Use of Photobiomodulation Combined with Fibrin Sealant and Bone Substitute Improving the Bone Repair of Critical Defects
Abstract
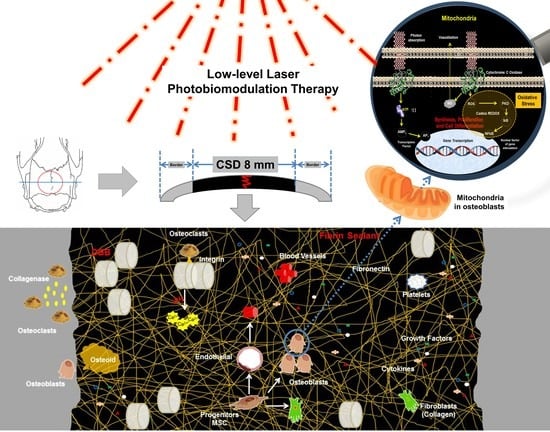
:1. Introduction
2. Materials and Methods
2.1. Bone Graft Substitutes—Xenograft
2.2. Fibrin Sealant—Human-Blood Derived
2.3. Experimental Design
2.4. Surgical Procedures
2.5. Photobiomodulation Therapy Protocol
2.6. Euthanasia
2.7. Micro-CT Scanning
2.8. Histotechnical Processing
2.9. Histological Evaluation of Defects Bone Healing
2.10. Birefringence Analysis of Collagen Content of Bone Healing Defects
2.11. Quantitative Analysis of Osteocytes in Newly Formed Bone Tissue
2.12. Immunohistochemical Processing
2.13. Statistical Analysis
3. Results
3.1. µ-CT Analysis at 14 and 42 days
3.2. Histological Evaluation of Defects Bone Healing
3.3. Picrosirius Red Staining Showed Less Bone Collagen Organization/Maturation
3.4. Quantitative Analysis of Osteocytes in Newly Formed Bone Tissue
3.5. Immunolabelling Findings for BMP—2/4, VEGF, OCN and TRAP
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nagata, M.J.H.; Santinoni, C.S.; Pola, N.M.; De Campos, N.; Messora, M.R.; Bomfim, S.R.M.; Ervolino, E.; Fucini, S.E.; Faleiros, P.L.; Garcia, V.G.; et al. Bone Marrow Aspirate Combined with Low-Level Laser Therapy: A New Therapeutic Approach to Enhance Bone Healing. J. Photochem. Photobiol. B Biol. 2013, 121, 6–14. [Google Scholar] [CrossRef]
- Codrea, C.I.; Croitoru, A.M.; Baciu, C.C.; Melinescu, A.; Ficai, D.; Fruth, V.; Ficai, A. Advances in Osteoporotic Bone Tissue Engineering. J. Clin. Med. 2021, 10, 253. [Google Scholar] [CrossRef] [PubMed]
- Buchaim, D.V.; Dos Santos Bueno, P.C.; Andreo, J.C.; Roque, D.D.; Roque, J.S.; Zilio, M.G.; Salatin, J.A.; Kawano, N.; Furlanette, G.; Buchaim, R.L. Action of a Deproteinized Xenogenic Biomaterial in the Process of Bone Repair in Rats Submitted to Inhalation of Cigarette Smoke. Acta Cir. Bras. 2018, 33, 324–332. [Google Scholar] [CrossRef] [Green Version]
- Pomini, K.T.; Cestari, T.M.; German, J.S.; Rosso, M.P.D.O.; Gonçalves, J.B.D.O.; Buchaim, D.V.; Pereira, M.; Andreo, J.C.; Rosa, G.M.; Della Coletta, B.B.; et al. Influence of Experimental Alcoholism on the Repair Process of Bone Defects Filled with Beta-Tricalcium Phosphate. Drug Alcohol Depend. 2019, 197, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, D.M.B.; de Faria Figadoli, A.L.; Alcantara, P.L.; Pomini, K.T.; German, I.J.S.; Reis, C.H.B.; Júnior, G.M.R.; de Oliveira Rosso, M.P.; da Silva Santos, P.S.; Zangrando, M.S.R.; et al. Biological Behavior of Xenogenic Scaffolds in Alcohol-Induced Rats: Histomorphometric and Picrosirius Red Staining Analysis. Polymers 2022, 14, 584. [Google Scholar] [CrossRef]
- German, I.J.S.; Pomini, K.T.; Bighetti, A.C.C.; Andreo, J.C.; Reis, C.H.B.; Shinohara, A.L.; Rosa, G.M.; de Bortoli Teixeira, D.; de Oliveira Rosso, M.P.; Buchaim, D.V.; et al. Evaluation of the Use of an Inorganic Bone Matrix in the Repair of Bone Defects in Rats Submitted to Experimental Alcoholism. Materials 2020, 13, 695. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pountos, I.; Giannoudis, P. Is There a Role of Coral Bone Substitutes in Bone Repair? Injury 2016, 47, 2606–2613. [Google Scholar] [CrossRef] [Green Version]
- Reis, C.H.B.; Buchaim, R.L.; Pomini, K.T.; Hamzé, A.L.; Zattiti, I.V.; Duarte, M.A.H.; Alcalde, M.P.; Barraviera, B.; Ferreira Júnior, R.S.; Pontes, F.M.L.; et al. Effects of a Biocomplex Formed by Two Scaffold Biomaterials, Hydroxyapatite/Tricalcium Phosphate Ceramic and Fibrin Biopolymer, with Photobiomodulation, on Bone Repair. Polymers 2022, 14, 2075. [Google Scholar] [CrossRef]
- Sakkas, A.; Wilde, F.; Heufelder, M.; Winter, K.; Schramm, A. Autogenous Bone Grafts in Oral Implantology—Is It Still a “Gold Standard”? A Consecutive Review of 279 Patients with 456 Clinical Procedures. Int. J. Implant Dent. 2017, 3, 23. [Google Scholar] [CrossRef]
- Schmidt, A.H. Autologous Bone Graft: Is It Still the Gold Standard? Injury 2021, 52, S18–S22. [Google Scholar] [CrossRef]
- Delgado-Ruiz, R.; Calvo Guirado, J.; Romanos, G. Bone Grafting Materials in Critical Defects in Rabbit Calvariae. A Systematic Review and Quality Evaluation Using ARRIVE Guidelines. Clin. Oral Implant. Res. 2015, 29, 620–634. [Google Scholar] [CrossRef]
- Tang, G.; Liu, Z.; Liu, Y.; Yu, J.; Wang, X.; Tan, Z.; Ye, X. Recent Trends in the Development of Bone Regenerative Biomaterials. Front. Cell Dev. Biol. 2021, 9, 1–18. [Google Scholar] [CrossRef]
- Manfro, R.; Fonseca, F.; Bortoluzzi, M.; Sendyk, W. Comparative, Histological and Histomorphometric Analysis of Three Anorganic Bovine Xenogenous Bone Substitutes: Bio-Oss, Bone-Fill and Gen-Ox Anorganic. J. Maxillofac. Oral Surg. 2014, 13, 464–470. [Google Scholar] [CrossRef] [Green Version]
- Di Stefano, D.A.; Zaniol, T.; Cinci, L.; Pieri, L. Chemical, Clinical and Histomorphometric Comparison between Equine Bone Manufactured through Enzymatic Antigen-Elimination and Bovine Bone Made Non-Antigenic Using a High-Temperature Process in Post-Extractive Socket Grafting. A Comparative Retrospective. Dent. J. 2019, 7, 70. [Google Scholar] [CrossRef] [Green Version]
- Do Desterro, F.d.P.; Sader, M.S.; de Almeida Soares, G.D.; Vidigal, G.M., Jr. Can Inorganic Bovine Bone Grafts Present Distinct Properties? Braz. Dent. J. 2014, 25, 282–288. [Google Scholar] [CrossRef] [Green Version]
- Noori, A.; Ashrafi, S.; Vaez-Ghaemi, R.; Hatamian-Zaremi, A.; Webster, T. A Review of Fibrin and Fibrin Composites for Bone Tissue Engineering. Int. J. Nanomed. 2017, 12, 4937–4961. [Google Scholar] [CrossRef] [Green Version]
- Saffarzadeh, A.; Gauthier, O.; Bilban, M.; Bagot, D.M.; Daculsi, G. Comparison of Two Bone Substitute Biomaterials Consisting of a Mixture of Fibrin Sealant (Tisseel®) and MBCP t (TricOs®) with an Autograft in Sinus Lift Surgery in Sheep. Clin. Oral Implant. Res. 2009, 20, 1133–1139. [Google Scholar] [CrossRef]
- Zheng, K.; Gu, Q.; Zhou, D.; Zhou, M.; Zhang, L. Recent Progress in Surgical Adhesives for Biomedical Applications. Smart Mater. Med. 2022, 3, 41–65. [Google Scholar] [CrossRef]
- Pomini, K.T.; Andreo, J.C.; De Rodrigues, A.C.; De Gonçalves, J.B.O.; Daré, L.R.; German, I.J.S.; Rosa, G.M.; Buchaim, R.L. Effect of Low-Intensity Pulsed Ultrasound on Bone Regeneration Biochemical and Radiologic Analyses. J. Ultrasound Med. 2014, 33, 713–717. [Google Scholar] [CrossRef] [Green Version]
- Buchaim, D.; Rodrigues Ade, C.; Buchaim, R.; Barraviera, B.; Júnior, R.; Júnior, G.; Bueno, C.; Roque, D.; Dias, D.; Desafio, L.; et al. The New Heterologous Fibrin Sealant in Combination with Low-Level Laser Therapy (LLLT) in the Repair of the Buccal Branch of the Facial Nerve. Lasers Med. Sci. 2016, 31, 965–972. [Google Scholar] [CrossRef]
- De Oliveira Gonçalves, J.; Buchaim, D.; de Souza Bueno, C.; Pomini, K.; Barraviera, B.; Júnior, R.; Andreo, J.; de Castro Rodrigues, A.; Cestari, T.M.; Buchaim, R.L. Effects of Low-Level Laser Therapy on Autogenous Bone Graft Stabilized with a New Heterologous Fibrin Sealant. J. Photochem. Photobiol. B 2016, 162, 663–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Escudero, J.S.B.; Perez, M.G.B.; de Oliveira Rosso, M.P.; Buchaim, D.V.; Pomini, K.T.; Campos, L.M.G.; Audi, M.; Buchaim, R.L. Photobiomodulation Therapy (PBMT) in Bone Repair: A Systematic Review. Injury 2019, 50, 1853–1867. [Google Scholar] [CrossRef] [PubMed]
- Khadra, M.; Kasem, N.; Haanaes, H.; Ellingsen, J.; Lyngstadaas, S. Enhancement of Bone Formation in Rat Calvarial Bone Defects Using Low-Level Laser Therapy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Jawad, M.M.; Husein, A.; Azlina, A.; Alam, M.K.; Hassan, R.; Shaari, R. Effect of 940 Nm Low-Level Laser Therapy on Osteogenesis in Vitro. J. Biomed. Opt. 2013, 18, 128001. [Google Scholar] [CrossRef] [PubMed]
- De Marco, A.C.; Torquato, L.C.; Gonçalves, P.R.; Ribeiro, T.C.; Nunes, C.M.; Bernardo, D.V.; Gomes, M.F.; Jardini, M.A.N.; Santamaria, M.P. The Effect of Photobiomodulation Therapy in Different Doses on Bone Repair of Critical Size Defects in Rats: A Histomorphometric Study. J. Lasers Med. Sci. 2021, 12, e53. [Google Scholar] [CrossRef] [PubMed]
- Atasoy, K.T.; Korkmaz, Y.T.; Odaci, E.; Hanci, H. The Efficacy of Low-Level 940 Nm Laser Therapy with Different Energy Intensities on Bone Healing. Braz. Oral Res. 2017, 31, e7. [Google Scholar] [CrossRef] [Green Version]
- Percie du Sert, N.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Dirnagl, U.; Emerson, M.; et al. Reporting animal research: Explanation and elaboration for the ARRIVE guidelines 2.0. PLoS Biol. 2020, 18, e3000411. [Google Scholar] [CrossRef]
- Pomini, K.T.; Buchaim, D.V.; Andreo, J.C.; de Oliveira Rosso, M.P.; Della Coletta, B.B.; German, Í.J.S.; Biguetti, A.C.C.; Shinohara, A.L.; Rosa Júnior, G.M.; Cosin Shindo, J.V.T.; et al. Fibrin Sealant Derived from Human Plasma as a Scaffold for Bone Grafts Associated with Photobiomodulation Therapy. Int. J. Mol. Sci. 2019, 20, 1761. [Google Scholar] [CrossRef] [Green Version]
- Parasuraman, S.; Raveendran, R.; Kesavan, R. Blood Sample Collection in Small Laboratory Animals. J. Pharmacol. Pharmacother. 2010, 1, 87. [Google Scholar] [CrossRef] [Green Version]
- Neagu, T.P.; Ţigliş, M.; Cocoloş, I.; Jecan, C.R. The Relationship between Periosteum and Fracture Healing. Rom. J. Morphol. Embryol. 2016, 57, 1215–1220. [Google Scholar]
- Weibel, E. Stereological Principles for Morphometry in Electron Microscopic Cytology. Int. Rev. Cytol. 1969, 26, 235–302. [Google Scholar] [CrossRef]
- Theodoro, L.H.; Caiado, R.C.; Longo, M.; Novaes, V.C.N.; Zanini, N.A.; Ervolino, E.; de Almeida, J.M.; Garcia, V.G. Effectiveness of the Diode Laser in the Treatment of Ligature-Induced Periodontitis in Rats: A Histopathological, Histometric, and Immunohistochemical Study. Lasers Med. Sci. 2015, 30, 1209–1218. [Google Scholar] [CrossRef]
- Zein, R.; Selting, W.; Benedicenti, S. Effect of Low-Level Laser Therapy on Bone Regeneration During Osseointegration and Bone Graft. Photomed. Laser Surg. 2017, 35, 649–658. [Google Scholar] [CrossRef]
- Tam, S.Y.; Tam, V.C.W.; Ramkumar, S.; Khaw, M.L.; Law, H.K.W.; Lee, S.W.Y. Review on the Cellular Mechanisms of Low-Level Laser Therapy Use in Oncology. Front. Oncol. 2020, 10, 1255. [Google Scholar] [CrossRef]
- Dompe, C.; Moncrieff, L.; Matys, J.; Grzech-Leśniak, K.; Kocherova, I.; Bryja, A.; Bruska, M.; Dominiak, M.; Mozdziak, P.; Skiba, T.H.I.; et al. Photobiomodulation-Underlying Mechanism and Clinical Applications. J. Clin. Med. 2020, 3, 1724. [Google Scholar] [CrossRef]
- Murphy, M.P.; Quarto, N.; Longaker, M.T.; Wan, D.C. Calvarial Defects: Cell-Based Reconstructive Strategies in the Murine Model. Tissue Eng. Part C Methods 2017, 23, 971–981. [Google Scholar] [CrossRef]
- Kotagudda Ranganath, S.; Schlund, M.; Delattre, J.; Ferri, J.; Chai, F. Bilateral Double Site (Calvarial and Mandibular) Critical-Size Bone Defect Model in Rabbits for Evaluation of a Craniofacial Tissue Engineering Constructs. Mater Today Bio 2022, 14, 100267. [Google Scholar] [CrossRef]
- Senos, R.; Hankenson, K.D. Calvaria Critical-Size Defects in Rats Using Piezoelectric Equipment: A Comparison with the Classic Trephine. Injury 2020, 51, 1509–1514. [Google Scholar] [CrossRef]
- Borie, E.; Calzzani, R.; Dias, F.J.; Fuentes, R.; Salamanca, C. Morphometry of Rabbit Anatomical Regions Used as Experimental Models in Implantology and Oral Surgery. Biomed. Res. 2017, 28, 5468–5472. [Google Scholar]
- Fujihara, N.A.; Hiraki, K.R.N.; Marques, M.M. Irradiation at 780 Nm Increases Proliferation Rate of Osteoblasts Independently of Dexamethasone Presence. Lasers Surg. Med. 2006, 38, 332–336. [Google Scholar] [CrossRef]
- Zielińska, P.; Soroko, M.; Howell, K.; Godlewska, M.; Hildebrand, W.; Dudek, K. Comparison of the Effect of High-Intensity Laser Therapy (Hilt) on Skin Surface Temperature and Vein Diameter in Pigmented and Non-Pigmented Skin in Healthy Racehorses. Animals 2021, 11, 1965. [Google Scholar] [CrossRef] [PubMed]
- Park, J.J.; Kang, K.L. Effect of 980-Nm GaAlAs Diode Laser Irradiation on Healing of Extraction Sockets in Streptozotocin-Induced Diabetic Rats: A Pilot Study. Lasers Med. Sci. 2012, 27, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpour, S.; Fekrazad, R.; Arany, P.R.; Ye, Q. Molecular Impacts of Photobiomodulation on Bone Regeneration: A Systematic Review. Prog. Biophys. Mol. Biol. 2019, 149, 147–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumoto, M.A.; Ferino, R.V.; Monteleone, G.F.; Ribeiro, D.A. Low-Level Laser Therapy Modulates Cyclo-Oxygenase-2 Expression during Bone Repair in Rats. Lasers Med. Sci. 2009, 24, 195–201. [Google Scholar] [CrossRef]
- Basford, J. Low Intensity Laser Therapy: Still Not an Established Clinical Tool. Lasers Surg. Med. 1995, 16, 331–342. [Google Scholar] [CrossRef]
- Ma, H.; Yang, J.; Tan, R.; Lee, H.; Han, S. Effect of Low-Level Laser Therapy on Proliferation and Collagen Synthesis of Human Fibroblasts in Vitro. JWMR 2018, 14, 1–6. [Google Scholar] [CrossRef]
- Della Coletta, B.B.; Jacob, T.B.; De Carvalho Moreira, L.A.; Pomini, K.T.; Buchaim, D.V.; Eleutério, R.G.; Bastos Mazuqueli Pereira, E.D.S.; Roque, D.D.; De Oliveira Rosso, M.P.; Cosin Shindo, J.V.T.; et al. Photobiomodulation Therapy on the Guided Bone Regeneration Process in Defects Filled by Biphasic Calcium Phosphate Associated with Fibrin Biopolymer. Molecules 2021, 26, 847. [Google Scholar] [CrossRef]
- Tumedei, M.; Mijiritsky, E.; Fernando, C.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. Histological and Biological Response to Different Types of Biomaterials: A Narrative Single Research Center Experience over Three Decades. Int. J. Environ. Res. Public Health 2022, 19, 7942. [Google Scholar] [CrossRef]
- Benke, D.; Olah, A.; Möhler, H. Protein-Chemical Analysis of Bio-Oss Bone Substitute and Evidence on Its Carbonate Content. Biomaterials 2001, 22, 1005–1012. [Google Scholar] [CrossRef]
- Li, X.; Li, S.; Qi, H.; Han, D.; Chen, N.; Zhan, Q.; Li, Z.; Zhao, J.; Hou, X.; Yuan, X.; et al. Early Healing of Alveolar Bone Promoted by MicroRNA-21-Loaded Nanoparticles Combined with Bio-Oss Particles. Chem. Eng. J. 2020, 401, 126026. [Google Scholar] [CrossRef]
- Tadjoedin, E.S.; De Lange, G.L.; Bronckers, A.L.J.J.; Lyaruu, D.M.; Burger, E.H. Deproteinized Cancellous Bovine Bone (Bio-Oss®) as Bone Substitute for Sinus Floor Elevation. A Retrospective, Histomorphometrical Study of Five Cases. J. Clin. Periodontol. 2003, 30, 261–270. [Google Scholar] [CrossRef]
- Block, M.S.; Zoccolillo, M. Use of Tisseel, a Fibrin Sealant, for Particulate Graft Stabilization. J. Oral Maxillofac. Surg. 2020, 78, 1674–1681. [Google Scholar] [CrossRef]
- Diamond, M.P.; Kruger, M.; Saed, G.M. Effect of Tisseel® on Expression of Tissue Plasminogen Activator and Plasminogen Activator Inhibitor-1. Fertil. Steril. 2004, 81, 1657–1664. [Google Scholar] [CrossRef]
- Rechtin, M.; Broccoli, N.; Krishnan, D.G.; Phero, J.A. Review Use of Tisseel, a Fibrin Sealant, for Particulate Graft Stabilization. J. Oral Maxillofac. Surg. 2020, 78, e2–e5. [Google Scholar] [CrossRef]
- Sung, Y.K.; Lee, D.R.; Chung, D.J. Advances in the Development of Hemostatic Biomaterials for Medical Application. Biomater. Res. 2021, 25, 1–10. [Google Scholar] [CrossRef]
- Lohmann, P.; Willuweit, A.; Neffe, A.T.; Geisler, S.; Gebauer, T.P.; Beer, S.; Coenen, H.H.; Fischer, H.; Hermanns-Sachweh, B.; Lendlein, A.; et al. Bone Regeneration Induced by a 3D Architectured Hydrogel in a Rat Critical-Size Calvarial Defect. Biomaterials 2017, 113, 158–169. [Google Scholar] [CrossRef]
- Liu, W.; Kang, N.; Seriwatanachai, D.; Dong, Y.; Zhou, L.; Lin, Y.; Ye, L.; Liang, X.; Yuan, Q. Chronic Kidney Disease Impairs Bone Defect Healing in Rats. Sci. Rep. 2016, 6, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Lienemann, P.; Metzger, S.; Kiveliö, A.; Blanc, A.; Papageorgiou, P.; Astolfo, A.; Pinzer, B.; Cinelli, P.; Weber, F.; Schibli, R.; et al. Longitudinal In Vivo Evaluation of Bone Regeneration by Combined Measurement of Multi-Pinhole SPECT and Micro-CT for Tissue Engineering. Sci. Rep. 2015, 5, srep10238. [Google Scholar] [CrossRef] [Green Version]
- Biguetti, C.; Cavalla, F.; Tim, C.; Saraiva, P.; Orcini, W.; de Andrade Holgado, L.; Rennó, A.; Matsumoto, M. Bioactive Glass-Ceramic Bone Repair Associated or Not with Autogenous Bone: A Study of Organic Bone Matrix Organization in a Rabbit Critical-Sized Calvarial Model. Clin. Oral Investig. 2018, 23, 413–421. [Google Scholar] [CrossRef] [Green Version]
- Lattouf, R.; Younes, R.; Lutomski, D.; Naaman, N.; Godeau, G.; Senni, K.; Changotade, S. Picrosirius Red Staining: A Useful Tool to Appraise Collagen Networks in Normal and Pathological Tissues. J. Histochem. Cytochem. 2014, 62, 751–758. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Yeung, K.W.K. Bone Grafts and Biomaterials Substitutes for Bone Defect Repair: A Review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Hernández-Cortés, P.; Mesa, F.; Carranza, N.; Juodzbalys, G.; Aguilar, M.; O’Valle, F. Slow Resorption of Anorganic Bovine Bone by Osteoclasts in Maxillary Sinus Augmentation. Clin. Implant Dent. Relat. Res. 2013, 15, 858–866. [Google Scholar] [CrossRef]
- Hughes, D.E.; Dai, A.; Tiffee, J.C.; Li, H.H.; Munoy, G.R.; Boyce, B.F. Estrogen Promotes Apoptosis of Murine Osteoclasts Mediated by TGF-. Nat. Med. 1996, 2, 1132–1135. [Google Scholar] [CrossRef]
- Kameda, T.; Mano, H.; Yamada, Y.; Takai, H.; Amizuka, N.; Kobori, M.; Izumi, N.; Kawashima, H.; Ozawa, H.; Ikeda, K.; et al. Calcium-Sensing Receptor in Mature Osteoclasts, Which Are Bone Resorbing Cells. Biochem. Biophys. Res. Commun. 1998, 422, 419–422. [Google Scholar] [CrossRef]
- Tapety, F.; Amizuka, N.; Uoshima, K.; Nomura, S.; Maeda, T. A Histological Evaluation of the Involvement of Bio-Oss in Osteoblastic Differentiation and Matrix Synthesis. Clin. Oral Implant. Res. 2004, 15, 315–324. [Google Scholar] [CrossRef]
- Chen, K.; Shyu, P.; Dong, G.; Chen, Y.; Kuo, W.; Yao, C. Reconstruction of Calvarial Defect Using a Tricalcium Phosphate-Oligomeric Proanthocyanidins Cross-Linked Gelatin Composite. Biomaterials 2009, 30, 1682–1688. [Google Scholar] [CrossRef]
- Brown, A.; Barker, T. Fibrin-Based Biomaterials: Modulation of Macroscopic Properties through Rational Design at the Molecular Level Ashley. Biomaterials 2015, 10, 1502–1514. [Google Scholar] [CrossRef] [Green Version]
- Scognamiglio, F.; Travan, A.; Rustighi, I.; Tarchi, P.; Palmisano, S.; Marsich, E.; Borgogna, M.; Donati, I.; de Manzini, N.; Paoletti, S. Review Article Adhesive and Sealant Interfaces for General Surgery Applications. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 104, 626–639. [Google Scholar] [CrossRef] [Green Version]
- Schmitt, C.; Doering, H.; Schmidt, T.; Lutz, R.; Neukam, F.; Schlegel, K. Histological Results after Maxillary Sinus Augmentation with Straumann® BoneCeramic, Bio-Oss®, Puros®, and Autologous Bone. A Randomized Controlled Clinical Trial. Clin. Oral Implant. Res. 2013, 24, 576–585. [Google Scholar] [CrossRef]
- Nkenke, E.; Neukam, F. Autogenous Bone Harvesting and Grafting in Advanced Jaw Resorption: Morbidity, Resorption and Implant Survival. Eur. J. Oral Implant. 2014, 7, 203–217. [Google Scholar] [CrossRef] [Green Version]
- Buchaim, R.L.; Goissis, G.; Andreo, J.C.; Roque, D.D.; Sidney, J.S.; Buchaim, D.V.; Rodrigues, A.C. Biocompatibility of Anionic Collagen Matrices and Its Influence on the Orientation of Cellular Growth. Cienc. Odontol. Bras. 2007, 10, 12–20. [Google Scholar] [CrossRef]
- Karavitis, J.; Kovacs, E.J. Macrophage Phagocytosis: Effects of Environmental Pollutants, Alcohol, Cigarette Smoke, and Other External Factors. J. Leukoc. Biol. 2011, 90, 1065–1078. [Google Scholar] [CrossRef] [PubMed]
- Hench, L.L.; Polak, J.M. Third-Generation Biomedical Materials. Science 2002, 295, 1014–1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kazancioglu, H.; Ezirganli, S.; Aydin, M. Effects of Laser and Ozone Therapies on Bone Healing in the Calvarial Defects. J. Craniofac. Surg. 2013, 24, 2141–2146. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, L.; de Araújo, A.; de Araújo Júnior, R.; Barboza, C.; Borges, B.; da Silva, J. Low-Level Laser Therapy (780 Nm) Combined with Collagen Sponge Scaffold Promotes Repair of Rat Cranial Critical-Size Defects and Increases TGF-b, FGF-2, OPG/RANK and Osteocalcin Expression. Int. J. Exp. Pathol. 2017, 98, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Fekrazad, R.; Sadeghi Ghuchani, M.; Eslaminejad, M.B.; Taghiyar, L.; Kalhori, K.A.M.; Pedram, M.S.; Shayan, A.M.; Aghdami, N.; Abrahamse, H. The Effects of Combined Low Level Laser Therapy and Mesenchymal Stem Cells on Bone Regeneration in Rabbit Calvarial Defects. J. Photochem. Photobiol. B Biol. 2015, 151, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Walski, T.; Dąbrowska, K.; Drohomirecka, A.; Jędruchniewicz, N.; Trochanowska-Pauk, N.; Witkiewicz, W.; Komorowska, M. The Effect of Red-to-near-Infrared (R/NIR) Irradiation on Inflammatory Processes. Int. J. Radiat. Biol. 2019, 95, 1326–1336. [Google Scholar] [CrossRef]
- Klopfleisch, R. Macrophage Reaction against Biomaterials in the Mouse Model–Phenotypes, Functions and Markers. Acta Biomater. 2016, 43, 3–13. [Google Scholar] [CrossRef]
- Na, S.; TruongVo, T.; Jiang, F.; Joll, J.; Guo, Y.; Utreja, A.; Chen, J. Dose Analysis of Photobiomodulation Therapy on Osteoblast, Osteoclast, and Osteocyte Dose Analysis of Photobiomodulation Therapy on Osteoblast, Osteoclast, and Osteocyte. J. Biomed. Opt. 2018, 23, 075008. [Google Scholar] [CrossRef] [Green Version]
- Tim, C.; Bossini, P.; Kido, H.; Malavazi, I.; Von Zeska Kress, M.; Carazzolle, M.; Parizotto, N.; Rennó, A. Effects of Low-Level Laser Therapy on the Expression of Osteogenic Genes during the Initial Stages of Bone Healing in Rats: A Microarray Analysis. Lasers Med. Sci. 2015, 30, 2325–2333. [Google Scholar] [CrossRef]
- Amaroli, A.; Pasquale, C.; Zekiy, A.; Benedicenti, S.; Marchegiani, A.; Sabbieti, M.G.; Agas, D. Steering the Multipotent Mesenchymal Cells towards an Anti-Inflammatory and Osteogenic Bias via Photobiomodulation Therapy: How to Kill Two Birds with One Stone. J. Tissue Eng. 2022, 5, 20417314221110192. [Google Scholar] [CrossRef]
- Soardi, C.; Clozza, E.; Turco, G.; Biasotto, M.; Engebretson, S.; Wang, H.; Zaffe, D. Microradiography and Microcomputed Tomography Comparative Analysis in Human Bone Cores Harvested after Maxillary Sinus Augmentation: A Pilot Study. Clin. Oral Implant. Res. 2013, 25, 1161–1168. [Google Scholar] [CrossRef]
- Saygun, I.; Nizam, N.; Ural, A.U.; Serdar, M.A.; Avcu, F.; Tözüm, T.F. Low-Level Laser Irradiation Affects the Release of Basic Fibroblast Growth Factor (BFGF), Insulin-Like Growth Factor-I (IGF-I), and Receptor of IGF-I (IGFBP3) from Osteoblasts. Photomed. Laser Surg. 2012, 30, 149–154. [Google Scholar] [CrossRef]
- Coffin, J.D.; Homer-Bouthiette, C.; Hurley, M.M. Fibroblast Growth Factor 2 and Its Receptors in Bone Biology and Disease. J. Endocr. Soc. 2018, 2, 657–671. [Google Scholar] [CrossRef]
- Xie, Y.; Su, N.; Yang, J.; Tan, Q.; Huang, S.; Jin, M.; Ni, Z.; Zhang, B.; Zhang, D.; Luo, F.; et al. FGF/FGFR Signaling in Health and Disease. Signal Transduct. Target Ther. 2020, 5, 1–38. [Google Scholar] [CrossRef]
- Rosso, M.P.D.O.; Buchaim, D.V.; Pomini, K.T.; Botteon, B.D.C.; Reis, C.H.B.; Pilon, J.P.G.; Duarte Júnior, G.; Buchaim, R.L. Photobiomodulation Therapy (PBMT™) Applied in Bone Reconstructive Surgery Using Bovine Bone Grafts: A Systematic Review. Materials 2019, 12, 4051. [Google Scholar] [CrossRef] [Green Version]
- Fabris, A.L.d.S.; Faverani, L.P.; Gomes-Ferreira, P.H.S.; Polo, T.O.B.; Santiago-Júnior, J.F.; Okamoto, R. Bone Repair Access of BoneceramicTM in 5-Mm Defects: Study on Rat Calvaria. J. Appl. Oral Sci. 2018, 26, e20160531. [Google Scholar] [CrossRef] [Green Version]
- Hamblin, M.R. Mechanisms and Applications of the Anti-Inflammatory Effects of Photobiomodulation. AIMS Biophys. 2017, 4, 337–361. [Google Scholar] [CrossRef]
- Matheus, H.R.; Ervolino, E.; Gusman, D.J.R.; Alves, B.E.S.; Fiorin, L.G.; Pereira, P.A.; de Almeida, J.M. Association of Hyaluronic Acid with a Deproteinized Bovine Graft Improves Bone Repair and Increases Bone Formation in Critical-Size Bone Defects. J. Periodontol. 2020, 92, 1646–1658. [Google Scholar] [CrossRef]
- Haridy, Y.; Osenberg, M.; Hilger, A.; Manke, I.; Davesne, D.; Witzmann, F. Bone Metabolism and Evolutionary Origin of Osteocytes: Novel Application of FIB-SEM Tomography. Sci. Adv. 2021, 7, eabb9113. [Google Scholar] [CrossRef]





| Parameter | Period (Days) | Groups | |||
|---|---|---|---|---|---|
| BC | BCP | BT | BTP | ||
| Total volume (TV, mm3) | 14 | 36.52 ± 3.59 aA | 36.22 ± 3.48 aA | 114.0 ± 9.20 bA | 112.8 ± 11.84 bA |
| 42 | 36.60 ± 3.35 aA | 35.80 ± 4.38 aA | 115.4 ± 13.3 bA | 106.7 ± 13.72 bA | |
| Material volume (MV, mm3) | 14 | - | - | 41.09 ± 5.90 aA | 42.35 ± 8.32 aA |
| 42 | - | - | 41.28 ± 7.73 aA | 35.97 ± 5.57 aA | |
| Bone volume (BV, mm3) | 14 | 2.93 ± 1.43 aA | 3.02 ± 0.71 aA | 17.76 ± 3.52 bA | 19.88 ± 5.47 bA |
| 42 | 5.20 ± 1.02 aB | 6.16 ± 2.10 aB | 15.56 ± 4.68 bA | 18.17 ± 3.04 bA | |
| Soft tissue volume (StV, mm3) | 14 | 33.59 ± 2.94 aA | 33.20 ± 3.19 aA | 50.61 ± 5.34 bA | 56.88 ± 9.82 bA |
| 42 | 31.40 ± 4.00 aA | 29.64 ± 3.00 aA | 58.51 ± 13.1 bA | 52.61 ± 13.5 bA | |
| Material volume (MV/TV, %) | 14 | - | - | 36.20 ± 5.71 aA | 37.52 ± 5.75 aA |
| 42 | - | - | 35.99 ± 7.00 aA | 33.85 ± 4.50 aA | |
| Bone volume (BV/TV, %) | 14 | 7.89 ± 3.54 aA | 8.32 ± 1.60 aA | 15.53 ± 2.38 bA | 17.56 ± 4.04 bA |
| 42 | 14.42 ± 3.66 aB | 16.96 ± 4.38 aB | 13.44 ± 3.88 aA | 17.37 ± 4.38 aA | |
| Soft tissue volume (StV/TV, %) | 14 | 92.10 ± 3.54 aA | 91.68 ± 1.60 aA | 48.27 ± 7.21 bA | 44.92 ± 3.02 bA |
| 42 | 85.58 ± 3.66 aB | 83.04 ± 4.38 aB | 50.57 ± 9.74 bA | 48.78 ± 8.16 bA | |
| Cell Numbers/mm2 Bone Matrix | Period (Days) | Groups | |||
|---|---|---|---|---|---|
| BC | BCP | BT | BTP | ||
| Osteocytes | 14 | 787 ± 111.6 aA | 764 ± 222.7 aA | 789 ± 80.2 aA | 740 ± 43.8 aA |
| 42 | 558 ± 50.2 aB | 476 ± 87.3 aB | 453 ± 65.1 aB | 493 ± 79.0 aB | |
| Parameter | Period (Days) | Groups: Median (Min–Max) | |||
|---|---|---|---|---|---|
| BC | BCP | BT | BTP | ||
| BMP | 14 days | 1(1-1) A | 2(2-3) B | 1(1-1) A | 2(2-2) B |
| 42 days | 1(1-1) A | 2(2-3) B | 1(1-1) A | 2(2-3) B | |
| VEGF | 14 days | 1(1-1) A | 3(2-3) B | 1(1-2) A | 2(2-2) AB |
| 42 days | 1(1-2) A,B | 3(2-3) B | 1(1-1) A | 3(2-3) B | |
| OCN | 14 days | 1(1-1) A | 2(2-2) B | 1(1-1) A | 2(1-2) AB |
| 42 days | 1(1-1) A | 2(2-2) B | 1(1-1) A | 2(2-2) B | |
| Cell Numbers/mm2 Bone Matrix | Period (Days) | Groups | |||
|---|---|---|---|---|---|
| BC | BCP | BT | BTP | ||
| TRAP+ | 14 | 2.8 ± 0.84 aA | 4.8 ± 0.83 bA | 20.2 ± 4.02 cA | 30.4 ± 1.34 dA |
| 42 | 4.0 ± 1.23 aA | 5.8 ± 2.19 bA | 22.0 ± 2.45 cA | 36.6 ± 4.51 dB | |
| Biomaterials | Characteristics | Mechanism of Action |
|---|---|---|
| Bio-OssTM | HAP(h) ∼ HAP (x) |
|
| 70–75% porosity |
| |
| Interconnected micro and macropores (300–1500 µm) |
| |
| Deproteinization (≤300 °C)—no organic components |
| |
| Tisseel Lyo™ | Cross-linked fibrin |
|
| Fibrin polymerization—fibrin polymer |
| |
| Aprotinin component (antifibrinolytic) |
| |
| Blood components | ||
| Hemostatic mechanisms |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pomini, K.T.; Buchaim, D.V.; Bighetti, A.C.C.; Andreo, J.C.; Rosso, M.P.d.O.; Escudero, J.S.B.; Della Coletta, B.B.; Alcalde, M.P.; Duarte, M.A.H.; Pitol, D.L.; et al. Use of Photobiomodulation Combined with Fibrin Sealant and Bone Substitute Improving the Bone Repair of Critical Defects. Polymers 2022, 14, 4170. https://doi.org/10.3390/polym14194170
Pomini KT, Buchaim DV, Bighetti ACC, Andreo JC, Rosso MPdO, Escudero JSB, Della Coletta BB, Alcalde MP, Duarte MAH, Pitol DL, et al. Use of Photobiomodulation Combined with Fibrin Sealant and Bone Substitute Improving the Bone Repair of Critical Defects. Polymers. 2022; 14(19):4170. https://doi.org/10.3390/polym14194170
Chicago/Turabian StylePomini, Karina Torres, Daniela Vieira Buchaim, Ana Carolina Cestari Bighetti, Jesus Carlos Andreo, Marcelie Priscila de Oliveira Rosso, José Stalin Bayas Escudero, Bruna Botteon Della Coletta, Murilo Priori Alcalde, Marco Antonio Hungaro Duarte, Dimitrius Leonardo Pitol, and et al. 2022. "Use of Photobiomodulation Combined with Fibrin Sealant and Bone Substitute Improving the Bone Repair of Critical Defects" Polymers 14, no. 19: 4170. https://doi.org/10.3390/polym14194170