Effect of Low Hydroxyapatite Loading Fraction on the Mechanical and Tribological Characteristics of Poly(Methyl Methacrylate) Nanocomposites for Dentures
Abstract
:1. Introduction
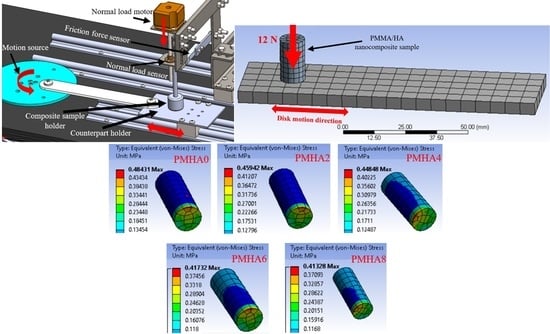
2. Experimental
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lassila, L.V.J.; Vallittu, P.K. Denture base polymer Alldent Sinomer®: Mechanical properties, water sorption and release of residual compounds. J. Oral Rehabil. 2001, 28, 607–613. [Google Scholar]
- Gad, M.M.; Abualsaud, R. Behavior of PMMA denture base materials containing titanium dioxide nanoparticles: A literature review. Int. J. Biomater. 2019, 2019. [Google Scholar] [CrossRef]
- Hassan, M.; Asghar, M.; Din, S.U.; Zafar, M.S. Thermoset polymethacrylate-based materials for dental applications. In Materials for Biomedical Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 273–308. [Google Scholar]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar]
- Murakami, N.; Wakabayashi, N.; Matsushima, R.; Kishida, A.; Igarashi, Y. Effect of high-pressure polymerization on mechanical properties of PMMA denture base resin. J. Mech. Behav. Biomed. Mater. 2013, 20, 98–104. [Google Scholar]
- Alhareb, A.O.; Akil, H.M.; Ahmad, Z.A. Mechanical properties of PMMA denture base reinforced by nitrile rubber particles with Al2O3/YSZ fillers. Procedia Manuf. 2015, 2, 301–306. [Google Scholar]
- Darbar, U.R.; Huggett, R.; Harrison, A. Denture fracture–a survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar]
- Puri, G.; Berzins, D.W.; Dhuru, V.B.; Raj, P.A.; Rambhia, S.K.; Dhir, G.; Dentino, A.R. Effect of phosphate group addition on the properties of denture base resins. J. Prosthet. Dent. 2008, 100, 302–308. [Google Scholar]
- Li, R.; Ye, L.; Mai, Y.-W. Application of plasma technologies in fibre-reinforced polymer composites: A review of recent developments. Compos. Part Appl. Sci. Manuf. 1997, 28, 73–86. [Google Scholar]
- Karthick, R.; Sirisha, P.; Sankar, M.R. Mechanical and tribological properties of PMMA-sea shell based biocomposite for dental application. Procedia Mater. Sci. 2014, 6, 1989–2000. [Google Scholar]
- Kanie, T.; Fujii, K.; Arikawa, H.; Inoue, K. Flexural properties and impact strength of denture base polymer reinforced with woven glass fibers. Dent. Mater. 2000, 16, 150–158. [Google Scholar]
- Asar, N.V.; Albayrak, H.; Korkmaz, T.; Turkyilmaz, I. Influence of various metal oxides on mechanical and physical properties of heat-cured polymethyl methacrylate denture base resins. J. Adv. Prosthodont. 2013, 5, 241–247. [Google Scholar]
- Alhareb, A.O.; Ahmad, Z.A. Effect of Al2O3/ZrO2 reinforcement on the mechanical properties of PMMA denture base. J. Reinf. Plast. Compos. 2011, 30, 86–93. [Google Scholar]
- Alhareb, A.O.; Akil, H.M.; Ahmad, Z.A. Impact strength, fracture toughness and hardness improvement of PMMA denture base through addition of nitrile rubber/ceramic fillers. Saudi J. Dent. Res. 2017, 8, 26–34. [Google Scholar]
- Khurshid, Z.; Zafar, M.; Qasim, S.; Shahab, S.; Naseem, M.; AbuReqaiba, A. Advances in nanotechnology for restorative dentistry. Materials 2015, 8, 717–731. [Google Scholar]
- Zafar, M.S.; Khurshid, Z.; Najeeb, S.; Zohaib, S.; Rehman, I.U. Therapeutic applications of nanotechnology in dentistry. In Nanostructures for Oral Medicine; Elsevier: Amsterdam, The Netherlands, 2017; pp. 833–862. [Google Scholar]
- Zafar, M.S.; Alnazzawi, A.A.; Alrahabi, M.; Fareed, M.A.; Najeeb, S.; Khurshid, Z. Nanotechnology and nanomaterials in dentistry. In Advanced Dental Biomaterials; Elsevier: Amsterdam, The Netherlands, 2019; pp. 477–505. [Google Scholar]
- Ibrahim, A.M.M.; Shi, X.; Radwan, A.R.; Mohamed, A.F.A.; Ezzat, M.F. Enhancing the tribological properties of NiAl based nanocomposites for aerospace bearing applications. Mater. Res. Express 2019, 6, 085067. [Google Scholar]
- Jordan, J.; Jacob, K.I.; Tannenbaum, R.; Sharaf, M.A.; Jasiuk, I. Experimental trends in polymer nanocomposites—A review. Mater. Sci. Eng. A 2005, 393, 1–11. [Google Scholar]
- Fouly, A.; Ibrahim, A.; Fath-elbab, A.; Promoting the Tribological Properties of Epoxy Composites via Using Graphene Nanoplatelets as a Functional Additive. Kgk-Rubberpointde. Available online: https://www.kgk-rubberpoint.de/en/forschung/promoting-the-tribological-properties-of-epoxy-composites-via-using-graphene-nanoplatelets-as-a-functional-additive/ (accessed on 15 May 2020).
- Shakeri, F.; Nodehi, A.; Atai, M. PMMA/double-modified organoclay nanocomposites as fillers for denture base materials with improved mechanical properties. J. Mech. Behav. Biomed. Mater. 2019, 90, 11–19. [Google Scholar]
- Salahuddin, N.; El-Kemary, M.; Ibrahim, E. Reinforcement of polymethyl methacrylate denture base resin with ZnO nanostructures. Int. J. Appl. Ceram. Technol. 2018, 15, 448–459. [Google Scholar]
- Salim, F.M. Tribological and Mechanical Characteristics of Dental Fillings Nanocomposites. Energy Procedia 2019, 157, 512–521. [Google Scholar] [CrossRef]
- Rashed, A.; Nabhan, A. Influence of Adding Nano Graphene and Hybrid SiO2-TiO2 Nano Particles on Tribological Characteristics of Polymethyl methacrylate (PMMA). KGK-kautsch. Gummi Kunstst. 2018, 71, 32–37. [Google Scholar]
- Yang, Z.; Dong, B.; Huang, Y.; Liu, L.; Yan, F.-Y.; Li, H.-L. A study on carbon nanotubes reinforced poly(methyl methacrylate) nanocomposites. Mater. Lett. 2005, 59, 2128–2132. [Google Scholar] [CrossRef]
- Farhan, F.K.; Kadhim, B.B.; Ablawa, B.D.; Shakir, W.A. Wear and Friction Characteristics of TiO2–ZnO/PMMA Nanocomposites. Eur. J. Eng. Res. Sci. 2017, 2, 6–9. [Google Scholar]
- Ameer, A.K.; Mousa, M.O.; Ali, W.Y. Tribological Behaviour of Poly-methyl Methacrylate reinforced by Multi-Walled Carbon Nanotubes. KGK-kautsch. Gummi Kunstst. 2018, 71, 40–46. [Google Scholar]
- Miljković, M.; Kljajević, L.; Filipović, S.; Pavlović, V.B.; Nenadović, S.S. Study of Nanosized Hydroxyapatite Material Annealing at Different Retention Times. Sci. Sinter. 2020, 52, 405–413. [Google Scholar]
- Zhang, S.M.; Cui, F.Z.; Liao, S.S.; Zhu, Y.; Han, L. Synthesis and biocompatibility of porous nano-hydroxyapatite/collagen/alginate composite. J. Mater. Sci. Mater. Med. 2003, 14, 641–645. [Google Scholar]
- Wang, H.; Li, Y.; Zuo, Y.; Li, J.; Ma, S.; Cheng, L. Biocompatibility and osteogenesis of biomimetic nano-hydroxyapatite/polyamide composite scaffolds for bone tissue engineering. Biomaterials 2007, 28, 3338–3348. [Google Scholar]
- Influence of Hydroxyapatite Nanoparticles on the Properties of Glass Ionomer Cement|Elsevier Enhanced Reader. Available online: https://reader.elsevier.com/reader/sd/pii/S2238785417305410?token=FB781748E07820FF210C61512395F08F951F4B6887172EEFB23F276BCFB5CF9EC946C9D374A3AEBF8BA6675FBE9A7377 (accessed on 12 May 2020).
- Mohandesnezhad, S.; Alizadeh, E.; Pilehvar-Soltanahmadi, Y.; Davaran, S.; Goodarzi, A.; Khatamian, M.; Zarghami, N.; Samiei, M.; Aghazadeh, M. In vitro evaluation of novel Zeolite-hydroxyapatite blended scaffold for dental tissue engineering. Mater. Chem. Phys. 2020. [Google Scholar] [CrossRef] [Green Version]
- Marra, K.G.; Szem, J.W.; Kumta, P.N.; DiMilla, P.A.; Weiss, L.E. In vitro analysis of biodegradable polymer blend/hydroxyapatite composites for bone tissue engineering. J. Biomed. Mater. Res. Off. J. Soc. Biomater. Jpn. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 1999, 47, 324–335. [Google Scholar]
- Bakar, M.S.A.; Cheng, M.H.; Tang, S.M.; Yu, S.C.; Liao, K.; Tan, C.T.; Khor, K.A.; Cheang, P. Tensile properties, tension–tension fatigue and biological response of polyetheretherketone–hydroxyapatite composites for load-bearing orthopedic implants. Biomaterials 2003, 24, 2245–2250. [Google Scholar] [CrossRef]
- Converse, G.L.; Yue, W.; Roeder, R.K. Processing and tensile properties of hydroxyapatite-whisker-reinforced polyetheretherketone. Biomaterials 2007, 28, 927–935. [Google Scholar] [CrossRef]
- Zebarjad, S.M.; Sajjadi, S.A.; Sdrabadi, T.E.; Yaghmaei, A.; Naderi, B. A study on mechanical properties of PMMA/hydroxyapatite nanocomposite. Engineering 2011, 3. [Google Scholar] [CrossRef] [Green Version]
- WChow, S.; Tay, H.K.; Azlan, A.; Ishak, Z.M. Mechanical and thermal properties of hydroxyapatite filled poly (methyl methacrylate) composites. In Proceedings of the Polymer Processing Society 24th Annual Meeting 2008, Salerno, Italy, 15–19 June 2008. [Google Scholar]
- Campos-Sanabria, V.; Hernández-Sierra, M.T.; Bravo-Sánchez, M.G.; Aguilera-Camacho, L.D.; García-Miranda, J.S.; Moreno, K.J. Tribological and mechanical characterization of PMMA/HAp nanocomposites obtained by free-radical polymerization. MRS Adv. 2018, 3, 3763–3768. [Google Scholar]
- Fouly, A.; Alkalla, M. Effect of low nanosized alumina loading fraction on the physicomechanical and tribological behavior of epoxy. Tribol. Int. 2020, 106550. [Google Scholar] [CrossRef]
- Bogdanova, L.; Lesnichaya, V.; Spirin, M.; Shershnev, V.; Irzhak, V.; Kydralieva, K.; Zarrelli, M.; Dzhardimalieva, G. Mechanical properties of polycondensate epoxy nanocomposites filled with Ag nanoparticles synthesized in situ. Mater. Today Proc. 2020. In press. [Google Scholar]
- Rafiee, M.A.; Rafiee, J.; Srivastava, I.; Wang, Z.; Song, H.; Yu, Z.Z.; Koratkar, N. Fracture and fatigue in graphene nanocomposites. Small 2010, 6, 179–183. [Google Scholar]
- Shen, X.J.; Pei, X.Q.; Fu, S.Y.; Friedrich, K. Significantly modified tribological performance of epoxy nanocomposites at very low graphene oxide content. Polymer 2013, 54, 1234–1242. [Google Scholar]
- Shi, G.; Zhang, M.Q.; Rong, M.Z.; Wetzel, B.; Friedrich, K. Sliding wear behavior of epoxy containing nano-Al2O3 particles with different pretreatments. Wear 2004, 256, 1072–1081. [Google Scholar]
- Ji, Q.L.; Zhang, M.Q.; Rong, M.Z.; Wetzel, B.; Friedrich, K. Tribological properties of surface modified nano-alumina/epoxy composites. J. Mater. Sci. 2004, 39, 6487–6493. [Google Scholar]
- Rameshkumar, C.; Sarojini, S.; Naresh, K.; Subalakshmi, R. Preparation and Characterization of Pristine PMMA and PVDF Thin Film Using Solution Casting Process for Optoelectronic Devices. J. Surf. Sci. Technol. 2017, 33, 12–18. [Google Scholar]
- Hashem, M.; Rez, M.F.; Fouad, H.; Elsarnagawy, T.; Elsharawy, M.A.; Umar, A.; Assery, M.; Ansari, S.G. Influence of titanium oxide nanoparticles on the physical and thermomechanical behavior of poly methyl methacrylate (PMMA): A denture base resin. Sci. Adv. Mater. 2017, 9, 938–944. [Google Scholar]
- Venkateswarlu, K.; Sreekanth, D.; Sandhyarani, M.; Muthupandi, V.; Bose, A.C.; Rameshbabu, N. X-ray peak profile analysis of nanostructured hydroxyapatite and fluorapatite. Int. J. Biosci. Biochem. Bioinforma. 2012, 2, 389–393. [Google Scholar]
- ASTM Committee D-20 on Plastics. Standard Test Methods for Density and Specific Gravity (Relative Density) of Plastics by Displacement; ASTM International: West Conshohocken, PA, USA, 2008. [Google Scholar]
- Zhao, H.; Allanson, D.; Ren, X.J. Use of shore hardness tests for in-process properties estimation/monitoring of silicone rubbers. J. Mater. Sci. Chem. Eng. 2015, 3, 142–147. [Google Scholar]
- E-Standard of American Society for Testing and Materials UU. G99, Standard Test Method for Wear Testing with a Pin-on-Disk Apparatus; ASTM International: West Conshohocken, PA, USA, 2008. [Google Scholar]
- Ünalan, F.; Gürbüz, Ö.; Nihan, N.; Bilgin, P.; Sermet, B. Effect of mica as filler on wear of denture teeth polymethylmethacrylate (PMMA) resin. Balk. J. Stomatol. 2007, 11, 133–137. [Google Scholar]
- Champagne, C.; Waggoner, W.; Ditmyer, M.; Casamassimo, P.S. Parental satisfaction with preveneered stainless steel crowns for primary anterior teeth. Pediatr. Dent. 2007, 29, 465–469. [Google Scholar]
- Panda, P.; Mishra, G.; Mantry, S.; Singh, S.K.; Sinha, S.P. A study on mechanical, thermal, and electrical properties of glass fiber-reinforced epoxy hybrid composites filled with plasma-synthesized AlN. J. Compos. Mater. 2014, 48, 3073–3082. [Google Scholar]
- Latief, F.H.; Chafidz, A.; Junaedi, H.; Alfozan, A.; Khan, R. Effect of Alumina Contents on the Physicomechanical Properties of Alumina (Al2O3) Reinforced Polyester Composites. Adv. Polym. Technol. 2019, 2019, 5173537. [Google Scholar] [CrossRef] [Green Version]
- Ramanathan, T.; Stankovich, S.; Dikin, D.A.; Liu, H.; Shen, H.; Nguyen, S.T.; Brinson, L.C. Graphitic nanofillers in PMMA nanocomposites—an investigation of particle size and dispersion and their influence on nanocomposite properties. J. Polym. Sci. Part B Polym. Phys. 2007, 45, 2097–2112. [Google Scholar]
- Powers, J.M.; Sakaguchi, R.L.; Craig, R.G. Craig’s Restorative Dental Materials; Sakaguchi, R.L., Powers, J.M., Eds.; Elsevier/Mosby: Philadelphia, PA, USA, 2012. [Google Scholar]
- Franklin, P.; Wood, D.J.; Bubb, N.L. Reinforcement of poly (methyl methacrylate) denture base with glass flake. Dent. Mater. 2005, 21, 365–370. [Google Scholar]
- Rajkumar, K.; Sirisha, P.; Sankar, M.R. Tribomechanical and Surface Topographical Investigations of Poly Methyl Methacrylate-Seashell Particle based Biocomposite. Procedia Mater. Sci. 2014, 5, 1248–1257. [Google Scholar] [CrossRef] [Green Version]
- Elmadani, A.A.; Radović, I.; Tomić, N.Z.; Petrović, M.; Stojanović, D.B.; Heinemann, R.J.; Radojević, V. Hybrid denture acrylic composites with nanozirconia and electrospun polystyrene fibers. PLoS ONE 2019, 14, e0226528. [Google Scholar]
- Ananthu, M.; Shamnadh, M.; Dileep, P.N. Experimental Evaluation on Mechanical Properties and Wear Resistance in PMMA Seashell Bionanocomposite for Medical Application. Mater. Today Proc. 2018, 5, 25657–25666. [Google Scholar]
- Chang, L.; Zhang, Z.; Zhang, H.; Friedrich, K. Effect of nanoparticles on the tribological behaviour of short carbon fibre reinforced poly (etherimide) composites. Tribol. Int. 2005, 38, 966–973. [Google Scholar]
- Khun, N.W.; Zhang, H.; Lim, L.H.; Yue, C.Y.; Hu, X.; Yang, J. Tribological properties of short carbon fibers reinforced epoxy composites. Friction 2014, 2, 226–239. [Google Scholar]
- Kuminek, T.; Aniołek, K.; Młyńczak, J. A numerical analysis of the contact stress distribution and physical modelling of abrasive wear in the tram wheel-frog system. Wear 2015, 328, 177–185. [Google Scholar]
- Tang, W.; Zhou, Y.; Zhu, H.; Yang, H. The effect of surface texturing on reducing the friction and wear of steel under lubricated sliding contact. Appl. Surf. Sci. 2013, 273, 199–204. [Google Scholar]
- Ibrahim, A.M.M.; Mohamed, A.F.A.; Fathelbab, A.M.; Essa, F.A. Enhancing the tribological performance of epoxy composites utilizing carbon nano fibers additives for journal bearings. Mater. Res. Express 2018, 6, 035307. [Google Scholar]
- Ibrahim, A.M.M.; Shi, X.; Zhang, A.; Yang, K.; Zhai, W. Tribological characteristics of NiAl matrix composites with 1.5 wt.% graphene at elevated temperatures: An experimental and theoretical study. Tribol. Trans. 2015, 58, 1076–1083. [Google Scholar]















Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fouly, A.; Ibrahim, A.M.M.; Sherif, E.-S.M.; FathEl-Bab, A.M.R.; Badran, A.H. Effect of Low Hydroxyapatite Loading Fraction on the Mechanical and Tribological Characteristics of Poly(Methyl Methacrylate) Nanocomposites for Dentures. Polymers 2021, 13, 857. https://doi.org/10.3390/polym13060857
Fouly A, Ibrahim AMM, Sherif E-SM, FathEl-Bab AMR, Badran AH. Effect of Low Hydroxyapatite Loading Fraction on the Mechanical and Tribological Characteristics of Poly(Methyl Methacrylate) Nanocomposites for Dentures. Polymers. 2021; 13(6):857. https://doi.org/10.3390/polym13060857
Chicago/Turabian StyleFouly, Ahmed, Ahmed Mohamed Mahmoud Ibrahim, El-Sayed M. Sherif, Ahmed M.R. FathEl-Bab, and A.H. Badran. 2021. "Effect of Low Hydroxyapatite Loading Fraction on the Mechanical and Tribological Characteristics of Poly(Methyl Methacrylate) Nanocomposites for Dentures" Polymers 13, no. 6: 857. https://doi.org/10.3390/polym13060857