Influence of Post-Core and Crown Type on the Fracture Resistance of Incisors Submitted to Quasistatic Loading
Abstract
:1. Introduction
2. Materials and Methods
2.1. Post and Core Fabrication
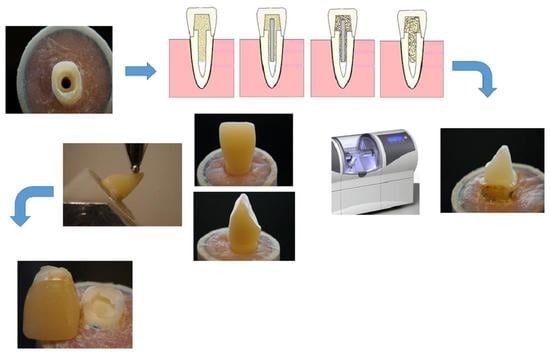
2.2. Crown Fabrication
2.2.1. Direct PFC Crowns (Groups 1–4)
2.2.2. Indirect CAD/CAM Crowns (Groups 5–10)
2.3. Fracture Load Test
2.4. Microscopic Analysis of Fiber Post–Cement Interface
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- For restoring extensively damaged anterior teeth, unidirectional fiber posts are recommended.
- The use of flowable SFRC as post-luting and core material, with regular fiber posts, revealed promising outcomes regarding load-bearing capacity and failure modes.
- Indirect CAD/CAM crown restorations showed improved load capacities compared to direct conventional composite restorations.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lassila, L.; Oksanen, V.; Fráter, M.; Vallittu, P.K.; Garoushi, S. The influence of resin composite with high fiber aspect ratio on fracture resistance of severely damaged bovine incisors. Dent. Mater. J. 2020, 39, 381–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pantaleón, D.S.; Morrow, B.R.; Cagna, D.R.; Pameijer, C.H.; Garcia-Godoy, F. Influence of remaining coronal tooth structure on fracture resistance and failure mode of restored endodontically treated maxillary incisors. J. Prosthet. Dent. 2018, 119, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Zarow, M.; Ramírez-Sebastià, A.; Paolone, G.; de Ribot Porta, J.; Mora, J.; Espona, J.; Durán-Sindreu, F.; Roig, M. A new classification system for the restoration of root filled teeth. Int. Endod. J. 2018, 51, 318–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyenberg, K. The ideal restoration of endodontically treated teeth—Structural and esthetic considerations: A review of the literature and clinical guidelines for the restorative clinician. Eur. J. Esthet. Dent. 2013, 8, 238–268. [Google Scholar] [PubMed]
- Fragou, T.; Tortopidis, D.; Kontonasaki, E.; Evangelinaki, E.; Ioannidis, K.; Petridis, H.; Koidis, P. The effect of ferrule on the fracture mode of endodontically treated canines restored with fibre posts and metal-ceramic or all-ceramic crowns. J. Dent. 2012, 40, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Cheung, W. A review of the management of endodontically treated teeth. Post, core and the final restoration. J. Am. Dent. Assoc. 2005, 136, 611–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheung, G.S.; Chan, T.K. Long-term survival of primary root canal treatment carried out in a dental teaching hospital. Int. Endod. J. 2003, 36, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, F.; Bertelli, E.; Sherriff, M.; Watson, T.F.; Ford, T.R. Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J. Prosthet. Dent. 2002, 88, 297–301. [Google Scholar] [CrossRef] [Green Version]
- Stavropoulou, A.F.; Koidis, P.T. A systematic review of single crowns on endodontically treated teeth. J. Dent. 2007, 35, 761–767. [Google Scholar] [CrossRef]
- Stenhagen, S.; Skeie, H.; Bårdsen, A.; Laegreid, T. Influence of the coronal restoration on the outcome of endodontically treated teeth. Acta Odontol. Scand. 2020, 78, 81–86. [Google Scholar] [CrossRef]
- Qualtrough, A.J.; Mannocci, F. Tooth-colored post system: A review. Oper. Dent. 2003, 28, 86–91. [Google Scholar]
- Garcia, P.P.; Wambier, L.M.; de Geus, J.L.; da Cunha, L.F.; Correr, G.M.; Gonzaga, C.C. Do anterior and posterior teeth treated with post-and-core restorations have similar failure rates? A systematic review and meta-analysis. J. Prosthet. Dent. 2019, 121, 887–894. [Google Scholar] [CrossRef]
- Naumann, M.; Blankenstein, F.; Kiessling, S.; Dietrich, T. Risk factors for failure of glass fiber-reinforced composite post restorations: A prospective observational clinical study. Eur. J. Oral Sci. 2005, 113, 519–524. [Google Scholar] [CrossRef] [PubMed]
- Zicari, F.; De Munck, J.; Scotti, R.; Naert, I.; Van Meerbeek, B. Factors affecting the cement-post interface. Dent. Mater. 2012, 28, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K. Are we misusing fiber posts? Guest editorial. Dent. Mater. 2016, 32, 125–126. [Google Scholar] [CrossRef] [PubMed]
- Egilmez, F.; Ergun, G.; Cekic-Nagas, I.; Vallittu, P.K.; Lassila, L.V. Influence of cement thickness on the bond strength of tooth-colored posts to root dentin after thermal cycling. Acta Odontol. Scand. 2013, 71, 175–182. [Google Scholar] [CrossRef]
- Hatta, M.; Shinya, A.; Vallittu, P.K.; Shinya, A.; Lassila, L.V. High volume individual fibre post versus low volume fibre post: The fracture load of the restored tooth. J. Dent. 2011, 39, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Fráter, M.; Forster, A.; Jantyik, Á.; Braunitzer, G.; Nagy, K.; Grandini, S. In vitro fracture resistance of premolar teeth restored with fibre-reinforced composite posts using a single or a multi-post technique. Aust. Endod. J. 2017, 43, 16–22. [Google Scholar] [CrossRef] [Green Version]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Continuous and short fiber reinforced composite in root post-core system of severely damaged incisors. Open Dent. J. 2009, 3, 36–41. [Google Scholar] [CrossRef] [Green Version]
- Forster, A.; Sáry, T.; Braunitzer, G.; Fráter, M. In vitro fracture resistance of endodontically treated premolar teeth restored with a direct layered fiber-reinforced composite post and core. J. Adhes. Sci. Technol. 2016, 31, 1454–1466. [Google Scholar] [CrossRef] [Green Version]
- Fráter, M.; Lassila, L.; Braunitzer, G.; Vallittu, P.K.; Garoushi, S. Fracture resistance and marginal gap formation of post-core restorations: Influence of different fiber-reinforced composites. Clin. Oral Investig. 2020, 24, 265–276. [Google Scholar] [CrossRef] [Green Version]
- Fráter, M.; Sáry, T.; Néma, V.; Braunitzer, G.; Vallittu, P.; Lassila, L.; Garoushi, S. Fatigue failure load of immature anterior teeth: Influence of different fiber post-core systems. Odontology 2021, 109, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Fráter, M.; Sáry, T.; Jókai, B.; Braunitzer, G.; Säilynoja, E.; Vallittu, P.; Lassila, L.; Garoushi, S. Fatigue behavior of endodontically treated premolars restored with different fiber-reinforced designs. Dent. Mater. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Fráter, M.; Sáry, T.; Braunitzer, G.; Szabó, P.B.; Lassila, L.; Vallittu, P.K.; Garoushi, S. Fatigue failure of anterior teeth without ferrule restored with individualized fiber-reinforced post-core foundations. J. Mech. Behav. Biomed. Mater. 2021, 118, 104440. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Tanner, J.; Keulemans, F.; Le Bell-Rönnlöf, A.M.; Lassila, L.; Vallittu, P.K. Fiber Reinforcement of Endodontically Treated Teeth: What Options Do We Have? Literature Review. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S.; Amin, F.; Fareed, M.A.; Ghabbani, H.; Riaz, S.; Khurshid, Z.; Kumar, N. Biomimetic Aspects of Restorative Dentistry Biomaterials. Biomimetics 2020, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Keulemans, F.; Vallittu, P.K.; Garoushi, S. Characterization of restorative short-fiber reinforced dental composites. Dent. Mater. J. 2020, 39, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Säilynoja, E.; Prinssi, R.; Vallittu, P.; Garoushi, S. Characterization of a new fiber-reinforced flowable composite. Odontology 2019, 107, 342–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bijelic, J.; Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Short fiber reinforced composite in restoring severely damaged incisors. Acta Odontol. Scand. 2013, 71, 1221–1231. [Google Scholar] [CrossRef]
- Le Bell-Rönnlöf, A.M.; Lassila, L.V.; Kangasniemi, I.; Vallittu, P.K. Load-bearing capacity of human incisor restored with various fiber-reinforced composite posts. Dent. Mater. 2011, 27, 107–115. [Google Scholar] [CrossRef]
- Zicari, F.; Van Meerbeek, B.; Scotti, R.; Naert, I. Effect of ferrule and post placement on fracture resistance of endodontically treated teeth after fatigue loading. J. Dent. 2013, 41, 207–215. [Google Scholar] [CrossRef]
- Lazari, P.C.; de Carvalho, M.A.; Del Bel Cury, A.A.; Magne, P. Survival of extensively damaged endodontically treated incisors restored with different types of posts-and-core foundation restoration material. J. Prosthet. Dent. 2018, 119, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Nothdurft, F.P.; Schmitt, T.; Rupf, S.; Pospiech, P.R. Influence of fatigue testing and cementation mode on the load-bearing capability of bovine incisors restored with crowns and FRC posts. Dent. Mater. J. 2011, 30, 109–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dietschi, D.; Ardu, S.; Rossier-Gerber, A.; Krejci, I. Adaptation of adhesive post and cores to dentin after in vitro occlusal loading: Evaluation of post material influence. J. Adhes. Dent. 2006, 8, 409–419. [Google Scholar]
- Garner, J.R.; Wajdowicz, M.N.; DuVall, N.B.; Roberts, H.W. Selected physical properties of new resin-modified glass ionomer luting cements. J. Prosthet. Dent. 2017, 117, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Azar, M.R.; Bagheri, R.; Burrow, M.F. Effect of storage media and time on the fracture toughness of resin-based luting cements. Aust. Dent. J. 2012, 57, 349–354. [Google Scholar] [CrossRef]
- Lohbauer, U.; Belli, R. The Mechanical Performance of a Novel Self-Adhesive Restorative Material. J. Adhes. Dent. 2020, 22, 47–58. [Google Scholar]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Depth of cure and surface microhardness of experimental short fiber-reinforced composite. Acta Odontol. Scand. 2008, 66, 38–42. [Google Scholar] [CrossRef]
- Lassila, L.V.; Nagas, E.; Vallittu, P.K.; Garoushi, S. Translucency of flowable bulk-filling composites of various thicknesses. Chin. J. Dent. Res. 2012, 15, 31–35. [Google Scholar]
- Garoushi, S.; Vallittu, P.; Shinya, A.; Lassila, L. Influence of increment thickness on light transmission, degree of conversion and micro hardness of bulk fill composites. Odontology 2016, 104, 291–297. [Google Scholar] [CrossRef]
- Sequeira-Byron, P.; Fedorowicz, Z.; Carter, B.; Nasser, M.; Alrowaili, E.F. Single crowns versus conventional fillings for the restoration of root-filled teeth. Cochrane Database Syst. Rev. 2015, 9, CD009109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Nieuwenhuysen, J.P.; D’Hoore, W.; Carvalho, J. Long-term evaluation of extensive restorations in permanent teeth. J. Dent. 2003, 31, 395–405. [Google Scholar] [CrossRef]
- Opdam, N.J.M.; Bronkhorst, E.M.; Roeters, J.M.; Loomans, B.A. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent. Mater. 2007, 23, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Lazari, P.C.; Carvalho, M.A.; Johnson, T.; Del Bel Cury, A.A. Ferrule-Effect Dominates Over Use of a Fiber Post When Restoring Endodontically Treated Incisors: An In Vitro Study. Oper. Dent. 2017, 42, 396–406. [Google Scholar] [CrossRef]
- Saunders, W.P.; Saunders, E.M. Coronal leakage as a cause of failure in root-canal therapy: A review. Endod. Dent. Traumatol. 1994, 10, 105–108. [Google Scholar] [CrossRef]
- Anusavice, K.J. Phillips’ Science of Dental Materials, 11th ed.; Elsevier: St. Louis, MO, USA, 2003; pp. 93–94. [Google Scholar]
- Garoushi, S.; Lassila, L.V.J.; Tezvergil, A.; Vallittu, P.K. Static and fatigue compression test for particulate filler composite resin with fiber-reinforced composite substructure. Dent. Mater. 2007, 23, 17–23. [Google Scholar] [CrossRef]
- Garoushi, S.; Säilynoja, E.; Vallittu, P.K.; Lassila, L. Fracture-behavior of CAD/CAM ceramic crowns before and after cyclic fatigue aging. Int. J. Prosthodont. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]






| Brand (Code) | Manufacturer | Type | Composition | ||||
|---|---|---|---|---|---|---|---|
| G-aenial Anterior (PFC) | GC Corp, Tokyo, Japan | Hybrid microfilled composite | UDMA, dimethacrylate co-monomers, pre-polymerized silica and strontium fluoride containing fillers 76 wt% | ||||
| everX Flow (SFRC) | GC Corp, Tokyo, Japan | Flowable fiber reinforced composite (bulk shade) | Bis-EMA, TEGDMA, UDMA, micrometer scale glass fiber filler (100–300 µm and Ø7 μm), Barium glass 70 wt%, 46 vol% | ||||
| Gradia Core | GC Corp, Tokyo, Japan | Dual-cured core build-up composite | Methacrylic acid ester 20–30 wt%, fluoro-alumino-silicate glass 70–75 wt%, silicon dioxide 1–5 wt%. | ||||
| Cerasmart 270 | GC Corp, Tokyo, Japan | CAD/CAM block | Bis-MEPP, UDMA, dimethacrylate co-monomers, silica and barium nano glass 71 wt% | ||||
| Initial LiSi Block | GC Corp, Tokyo, Japan | CAD/CAM block | Not available | ||||
| G-CEM LinkForce | GC Corp, Tokyo, Japan | Dual-cured, self-adhesive cement | Paste A: fluoroalumino silicate glass, initiator, UDMA, dimethacrylate, silicon dioxide. Paste B: silicon dioxide, UDMA, dimethacrylate, initiator, inhibitor | ||||
| MI Core Fiber Post | GC Corp, Tokyo, Japan | Regular fiber post | UDMA, PMMA, glass fibers | ||||
| Group | Post-Core Restoration | Final Crown Restoration |
|---|---|---|
| 1 | Gradia Core as post-core | Conventional direct PFC |
| 2 | Fiber post and Gradia Core | Conventional direct PFC |
| 3 | Fiber post and SFRC core | Conventional direct PFC |
| 4 | SFRC as post-core | Conventional direct PFC |
| 5 | Fiber post and Gradia Core | Cerasmart 270 CAD/CAM |
| 6 | Fiber post and SFRC core | Cerasmart 270 CAD/CAM |
| 7 | SFRC as post-core | Cerasmart 270 CAD/CAM |
| 8 | Fiber post and Gradia Core | LiSi Block CAD/CAM |
| 9 | Fiber post and SFRC core | LiSi Block CAD/CAM |
| 10 | SFRC as post-core | LiSi Block CAD/CAM |
| 11 | Sound teeth as control | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uctasli, S.; Boz, Y.; Sungur, S.; Vallittu, P.K.; Garoushi, S.; Lassila, L. Influence of Post-Core and Crown Type on the Fracture Resistance of Incisors Submitted to Quasistatic Loading. Polymers 2021, 13, 1130. https://doi.org/10.3390/polym13071130
Uctasli S, Boz Y, Sungur S, Vallittu PK, Garoushi S, Lassila L. Influence of Post-Core and Crown Type on the Fracture Resistance of Incisors Submitted to Quasistatic Loading. Polymers. 2021; 13(7):1130. https://doi.org/10.3390/polym13071130
Chicago/Turabian StyleUctasli, Sadullah, Yakup Boz, Sercan Sungur, Pekka K. Vallittu, Sufyan Garoushi, and Lippo Lassila. 2021. "Influence of Post-Core and Crown Type on the Fracture Resistance of Incisors Submitted to Quasistatic Loading" Polymers 13, no. 7: 1130. https://doi.org/10.3390/polym13071130