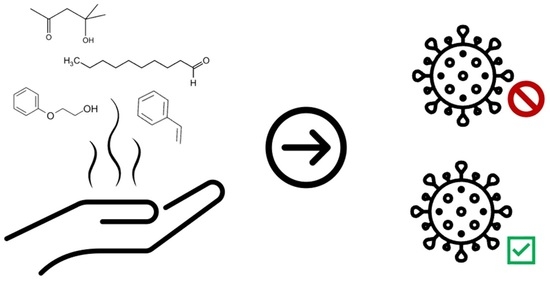
Investigating the Use of SARS-CoV-2 (COVID-19) Odor Expression as a Non-Invasive Diagnostic Tool—Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Human Hand Odor Collection
2.1.1. Sample Collection Details
2.1.2. Late 2021 Hand Odor Samples
2.1.3. Early-2022 and Mid-2022 Hand Odor Samples
2.2. Confirmation of SARS-CoV-2 Infection
2.3. Patient Demographics
2.4. Preparation of Collection Materials
2.4.1. Vial Cleaning Procedure
2.4.2. Pre-Treatment of Cotton Gauze
2.4.3. Storage & Containment
2.5. HS-SPME-GC-MS Method
2.6. Data Pre-Processing
2.7. Statistical Analysis
3. Results
3.1. sPLS-DA Modeling for All Timeframes
3.2. sPLS-DA Modeling for Individual Timeframes
3.3. Identification of Features of Interest
4. Discussion
4.1. SARS-CoV-2 Infection Diagnostic Model Performance
4.2. Limitations and Future Perspective
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Race | Sex at Birth | SARS-CoV-2 Infection Status | Age | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Delta (+) | Omicron BA.2 (+) | Omicron BA.5 (+) | (−) | 18–30 | 31–45 | 46–60 | 60+ | |
| Asian | 3 | 0 | 0 | 0 | 0 | 3 | 1 | 2 | 0 | 0 |
| Black | 29 | 46 | 18 | 4 | 17 | 36 | 15 | 19 | 19 | 22 |
| Hispanic/Latinx * | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| Unknown | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| White | 7 | 15 | 1 | 8 | 6 | 7 | 8 | 3 | 6 | 5 |


References
- World Health Organization WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 13 August 2022).
- Fernandes, Q.; Inchakalody, V.P.; Merhi, M.; Mestiri, S.; Taib, N.; Moustafa Abo El-Ella, D.; Bedhiafi, T.; Raza, A.; Al-Zaidan, L.; Mohsen, M.O.; et al. Emerging COVID-19 variants and their impact on SARS-CoV-2 diagnosis, therapeutics and vaccines. Ann. Med. 2022, 54, 524–540. [Google Scholar] [CrossRef] [PubMed]
- Abumeeiz, M.; Elliott, L.; Olla, P. Use of Breath Analysis for Diagnosing COVID-19: Opportunities, Challenges, and Considerations for Future Pandemic Responses. Disaster Med. Public Health Prep. 2021, 16, 2137–2140. [Google Scholar] [CrossRef] [PubMed]
- Mendel, J.; Frank, K.; Edlin, L.; Hall, K.; Webb, D.; Mills, J.; Holness, H.K.; Furton, K.G.; Mills, D.E. Preliminary accuracy of COVID-19 odor detection by canines and HS-SPME-GC-MS using exhaled breath samples. Forensic Sci. Int. Synerg. 2021, 3, 100155. [Google Scholar] [CrossRef] [PubMed]
- Sharun, K.; Jose, B.; Tiwari, R.; Natesan, S.; Dhama, K. Biodetection dogs for COVID-19: An alternative diagnostic screening strategy. Public Health 2021, 197, e10. [Google Scholar] [CrossRef]
- Kritikos, A.; Caruana, G.; Brouillet, R.; Miroz, J.P.; Abed-Maillard, S.; Stieger, G.; Opota, O.; Croxatto, A.; Vollenweider, P.; Bart, P.A.; et al. Sensitivity of rapid antigen testing and rt-pcr performed on nasopharyngeal swabs versus saliva samples in COVID-19 hospitalized patients: Results of a prospective comparative trial (restart). Microorganisms 2021, 9, 1910. [Google Scholar] [CrossRef]
- Dinnes, J.; Deeks, J.J.; Berhane, S.; Taylor, M.; Adriano, A.; Davenport, C.; Dittrich, S.; Emperador, D.; Takwoingi, Y.; Cunningham, J.; et al. Rapid, point-of-care antigen and molecular-based tests for diagnosis of SARS-CoV-2 infection. Cochrane Database Syst. Rev. 2021, 3, 1–129. [Google Scholar] [CrossRef]
- Alcoba-Florez, J.; Gil-Campesino, H.; de Artola, D.G.M.; González-Montelongo, R.; Valenzuela-Fernández, A.; Ciuffreda, L.; Flores, C. Sensitivity of different RT-qPCR solutions for SARS-CoV-2 detection. Int. J. Infect. Dis. 2020, 99, 190. [Google Scholar] [CrossRef]
- Brihn, A.; Chang, J.; OYong, K.; Balter, S.; Terashita, D.; Rubin, Z.; Yeganeh, N. Diagnostic Performance of an Antigen Test with RT-PCR for the Detection of SARS-CoV-2 in a Hospital Setting—Los Angeles County, California, June–August 2020. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 702–706. [Google Scholar] [CrossRef]
- Mouliou, D.S.; Gourgoulianis, K.I. False-positive and false-negative COVID-19 cases: Respiratory prevention and management strategies, vaccination, and further perspectives. Expert Rev. Respir. Med. 2021, 15, 993–1002. [Google Scholar] [CrossRef]
- Marra, P.; Colacurcio, V.; Bisogno, A.; De Luca, P.; Calvanese, M.; Petrosino, M.; De Bonis, E.; Troisi, D.; Cassandro, C.; Cavaliere, M.; et al. Evaluation of Discomfort in Nasopharyngeal Swab Specimen Collection for SARS-CoV-2 Diagnosis. Clin. Ter. 2021, 172, 448–452. [Google Scholar] [CrossRef]
- Gokool, V.A.; Crespo-Cajigas, J.; Mallikarjun, A.; Collins, A.; Kane, S.A.; Plymouth, V.; Nguyen, E.; Abella, B.S.; Holness, H.K.; Furton, K.G.; et al. The Use of Biological Sensors and Instrumental Analysis to Discriminate COVID-19 Odor Signatures. Biosensors 2022, 12, 1003. [Google Scholar] [CrossRef]
- Bordbar, M.M.; Samadinia, H.; Hajian, A.; Sheini, A.; Safaei, E.; Aboonajmi, J.; Arduini, F.; Sharghi, H.; Hashemi, P.; Khoshsafar, H.; et al. Mask assistance to colorimetric sniffers for detection of COVID-19 disease using exhaled breath metabolites. Sens. Actuators B Chem. 2022, 369, 132379. [Google Scholar] [CrossRef]
- Eskandari, E.; Ahmadi Marzaleh, M.; Roudgari, H.; Hamidi Farahani, R.; Nezami-Asl, A.; Laripour, R.; Aliyazdi, H.; Dabbagh Moghaddam, A.; Zibaseresht, R.; Akbarialiabad, H.; et al. Sniffer dogs as a screening/diagnostic tool for COVID-19: A proof of concept study. BMC Infect. Dis. 2021, 21, 243. [Google Scholar] [CrossRef]
- Curran, A.M.; Rabin, S.I.; Furton, K.G. Analysis of the Uniqueness and Persistence of Human Scent. Forensic Sci. Commun. 2005, 7, 1–12. [Google Scholar]
- Kusano, M.; Mendez, E.; Furton, K.G. Comparison of the Volatile Organic Compounds from Different Biological Specimens for Profiling Potential. J. Forensic Sci. 2013, 58, 29–39. [Google Scholar] [CrossRef]
- Shirasu, M.; Touhara, K. The scent of disease: Volatile organic compounds of the human body related to disease and disorder. J. Biochem. 2011, 150, 257–266. [Google Scholar] [CrossRef]
- Wilson, A.D. Noninvasive early disease diagnosis by electronic-nose and related VOC-detection devices. Biosensors 2020, 10, 73. [Google Scholar] [CrossRef]
- Buljubasic, F.; Buchbauer, G. The scent of human diseases: A review on specific volatile organic compounds as diagnostic biomarkers. Flavour Fragr. J. 2015, 30, 5–25. [Google Scholar] [CrossRef]
- Chen, H.; Qi, X.; Zhang, L.; Li, X.; Ma, J.; Zhang, C.; Feng, H.; Yao, M. COVID-19 screening using breath-borne volatile organic compounds. J. Breath Res. 2021, 15, 047104. [Google Scholar] [CrossRef]
- Lamote, K.; Janssens, E.; Schillebeeckx, E.; Lapperre, T.S.; De Winter, B.Y.; Van Meerbeeck, J.P. The scent of COVID-19: Viral (semi-)volatiles as fast diagnostic biomarkers? J. Breath Res. 2020, 14, 042001. [Google Scholar] [CrossRef]
- Ruszkiewicz, D.M.; Sanders, D.; O’Brien, R.; Hempel, F.; Reed, M.J.; Riepe, A.C.; Bailie, K.; Brodrick, E.; Darnley, K.; Ellerkmann, R.; et al. Diagnosis of COVID-19 by analysis of breath with gas chromatography-ion mobility spectrometry—A feasibility study. EClinicalMedicine 2020, 29, 100609. [Google Scholar] [CrossRef]
- Curran, A.M.; Rabin, S.I.; Prada, P.A.; Furton, K.G. Comparison of the volatile organic compounds present in human odor using SPME-GC/MS. J. Chem. Ecol. 2005, 31, 1607–1619. [Google Scholar] [CrossRef] [PubMed]
- Curran, A.M.; Ramirez, C.F.; Schoon, A.A.; Furton, K.G. The frequency of occurrence and discriminatory power of compounds found in human scent across a population determined by SPME-GC/MS. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2007, 846, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Curran, A.M.; Prada, P.A.; Furton, K.G. The differentiation of the volatile organic signatures of individuals through SPME-GC/ms of characteristic human scent compounds. J. Forensic Sci. 2010, 55, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Cobas SARS-CoV-2—Instructions For Use. Available online: https://www.fda.gov/media/136049/download (accessed on 15 January 2023).
- Food and Drug Administration. BINAXNOW COVID-19 AG CARD (PN 195-000)—Instructions for Use. Available online: https://www.fda.gov/media/141570/download (accessed on 15 January 2023).
- Gokool, V.A.; Holness, H.K.; Furton, K.G. The influence of intra-personal variations in human hand odor on the determination of sample donor. Forensic Sci. Int. 2022, 334, 111235. [Google Scholar] [CrossRef]
- Le Cao, K.-A.; Rohart, F.; Gonzalez, I.; Dejean, S.; Gautier, B.; Bartolo, F.; Monget, P.; Coquery, J.; Yao, F.; Liquet, B. mixOmics: Omics Data Integration Project. R Package Version 6.1.1. Available online: https://cran.r-project.org/package=mixOmics (accessed on 13 August 2022).
- Bernier, U.R.; Kline, D.L.; Barnard, D.R.; Schreck, C.E.; Yost, R.A. Analysis of human skin emanations by gas chromatography/mass spectrometry. 2. Identification of volatile compounds that are candidate attractants for the yellow fever mosquito (Aedes aegypti). Anal. Chem. 2000, 72, 747–756. [Google Scholar] [CrossRef]
- Brown, J.S.; Prada, P.A.; Curran, A.M.; Furton, K.G. Applicability of emanating volatile organic compounds from various forensic specimens for individual differentiation. Forensic Sci. Int. 2013, 226, 173–182. [Google Scholar] [CrossRef]
- Tavares, D.d.S.; Salgado, V.R.; Miranda, J.C.; Mesquita, P.R.R.; Rodrigues, F.d.M.; Barral-Netto, M.; de Andrade, J.B.; Barral, A. Attraction of phlebotomine sandflies to volatiles from skin odors of individuals residing in an endemic area of tegumentary leishmaniasis. PLoS ONE 2018, 13, e0203989. [Google Scholar] [CrossRef]
- Zhang, Z.-M.; Cai, J.-J.; Ruan, G.-H.; Li, G.-K. The study of fingerprint characteristics of the emanations from human arm skin using the original sampling system by SPME-GC/MS. J. Chromatogr. B 2005, 822, 244–252. [Google Scholar] [CrossRef]
- Caraballo, N.I.; Mendel, J.; Holness, H.; La Salvia, J.; Moroose, T.; Eckenrode, B.; Stockham, R.; Furton, K.; Mills, D.E. An investigation into the concurrent collection of human scent and epithelial skin cells using a non-contact sampling device. Forensic Sci. Int. 2016, 266, 148–159. [Google Scholar] [CrossRef]
- Prada, P.A.; Curran, A.M.; Furton, K.G. The Evaluation of Human Hand Odor Volatiles on Various Textiles: A Comparison Between Contact and Noncontact Sampling Methods. J. Forensic Sci. 2011, 56, 866–881. [Google Scholar] [CrossRef]
- Meijerink, J.; Braks, M.A.H.; Brack, A.A.; Adam, W.; Dekker, T.; Posthumus, M.A.; Beek, T.A.; Van Loon, J.J.A. Identification of olfactory stimulants for anopheles gambiae from human scent samples. J. Chem. Ecol. 2000, 26, 1367–1382. [Google Scholar] [CrossRef]
- Vaglio, S.; Minicozzi, P.; Bonometti, E.; Mello, G.; Chiarelli, B. Volatile signals during pregnancy: A possible chemical basis for mother-infant recognition. J. Chem. Ecol. 2009, 35, 131–139. [Google Scholar] [CrossRef]
- Colón-Crespo, L.J.; Herrera-Hernández, D.; Holness, H.; Furton, K.G. Determination of VOC marker combinations for the classification of individuals by gender and race/ethnicity. Forensic Sci. Int. 2017, 270, 193–199. [Google Scholar] [CrossRef]
- Curran, A.M.; Prada, P.A.; Furton, K.G. Canine human scent identifications with post-blast debris collected from improvised explosive devices. Forensic Sci. Int. 2010, 199, 103–108. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. CDC COVID Data Tracker: Variant Proportions. Available online: https://covid.cdc.gov/covid-data-tracker/#variant-proportions (accessed on 13 August 2022).
- Twele, F.; ten Hagen, N.A.; Meller, S.; Schulz, C.; Osterhaus, A.; Jendrny, P.; Ebbers, H.; Pink, I.; Drick, N.; Welte, T.; et al. Detection of Post-COVID-19 Patients Using Medical Scent Detection Dogs—A Pilot Study. Front. Med. 2022, 9, 877259. [Google Scholar] [CrossRef]




| SARS-CoV-2 Infection Status | Timeframe | Collection Timespan | Dominant SARS-CoV-2 Variant at Time of Collection | Number of Samples |
|---|---|---|---|---|
| Positive | Late 2021 | June 2021–October 2021 | Delta | 20 |
| Early 2022 | February 2022–May 2022 | Omicron BA.2 | 13 | |
| Mid 2022 | July 2022–September 2022 | Omicron BA.5 | 23 | |
| Negative | 2021–2022 | September 2021–October 2022 | Delta/Omicron BA.2/ Omicron BA.5 | 46 |
| Retention Time (15 M HP5-MS) | CAS# | Compound of Interest | Reported Presence in Human Skin Emanations |
|---|---|---|---|
| 3.109 | 00123-42-2 | Diacetone alcohol | - |
| 4.033 | 00100-42-5 | Styrene | [16,30] |
| 6.577 | 03777-69-3 | 2-Pentylfuran | [16,31] |
| 7.897 | 00122-78-1 | Phenylacetaldehyde | [32] |
| 9.552 | 01120-21-4 | Undecane | [16,24,25,26,31,33,34] |
| 10.366 | 00111-11-5 | Methyl caprylate | [24,25,26,31,34,35] |
| 11.235 | 18829-56-6 | trans-2-Nonenal | [16,24,25,31,35] |
| 11.679 | 00143-08-7 | 1-Nonanol | [24,31,34,35] |
| 12.561 | 00112-31-2 | Decanal | [16,24,25,26,30,31,33,35] |
| 12.836 | 00122-99-6 | 2-Phenoxyethanol | - |
| 17.798 | 00112-54-9 | Dodecanal | [24,26,30,31,35] |
| 18.841 | 00689-67-8 | 6,10-Dimethyl-5,9-undecadien-2-one-(E) | [16,24,25,26,30,31,33,34,35] |
| 19.366 | 00112-53-8 | 1-Dodecanol | [36,37] |
| 21.668 | 00143-07-7 | Dodecanoic acid | [24,30,31,35,38,39] |
| sPLS-DA Model Correct Prediction Rates * | ||||
|---|---|---|---|---|
| Time Range | 2021–2022 | Late 2021 | Early 2022 | Mid 2022 |
| Suspected Variant | All | Delta | Omicron BA.2 | Omicron BA.5 |
| Accuracy | 75.8% (±0.4) | 86.7% (±0.6) | 64.4% (±1.0) | 84.4% (±0.8) |
| Sensitivity (TPR) | 81.8% (±0.5) | 84.2% (±0.6) | 73.7% (±0.7) | 90.5% (±0.9) |
| Specificity (TNR) | 69.7% (±0.6) | 89.2% (±0.9) | 55.0% (±1.7) | 76.7% (±1.0) |
| FNR | 18.2% (±0.5) | 15.8% (±0.6) | 26.3% (±0.7) | 9.5% (±0.9) |
| FPR | 30.3% (±0.6) | 10.8% (±0.9) | 45.0% (±1.7) | 23.3% (±1.0) |
| PPV | 73.0% (±0.4) | 89.0% (±0.9) | 62.7% (±1.0) | 79.7% (±0.8) |
| NPV | 79.4% (±0.5) | 85.0% (±0.5) | 67.1% (±1.0) | 89.3% (±1.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crespo-Cajigas, J.; Gokool, V.A.; Ramírez Torres, A.; Forsythe, L.; Abella, B.S.; Holness, H.K.; Johnson, A.T.C.; Postrel, R.; Furton, K.G. Investigating the Use of SARS-CoV-2 (COVID-19) Odor Expression as a Non-Invasive Diagnostic Tool—Pilot Study. Diagnostics 2023, 13, 707. https://doi.org/10.3390/diagnostics13040707
Crespo-Cajigas J, Gokool VA, Ramírez Torres A, Forsythe L, Abella BS, Holness HK, Johnson ATC, Postrel R, Furton KG. Investigating the Use of SARS-CoV-2 (COVID-19) Odor Expression as a Non-Invasive Diagnostic Tool—Pilot Study. Diagnostics. 2023; 13(4):707. https://doi.org/10.3390/diagnostics13040707
Chicago/Turabian StyleCrespo-Cajigas, Janet, Vidia A. Gokool, Andrea Ramírez Torres, Liam Forsythe, Benjamin S. Abella, Howard K. Holness, Alan T. Charlie Johnson, Richard Postrel, and Kenneth G. Furton. 2023. "Investigating the Use of SARS-CoV-2 (COVID-19) Odor Expression as a Non-Invasive Diagnostic Tool—Pilot Study" Diagnostics 13, no. 4: 707. https://doi.org/10.3390/diagnostics13040707