FHH Quick App Review: How Can a Quality Review Process Assist Primary Care Providers in Choosing a Family Health History App for Patient Care?
Abstract
:1. Introduction
1.1. FHH as First Assessment of Genetic Risk
1.2. Utility of FHH Not Fully Realized
1.3. More Examples
1.4. Determining eHealth Quality
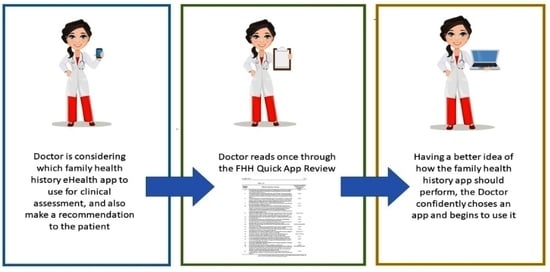
1.5. The FHH Quick App Review
2. Materials and Methods
2.1. Health App Quality Scores
2.2. Application to Family Health History
3. Results
4. Discussion
4.1. The FHH Quick App Review as a New Skill
4.2. Many Types of FHH Apps
4.3. Use in Implementation
4.4. Future Work
- Promote ISO/TS 82304-2 beyond the EU. Many other countries still do not mention the quality label on their national websites.
- The Global Alliance for Genomics and Health (GA4GH) is close to publishing its Recommendation of a Common Data Set for FHH, which includes a list of data elements that every FHH app should collect.
- The Global Genomic Medicine Consortium Family Health History Flagship Project piloting clinical FHH implementations around the world.
- Build consent systems and shared FHH risk algorithm repositories for FHH apps. Consent systems for FHH apps using locker-type systems as consent management. For example, the PGL project [27].
- Implement an FHH tool that is interoperable with other (EMR) systems. For example, through lockers and European Health Data Spaces [28].
- Case studies for finding out if and how physicians will use the FHH Quick App Review, which should be part of general eHealth education and integrated into vocational training and continuous professional development programs [29].
- With multiple stakeholders collecting and storing FHH data separately, the most efficient model would be a shared family-centric record, with access controlled by each family member to support their own needs [30].
- Include family medication history and pharmacogenomic results in the FHH pedigree to further optimize medication therapy [16].
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wildin, R.S.; Messersmith, D.J.; Houwink, E.J.F. Modernizing family health history: Achievable strategies to reduce implementation gaps. J. Community Genet. 2021, 12, 493–496. [Google Scholar] [CrossRef]
- Ginsburg, G.S.; Wu, R.R.; Orlando, L.A. Family health history: Underused for actionable risk assessment. Lancet 2019, 394, 596–603. [Google Scholar] [CrossRef]
- Hujoel, M.L.; Loh, P.R.; Neale, B.M.; Price, A.L. Incorporating family history of disease improves polygenic risk scores in diverse populations. Cell Genom. 2022, 2, 100152. [Google Scholar] [CrossRef]
- Allen, C.G.; Duquette, D.; Guan, Y.; McBride, C.M. Applying theory to characterize impediments to dissemination of community-facing family health history tools: A review of the literature. J. Community Genet. 2020, 11, 147–159. [Google Scholar] [CrossRef]
- Valdez, R.; Yoon, P.W.; Qureshi, N.; Green, R.F.; Khoury, M.J. Family History in Public Health Practice: A Genomic Tool for Disease Prevention and Health Promotion. Annu. Rev. Public Health 2010, 31, 69–87. [Google Scholar] [CrossRef]
- Wu, R.R.; Orlando, L.A. Implementation of health risk assessments with family health history: Barriers and benefits. Postgrad. Med. J. 2015, 91, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, N.; Armstrong, S.; Dhiman, P.; Saukko, P.; Middlemass, J.; Evans, P.H.; Kai, J.; ADDFAM (Added Value of Family History in CVD Risk Assessment) Study Group. Effect of Adding Systematic Family History Enquiry to Cardiovascular Disease Risk Assessment in Primary Care: A matched-pair, cluster randomized trial. Ann. Intern. Med. 2012, 156, 253–262. [Google Scholar] [CrossRef]
- Orlando, L.A.; Wu, R.R.; Myers, R.A.; Neuner, J.; McCarty, C.; Haller, I.V.; Harry, M.; Fulda, K.G.; Dimmock, D.; Rakhra-Burris, T.; et al. At the intersection of precision medicine and population health: An implementation-effectiveness study of family health history based systematic risk assessment in primary care. BMC Health Serv. Res. 2020, 20, 1015. [Google Scholar] [CrossRef]
- Wang, C.; Paasche-Orlow, M.K.; Bowen, D.J.; Cabral, H.; Winter, M.R.; Norkunas Cunningham, T.; Trevino-Talbot, M.; Toledo, D.M.; Cortes, D.E.; Campion, M.; et al. Utility of a virtual counselor (VICKY) to collect family health histories among vulnerable patient populations: A randomized controlled trial. Patient Educ. Couns. 2021, 104, 979–988. [Google Scholar] [CrossRef]
- Lin, J.; Marcum, C.S.; Myers, M.F.; Koehly, L.M. Put the Family Back in Family Health History: A Multiple-Informant Approach. Am. J. Prev. Med. 2017, 52, 640–644. [Google Scholar] [CrossRef]
- Welch, B.M.; Dere, W.; Schiffman, J.D. Family Health History: The case for better tools. JAMA 2015, 313, 1711–1712. [Google Scholar] [CrossRef]
- Houwink, E.J.; Van Teeffelen, S.R.; Muijtjens, A.M.M.; Henneman, L.; Jacobi, F.; Van Luijk, S.J.; Dinant, G.J.; Van Der Vleuten, C.; Cornel, M.C. Sustained effects of online genetics education: A randomized controlled trial on oncogenetics. Eur. J. Hum. Genet. 2014, 22, 310–316. [Google Scholar] [CrossRef]
- Manolio, T.A.; Chisholm, R.L.; Ozenberger, B.; Roden, D.M.; Williams, M.S.; Wilson, R.; Bick, D.; Bottinger, E.P.; Brilliant, M.H.; Eng, C.; et al. Implementing genomic medicine in the clinic: The future is here. Genet. Med. 2013, 15, 258–267. [Google Scholar] [CrossRef]
- David, S.P.; Johnson, S.G.; Berger, A.C.; Feero, W.G.; Terry, S.F.; Green, L.A.; Phillips, R.L.; Ginsburg, G.S. Making Personalized Health Care Even More Personalized: Insights From Activities of the IOM Genomics Roundtable. Ann. Fam. Med. 2015, 13, 373–380. [Google Scholar] [CrossRef]
- Hantula, D.A. Editorial: Reductionism and Holism in Behavior Science and Art. Perspect. Behav. Sci. 2018, 41, 325–333. [Google Scholar] [CrossRef]
- Smith, T.R.; Kearney, E.; Hulick, P.J.; Kisor, D.F. History repeats itself: The family medication history and pharmacogenomics. Pharmacogenomics 2016, 17, 669–678. [Google Scholar] [CrossRef]
- Welch, B.M.; Wiley, K.; Pflieger, L.; Achiangia, R.; Baker, K.; Hughes-Halbert, C.; Morrison, H.; Schiffman, J.; Doerr, M. Review and Comparison of Electronic Patient-Facing Family Health History Tools. J. Genet. Couns. 2018, 27, 381–391. [Google Scholar] [CrossRef]
- Cohn, W.F.; Ropka, M.E.; Pelletier, S.L.; Barrett, J.R.; Kinzie, M.B.; Harrison, M.B.; Liu, Z.; Miesfeldt, S.; Tucker, A.L.; Worrall, B.B.; et al. Health Heritage©, a Web-Based Tool for the Collection and Assessment of Family Health History: Initial User Experience and Analytic Validity. Public Health Genom. 2010, 13, 477–491. [Google Scholar] [CrossRef]
- Facio, F.M.; Feero, W.G.; Linn, A.; Oden, N.; Manickam, K.; Biesecker, L.G. Validation of My Family Health Portrait for six common heritable conditions. Genet. Med. 2010, 12, 370–375. [Google Scholar] [CrossRef]
- International Standards Organization (ISO). Available online: https://www.iso.org/home.html (accessed on 1 June 2022).
- ISO. ISO/TS 82304-2:2021 Health Software—Part 2: Health and Wellness Apps—Quality and Reliability. Available online: https://www.iso.org/standard/78182.html (accessed on 1 June 2022).
- The European Union. mHealth Label Published. Available online: https://digital-strategy.ec.europa.eu/en/news/mhealth-label-published (accessed on 1 June 2022).
- Barrett, D.; Heale, R. What are Delphi studies? Evid. Based Nurs. 2020, 23, 68–69. [Google Scholar] [CrossRef]
- Stichting Koninklijk Nederlands Normalisatie Instituut. New International Guidelines to Help to Sort the Best from the Rest. Available online: https://www.nen.nl/en/health-and-welness-apps (accessed on 1 June 2022).
- Van der Kleij, R.; Kasteleyn, M.J.; Meijer, E.; Bonten, T.N.; Houwink, E.J.; Teichert, M.; van Luenen, S.; Vedanthan, R.; Evers, A.; Car, J.; et al. SERIES: eHealth in primary care. Part 1: Concepts, conditions and challenges. Eur. J. Gen. Pract. 2019, 25, 179–189. [Google Scholar] [CrossRef]
- Table 1 Only from the Paper Cited in Reference #1 Above. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8241955/table/Tab1/?report=objectonly (accessed on 1 June 2022).
- Overkleeft, R.; Tommel, J.; Evers, A.W.M.; den Dunnen, J.T.; Roos, M.; Hoefmans, M.-J.; Schrader, W.; Swen, J.; Numans, M.; Houwink, E. Using Personal Genomic Data within Primary Care: A Bioinformatics Approach to Pharmacogenomics. Genes 2020, 11, 1443. [Google Scholar] [CrossRef]
- The European Union. European Health Data Space. Available online: https://ec.europa.eu/health/ehealth-digital-health-and-care/european-health-data-space_en (accessed on 1 June 2022).
- Houwink, E.J.F.; Kasteleyn, M.J.; Alpay, L.; Pearce, C.; Butler-Henderson, K.; Meijer, E.; Van Kampen, S.; Versluis, A.; Bonten, T.N.; Van Dalfsen, J.H.; et al. SERIES: eHealth in primary care. Part 3: eHealth education in primary care. Eur. J. Gen. Pract. 2020, 26, 108–118. [Google Scholar] [CrossRef]
- Global Genomic Medicine Collaborative. Family Health History. Available online: https://g2mc.org/family-health-history/ (accessed on 1 June 2022).

| Question Number | FHH Quick App Review Question | Derived from ISO/TS 82304-2 Question Number * |
|---|---|---|
| 1 | Who are the intended users of the FHH app? (Health professionals, patients, researchers, genetic/genomic/testing labs) | 5.2.1.1 |
| 2 | Are potential customers and users provided with adequate product information about the FHH app? (Full pedigree functionality or just a form, general or single disease focus, and use of personal data by the app, etc.) | 5.3.2.5 |
| 3 | What is the intended use or purpose of the FHH app? a./Inform–learning the value of FHH in genetic-based care. b./Simple monitoring–personal health tracking that may benefit both the patient and their family members. c./Communicate–between family members, between patient and doctor or genetic counselor, and other health services. d./Research–consenting and sharing FHH data and information with one or many research organizations. e./Calculate–FHH app generates a heritable risk assessment, a percentage risk of a genetic mutation for a relative yet to be sequenced, and relatives indicated for cascade testing. f./Diagnose–determine heritable risk, provide validated information and clinical interpretation on genetic variants, recommend appropriate genetic/genomic testing, all under physician and genetic counselor guidance (see/Communicate). g./Treat–order, schedule, and track testing, clinical use of genomics and pharmacogenomics, initiating indicated clinical surveillance, and genetic counseling. h./Preventative behavior change–makes recommendations and tracks lifestyle changes. i./Self-manage–provides tools for patients who collect and examine their medical, ‘Omic, and family health history data, along with patient-generated data (wearables, other devices). | 5.2.1.4 |
| 4 | For which health issue(s) and/or health need(s) is the FHH app intended? (a specific gene, disease?) | 5.2.1.3 |
| 5 | In which languages is the FHH app available? | 5.1.1.4 |
| 6 | Are the health risks of the health app analyzed? (Health risks may include over-reliance on the app, misinterpretation of information, medical judgments made without input from a medical professional, etc.) | 5.2.2.1 |
| 7 | Are measures in place to control the health risks of the FHH app? (Is there information covering user safety, including warnings and limitations of use? Is user training offered? Is there documented verification and validation of risk reports and algorithms used by the app, etc.) | 5.2.2.2 |
| 8 | Are the residual risks of using the health app found to be acceptable? Is a consent system in place for patient privacy and security (data sharing options explained, data hiding or limiting options available with family members, healthcare providers, medical systems, protecting paternity confidences, how is de-identified data created, etc.)? | 5.2.2.3 |
| 9 | Is a process in place to collect and review safety concerns and incidents for the FHH app? (how can users report incidents or issues)? | 5.2.2.6 |
| 10 | Are ethical challenges of the health app assessed with both health professionals and intended users in mind? (information not used for health insurance qualification, being sensitive to cultural issues, how to report medically actionable health risks without causing undue concern, understanding the role of biological relationships vs. non-biological and chromosomal sex for risk assessment purposes, respecting the privacy of the user’s family members, etc.)? | 5.2.3.1 |
| 11 | Describe the health benefits of using the FHH app. Are potential users made aware of the health interventions applied to achieve the health benefits? Is there a review of possible interventions that could be ordered or performed by the Primary Care physician? | 5.2.4.1, 5.2.4.2 |
| 12 | Are potential users made aware of the need for support of a health professional to achieve the health benefits? | 5.2.4.2 |
| 13 | Are potential users made aware of the financial costs to achieve the health benefits? (out-of-pocket costs for laboratory testing and other interventions) | 5.2.4.3 |
| 14 | Are there maintenance processes for the health information in the FHH app by the app developer? Are all sources for the health information disclosed to users? | 5.2.4.6 |
| 15 | Does the FHH app encourage and track the user by keeping the pedigree and FHH information up to date? | Not derived from ISO |
| 16 | Is the design of the FHH app driven and refined by user-centered evaluation? Is the app design based on an explicit understanding of users, tasks, and environment? | 5.3.2.3 |
| 17 | Are measures in place to avoid user error and reasonably foreseeable misuse of the health app? (Input error detection, context-sensitive help, etc.) | 5.3.2.4 |
| 18 | Are instructions for use readily available for users? Are appropriate resources available to adequately help users who experience problems with the app? | 5.3.2.6, 5.3.2.7 |
| 19 | Is a privacy statement readily available to potential users of the FHH app? Is an appropriate retention policy established to erase or review the data stored? | 5.4.1.1.3, 5.4.1.1.4 |
| 20 | Is a secure by design process followed? (Security by design ensures that information security is designed and implemented within the development lifecycle of the app.) | 5.4.2.3 |
| 21 | Is user authentication, authorization, and session management implemented to secure access to the health app? (The identity of an app user is authenticated prior to access of any personal identifying information.) | 5.4.2.7 |
| 22 | Are security vulnerabilities reported, identified, assessed, logged, responded to, disclosed, and quickly and effectively resolved? | 5.4.2.9 |
| 23 | Is the information security policy readily available to potential users? | 5.4.2.11 |
| 24 | Is data interoperability achieved via published FHH data standards like HL7 FHIR (Fast Healthcare Interoperability Resources) and GA4GH (Global Alliance for Genomics and Health)? Are certified interoperable systems listed (what other apps, data repositories, and major medical systems does the app communicate with)? | Not derived from ISO |
| 25 | Can users obtain or share their health-related PII by a data import/export from/to another FHH app or platform? Can the app import pedigree data from other genealogical services? | 5.5.2.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wood, G.M.; van Boom, S.; Recourt, K.; Houwink, E.J.F. FHH Quick App Review: How Can a Quality Review Process Assist Primary Care Providers in Choosing a Family Health History App for Patient Care? Genes 2022, 13, 1407. https://doi.org/10.3390/genes13081407
Wood GM, van Boom S, Recourt K, Houwink EJF. FHH Quick App Review: How Can a Quality Review Process Assist Primary Care Providers in Choosing a Family Health History App for Patient Care? Genes. 2022; 13(8):1407. https://doi.org/10.3390/genes13081407
Chicago/Turabian StyleWood, Grant M., Sander van Boom, Kasper Recourt, and Elisa J. F. Houwink. 2022. "FHH Quick App Review: How Can a Quality Review Process Assist Primary Care Providers in Choosing a Family Health History App for Patient Care?" Genes 13, no. 8: 1407. https://doi.org/10.3390/genes13081407