Relationships between Flexural and Bonding Properties, Marginal Adaptation, and Polymerization Shrinkage in Flowable Composite Restorations for Dental Application
Abstract
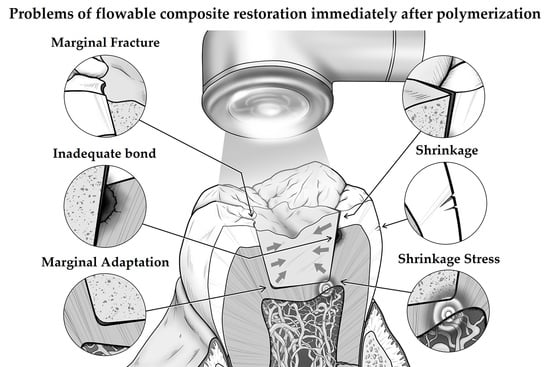
:1. Introduction
2. Materials and Methods
2.1. Measurement of Flexural Properties
2.2. Shear Bond Strength
2.3. Marginal Adaptation
2.4. Polymerization Shrinkage
2.5. Polymerization Shrinkage Stress
2.6. Statistical Analysis
3. Results
3.1. Flexural Properties
3.2. Shear Bond Strength
3.3. Marginal Adaptation
3.4. Polymerization Shrinkage
3.5. Polymerization Shrinkage Stress
3.6. Linear Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moraschini, V.; Fai, C.K.; Alto, R.M.; Santos, G.O.D. Amalgam and resin composite longevity of posterior restorations: A systematic review and meta-analysis. J. Dent. 2015, 43, 1043–1050. [Google Scholar] [CrossRef]
- Chesterman, J.; Jowett, A.; Gallacher, A.; Nixon, P. Bulk-fill resin-based composite restorative materials: A review. Br. Dent. J. 2017, 222, 337–344. [Google Scholar] [CrossRef]
- Tsujimoto, A.; Barkmeier, W.W.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Influence of thermal stress on simulated localized and generalized wear of nanofilled resin composites. Oper. Dent. 2018, 43, 380–390. [Google Scholar] [CrossRef]
- Bayne, S.C.; Thompson, J.Y.; Stamatiades, P.S.E.; Wilkerson, M. A characterization of first-generation flowable composites. J. Am. Dent. Assoc. 1998, 129, 567–577. [Google Scholar] [CrossRef]
- Lawson, N.C.; Radhakrishnan, R.; Givan, D.A.; Ramp, L.C.; Burgess, J.O. Two-year randomized, controlled clinical trial of a flowable and conventional composite in class I restorations. Oper. Dent. 2015, 40, 594–602. [Google Scholar] [CrossRef]
- Seemann, R.; Pfefferkorn, F.; Hickel, R. Behaviour of general dental practitioners in Germany regarding posterior restorations with flowable composites. Int. Dent. J. 2011, 61, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Boruziniat, A.; Gharaee, S.; Shirazi, A.S.; Majidinia, S.; Vatanpour, M. Evaluation of the efficacy of flowable composite as lining material on microleakage e of composite resin restorations: A systematic review and meta-analysis. Quintessence Int. 2016, 47, 93–101. [Google Scholar] [PubMed]
- Shimatani, Y.; Tsujimoto, A.; Barkmeier, W.W.; Fischer, N.G.; Nagura, Y.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Simulated cuspal deflection and flexural properties of bulk-fill and conventional flowable resin composites. Oper. Dent. 2020, 45, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Ujiie, M.; Tsujimoto, A.; Barkmeier, W.W.; Jurado, C.A.; Villalobos-Tinoco, J.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Comparison of occlusal wear between bulk-fill and conventional flowable resin composites. Am. J. Dent. 2020, 33, 74–78. [Google Scholar]
- Tsujimoto, A.; Jurado, C.A.; Barkmeier, W.W.; Sayed, M.E.; Takamizawa, T.; Latta, M.A.; Miyazaki, M.; Garcia-Godoy, F. Effect of layering techniques on polymerization shrinkage stress of high- and low-viscosity bulk-fill resins. Oper. Dent. 2020, 45, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Hirata-Tsuchiya, S.; Yoshii, S.; Ichimaru-Suematsu, M.; Washio, A.; Saito, N.; Urata, M.; Hanada, K.; Morotomi, T.; Kitamura, C. Two-year clinical comparison of a flowable-type nano-hybrid composite and a paste-type composite in posterior restoration. J. Investig. Clin. Dent. 2017, 8, e12227. [Google Scholar] [CrossRef]
- Kitasako, Y.; Sadr, A.; Burrow, M.F.; Tagami, J. Thirty-six month clinical evaluation of a highly filled flowable composite for direct posterior restorations. Aust. Dent. J. 2016, 61, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Guney, T.; Yazici, A.R. 24-month clinical evaluation of different bulk-fill restorative resins in Class II restorations. Oper. Dent. 2020, 45, 123–133. [Google Scholar] [CrossRef] [PubMed]
- American Dental Association. ACE Panel Report Posterior Composite Restorations ADA Clinical Evaluator (ACE) Panel Report; American Dental Association: Chicago, IL, USA, 2018. [Google Scholar]
- Hayashi, J.; Espigares, J.; Takagaki, T.; Shimada, Y.; Tagami, J.; Numata, T.; Chan, D.; Sadr, A. Real-time in-depth imaging of gap formation in bulk-fill resin composites. Dent. Mater. 2019, 35, 585–596. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, A.; Barkmeier, W.W.; Takamizawa, T.; Watanabe, H.; Johnson, W.W.; Latta, M.A.; Miyazaki, M. Simulated localized wear of resin luting cements for universal adhesive systems with different curing mode. J. Oral Sci. 2018, 60, 29–36. [Google Scholar] [CrossRef] [Green Version]
- Shinkai, K.; Taira, Y.; Suzuki, S.; Suzuki, M. In Vitro wear of flowable resin composite for posterior restorations. Dent. Mater. J. 2016, 35, 37–44. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, F.; Kawano, Y.; Braga, R.R. Contraction stress related to composite inorganic content. Dent. Mater. 2010, 26, 704–709. [Google Scholar] [CrossRef]
- Bicalho, A.A.; Valdívia, A.D.; Barreto, B.C.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Incremental filling technique and composite material—Part II: Shrinkage and shrinkage stresses. Oper. Dent. 2014, 39, e83–e93. [Google Scholar] [CrossRef]
- Meereis, C.T.W.; Münchow, E.A.; da Rosa, W.L.d.O.; da Silva, A.F.; Piva, E. Polymerization shrinkage stress of resin-based dental materials: A systematic review and meta-analyses of composition strategies. J. Mech. Behav. Biomed. Mater. 2018, 82, 268–281. [Google Scholar] [CrossRef]
- Irie, M.; Maruo, Y.; Nishigawa, G.; Suzuki, K.; Watts, D.C. Physical properties of dual-cured luting-agents correlated to early no interfacial-gap incidence with composite inlay restorations. Dent. Mater. 2010, 26, 608–615. [Google Scholar] [CrossRef]
- Sunbul, H.A.; Silikas, N.; Watts, D.C. Polymerization shrinkage kinetics and shrinkage-stress in dental resin-composites. Dent. Mater. 2016, 32, 998–1006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, S.H.; Sadr, A.; Shimada, Y.; Tagami, J.; Park, S.H. Internal adaptation of composite restorations with or without an intermediate layer: Effect of polymerization shrinkage parameters of the layer material. J. Dent. 2019, 80, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, J.; Tagami, J.; Chan, D.; Sadr, A. New bulk-fill composite system with high irradiance light polymerization: Integrity and degree of conversion. Dent. Mater. 2020, 36, 1615–1623. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, A.; Nagura, Y.; Barkmeier, W.W.; Watanabe, H.; Johnson, W.W.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Simulated cuspal deflection and flexural properties of high viscosity bulk-fill and conventional resin composites. J. Mech. Behav. Biomed. Mater. 2018, 87, 111–118. [Google Scholar] [CrossRef] [PubMed]

| Material (Abbrevistion) | Type of Composite (vol% of Fillers) | Main Components | Manufacturer |
|---|---|---|---|
| Beautifil Flow Plus X F03 (BF) | New generation flowable (50–60 vol%) | Bis-GMA, Bis-MPEPP, TEGDMA, Aluminofluoro-borosilicte glass filler, Photoinitiators, Accelerators, Pigments | Shofu, Kyoto, Japan |
| Clearfil Majesty ES Flow Low (CM) | New generation flowable (64 vol%, 78 wt%) | Hydrophobic aromatic dimethacrylate, TEGDMA, Silanated barium glass filler, Silanated silica filler, Photoinitiators, Accelerators, Pigments | Kuraray Noritake Dental, Tokyo, Japan |
| Estelite Universal Flow Medium Low (EU) | New generation flowable (57% vol%, 71 wt%) | Bis-GMA, Bis-MPEPP, TEGDMA, UDMA, Zirconia/silica filler, Photoinitiators, Accelerators, Pigments | Tokuyama Dental, Tokyo, Japan |
| G-ænial Universal Flo (GU) | New generation flowable (50 vol%, 69 wt%) | Bis-MPEPP, TEGDMA, UDMA, Silica filler, Strontium glass filler, Photoinitiators, Accelerators, Pigments | GC, Tokyo, Japan |
| Unifil LoFlow Plus (UP) | Conventional (42 vol%, 63 wt%) | UDMA, TEGDMA, Aluminofluoro-borosilicate glass filler, Photoinitiator, Accelerators, Pigments | GC, Tokyo, Japan |
| Filtek Bulk Fill Flowable Restorative (FF) | Bulk-fill (43 vol%, 65 wt%) | Bis-GMA, UDMA, Silica filler, Zirconia filler, Zirconia/silica cluster filler, Accelerators, Photoinitiators | 3M Oral Care, St. Paul, MN, USA |
| Universal Adhesive | Type of Polymerization | Main Components | Manufacturer |
|---|---|---|---|
| BeautiBond Universal | Light-cure | Bis-GMA, Carboxylic acid monomer, Phosphonic acid monomer, TEGDMA, Acetone, Water, Photoinitiators, Accelerator | Shofu, Kyoto, Japan |
| Clearfil Universal Bond | Light-cure | Bis-GMA, HEMA, Hydrophilic amide monomer, 10-MDP, Filler, Ethanol, Water, NaF, Photoinitiators, Accelerator, Silane coupling agent | Kuraray Noritake Dental, Tokyo, Japan |
| G-Premio Bond | Light-cure | MEPS, Methacrylate monomer, 4-MET, 10-MDP, Silica filler, Acetone, Water, Photoinitiators, Accelerator | GC, Tokyo, Japan |
| Scotchbond Universal Adhesive | Light-cure | Bis-GMA, HEMA, Decamethylene dimethacrylate, Ethyl methacrylate, Propenoic acid, Methyl-reaction products with decanediol and phosphorous oxide, Copolymer of acrylic and itaconic acid, Dimethylaminobenzoate, Methyl ethyl ketone, Silica filler, Ethanol, Water, Photoinitiators, Accelerator | 3M Oral Care, St. Paul, MN, USA |
| Tokuyama Universal Bond | Chemical-cure | Liquid A: Bis-GMA, HEMA, MTU-6 Phosphoric acid monomer, TEGDMA, Acetone, Others Liquid B: γ-MPTES, Acryl borate catalyst, Peroxide, Acetone, Isopropyl alcohol, Water, Others | Tokuyama Dental, Tokyo, Japan |
| Universal Adhesive | Application Protocol |
|---|---|
| BeautiBond Universal | Adhesive was applied to the air-dried surface for 10 s and then strong air pressure was applied over the liquid adhesive for 5 s or until adhesive no longer moved and the solvent was completely evaporated. Light-cured for 10 s. |
| Clearfil Universal Bond | Adhesive was applied to the air-dried surface for 10 s and then medium air pressure was applied over the liquid adhesive for 5 s or until adhesive no longer moved and the solvent was completely evaporated. Light-cured for 10 s. |
| G-Premio Bond | Adhesive was applied to the air-dried surface for 10 s and the strong air pressure was applied over the liquid adhesive for 5 s or until the adhesive no longer moved and the solvent was completely evaporated. Light-cure for 10 s. |
| Scotchbond Universal Adhesive | Adhesive was applied to the air-dried surface with a rubbing motion for 20 s and then medium air pressure was applied to the surface for 5 s. Adhesive was light cured for 10 s. |
| Tokuyama Universal Bond | Adhesive was applied to the air-dried surface for 10 s and then medium air pressure was applied over the liquid adhesive for 5 s. No light irradiation. |
| Material (Type of Composite) | FS (IM) (MPa) | FS (24 h) (MPa) | EM (IM) (GPa) | EM (24 h) (GPa) | SBS-E (IM) (MPa) | SBS-E (24 h) (MPa) | SBS-D (IM) (MPa) | SBS-D (24 h) (MPa) | MA (%) | PS (%) | PSS (µm) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| BF (New generation) | 95.2 (9.5) a,A | 128.6 (6.0) a,B | 4.12 (0.47) a,A | 8.27 (0.71) a,B | 14.0 (1.7) a,A | 21.2 (3.0) a,B | 13.2 (3.4) a,A | 20.1 (4.5) a,B | 0.22 (0.03) a | 3.95 (0.16) a | 15.44 (0.72) a |
| CM (New generation) | 51.3 (4.3) b,A | 151.7 (5.4) b,B | 2.07 (0.17) b,A | 7.52 (0.28) a,B | 14.8 (2.6) a,A | 21.0 (3.1) a,B | 16.0 (2.2) a,A | 21.1 (4.0) a,B | 0.16 (0.07) a | 3.53 (0.08) b | 13.82 (0.56) b |
| EU (New generation) | 102.4 (10.6) a,A | 152.3 (8.5) b,c,B | 5.04 (0.60) c,A | 8.28 (0.49) a,B | 14.8 (3.2) a,A | 19.7 (3.4) a,B | 15.2 (3.4) a,A | 21.4 (3.6) a,B | 0.19 (0.08) a | 3.18 (0.07) c | 15.77 (0.74) a |
| GU (New generation) | 80.3 (4.1) c,A | 162.0 (9.1) c,B | 3.22 (0.33) e,A | 9.24 (0.59) c,B | 15.2 (2.9) a,A | 20.5 (3.7) a,B | 14.1 (2.9) a,A | 19.1 (2.9) a,B | 0.20 (0.08) a | 3.47 (0.10) b | 12.07 (0.34) c |
| UP (Conventional) | 51.7 (4.0) b,A | 92.9 (6.7) d,B | 1.80 (0.30) b,A | 4.15 (0.41) e,B | 17.8 (3.6) a,A | 19.6 (5.3) a,A | 16.3 (3.1) a,A | 20.2 (3.3) a,B | 0.17 (0.04) a | 3.48 (0.08) b | 10.13 (0.56) d |
| FF (Bulk-fill) | 50.3 (1.8) b,A | 144.9 (5.3) b,B | 1.44 (0.22) d,A | 6.01 (0.49) b,B | 15.0 (2.7) a,A | 21.7 (3.8) a,B | 16.3 (2.6) a,A | 23.6 (3.0) a,B | 0.14 (0.09) a | 2.81 (0.12) d | 7.49 (0.36) e |
| Measured Indicators | R and p Values | FS (IM) | FS (24 h) | EM (IM) | EM (24 h) | SBS-E (IM) | SBS-E (24 h) | SBS-D (IM) | SBS-D (24 h) | MA | PS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| FS (24 h) | R | 0.3010 | - | - | - | - | - | - | - | - | - |
| p | 0.5621 | ||||||||||
| EM (IM) | R | 0.9828 | 0.3065 | - | - | - | - | - | - | - | - |
| p | 0.0004 | 0.5547 | |||||||||
| EM (24 h) | R | 0.7026 | 0.8072 | 0.6846 | - | - | - | - | - | - | - |
| p | 0.1195 | 0.0522 | 0.1335 | ||||||||
| SBS-E (IM) | R | −0.5143 | −0.7267 | −0.4907 | −0.7867 | - | - | - | - | - | - |
| p | 0.2965 | 0.1019 | 0.3230 | 0.0634 | |||||||
| SBS-E (24 h) | R | −0.2599 | 0.3526 | −0.3441 | 0.1699 | −0.6082 | - | - | - | - | - |
| p | 0.6189 | 0.4930 | 0.5042 | 0.7476 | 0.2002 | ||||||
| SBS-D (IM) | R | −0.7717 | −0.2397 | −0.6829 | −0.7351 | 0.5627 | −0.1215 | - | - | - | - |
| p | 0.0723 | 0.6474 | 0.1349 | 0.0959 | 0.2450 | 0.8186 | |||||
| SBS-D (24 h) | R | −0.3625 | 0.1257 | 0.3467 | 0.3484 | −0.1670 | 0.4605 | 0.5978 | - | - | - |
| p | 0.4801 | 0.8124 | 0.5008 | 0.4985 | 0.7518 | 0.3581 | 0.2101 | ||||
| MA | R | 0.8344 | 0.0408 | 0.7861 | 0.6165 | −0.3275 | −0.2376 | −0.9284 | −0.7499 | - | - |
| p | 0.0389 | 0.9389 | 0.0637 | 0.1924 | 0.5263 | 0.6504 | 0.0075 | 0.0860 | |||
| PS | R | 0.3331 | −0.2628 | 0.326 | 0.2800 | −0.1202 | −0.0973 | −0.663 | −0.7801 | 0.7491 | - |
| p | 0.5188 | 0.6148 | 0.5284 | 0.591 | 0.8206 | 0.8545 | 0.1485 | 0.0672 | 0.0865 | ||
| PSS | R | 0.7637 | 0.2463 | 0.8382 | 0.6820 | −0.4989 | −0.2757 | −0.6018 | −0.4632 | 0.7265 | 0.6192 |
| p | 0.0772 | 0.6380 | 0.0371 | 0.1639 | 0.2489 | 0.5969 | 0.2063 | 0.3549 | 0.102 | 0.1899 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsujimoto, A.; Irie, M.; Teixeira, E.C.N.; Jurado, C.A.; Maruo, Y.; Nishigawa, G.; Matsumoto, T.; Garcia-Godoy, F. Relationships between Flexural and Bonding Properties, Marginal Adaptation, and Polymerization Shrinkage in Flowable Composite Restorations for Dental Application. Polymers 2021, 13, 2613. https://doi.org/10.3390/polym13162613
Tsujimoto A, Irie M, Teixeira ECN, Jurado CA, Maruo Y, Nishigawa G, Matsumoto T, Garcia-Godoy F. Relationships between Flexural and Bonding Properties, Marginal Adaptation, and Polymerization Shrinkage in Flowable Composite Restorations for Dental Application. Polymers. 2021; 13(16):2613. https://doi.org/10.3390/polym13162613
Chicago/Turabian StyleTsujimoto, Akimasa, Masao Irie, Erica Cappelletto Nogueira Teixeira, Carlos Alberto Jurado, Yukinori Maruo, Goro Nishigawa, Takuya Matsumoto, and Franklin Garcia-Godoy. 2021. "Relationships between Flexural and Bonding Properties, Marginal Adaptation, and Polymerization Shrinkage in Flowable Composite Restorations for Dental Application" Polymers 13, no. 16: 2613. https://doi.org/10.3390/polym13162613