Circulating Tumor Cells Predict Response of Neoadjuvant Chemotherapy in Patients with Bladder Cancer: A Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Samples Collection
2.2. Immunomagnetic Beads Preparation for CTC Isolation
2.3. Blood Sample Preparation
2.4. CTC Enrichment and IsoFlux™
2.5. Sample Isolation and Collection
2.6. CTC Detection and Immunofluorescence
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Detection of Circulating UC Cells in Patients with MIBC
3.3. Relationship between the Number of CTCs and Treatment Modality during Time Course
3.4. Correlation of the CTC Values with the Tumor Stage
4. Discussion
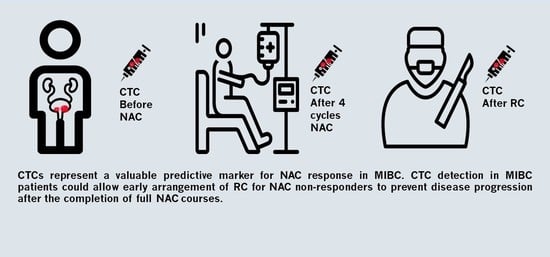
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Witjes, J.A.; Bruins, H.M.; Cathomas, R.; Compérat, E.M.; Cowan, N.C.; Gakis, G.; Hernández, V.; Linares Espinós, E.; Lorch, A.; Neuzillet, Y.; et al. European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur. Urol. 2021, 79, 82–104. [Google Scholar] [CrossRef] [PubMed]
- Yin, M.; Joshi, M.; Meijer, R.P.; Glantz, M.; Holder, S.; Harvey, H.A.; Kaag, M.; Fransen van de Putte, E.E.; Horenblas, S.; Drabick, J.J. Neoadjuvant Chemotherapy for Muscle-Invasive Bladder Cancer: A Systematic Review and Two-Step Meta-Analysis. Oncologist 2016, 21, 708–715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stein, J.P.; Lieskovsky, G.; Cote, R.; Groshen, S.; Feng, A.C.; Boyd, S.; Skinner, E.; Bochner, B.; Thangathurai, D.; Mikhail, M.; et al. Radical cystectomy in the treatment of invasive bladder cancer: Long-term results in 1054 patients. J. Clin. Oncol. 2001, 19, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Yafi, F.A.; Aprikian, A.G.; Chin, J.L.; Fradet, Y.; Izawa, J.; Estey, E.; Fairey, A.; Rendon, R.; Cagiannos, I.; Lacombe, L.; et al. Contemporary outcomes of 2287 patients with bladder cancer who were treated with radical cystectomy: A Canadian multicentre experience. BJU Int. 2011, 108, 539–545. [Google Scholar] [CrossRef]
- Grossman, H.B.; Natale, R.B.; Tangen, C.M.; Speights, V.O.; Vogelzang, N.J.; Trump, D.L.; deVere White, R.W.; Sarosdy, M.F.; Wood, D.P., Jr.; Raghavan, D.; et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N. Engl. J. Med. 2003, 349, 859–866. [Google Scholar] [CrossRef]
- Vale, C.L. Neoadjuvant chemotherapy in invasive bladder cancer: Update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration. Eur. Urol. 2005, 48, 202–206. [Google Scholar] [CrossRef]
- Motterle, G.; Andrews, J.R.; Morlacco, A.; Karnes, R.J. Predicting Response to Neoadjuvant Chemotherapy in Bladder Cancer. Eur. Urol. Focus 2020, 6, 642–649. [Google Scholar] [CrossRef] [Green Version]
- Abrahamsson, J.; Aaltonen, K.; Engilbertsson, H.; Liedberg, F.; Patschan, O.; Rydén, L.; Sjödahl, G.; Gudjonsson, S. Circulating tumor cells in patients with advanced urothelial carcinoma of the bladder: Association with tumor stage, lymph node metastases, FDG-PET findings, and survival. Urol. Oncol. 2017, 35, 606.e609–606.e616. [Google Scholar] [CrossRef]
- Chalfin, H.J.; Glavaris, S.A.; Gorin, M.A.; Kates, M.R.; Fong, M.H.; Dong, L.; Matoso, A.; Bivalacqua, T.J.; Johnson, M.H.; Pienta, K.J.; et al. Circulating Tumor Cell and Circulating Tumor DNA Assays Reveal Complementary Information for Patients with Metastatic Urothelial Cancer. Eur. Urol. Oncol. 2021, 4, 310–314. [Google Scholar] [CrossRef] [Green Version]
- Pantel, K.; Alix-Panabières, C. Circulating tumour cells in cancer patients: Challenges and perspectives. Trends Mol. Med. 2010, 16, 398–406. [Google Scholar] [CrossRef]
- Rink, M.; Schwarzenbach, H.; Riethdorf, S.; Soave, A. The current role and future directions of circulating tumor cells and circulating tumor DNA in urothelial carcinoma of the bladder. World J. Urol. 2019, 37, 1785–1799. [Google Scholar] [CrossRef]
- Chiang, P.J.; Xu, T.; Cha, T.L.; Tsai, Y.T.; Liu, S.Y.; Wu, S.T.; Meng, E.; Tsao, C.W.; Kao, C.C.; Chen, C.L.; et al. Programmed Cell Death Ligand 1 Expression in Circulating Tumor Cells as a Predictor of Treatment Response in Patients with Urothelial Carcinoma. Biology 2021, 10, 674. [Google Scholar] [CrossRef]
- Flaig, T.W.; Wilson, S.; van Bokhoven, A.; Varella-Garcia, M.; Wolfe, P.; Maroni, P.; Genova, E.E.; Morales, D.; Lucia, M.S. Detection of circulating tumor cells in metastatic and clinically localized urothelial carcinoma. Urology 2011, 78, 863–867. [Google Scholar] [CrossRef] [Green Version]
- Lu, J.J.; Kakehi, Y.; Takahashi, T.; Wu, X.X.; Yuasa, T.; Yoshiki, T.; Okada, Y.; Terachi, T.; Ogawa, O. Detection of circulating cancer cells by reverse transcription-polymerase chain reaction for uroplakin II in peripheral blood of patients with urothelial cancer. Clin. Cancer Res. 2000, 6, 3166–3171. [Google Scholar]
- Naoe, M.; Ogawa, Y.; Morita, J.; Omori, K.; Takeshita, K.; Shichijyo, T.; Okumura, T.; Igarashi, A.; Yanaihara, A.; Iwamoto, S.; et al. Detection of circulating urothelial cancer cells in the blood using the CellSearch System. Cancer 2007, 109, 1439–1445. [Google Scholar] [CrossRef]
- Naoe, M.; Ohta, M.; Hasebe, Y.; Matsui, Y.; Unoki, T.; Shimoyama, H.; Nakasato, T.; Ogawa, Y.; Tsukada, M.; Sunagawa, M. Detection of circulating tumor cells and the importance of their measurement in urological cancers. Urol. Sci. 2018, 29, 176. [Google Scholar] [CrossRef]
- Wolchok, J.D.; Hoos, A.; O’Day, S.; Weber, J.S.; Hamid, O.; Lebbé, C.; Maio, M.; Binder, M.; Bohnsack, O.; Nichol, G.; et al. Guidelines for the evaluation of immune therapy activity in solid tumors: Immune-related response criteria. Clin. Cancer Res. 2009, 15, 7412–7420. [Google Scholar] [CrossRef] [Green Version]
- Marcq, G.; Jarry, E.; Ouzaid, I.; Hermieu, J.F.; Henon, F.; Fantoni, J.C.; Xylinas, E. Contemporary best practice in the use of neoadjuvant chemotherapy in muscle-invasive bladder cancer. Ther. Adv. Urol. 2019, 11, 1756287218823678. [Google Scholar] [CrossRef]
- Griffiths, G.; Hall, R.; Sylvester, R.; Raghavan, D.; Parmar, M.K. International phase III trial assessing neoadjuvant cisplatin, methotrexate, and vinblastine chemotherapy for muscle-invasive bladder cancer: Long-term results of the BA06 30894 trial. J. Clin. Oncol. 2011, 29, 2171–2177. [Google Scholar] [CrossRef] [Green Version]
- Gandaglia, G.; Popa, I.; Abdollah, F.; Schiffmann, J.; Shariat, S.F.; Briganti, A.; Montorsi, F.; Trinh, Q.D.; Karakiewicz, P.I.; Sun, M. The effect of neoadjuvant chemotherapy on perioperative outcomes in patients who have bladder cancer treated with radical cystectomy: A population-based study. Eur. Urol. 2014, 66, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Tyson, M.D., 2nd; Bryce, A.H.; Ho, T.H.; Carballido, E.M.; Castle, E.P. Perioperative complications after neoadjuvant chemotherapy and radical cystectomy for bladder cancer. Can. J. Urol. 2014, 21, 7259–7265. [Google Scholar] [PubMed]
- Cristofanilli, M.; Budd, G.T.; Ellis, M.J.; Stopeck, A.; Matera, J.; Miller, M.C.; Reuben, J.M.; Doyle, G.V.; Allard, W.J.; Terstappen, L.W.; et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N. Engl. J. Med. 2004, 351, 781–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, M.C.; Doyle, G.V.; Terstappen, L.W. Significance of Circulating Tumor Cells Detected by the CellSearch System in Patients with Metastatic Breast Colorectal and Prostate Cancer. J. Oncol. 2010, 2010, 617421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Riethdorf, S.; Wu, G.; Wang, T.; Yang, K.; Peng, G.; Liu, J.; Pantel, K. Meta-analysis of the prognostic value of circulating tumor cells in breast cancer. Clin. Cancer Res. 2012, 18, 5701–5710. [Google Scholar] [CrossRef] [Green Version]
- Lucci, A.; Hall, C.S.; Lodhi, A.K.; Bhattacharyya, A.; Anderson, A.E.; Xiao, L.; Bedrosian, I.; Kuerer, H.M.; Krishnamurthy, S. Circulating tumour cells in non-metastatic breast cancer: A prospective study. Lancet Oncol. 2012, 13, 688–695. [Google Scholar] [CrossRef]
- De Bono, J.S.; Scher, H.I.; Montgomery, R.B.; Parker, C.; Miller, M.C.; Tissing, H.; Doyle, G.V.; Terstappen, L.W.; Pienta, K.J.; Raghavan, D. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin. Cancer Res. 2008, 14, 6302–6309. [Google Scholar] [CrossRef] [Green Version]
- Denève, E.; Riethdorf, S.; Ramos, J.; Nocca, D.; Coffy, A.; Daurès, J.P.; Maudelonde, T.; Fabre, J.M.; Pantel, K.; Alix-Panabières, C. Capture of viable circulating tumor cells in the liver of colorectal cancer patients. Clin. Chem. 2013, 59, 1384–1392. [Google Scholar] [CrossRef] [Green Version]
- Rink, M.; Chun, F.K.; Dahlem, R.; Soave, A.; Minner, S.; Hansen, J.; Stoupiec, M.; Coith, C.; Kluth, L.A.; Ahyai, S.A.; et al. Prognostic role and HER2 expression of circulating tumor cells in peripheral blood of patients prior to radical cystectomy: A prospective study. Eur. Urol. 2012, 61, 810–817. [Google Scholar] [CrossRef]
- Gazzaniga, P.; de Berardinis, E.; Raimondi, C.; Gradilone, A.; Busetto, G.M.; De Falco, E.; Nicolazzo, C.; Giovannone, R.; Gentile, V.; Cortesi, E.; et al. Circulating tumor cells detection has independent prognostic impact in high-risk non-muscle invasive bladder cancer. Int. J. Cancer 2014, 135, 1978–1982. [Google Scholar] [CrossRef] [Green Version]
- Schulze, K.; Gasch, C.; Staufer, K.; Nashan, B.; Lohse, A.W.; Pantel, K.; Riethdorf, S.; Wege, H. Presence of EpCAM-positive circulating tumor cells as biomarker for systemic disease strongly correlates to survival in patients with hepatocellular carcinoma. Int. J. Cancer 2013, 133, 2165–2171. [Google Scholar] [CrossRef]
- Vashist, Y.K.; Effenberger, K.E.; Vettorazzi, E.; Riethdorf, S.; Yekebas, E.F.; Izbicki, J.R.; Pantel, K. Disseminated tumor cells in bone marrow and the natural course of resected esophageal cancer. Ann. Surg. 2012, 255, 1105–1112. [Google Scholar] [CrossRef]
- Chen, B.H.; Kao, C.C.; Xu, T.; Yang, Y.N.; Cha, T.L.; Tsai, Y.T.; Liu, S.Y.; Wu, S.T.; Meng, E.; Tsao, C.W.; et al. Determining programmed cell death ligand 1 expression in circulating tumor cells of patients with clear cell renal cell carcinoma and its correlation with response to programmed cell death protein 1 inhibitors. Int. J. Urol. 2022, 29, 947–954. [Google Scholar] [CrossRef]
- Kao, C.C.; Xu, T.; Yang, Y.N.; Tsai, Y.T.; Liu, S.Y.; Wu, S.T.; Meng, E.; Tsao, C.W.; Chen, C.L.; Sun, G.H.; et al. Detection of circulating tumor cells as therapeutic markers in patients with penile squamous cell carcinoma: A preliminary study. J. Chin. Med. Assoc. 2022, 85, 95–101. [Google Scholar] [CrossRef]
- Amir, E.; Clemons, M.; Purdie, C.A.; Miller, N.; Quinlan, P.; Geddie, W.; Coleman, R.E.; Freedman, O.C.; Jordan, L.B.; Thompson, A.M. Tissue confirmation of disease recurrence in breast cancer patients: Pooled analysis of multi-centre, multi-disciplinary prospective studies. Cancer Treat. Rev. 2012, 38, 708–714. [Google Scholar] [CrossRef]
- Nakagawa, T.; Martinez, S.R.; Goto, Y.; Koyanagi, K.; Kitago, M.; Shingai, T.; Elashoff, D.A.; Ye, X.; Singer, F.R.; Giuliano, A.E.; et al. Detection of circulating tumor cells in early-stage breast cancer metastasis to axillary lymph nodes. Clin. Cancer Res. 2007, 13, 4105–4110. [Google Scholar] [CrossRef] [Green Version]
- Bidard, F.C.; Peeters, D.J.; Fehm, T.; Nolé, F.; Gisbert-Criado, R.; Mavroudis, D.; Grisanti, S.; Generali, D.; Garcia-Saenz, J.A.; Stebbing, J.; et al. Clinical validity of circulating tumour cells in patients with metastatic breast cancer: A pooled analysis of individual patient data. Lancet Oncol. 2014, 15, 406–414. [Google Scholar] [CrossRef]
- Scher, H.I.; Heller, G.; Molina, A.; Attard, G.; Danila, D.C.; Jia, X.; Peng, W.; Sandhu, S.K.; Olmos, D.; Riisnaes, R.; et al. Circulating tumor cell biomarker panel as an individual-level surrogate for survival in metastatic castration-resistant prostate cancer. J. Clin. Oncol. 2015, 33, 1348–1355. [Google Scholar] [CrossRef]
- Cohen, S.J.; Punt, C.J.; Iannotti, N.; Saidman, B.H.; Sabbath, K.D.; Gabrail, N.Y.; Picus, J.; Morse, M.; Mitchell, E.; Miller, M.C.; et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J. Clin. Oncol. 2008, 26, 3213–3221. [Google Scholar] [CrossRef]
- Pantel, K.; Brakenhoff, R.H.; Brandt, B. Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat. Rev. Cancer 2008, 8, 329–340. [Google Scholar] [CrossRef]
- Pantel, K.; Alix-Panabières, C.; Riethdorf, S. Cancer micrometastases. Nat. Rev. Clin. Oncol. 2009, 6, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Soave, A.; Riethdorf, S.; Dahlem, R.; von Amsberg, G.; Minner, S.; Weisbach, L.; Engel, O.; Fisch, M.; Pantel, K.; Rink, M. A nonrandomized, prospective, clinical study on the impact of circulating tumor cells on outcomes of urothelial carcinoma of the bladder patients treated with radical cystectomy with or without adjuvant chemotherapy. Int. J. Cancer 2017, 140, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Rink, M.; Zabor, E.C.; Furberg, H.; Xylinas, E.; Ehdaie, B.; Novara, G.; Babjuk, M.; Pycha, A.; Lotan, Y.; Trinh, Q.D.; et al. Impact of smoking and smoking cessation on outcomes in bladder cancer patients treated with radical cystectomy. Eur. Urol. 2013, 64, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Boeri, L.; Soligo, M.; Frank, I.; Boorjian, S.A.; Thompson, R.H.; Tollefson, M.; Quevedo, F.J.; Cheville, J.C.; Karnes, R.J. Cigarette smoking is associated with adverse pathological response and increased disease recurrence amongst patients with muscle-invasive bladder cancer treated with cisplatin-based neoadjuvant chemotherapy and radical cystectomy: A single-centre experience. BJU Int. 2019, 123, 1011–1019. [Google Scholar] [CrossRef]
- Yoshida, S.; Koga, F.; Kobayashi, S.; Ishii, C.; Tanaka, H.; Tanaka, H.; Komai, Y.; Saito, K.; Masuda, H.; Fujii, Y.; et al. Role of diffusion-weighted magnetic resonance imaging in predicting sensitivity to chemoradiotherapy in muscle-invasive bladder cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, e21–e27. [Google Scholar] [CrossRef]
- Ahmed, S.A.; Taher, M.G.A.; Ali, W.A.; Ebrahem, M. Diagnostic performance of contrast-enhanced dynamic and diffusion-weighted MR imaging in the assessment of tumor response to neoadjuvant therapy in muscle-invasive bladder cancer. Abdom. Radiol. 2021, 46, 2712–2721. [Google Scholar] [CrossRef]
- Choi, W.; Porten, S.; Kim, S.; Willis, D.; Plimack, E.R.; Hoffman-Censits, J.; Roth, B.; Cheng, T.; Tran, M.; Lee, I.L.; et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 2014, 25, 152–165. [Google Scholar] [CrossRef] [Green Version]
- Seiler, R.; Ashab, H.A.D.; Erho, N.; van Rhijn, B.W.G.; Winters, B.; Douglas, J.; Van Kessel, K.E.; Fransen van de Putte, E.E.; Sommerlad, M.; Wang, N.Q.; et al. Impact of Molecular Subtypes in Muscle-invasive Bladder Cancer on Predicting Response and Survival after Neoadjuvant Chemotherapy. Eur. Urol. 2017, 72, 544–554. [Google Scholar] [CrossRef]



| Age (Mean ± SD) 63.5 ± 6.6 | No. of Patients 33 | Percentage 100 |
|---|---|---|
| Gender | ||
| Male | 16 | 48.5 |
| Female | 17 | 51.5 |
| Grade | ||
| Low | 8 | 24.2 |
| High | 25 | 75.8 |
| Clinical T Stage | ||
| 1 | 0 | 0 |
| 2 | 25 | 75.8 |
| 3 | 5 | 15.2 |
| 4 | 3 | 9.1 |
| Pathological T Stage | 0 | |
| 0 | 7 | 21.2 |
| 1 | 12 | 36.4 |
| 2a | 4 | 12.1 |
| 2b | 1 | 3 |
| 3a | 4 | 12.1 |
| 3b | 2 | 6.1 |
| 4a | 3 | 9.1 |
| 4b | 0 | 0 |
| Chemotherapy regimen | ||
| Cisplatin | 26 | 78.8 |
| Carboplatin | 7 | 21.2 |
| No. of Patients | Baseline | CTC Numbers/7.5 mL after Four Cycles of Neoadjuvant Chemotherapy (Mean ± SD) | 2 Weeks after Radical Cystectomy |
|---|---|---|---|
| DC group: 19 | 2.3 ± 0.7 | 1.0 ± 0.6 | 0.3 ± 0.5 |
| PD group: 14 | 3.5 ± 1.6 | 4.6 ± 2.1 | 1.2 ± 0.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jhuo, Y.-C.; Cha, T.-L.; Kao, C.-C.; Tsai, Y.-T.; Wu, S.-T.; Meng, E.; Tsao, C.-W.; Chen, C.-L.; Ting, H.-K.; Sun, G.-H.; et al. Circulating Tumor Cells Predict Response of Neoadjuvant Chemotherapy in Patients with Bladder Cancer: A Preliminary Study. Diagnostics 2023, 13, 1032. https://doi.org/10.3390/diagnostics13061032
Jhuo Y-C, Cha T-L, Kao C-C, Tsai Y-T, Wu S-T, Meng E, Tsao C-W, Chen C-L, Ting H-K, Sun G-H, et al. Circulating Tumor Cells Predict Response of Neoadjuvant Chemotherapy in Patients with Bladder Cancer: A Preliminary Study. Diagnostics. 2023; 13(6):1032. https://doi.org/10.3390/diagnostics13061032
Chicago/Turabian StyleJhuo, Yu-Cing, Tai-Lung Cha, Chien-Chang Kao, Yi-Ta Tsai, Sheng-Tang Wu, En Meng, Chih-Wei Tsao, Chin-Li Chen, Hui-Kung Ting, Guang-Huan Sun, and et al. 2023. "Circulating Tumor Cells Predict Response of Neoadjuvant Chemotherapy in Patients with Bladder Cancer: A Preliminary Study" Diagnostics 13, no. 6: 1032. https://doi.org/10.3390/diagnostics13061032