Optimal Morphometric Characteristics of a Tubular Polymeric Scaffold to Promote Peripheral Nerve Regeneration: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Systematic Literature Search
2.2. Eligibility Criteria
2.3. Article Selection and Data Extraction
3. Results
3.1. Study Selection
3.2. Characteristics of the Selected Studies
4. Discussion
4.1. Polymers
4.2. Quantitative Characteristics
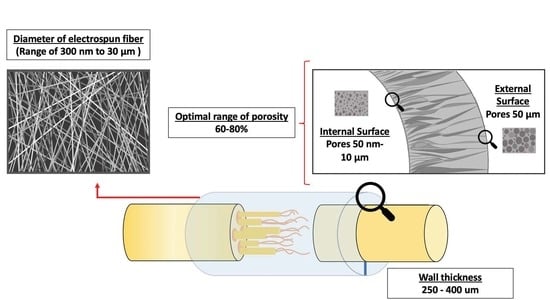
4.2.1. Scaffold Wall Thickness
4.2.2. Permeability
Porosity of the Scaffold
Pore Size
4.2.3. Diameter of Electrospun Fiber
4.3. Methods and Processing Parameters to Produce NGC
4.3.1. Electrospinning
4.3.2. Immersion–Precipitation Method and Immersion–Precipitation Phase Inversion Using a Casting Process
4.3.3. NaCl Used as a Porosifying Agent
4.3.4. Freeze-Drying and Freeze-Casting Methods
4.4. Mechanical Properties of the Scaffolds
4.4.1. Mechanical Properties and Polymeric Biomaterial
4.4.2. Influence of Morphometric Characteristics on Mechanical Properties
4.5. Biodegradable NGC Properties
4.6. NGC Hydrophilicity
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NGC | Nerve Guide Conduit |
| ECM | Extracellular matrix |
| PNS | Peripheral Nervous System |
| CNS | Central Nervous System |
| SC | Schwann cell |
| NTF | Neurotrophic factor |
| NSC | Neural stem cell |
| DRG | Dorsal root ganglia |
References
- Madduri, S.; Gander, B. Growth factor delivery systems and repair strategies for damaged peripheral nerves. J. Control. Release 2012, 161, 274–282. [Google Scholar] [CrossRef]
- Li, R.; Liu, Z.; Pan, Y.; Chen, L.; Zhang, Z.; Lu, L. Peripheral nerve injuries treatment: A systematic review. Cell Biochem. Biophys. 2014, 68, 449–454. [Google Scholar] [CrossRef]
- Du, J.; Chen, H.; Qing, L.; Yang, X.; Jia, X. Biomimetic neural scaffolds: A crucial step towards optimal peripheral nerve regeneration. Biomater. Sci. 2018, 6, 1299–1311. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.I.; Hwang, T.I.; Aguilar, L.E.; Park, C.H.; Kim, C.S. Controlled Design of Aligned and Random Nanofibers for 3D Bi-functionalized Nerve Conduits Fabricated via a Novel Electrospinning Set-up. Sci. Rep. 2016, 6, 23761. [Google Scholar] [CrossRef] [Green Version]
- Jiang, X.; Mi, R.; Hoke, A.; Chew, S.Y. Nanofibrous nerve conduit-enhanced peripheral nerve regeneration. J. Tissue Eng. Regen. Med. 2014, 8, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Wood, M.D.; Kemp, S.W.; Weber, C.; Borschel, G.H.; Gordon, T. Outcome measures of peripheral nerve regeneration. Ann. Anat—Anat. Anz. 2011, 193, 321–333. [Google Scholar] [CrossRef]
- Allodi, I.; Udina, E.; Navarro, X. Specificity of peripheral nerve regeneration: Interactions at the axon level. Prog. Neurobiol. 2012, 98, 16–37. [Google Scholar] [CrossRef] [PubMed]
- Lizarraga-Valderrama, L.R.; Taylor, C.S.; Claeyssens, F.; Haycock, J.W.; Knowles, J.C.; Roy, I. Unidirectional neuronal cell growth and differentiation on aligned polyhydroxyalkanoate blend microfibres with varying diameters. J. Tissue Eng. Regen. Med. 2019, 13, 1581–1594. [Google Scholar] [CrossRef]
- Quan, Q.; Meng, H.Y.; Chang, B.; Liu, G.B.; Cheng, X.Q.; Tang, H.; Wang, Y.; Peng, J.; Zhao, Q.; Lu, S.B. Aligned fibers enhance nerve guide conduits when bridging peripheral nerve defects focused on early repair stage. Neural Regen. Res. 2019, 14, 903–912. [Google Scholar] [CrossRef]
- Hu, J.; Tian, L.; Prabhakaran, M.P.; Ding, X.; Ramakrishna, S. Fabrication of Nerve Growth Factor Encapsulated Aligned Poly(ε-Caprolactone) Nanofibers and Their Assessment as a Potential Neural Tissue Engineering Scaffold. Polymers 2016, 8, 54. [Google Scholar] [CrossRef]
- Yao, L.; de Ruiter, G.C.; Wang, H.; Knight, A.M.; Spinner, R.J.; Yaszemski, M.J.; Windebank, A.J.; Pandit, A. Controlling dispersion of axonal regeneration using a multichannel collagen nerve conduit. Biomaterials 2010, 5789–5797. [Google Scholar] [CrossRef]
- Oh, S.H.; Kim, J.H.; Song, K.S.; Jeon, B.H.; Yoon, J.H.; Seo, T.B.; Namgung, U.; Lee, I.W.; Lee, J.H. Peripheral nerve regeneration within an asymmetrically porous PLGA/Pluronic F127 nerve guide conduit. Biomaterials 2008, 1601–1609. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.J.; Hsu, S.H.; Yen, H.J.; Chang, H.; Hsu, S.K. Effects of unidirectional permeability in asymmetric poly(DL-lactic acid-co-glycolic acid) conduits on peripheral nerve regeneration: An in vitro and in vivo study. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 83, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Panahi-Joo, Y.; Karkhaneh, A.; Nourinia, A.; Abd-Emami, B.; Negahdari, B.; Renaud, P.; Bonakdar, S. Design and fabrication of a nanofibrous polycaprolactone tubular nerve guide for peripheral nerve tissue engineering using a two-pole electrospinning system. Biomed. Mater. 2016, 11, 025017. [Google Scholar] [CrossRef] [Green Version]
- Haider, A.; Haider, S.; Rao, K.M.; Kamal, T.; Alghyamah, A.A.A.; Jan, I.F.; Bano, B.; Khan, N.; Amjid, A.M.; Soon, H.S.; et al. Advances in the Scaffolds fabrication techniques using biocompatible polymers and their biomedical application: A Technical and Statistical Review. J. Saudi Chem. Soc. 2020, 24, 186–215. [Google Scholar] [CrossRef]
- Xue, J.; Wu, T.; Dai, Y.; Xia, Y. Electrospinning and Electrospun Nanofibers: Methods, Materials, and Applications. Chem. Rev. 2019, 119, 5298–5415. [Google Scholar] [CrossRef] [PubMed]
- Geetha, B.R.; Muthoosamy, K.; Manickam, S.; Hilal-Alnaqbi, A. Graphene-based 3D scaffolds in tissue engineering: Fabrication, applications, and future scope in liver tissue engineering. Int. J. Nanomed. 2019, 14, 5753–5783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lietz, M.; Ullrich, A.; Schulte-Eversum, C.; Oberhoffner, S.; Fricke, C.; Müller, H.W.; Schlosshauer, B. Physical and biological performance of a novel block copolymer nerve guide. Biotechnol. Bioeng. 2006, 93, 99–109. [Google Scholar] [CrossRef]
- Hwang, C.M.; Khademhosseini, A.; Park, Y.; Sun, K.; Lee, S.H. Microfluidic chip-based fabrication of PLGA microfiber scaffolds for tissue engineering. Langmuir 2008, 24, 6845–6851. [Google Scholar] [CrossRef]
- Mu, Y.; Wu, F.; Lu, Y.; Wei, L.; Yuan, W. Progress of electrospun fibers as nerve conduits for neural tissue repair. Nanomedicine 2014, 9, 1869–1883. [Google Scholar] [CrossRef]
- Subramanian, A.; Krishnan, U.M.; Sethuraman, S. Development of biomaterial scaffold for nerve tissue engineering: Biomaterial mediated neural regeneration. J. Biomed. Sci. 2009, 16, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gnavi, S.; Fornasari, B.E.; Tonda-Turo, C.; Laurano, R.; Zanetti, M.; Ciardelli, G.; Geuna, S. In vitro evaluation of gelatin and chitosan electrospun fibres as an artificial guide in peripheral nerve repair: A comparative study. J. Tissue Eng. Regen. Med. 2018, 12, e679–e694. [Google Scholar] [CrossRef] [PubMed]
- Pateman, C.J.; Harding, A.J.; Glen, A.; Taylor, C.S.; Christmas, C.R.; Robinson, P.P.; Rimmer, S.; Boissonade, F.M.; Claeyssens, F.; Haycock, J.W. Nerve guides manufactured from photocurable polymers to aid peripheral nerve repair. Biomaterials 2015, 49, 77–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Apablaza, J.A.; Lezcano, M.F.; Lopez Marquez, A.; Godoy Sánchez, K.; Oporto, G.H.; Dias, F.J. Main Morphological Characteristics of Tubular Polymeric Scaffolds to Promote Peripheral Nerve Regeneration-A Scoping Review. Polymers 2021, 13, 2563. [Google Scholar] [CrossRef] [PubMed]
- Mobasseri, A.; Faroni, A.; Minogue, B.M.; Downes, S.; Terenghi, G.; Reid, A.J. Polymer scaffolds with preferential parallel grooves enhance nerve regeneration. Tissue Eng. Part A 2015, 21, 1152–1162. [Google Scholar] [CrossRef] [Green Version]
- Isaacs, J.; Mallu, S.; Yan, W.; Little, B. Consequences of oversizing: Nerve-to-nerve tube diameter mismatch. J. Bone. J. Sur. Am. 2014, 96, 1461–1467. [Google Scholar] [CrossRef]
- Shin, R.H.; Friedrich, P.F.; Crum, B.A.; Bishop, A.T.; Shin, A.Y. Treatment of a segmental nerve defect in the rat with use of bioabsorbable synthetic nerve conduits: A comparison of commercially available conduits. J. Bone Jt. Surgery Am. Vol. 2009, 91, 2194–2204. [Google Scholar] [CrossRef] [PubMed]
- Wen, X.; Tresco, P.A. Effect of filament diameter and extracellular matrix molecule precoating on neurite outgrowth and Schwann cell behavior on multifilament entubulation bridging device in vitro. J. Biomed. Mater. Res. A 2006, 76, 626–637. [Google Scholar] [CrossRef]
- Wang, H.B.; Mullins, M.E.; Cregg, J.M.; McCarthy, C.W.; Gilbert, R.J. Varying the diameter of aligned electrospun fibers alters neurite outgrowth and Schwann cell migration. Acta. Biomater. 2010, 6, 2970–2978. [Google Scholar] [CrossRef]
- Kim, Y.T.; Haftel, V.K.; Kumar, S.; Bellamkonda, R.V. The role of aligned polymer fiber-based constructs in the bridging of long peripheral nerve gaps. Biomaterials 2008, 29, 3117–3127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranjbar-Mohammadi, M.; Prabhakaran, M.P.; Bahrami, S.H.; Ramakrishna, S. Gum tragacanth/poly(l-lactic acid) nanofibrous scaffolds for application in regeneration of peripheral nerve damage. Carbohydr. Polym. 2016, 140, 104–112. [Google Scholar] [CrossRef]
- Jia, Y.; Yang, W.; Zhang, K.; Qiu, S.; Xu, J.; Wang, C.; Chai, Y. Nanofiber arrangement regulates peripheral nerve regeneration through differential modulation of macrophage phenotypes. Acta. Biomater. 2019, 83, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Den Dunnen, W.F.; Meek, M.F.; Robinson, P.H.; Schakernraad, J.M. Peripheral nerve regeneration through P(DLLA-epsilon-CL) nerve guides. J. Mater. Sci. Mater. Med. 1998, 9, 811–814. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Rutkowski, G.E.; Heath, C.A. Development of a bioartificial nerve graft. I. Design based on a reaction-diffusion model. Biotechnol. Prog. 2002, 18, 362–372. [Google Scholar] [CrossRef]
- Rutkowski, G.E.; Heath, C.A. Development of a bioartificial nerve graft. II. Nerve regeneration in vitro. Biotechnol. Prog. 2002, 18, 373–379. [Google Scholar] [CrossRef]
- Den Dunnen, W.F.A.; Van Der Lei, B.; Robinson, P.H.; Holwerda, A.; Pennings, A.J.; Schakenraad, J.M. Biological performance of a degradable poly (lactic acid-ε-caprolactone) nerve guide: Influence of tube dimensions. J. Biomed. Mater. Res. 1995, 29, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Murugan, R.; Wang, S.; Ramakrishna, S. Electrospinning of nano/micro scale poly(L-lactic acid) aligned fibers and their potential in neural tissue engineering. Biomaterials 2005, 26, 2603–2610. [Google Scholar] [CrossRef]
- Yao, L.; O’Brien, N.; Windebank, A.; Pandit, A. Orienting neurite growth in electrospun fibrous neural conduits. J. Biomed. Mater. Res. Appl. Biomater. 2009, 90, 483–491. [Google Scholar] [CrossRef]
- Wang, J.; Ye, R.; Wei, Y.; Wang, H.; Xu, X.; Zhang, F.; Qu, J.; Zuo, B.; Zhang, H. The effects of electrospun TSF nanofiber diameter and alignment on neuronal differentiation of human embryonic stem cells. J. Biomed. Mater. Res. A 2012, 100, 632–645. [Google Scholar] [CrossRef]
- Daud, M.F.; Pawar, K.C.; Claeyssens, F.; Ryan, A.J.; Haycock, J.W. An aligned 3D neuronal-glial co-culture model for peripheral nerve studies. Biomaterials 2012, 33, 5901–5913. [Google Scholar] [CrossRef] [PubMed]
- Gnavi, S.; Fornasari, B.E.; Tonda-Turo, C.; Ciardelli, G.; Zanetti, M.; Geuna, S.; Perroteau, I. The influence of electrospun fibre size on Schwann cell behaviour and axonal outgrowth. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 48, 620–631. [Google Scholar] [CrossRef]
- Oh, S.H.; Lee, J.H. Fabrication and characterization of hydrophilized porous PLGA nerve guide conduits by a modified immersion precipitation method. J. Biomed. Mater. Res. A 2007, 80, 530–538. [Google Scholar] [CrossRef]
- Kokai, L.E.; Lin, Y.C.; Oyster, N.M.; Marra, K.G. Diffusion of soluble factors through degradable polymer nerve guides: Controlling manufacturing parameters. Acta Biomater. 2009, 5, 2540–2550. [Google Scholar] [CrossRef]
- Pawelec, K.M.; Hix, J.; Shapiro, E.M.; Sakamoto, J. The mechanics of scaling-up multichannel scaffold technology for clinical nerve repair. J. Mech. Behav. Biomed. Mater. 2019, 91, 247–254. [Google Scholar] [CrossRef]
- Ghorbani, F.; Zamanian, A.; Nojehdehian, H. Effects of pore orientation on in-vitro properties of retinoic acid-loaded PLGA/gelatin scaffolds for artificial peripheral nerve application. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 77, 159–172. [Google Scholar] [CrossRef]
- Huang, L.; Zhu, L.; Shi, X.; Xia, B.; Liu, Z.; Zhu, S.; Yang, Y.; Ma, T.; Cheng, P.; Luo, K.; et al. A compound scaffold with uniform longitudinally oriented guidance cues and a porous sheath promotes peripheral nerve regeneration in vivo. Acta Biomater. 2018, 68, 223–236. [Google Scholar] [CrossRef]
- Vijayavenkataraman, S.; Zhang, S.; Thaharah, S.; Sriram, G.; Lu, W.F.; Fuh, J. Electrohydrodynamic Jet 3D Printed Nerve Guide Conduits (NGCs) for Peripheral Nerve Injury Repair. Polymers 2018, 10, 753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, C.J.; Hsu, S.H. The effect of high outflow permeability in asymmetric poly(dl-lactic acid-co-glycolic acid) conduits for peripheral nerve regeneration. Biomaterials 2006, 27, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Vleggeert-Lankamp, C.L.A.M.; de Ruiter, G.C.W.; Wolfs, J.F.C.; Pêgo, A.P.; van den Berg, R.J.; Feirabend, H.K.P.; Malessy, M.J.A.; Lakke, E.A.J.F. Pores in synthetic nerve conduits are beneficial to regeneration. J. Biomed. Mater. Res. A. 2007, 80, 965–982. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.H.; Kim, J.R.; Kwon, G.B.; Namgung, U.; Song, K.S.; Lee, J.H. Effect of surface pore structure of nerve guide conduit on peripheral nerve regeneration. Tissue Eng. Part C Methods 2013, 19, 233–243. [Google Scholar] [CrossRef]
- Choi, J.S.; Oh, S.H.; An, H.Y.; Kim, Y.M.; Lee, J.H.; Lim, J.Y. Functional regeneration of recurrent laryngeal nerve injury during thyroid surgery using an asymmetrically porous nerve guide conduit in an animal model. Thyroid 2014, 24, 52–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Liu, X.; Zeng, L.; Zhang, J.; Zuo, J.; Zou, J.; Chen, X. Polymer Fiber Scaffolds for Bone and Cartilage Tissue Engineering. Adv. Funct. Materials 2019, 29, 1903279. [Google Scholar] [CrossRef]
- Masaeli, E.; Morshed, M.; Nasr-Esfahani, M.H.; Sadri, S.; Hilderink, J.; Van Apeldoorn, A.; Van Blitterswijk, C.A.; Moroni, L. Fabrication, characterization and cellular compatibility of poly (hydroxy alkanoate) composite nanofibrous scaffolds for nerve tissue engineering. PLoS ONE 2013, 8, e57157. [Google Scholar] [CrossRef] [PubMed]
- Gnavi, S.; Fornasari, B.E.; Tonda-Turo, C.; Laurano, R.; Zanetti, M.; Ciardelli, G.; Geuna, S. The Effect of Electrospun Gelatin Fibers Alignment on Schwann Cell and Axon Behavior and Organization in the Perspective of Artificial Nerve Design. Int. J. Mol. Sci. 2015, 16, 12925. [Google Scholar] [CrossRef]
- Perego, G.; Cella, G.D.; Aldini, N.; Fini, M.; Giardino, R. Preparation of a new nerve guide from a poly(L-lactide-co-6-caprolactone). Biomaterials 1994, 15, 189–193. [Google Scholar] [CrossRef]
- Loh, Q.L.; Choong, C. Three-dimensional scaffolds for tissue engineering applications: Role of porosity and pore size. Tissue Eng. Part B Rev. 2013, 19, 485–502. [Google Scholar] [CrossRef] [Green Version]
- Neal, R.A.; Tholpady, S.S.; Foley, P.L.; Swami, N.; Ogle, R.C.; Botchwey, E.A. Alignment and composition of laminin-polycaprolactone nanofiber blends enhance peripheral nerve regeneration. J. Biomed. Mater. Res. A 2012, 100, 406–423. [Google Scholar] [CrossRef] [Green Version]




| Study | Type of Study | NGC Material | Quantitative Parameters | Main Outcome |
|---|---|---|---|---|
| Rutkowski et al., 2008 [35] | In vitro (In silico): Schwann cell cultures. Dorsal root ganglia (DRG) of Sprague. | Bioartificial nerve graft (BNG) composed of a tubular conduit of poly-D, L-lactide | Computer model predicting the wall thickness, porosity, and Schwann cell seeding density needed to maximize the axon extension rate and ensuring sufficient nutrients to the neurons. | Low porosity, greater wall and Schwann cell layer thickness led to a decrease in the amount of oxygen available to the axons and greater NGF concentrations. |
| Rutkowski et al., 2008 [36] | In vitro: SC Cultures. DRG of Sprague–Dawley rats. | Bioartificial nerve graft (BNG) composed of a tubular conduit of poly-D, L-lactide with Schwann cells | Porosities: 0.55–0.95 Wall thickness: 0.56–1.47 mm | Reduced axon growth in conduits with wall thicknesses greater than 0.81 mm, a greater wall thickness, and lower porosities have a detrimental effect on the growth of the axons. |
| Mobasseri et al., 2015 [25] | In vitro: stem cells differentiated to Schwann cell-like cells. In vivo: Sprague–Dawley rat sciatic nerve injury (n = 24). | Poly ε-caprolactone (PCL) and polylactic acid (PLA) | Wall thickness: 70, 100, 120, 210 µm | Increasing the wall thickness also increases stiffness and limits the permeability of the canal, so it did not show any positive effect on the biological response of the regenerating nerve. |
| Pateman et al., 2015 [23] | In vitro: SC and DRG. In vivo: common fibular nerve of mouse (n = 18). | poly(ethylene glycol) (PEG) | Wall thickness: 250 μm | NGC with 1 mm (internal diameter), 5 mm (long) and 250 μm wall thickness supported reinnervation through a 3 mm lesion space after 21 days, similar results to an autograft control. |
| Den Dunnen et al., 1995 [37] | In vivo: Sciatic nerve of rat (n = 24). | 50% lactic acid (LA) and 50% e-caprolactone (CL) | Type 1: N° of dip-coated: 2, Int. diameter: 1.23 mm Wall thickness: 0.34 mm. Type 2: N° of dip-coated: 3, Int. diameter:1.18 mm Wall thickness: 0.43 mm. Type 3: N° of dip-coated: 4, Int. diameter: 1.15 mm Wall thickness: 0.64 mm. Type 4: N° of dip-coated: 5 Int. diameter: 1.12 mm Wall thickness: 0.68 mm. | Better nerve regeneration with Type 1 (large amount of targeted neural tissue, a minimal amount of fibrous or scar tissue, and a normal amount and distribution of blood). Type 2: more fibrous tissue and had less favorable nerve regeneration due to nerve compression. Types 3 and 4: bone exposed by severe self-mutilation. Due to the swelling, the NGC lumen completely disappeared. |
| Den Dunnen et al., 1998 [33] | In vivo: Sciatic nerve of rat (n = 30). | Copolymer of DL-lactide and e-caprolactone | Type 1: N° of dip-coated: 2, Int. diameter: 1.23 mm Wall thickness: 0.34 mm. Type 2: N° of dip-coated:3, Int. diameter:1.18 mm Wall thickness: 0.43 mm. Type 3: N° of dip-coated:4, Int. diameter: 1.15 mm Wall thickness: 0.64 mm. Type 4: N° of dip-coated: 5 Int. diameter: 1.12 mm Wall thickness: 0.68 mm. | Thicker NGC wall: swelling of the degrading biomaterial will be so severe that the NGC becomes occluded. Thinner NGC wall: the nerve guides collapsed. Peripheral nerve regeneration across a 10 mm nerve gap inside a P(DLLA-e-CL) nerve guide was faster and qualitatively better in comparison with a 7 mm long autologous nerve graft. |
| Study | Type of Study | NGC Material | Technique | Diameter of Fibers | Main Outcome |
|---|---|---|---|---|---|
| Wen X. et al., 2005 [28] | In vitro: DRG explants | Poly(acrylonitrile-co-vinyl chloride) (PAN-PVC) | Wet-phase inversion process | Diameters: 5 ± 1.58, 30 ± 1.26, 100 ± 1.41, 200 ± 2.03, 500 ± 3.66 μm | 5 and 30 μm-diameter filaments increase the neurite outgrowth and SC migration. Robust and uniformly distributed neuronal growth was achieved with highly directional filaments. |
| Yang F. et al., 2005 [38] | In vitro: Neural stem cells (NSCs) | Poly(L-lactic acid) (PLLA) | Electrospinning | Aligned fibers: 300 nm nanometer scale 1.5 μm submicron scale | No significant changes to cell orientation were associated with fiber diameters. NSC differentiation was higher for PLLA nanofibers than microfibers, independent of their alignment. The main growing direction of NSC neurites was parallel to nano and microfibers. |
| Yao L.et al., 2009 [39] | In vitro: PC12 cells | Poly(caprolactone) (PCL) | Electrospinning | Randomly oriented fibers: 4.4 ± 0.5 μm. Aligned oriented fibers: 0.8 ± 0.7, 3.7 ± 0.5, 5.9 ± 0.9, 8.8 ± 0.9 μm. | PC12 cells’ neurites showed similar parallel growth on the aligned fibers irrespective of fiber diameter. Neurite length on aligned fibers (fiber Φ: 3.7 ± 0.5 and 5.9 ± 0.9 μm), was longer than neurite length on randomly oriented fibers. |
| Wang HB. et al., 2010 [29] | In vitro: Dorsal root ganglia (DRG) | Poly-L-lactic acid (PLLA) | Electrospinning | Highly aligned, electro-spun fiber scaffolds, fiber diameters: Large:1325 + 383 nm interm.:759 + 179 nm small: 293 + 65 nm | Small diameter: did not promote extensive neurite extension or SC migration. Intermediate diameter: promoted long, directed neurite extension independent of SC migration. Large diameter: promoted long, directed neurite extension and SC migration. |
| Junxia Wang, et al., 2012 [40] | In vitro: human embryonic stem cells (hESCs) | Tussah silk fibroin (TSF) | Electrospinning | Different diameter: 400 and 800 nm | Neurite outgrowth along the fibers was longer on aligned 400 nm TSF-scaffold than on-aligned 800 nm TSF-scaffold. 400 nm aligned TSF scaffold supports survival and promotes neuronal differentiation of hESC-derived NPs. |
| Daud M.F.B., et al., 2012 [41] | In vitro: I. neuronal or primary SC cultures; II. Neuronal and primary SC in co-culture; III. Isolated DRG cultures, containing both neuronal and SC. | Poly(caprolactone) | Electrospinning | Diameters: 1, 5 and 8 μm | For neuronal cells alone, 8 μm fibers promoted better neurite outgrowth. For neuronal cells plus primary SC or DRG explants, 1 μm fibers supported superior neurite outgrowth, SC migration, and elongation in comparison with 5 and 8 μm fibers. |
| Gnavi S. et al., 2014 [42] | In vitro: Explant cultures of SC and DRG Ex vivo: SC | Gelatin | Electrospinning | Nanofibrous matrices, diameters: 300 or 600 nm, 1000 or 1300 nm | Nanofibers (300 nm) promoted cell spreading and actin cytoskeleton organization, increasing cellular adhesion and SC proliferation rate. Migration rate and motility, axonal density was greater in cells cultured on microfibers (1300 nm). Microfibers promoted SC migration and axonal outgrowth. Nanofibers promoted SC proliferation and adhesion. |
| Hu J. et al., 2016 [10] | In vitro: PC12 cells | Poly(ε-caprolactone) (PCL)-Nerve Growth Factor (NGF) and Bovine Serum Albumin (BSA) | Emulsion electrospinning technique | Diameter Random: 343 ± 113 nm; 320 ± 97 nm; 371 ± 95 nm; 343 ± 113 nm Aligned: 354 ± 91 nm; 302 ± 70 nm; 333 ± 90 nm; 320 ± 87 nm. | Aligned nanofibers presented similar diameters to randomly aligned nanofibers, but the aligned nanofibers were more uniform. PC12 neurite length on PCL-NGF and BSA scaffold (diameter 320 ± 87) was higher on aligned nanofibers (70.17 μm) compared to randomly aligned nanofibers (41.67 μm). |
| Lizarraga LR. et al., 2019 [8] | In vitro: NG108-15 neuronal cells and Schwann cells | Poly(3-hydroxybutyrate) P(3HB) poly(3-hydroxyoctanoate) P(3HO) 25:75 % P(3HO)/P(3HB) blend (PHA blend) | Electrospinning | Highly aligned and uniform fibers diameters: Small: 2.4 ± 0.3 μm Medium: 3.7 ± 0.3μm Large: 13.5 ± 2.3 μm | A direct correlation between fiber diameter and neuronal growth and differentiation was noted. Highly aligned large fibers (13.50 ± 2.33 μm) resulted in better neurite outgrowth and higher neuronal cell differentiation in co-culture. With RN22 SC, the number of NG108-15 cells increased as the fiber diameter increased. |
| Jiang et al., 2012 [5] | In vivo: sciatic nerve injury model in female Sprague–Dawley rats (n = 26). | Poly(ε-caprolactone) (PCL) | Electrospinning | Microfibers (981 ± 83 nm) and nanofibers (251 ± 32 nm) | Nanofiber NGC resulted in a higher number of myelinated axons, thicker myelin sheaths, an increase in regenerated DRG sensory neurons, and functional recovery compared to microfiber and film NGC. Nanofiber conduits possessed a smaller pore size compared to microfiber conduits. |
| Study | Type of Study | Material | Technique | Porosity, Size or Distribution of Pores | Main Outcome |
|---|---|---|---|---|---|
| Oh et al., 2007 [43] | Pre-experimental study of biomaterials development | Poly(lactic-co-glycolic acid) PLGA and Pluronic F127 | Modified immersion precipitation | Inner tube surface: nano-pores ~50 nm/Outer tube surface: micropores ~50 μm | PLGA/F127 tube (3 wt%): optimal mechanical properties and hydrophilicity. Highly effective for nutrient permeability. The tubes show a decrease in mechanical resistance with an increase in the Pluronic F127 compositions. |
| Kokai et al., 2009 [44] | Pre-experimental study of biomaterials development | Poly(caprolactone) (PCL) | Dip-coating/ salt-leaching technique | Wall thickness: 0.2, 0.6 mm Porosities: 50, 80% Pore size:10–38; 75–150 μm | NGC (0.6 mm) decreased lysozyme loss (~10%) without diminishing glucose permeability. Low porosity NGC (50% porous) showed smooth inner walls and several blind-ended or closed pores. High porosity NGC (80%) showed fewer smooth walls with highly interconnected through-pores for transluminal flow and solute diffusion. NGC (0.6 mm; 10–38 μm pores, 50% porous) were almost impermeable for glucose and lysozyme. |
| Pawelec et al., 2019 [45] | Pre-experimental study of biomaterials development | Poly(lactide co-glycolide) (PLGA) Poly(caprolactone) (PCL) | Polymer and salt slurry | Relative density of porous films 70 vol% porosity and non-porous films Wall thickness: 61.5–150 µm | Porosity in the scaffold increased compliance from 0.05 ± 0.1 in non-porous PCL to 1.75 ± 0.2 in porous PCL. Porosity decreased flexural stiffness (×10−2 N / mm) from 57.40 ± 16.0 in non-porous PCL to 0.88 ± 0.4 in non-porous. In addition, the porous PLGA scaffolds were approximately 30 times stiffer than the porous PCL with higher deformation. On the other hand, the deformation behavior of the scaffolds depended to a great extent on the material. Porous PCL scaffolds exhibited less than 30% permanent deformation after compression. In contrast, the porous PLGA scaffolds experienced a deformation of more than 45%. |
| Kim et al., 2016 [4] | In vitro: PC12 and S42 cells | Poly lactic-co-glycolic acid (PLGA) and polyurethane (PU) | Electrospinning | Highly-aligned nanofibers and randomly-oriented nanofibers on a single mat with nano to micro sized pores (50 nm–5 μm) | The average diameter of the pores in the aligned nanofibrous mat is three times larger than that in the randomly-oriented mat. The porosity of the aligned nanofibrous scaffolds was higher. Aligned nanofibers served as a guide for neural cells and were able to achieve a higher cell proliferation and migration compared to randomly oriented nanofibers. |
| Ghorbani et al., 2017 [46] | In vitro: L929 fibroblast cells | Poly (lactic-co-glycolic acid) (PLGA) | Freeze-drying and freeze-cast molding method | Porosity (%): 96.33 or 96.16 Pore size (μm): 111.32 ± 160.2; 138.93 ± 302.6 and 152.71 ± 679.9 | Randomly oriented pore (freeze-dried) and interconnected pore (freeze-cast) NGC stimulate ECM to support cellular adhesion and migration. Different NGC manufacturing processes affect their properties by altering the microstructure of pores. |
| Huang et al., 2018 [47] | In vitro: DRG cells cultures | Poly(ε-caprolactone) (PCL) sheaths and collagen-chitosan (O-CCH) filler. | Electrospinning | Pores size: 6.5 ± 3.3 μm Wall thickness: 100, 200, 400 μm | NGC (100 µm) collapsed without additional force. NGC (200 µm) provided a strength lower than 0.02 N/mm at a lateral displacement of 0.3 mm. NGC (400 µm) provided a strength of 0.05–0.065 N/mm at a lateral displacement of 0.3 mm, comparable to commercially available NGC. A PCL porous sheath (pore size: 6.52 ± 3.28 μm) prevented fibroblast invasion and provided mechanical strength for fixation and resistance to compression, exhibiting the appropriate porosity to ensure the supply of oxygen and nutrients, also preventing fibrous tissue infiltration. |
| Vijayavenkataraman et al., 2018 [48] | In vitro: PC12 cells | Poly(ε-caprolactone) (PCL) | Electrohydrodynamic jet 3D printing (EHD-jetting) | Different pore sizes scaffolds (125–550 μm) and porosities (65–88%). | The Young’s modulus of the NGC structure decreases with increasing pore size from 275 ± 13 to 121 ± 16 MPa. Similarly, the yield stress also has a decreasing trend with increasing pore size from 24 ± 3 to 5.6 ± 2 MPa. The ultimate strength of the structure decreases from 32 ± 2.4 to 9 ± 1.4 MPa. Desirable NGC structure was observed to have 125 ± 15 μm pores. Porosity over 60%: Mechanical properties closer to the native peripheral nerves, and an optimal degradation rate in nerve regeneration post-injury. The percentage decrease of the mechanical properties from day 0 to day 28 was greater in the scaffolds with a greater pore size (550 μm) (~30 to 66%) and was the least in scaffolds with a smaller pore size (125 μm) (~22–45%). |
| Chan et al., 2007 [13] | In vitro: SC and fibroblasts In vivo: Sciatic nerve of Sprague–Dawley rats | Poly(DL-lactic acid-co-glycolic acid) (PLGA) | Immersion–precipitation phase inversion using a casting process | Asymmetric conduits with: high-porosity (permeability) 83.5 ± 5.3%; Medium-porosity (high outflow and low inflow) 73.6 ± 4.7 %; Low-porosity (permeability) 66.1 ± 3.4%. | NGC with different porosities prevented fibrous scar tissue invasion. Allowing the permeation of nutrients, oxygen, and proliferation of SC. Patent directional NGC showed more type A and B myelin fibers in the middle duct and distal nerve compared to the high bidirectional patency NGC. |
| Chang et al., 2006 [49] | In vivo: sciatic nerve defects in Sprague–Dawley rats (n = 80). | Poly(DL-lactic acid-co-glycolic acid) (PLGA) | Immersion–precipitation phase inversion using a casting process | NGC: Asymmetric: macrovoids (outer layer), and interconnected micropores (inner layer), possessed characters of larger outflow rate than inflow rate.
| Asymmetric PLGA NGC showed a stable supporting structure, inhibiting exogenous cell invasion during the regeneration process, higher regenerated axons at the mid-conduit, and distal nerve site of implanted grafts compared to the silicone and non-asymmetric groups at 4 and 6 weeks. The asymmetric structure in the conduit wall enhanced the removal of the blockage of the waste drain from the inner inflamed wound in the early stage. |
| Vleggeert-Lankamp et al., 2006 [50] | In vivo: sciatic nerve of female Wistar rat (n = 38). | Poly(ε-caprolactone) | NaCl used as a porosifying agent in the preparation of porous structures | Autografted; grafted nonporous; grafted with pores: outer layer: macroporous (10–230 μm) and inner layer microporous (1–10 μm), macroporous (10–230 μm) or nonporous. | Microporous nerve grafts performed better than nonporous and macroporous grafts. Formation of a tissue bridge with a large diameter, myelinated nerve fibers, more nerve fibers present distal to the graft, the electrophysiological response rate was higher, and the decrease in muscle cross-sectional area was smaller. |
| Oh et al., 2008 [12] | In vivo: Sciatic nerve of Sprague–Dawley rats (n = 63). | Poly(lactic-co-glycolic acid) (PLGA) and Pluronic F127 | Modified immersion precipitation method | Porosity: inner surface of the tube with nano-size pores (~50 nm); outer surface with micro-size pores (~50 μm) Nonporous: silicon tubes | PLGA/Pluronic F127 NGC (inner surface pore: ~50 nm) prevented the infiltration of fibrous tissue, retained neurotrophic factors, and provided optimal nutrient infiltration. NGC with the outer surface with micro-sized pores (~50 μm) allowed vascular growth for effective delivery of nutrients and oxygen, allowing rapid and continuous axonal growth from the proximal to the distal direction in ~4 weeks. |
| Oh et al., 2012 [51] | In vivo: Sciatic nerve of rats (n = 48). | Poly(caprolactone) (PCL)/Pluronic F127 | Immersion precipitation method | Membrane with nano-size pores (~100 nm) and opposite surface (mold contact side) with micro-size pores (~200 μm) | Nerve fibers regenerated along the longitudinal direction through the NGC with a nano-porous inner surface, while they were grown toward the porous wall of the NGC with a micro-porous inner surface. |
| Choi et al., 2014 [52] | In vivo: Recurrent laryngeal nerve of female New Zealand rabbits (n = 28). | Poly(caprolactone) (PCL)/Pluronic F127 | Immersion precipitation method | Asymmetrically porous NGC with selective permeability (inner surface, nano-sized pores; outer surface, micro-sized pores) Nonporous silicone tube. Wall thickness ~0.4 mm, inner diameter of ~1.5 mm and a length of ~12 mm. | Significantly better vocal cord paralysis in the asymmetrically porous PCL/F127 NGC than in the silicone tube. Asymmetrically porous PCL/F127 NGC tubes facilitated nerve regeneration compared with nonporous silicone tubes. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alarcón Apablaza, J.; Lezcano, M.F.; Godoy Sánchez, K.; Oporto, G.H.; Dias, F.J. Optimal Morphometric Characteristics of a Tubular Polymeric Scaffold to Promote Peripheral Nerve Regeneration: A Scoping Review. Polymers 2022, 14, 397. https://doi.org/10.3390/polym14030397
Alarcón Apablaza J, Lezcano MF, Godoy Sánchez K, Oporto GH, Dias FJ. Optimal Morphometric Characteristics of a Tubular Polymeric Scaffold to Promote Peripheral Nerve Regeneration: A Scoping Review. Polymers. 2022; 14(3):397. https://doi.org/10.3390/polym14030397
Chicago/Turabian StyleAlarcón Apablaza, Josefa, María Florencia Lezcano, Karina Godoy Sánchez, Gonzalo H. Oporto, and Fernando José Dias. 2022. "Optimal Morphometric Characteristics of a Tubular Polymeric Scaffold to Promote Peripheral Nerve Regeneration: A Scoping Review" Polymers 14, no. 3: 397. https://doi.org/10.3390/polym14030397