Krieger, J.; Sayre, G.; Nelson, K. The Value of Community Health Workers in Diabetes Management in Low-Income Populations: A Qualitative Study. J. Community Health 2018, 43, 842–847. [Google Scholar] [CrossRef]
- Vogenberg, F.R.; Isaacson Barash, C.; Pursel, M. Personalized medicine: Part 1: Evolution and development into theranostics. Pharm. Ther. 2010, 35, 560–576. [Google Scholar]
- Power, R.; Nolan, J.M.; Prado-Cabrero, A.; Coen, R.; Roche, W.; Power, T.; Howard, A.N.; Mulcahy, R. Targeted Nutritional Intervention for Patients with Mild Cognitive Impairment: The Cognitive impAiRmEnt Study (CARES) Trial 1. J. Pers. Med. 2020, 10, 43. [Google Scholar] [CrossRef] [PubMed]
- Colleran, K.; Harding, E.; Kipp, B.J.; Zurawski, A.; MacMillan, B.; Jelinkova, L.; Kalishman, S.; Dion, D.; Som, D.; Arora, S. Building capacity to reduce disparities in diabetes: Training community health workers using an integrated distance learning model. Diabetes Educ. 2012, 38, 386–396. [Google Scholar] [CrossRef]
- Vaughan, E.M.; Hyman, D.J.; Naik, A.D.; Samson, S.L.; Razjouyan, J.; Foreyt, J.P. A Telehealth-supported, Integrated care with CHWs, and MEdication-access (TIME) program for diabetes improves HbA1c: A randomized clinical trial. J. Gen. Int. Med. 2020. [Google Scholar] [CrossRef]
- Office of the Assistant Secretary for Planning and Evaluation. Poverty Guidelines. Available online: https://aspe.hhs.gov/poverty-guidelines (accessed on 17 August 2020).
- Texas Department of State Health Services. CHW Certification Requirements. Available online: https://www.dshs.texas.gov/chw/CertRequire.aspx (accessed on 4 September 2020).
- Zoom. Zoom for Healthcare. Available online: https://zoom.us/healthcare (accessed on 4 September 2020).
- Ohmd. The Modern Healthcare Communication Platform. Available online: https://www.ohmd.com (accessed on 4 September 2020).
- American Diabetes Association. Standards of medical care in diabetes 2020. Diabetes Care 2020, 42, S1–S193. [Google Scholar]
- Hoover, L.E. Cholesterol Management: ACC/AHA Updates Guideline. Am. Fam. Physician 2019, 99, 589–591. [Google Scholar]
- US Preventive Services Task Force. Final Recommendations (Screening). Available online: https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations (accessed on 13 July 2020).
- Lorig, K.; Holman, H.; Sobel, D.; Laurent, D.; Gonzalez, V.; Minor, M. Living a Healthy Life with Chronic Conditions, 4th ed.; Bull Publishing Company: Boulder, CO, USA, 2012. [Google Scholar]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [Green Version]
- Scott, K.; Beckham, S.W.; Gross, M.; Pariyo, G.; Rao, K.D.; Cometto, G.; Perry, H.B. What do we know about community-based health worker programs? A systematic review of existing reviews on community health workers. Hum. Resour. Health 2018, 16, 39. [Google Scholar] [CrossRef]
- De Witt Jansen, B.; Brazil, K.; Passmore, P.; Buchanan, H.; Maxwell, D.; McIlfatrick, S.J.; Morgan, S.M.; Watson, M.; Parsons, C. Evaluation of the impact of telementoring using ECHO(c) technology on healthcare professionals’ knowledge and self-efficacy in assessing and managing pain for people with advanced dementia nearing the end of life. BMC Health Serv. Res. 2018, 18, 228. [Google Scholar] [CrossRef] [PubMed]
- Edirippulige, S.; Armfield, N.R. Education and training to support the use of clinical telehealth: A review of the literature. J. Telemed Telecare 2017, 23, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Lam, W.Y.; Fresco, P. Medication Adherence Measures: An Overview. Biomed. Res. Int. 2015, 2015, 217047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United States Census Bureau. Census 2020. Available online: https://www.census.gov (accessed on 5 September 2020).

| n (%) or Mean (SD) | |
| Sex | |
| Female | 36 (65.5%) |
| Age (years) | 52.9 (±8.2) |
| Range | 27–80 |
| Work | |
| Construction/landscaping | 17 (30.9%) |
| Domestic | 26 (47.3%) |
| Food Service | 5 (9.1%) |
| Unknown | 7 (12.7%) |
| Religious Affiliation | |
| Christianity | 54 (98.2%) |
| Unknown | 1 (1.8%) |
| Time since diabetes diagnosis (years) | 11.5 (±8.0) |
| Range | 0.5–28 |
| HbA1c (%) | 8.98 * (±2.4) |
| Range | 5.7–14.9 ** |
| Antihyperglycemic Treatment | |
| Lifestyle only | 1 (1.8%) |
| Oral only | 36 (65.5%) |
| Orals + injectables | 18 (32.7%) |
| Injectables only | 0 (0.0%) |
| Blood Pressure (mmHg) | |
| Systolic | 131.5 (±17.2) |
| Range | 100–175 |
| Diastolic | 76.3 (±9.4) |
| Range | 56–111 |
| Body Mass Index (kg/m2) | 33.8 (±8.0) |
| Range | 23.2–56.9 |
| n (%) or Mean (SD) | |
| Sex | |
| Female | 4 (66.7%) |
| Age (years) | 48.3 (±10.37) |
| Work outside of current study | |
| Construction | 1 (16.7%) |
| Domestic | 1 (16.7%) |
| Ministerial/pastoral | 2 (33.3%) |
| Student | 1 (16.7%) |
| Religious Affiliation | |
| Christianity | 6 (100%) |
| Education (completed) | |
| High school | 6 (100%) |
| Junior college | 1 (16.7%) |
| Completed college | 2 (33.3%) |
| Language | |
| Bilingual (English/Spanish) | 5 (83.3%) |
| Spanish only | 1 (16.7%) |
| Birth origin | |
| United States (Texas) | 2 (33.33%) |
| International | |
| El Salvador | 1 (16.7%) |
| Guatemala | 1 (16.7%) |
| Mexico | 2 (33.3%) |
| Residential Demographics * | |
| Median Income ($) | 47,545 (±12,297.44) |
| Below federal poverty level | 19.3 (8.19%) |
| High school graduates | 76.7 (7.14%) |
| Latino(a) | 47.7 (11.4%) |
| Barrier-Level | Incidence (n) * |
| Patient | |
| Glucose level education | 367 |
| Adherence education | 195 |
| Correct dosing, titration | 48 |
| Provider | |
| Medication identification, use, and instructions | 93 |
| Medication side effects, adverse events, emergencies | 34 |
| Medication eligibility, cost | 24 |
| Healthcare system | |
| Obtaining refills; Correct dosing/amount from pharmacy | 105 |
| Clinic appointments | 81 |
| Clinic eligibility | 37 |
| Total | 984 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keegan, C.N.; Johnston, C.A.; Cardenas, V.J., Jr.; Vaughan, E.M. Evaluating the Impact of Telehealth-Based, Diabetes Medication Training for Community Health Workers on Glycemic Control. J. Pers. Med. 2020, 10, 121. https://doi.org/10.3390/jpm10030121
Keegan CN, Johnston CA, Cardenas VJ Jr., Vaughan EM. Evaluating the Impact of Telehealth-Based, Diabetes Medication Training for Community Health Workers on Glycemic Control. Journal of Personalized Medicine. 2020; 10(3):121. https://doi.org/10.3390/jpm10030121
Chicago/Turabian StyleKeegan, Casey N., Craig A. Johnston, Victor J. Cardenas, Jr., and Elizabeth M. Vaughan. 2020. "Evaluating the Impact of Telehealth-Based, Diabetes Medication Training for Community Health Workers on Glycemic Control" Journal of Personalized Medicine 10, no. 3: 121. https://doi.org/10.3390/jpm10030121