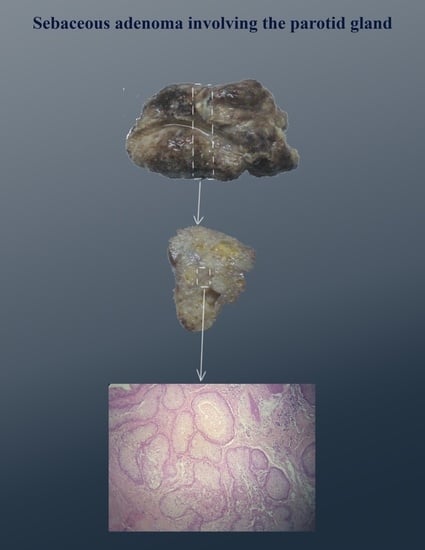
An Extremely Rare Case of Sebaceous Adenoma Involving the Parotid Gland
Abstract
:1. Introduction
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Gnepp, D.R. My Journey into the World of Salivary Gland Sebaceous Neoplasms. Head Neck Pathol. 2012, 6, 101–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ilhan, H.D.; Turkoglu, E.B.; Bilgin, A.B.; Bassorgun, I.; Dogan, M.E.; Unal, M. A Unique Case of Isolated Sebaceous Adenoma of the Bulbar Conjunctiva. Arq. Bras. Oftalmol. 2016, 79, 253–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walbeek, K.V. Adenoma of a Sebaceous Gland of the Lacrimal Caruncle. Ophthalmol. J. Int. Ophtalmol. 1949, 117, 370. [Google Scholar]
- Takayama, K.; Usui, Y.; Ito, M.; Goto, H.; Takeuchi, M. A Case of Sebaceous Adenoma of the Eyelid Showing Excessively Rapid Growth. Clin. Ophthalmol. 2013, 7, 667–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deprez, M.; Uffer, S. Clinicopathological Features of Eyelid Skin Tumors. A Retrospective Study of 5504 Cases and Review of Literature. Am. J. Dermatopathol. 2009, 31, 256–262. [Google Scholar] [CrossRef]
- Moscarella, E.; Argenziano, G.; Longo, C.; Cota, C.; Ardigò, M.; Stigliano, V.; Mete, L.S.; Donati, P.; Piana, S.; Silipo, V.; et al. Clinical, Dermoscopic and Reflectance Confocal Microscopy Features of Sebaceous Neoplasms in Muir-Torre Syndrome. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 699–705. [Google Scholar] [CrossRef]
- Ellis, G.L.; Auclair, P.L. Tumors of the Salivary Glands. In AFIP Atlas of Tumor Pathology; ARP Press: Silver Spring, MD, USA, 2008. [Google Scholar]
- Linhartová, A. Sebaceous Glands in Salivary Gland Tissue. Arch Pathol. 1974, 98, 320–324. [Google Scholar]
- Gorsky, M.; Buchner, A.; Fundoianu-Dayan, D.; Cohen, C. Fordyce’s Granules in the Oral Mucosa of Adult Israeli Jews. Community Dent. Oral Epidemiol. 1986, 14, 231–232. [Google Scholar] [CrossRef]
- Batsakis, J.G.; Littler, E.R.; Leahy, M.S. Sebaceous Cell Lesions of the Head and Neck. Arch. Otolaryngol. 1972, 95, 151–157. [Google Scholar] [CrossRef]
- Maffini, F.; Fasani, R.; Petrella, D.; Maiorano, E.; Bruschini, R.; Pelosi, G.; Viale, G. Sebaceous Lymphadenoma of Salivary Gland: A Case Report and a Review of the Literature. Acta Otorhinolaryngol. Ital. 2007, 27, 147–150. [Google Scholar]
- Auclair, P.L.; Ellis, G.L.; Gnepp, D.R. Other Benign Epithelial Neoplasms. In Surgical Pathology of the Salivary Glands; Ellis, G.L., Auclair, P.L., Gnepp, D.R., Eds.; WB Saunders Co.: Philadelphia, PA, USA, 1991; pp. 252–268. [Google Scholar]
- Som, P.M.; Curtin, H.D. Head and Neck Imaging; Mosby: St. Louis, MO, USA, 2003. [Google Scholar]
- Foote, F.W.; Frazell, E.L. Tumors of the Major Salivary Glands. Cancer 1953, 6, 1065–1133. [Google Scholar] [CrossRef]
- Bab, I.A.; Ulmansky, M. Simultaneously Occurring Salivary Gland Tumors of Different Types. J. Oral Surg. 1979, 37, 826–828. [Google Scholar] [PubMed]
- Pieterse, A.S.; Seymour, A.E. Parotid Cysts. An Analysis of 16 Cases and Suggested Classification. Pathology 1981, 13, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Gnepp, D.R.; Brannon, R. Sebaceous Neoplasms of Salivary Gland Origin. Report of 21 Cases. Cancer 1984, 53, 2155–2170. [Google Scholar] [CrossRef]
- Shen, W.C.; Kwan, P.C.; Ho, Y.J.; Lee, S.K. CT of Sebaceous Adenoma of the Parotid Gland. Am. J. Neuroradiol. 1994, 15, 1265–1266. [Google Scholar]
- Derias, N.W.; Chong, W.H.; Pambakian, H. Sebaceous Adenoma of Parotid Gland—A Rare Tumour Diagnosed by Fine Needle Aspiration Cytology. Cytopathology 1994, 5, 392–395. [Google Scholar] [CrossRef]
- Rodríguez, J.C.D.V.; Forcelledo, M.F.F.; García, M.G.; Andrea, C.A. Sebaceous Adenoma of the Parotid Gland. Medicina Oral, Patología Oral y Cirugía Bucal 2006, 11, E446–E448. [Google Scholar]
- Welch, K.C.; Papadimitriou, J.C.; Morales, R.; Wolf, J.S. Sebaceous Adenoma of the Parotid Gland in a 2-Year-Old Male. Otolaryngol. Head Neck Surg. 2007, 136, 672–673. [Google Scholar] [CrossRef]
- Apple, S.K.; Moatamed, N.A.; Lai, C.K.; Bhuta, S. Sebaceous Adenoma of the Parotid Gland: A Case Report with Fine Needle Aspiration Findings and Histologic Correlation. Acta Cytol. 2009, 53, 419–422. [Google Scholar] [CrossRef]
- Jagan, L.; Zoroquiain, P.; Bravo-Filho, V.; Logan, P.; Qutub, M.; Burnier, M.N. Sebaceous Adenomas of the Eyelid and Muir-Torre Syndrome. Br. J. Ophthalmol. 2015, 99, 909–913. [Google Scholar] [CrossRef]
- Abbott, J.J.; Hernandez-Rios, P.; Amirkhan, R.H.; Hoang, M.P. Cystic Sebaceous Neoplasms in Muir-Torre Syndrome. Arch. Pathol. Lab. Med. 2003, 127, 614–617. [Google Scholar] [CrossRef] [PubMed]
- Higgins, H.J.; Voutsalath, M.; Holland, J.M. Muir-Torre Syndrome: A Case Report. J. Clin. Aesthetic Dermatol. 2009, 2, 30–32. [Google Scholar]
- Somashekara, K.G.; Lakshmi, S.; Priya, N.S. A Rare Case of Sebaceous Adenoma of the Palate, with Literature Review. J. Laryngol. Otol. 2011, 125, 750–752. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-Y.; Chu, P.-Y.; Li, W.-Y.; Chang, S.-Y. Sebaceous Adenoma in the Submandibular Gland. Otolaryngol. Head Neck Surg. 2002, 126, 199–200. [Google Scholar] [CrossRef]
- Haynes, J.; Arnold, K.R.; Aguirre-Oskins, C.; Chandra, S. Evaluation of Neck Masses in Adults. Am. Fam. Physician 2015, 91, 698–706. [Google Scholar]
- Bialek, E.J.; Jakubowski, W.; Zajkowski, P.; Szopinski, K.T.; Osmolski, A. US of the Major Salivary Glands: Anatomy and Spatial Relationships, Pathologic Conditions, and Pitfalls. Radiographs 2006, 26, 745–763. [Google Scholar] [CrossRef] [Green Version]
- Rudack, C.; Jörg, S.; Kloska, S.; Stoll, W.; Thiede, O. Neither MRI, CT nor US is superior to diagnose tumors in the salivary glands-an extended case study. Head Face Med. 2007, 3, 19. [Google Scholar] [CrossRef] [Green Version]
- Shetty, A.; Geethamani, V. Role of fine-needle aspiration cytology in the diagnosis of major salivary gland tumors: A study with histological and clinical correlation. J. Oral Maxillofac. Pathol. 2016, 20, 224–229. [Google Scholar] [CrossRef] [Green Version]
- Alphs, H.H.; Eisele, D.W.; Westra, W.H. The role of fine needle aspiration in the evaluation of parotid masses. Curr. Opin. Otolaryngol. Head Neck Surg. 2006, 14, 62–66. [Google Scholar] [CrossRef]



| Author (Year) [Ref] | Age (Years) | Sex | Clinical Features of the Tumor | Follow-Up | |
|---|---|---|---|---|---|
| 1 | Foote and Frazell (1953) [14] | - | - | 3.5 cm mass | - |
| 2 | Bab and Ulmansky (1979) [15] | 57 | F | - | dead at 6 months of adenoid cystic carcinoma, no recurrence |
| 3 | Pieters and Seymour (1981) [16] | - | - | - | - |
| 4 | Gnepp and Brannon (1984) [17] | 71 74 | F M | 14 mm diameter mass 23 mm diameter mass | 1.5 years, no recurrence died with no evidence of disease at 6 years |
| 5 | Shen (1994) [18] | 39 | M | 5 × 6 × 4 cm mass | 19 months, no recurrence |
| 6 | Derias (1994) [19] | 73 | F | - | - |
| 7 | de Vicente Rodríguez (2006) [20] | 59 | F | 3.5 cm mass | 5 years, no recurrence |
| 8 | Welch (2007) [21] | 2 | M | 5 cm mass | - |
| 9 | Apple (2009) [22] | 29 | F | 4 cm mass | - |
| 10 | Present case (2022) | 65 | F | 3.2 × 2 × 1.6 cm mass | 4 months, no recurrence |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dincă, O.M.; Bucur, M.B.; Vlădan, G.C.; Varlas, V.N.; Bucur, A. An Extremely Rare Case of Sebaceous Adenoma Involving the Parotid Gland. Diagnostics 2022, 12, 1232. https://doi.org/10.3390/diagnostics12051232
Dincă OM, Bucur MB, Vlădan GC, Varlas VN, Bucur A. An Extremely Rare Case of Sebaceous Adenoma Involving the Parotid Gland. Diagnostics. 2022; 12(5):1232. https://doi.org/10.3390/diagnostics12051232
Chicago/Turabian StyleDincă, Octavian Marius, Mihai Bogdan Bucur, George Cristian Vlădan, Valentin Nicolae Varlas, and Alexandru Bucur. 2022. "An Extremely Rare Case of Sebaceous Adenoma Involving the Parotid Gland" Diagnostics 12, no. 5: 1232. https://doi.org/10.3390/diagnostics12051232