Multifunctional Bioactive Resin for Dental Restorative Materials
Abstract
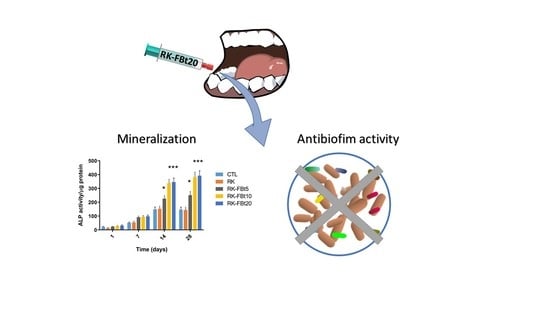
:1. Introduction
2. Materials and Methods
2.1. Sample Preparation
2.2. Characterization and Evaluation
2.2.1. Wide-Angle X-ray Diffraction (WAXD)
2.2.2. Gravimetric Measurements
2.2.3. Dynamic Mechanical Analysis
2.2.4. Fluoride Release Study
2.3. Biological Test Methods
2.3.1. Primary Cell Culture
2.3.2. Cytotoxicity Assay
2.3.3. Alkaline Phosphatase Activity
2.4. Microbiological Procedures
2.4.1. Bacteria
2.4.2. Direct Contact Test (DCT)
2.4.3. Biofilm Development under Dynamic Conditions
2.4.4. MTT Assay
2.5. Statistical Analysis
3. Results and Discussion
3.1. Structural Investigation
3.2. Water Absorption
3.3. Mechanical Properties
3.4. Resins Biocompatibility and Differentiation
3.5. Direct Contact Test (DCT)
3.6. Antibiofilm Analyses under Dynamic Conditions
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Marghalani, H.Y. Resin-Based Dental Composite Materials. In Handbook of Bioceramics and Biocomposites; Springer International Publishing: Berlin, Germany, 2016; pp. 357–405. [Google Scholar]
- Cramer, N.B.; Stansbury, J.W.; Bowman, C.N. Recent Advances and Developments in Composite Dental Restorative Materials. J. Dent. Res. 2011, 90, 402–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowen, R.L. Use of epoxy resins in restorative materials. J. Dent. Res. 1956, 35, 360–369. [Google Scholar] [CrossRef]
- Zagho, M.; Hussein, E.; Elzatahry, A. Recent Overviews in Functional Polymer Composites for Biomedical Applications. Polymers 2018, 10, 739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.; Darvell, B.W. Mechanical properties of hydroxyapatite whisker-reinforced bis-GMA-based resin composites. Dent. Mater. 2012, 28, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.W.H.S.H. Bentonite and fuller’s earth resources of the United States. Available online: https://pubs.er.usgs.gov/publication/pp1522 (accessed on 17 December 2019).
- Sorrentino, A.; Gorrasi, G.; Vittoria, V. Permeability in clay/polyesters nano-biocomposites. In Green Energy and Technology; Springer: London, UK, 2012; Volume 50, pp. 237–264. ISBN 9781447141013. [Google Scholar]
- Moosavi, M. Bentonite Clay as a Natural Remedy: A Brief Review. Iran. J. Public Health 2017, 46, 1176–1183. [Google Scholar]
- Gorrasi, G.; Milone, C.; Piperopoulos, E.; Lanza, M.; Sorrentino, A. Hybrid clay mineral-carbon nanotube-PLA nanocomposite films. Preparation and photodegradation effect on their mechanical, thermal and electrical properties. Appl. Clay Sci. 2013, 71, 49–54. [Google Scholar] [CrossRef]
- Miyazaki, M.; Ando, S.; Hinoura, K.; Onose, H.; Moore, B.K. Influence of filler addition to bonding agents on shear bond strength to bovine dentin. Dent. Mater. 1995, 11, 234–238. [Google Scholar] [CrossRef]
- Nunes, M.F.; Swift, E.J.; Perdigão, J. Effects of adhesive composition on microtensile bond strength to human dentin. Am. J. Dent. 2001, 14, 340–343. [Google Scholar]
- Atai, M.; Solhi, L.; Nodehi, A.; Mirabedini, S.M.; Kasraei, S.; Akbari, K.; Babanzadeh, S. PMMA-grafted nanoclay as novel filler for dental adhesives. Dent. Mater. 2009, 25, 339–347. [Google Scholar] [CrossRef]
- Nikolaidis, A.K.; Koulaouzidou, E.A.; Gogos, C.; Achilias, D.S. Synthesis and Characterization of Dental Nanocomposite Resins Filled with Different Clay Nanoparticles. Polymers 2019, 11, 730. [Google Scholar] [CrossRef] [Green Version]
- Soares, C.J.; Faria-E-Silva, A.L.; De Paula Rodrigues, M.; Vilela, A.B.F.; Pfeifer, C.S.; Tantbirojn, D.; Versluis, A. Polymerization shrinkage stress of composite resins and resin cements—What do we need to know? Braz. Oral Res. 2017, 31, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ersen, K.A.; Gürbüz, Ö.; Özcan, M. Evaluation of polymerization shrinkage of bulk-fill resin composites using microcomputed tomography. Clin. Oral Investig. 2019. [Google Scholar] [CrossRef] [PubMed]
- Fronza, B.M.; Lewis, S.; Shah, P.K.; Barros, M.D.; Giannini, M.; Stansbury, J.W. Modification of filler surface treatment of composite resins using alternative silanes and functional nanogels. Dent. Mater. 2019, 35, 928–936. [Google Scholar] [CrossRef] [PubMed]
- Tanner, J.; Tolvanen, M.; Garoushi, S.; Säilynoja, E. Clinical Evaluation of Fiber-Reinforced Composite Restorations in Posterior Teeth—Results of 2.5 Year Follow-up. Open Dent. J. 2018, 12, 476–485. [Google Scholar] [CrossRef]
- Nedeljkovic, I.; Teughels, W.; De Munck, J.; Van Meerbeek, B.; Van Landuyt, K.L. Is secondary caries with composites a material-based problem? Dent. Mater. 2015, 31, e247–e277. [Google Scholar] [CrossRef]
- Bernardo, M.; Luis, H.; Martin, M.D.; Leroux, B.G.; Rue, T.; Leitão, J.; DeRouen, T.A. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J. Am. Dent. Assoc. 2007, 138, 775–783. [Google Scholar] [CrossRef] [Green Version]
- Imazato, S.; McCabe, J.F. Influence of incorporation of antibacterial monomer on curing behavior of a dental composite. J. Dent. Res. 1994, 73, 1641–1645. [Google Scholar] [CrossRef] [Green Version]
- Mirsayar, M.M. On fracture analysis of dental restorative materials under combined tensile-shear loading. Theor. Appl. Fract. Mech. 2018, 93, 170–176. [Google Scholar] [CrossRef]
- Mirsayar, M.M.; Park, P. Modified maximum tangential stress criterion for fracture behavior of zirconia/veneer interfaces. J. Mech. Behav. Biomed. Mater. 2016, 59, 236–240. [Google Scholar] [CrossRef]
- Tavassoli Hojati, S.; Alaghemand, H.; Hamze, F.; Ahmadian Babaki, F.; Rajab-Nia, R.; Rezvani, M.B.; Kaviani, M.; Atai, M. Antibacterial, physical and mechanical properties of flowable resin composites containing zinc oxide nanoparticles. Dent. Mater. 2013, 29, 495–505. [Google Scholar] [CrossRef]
- Costantino, U.; Nocchetti, M.; Gorrasi, G.; Tammaro, L. Hydrotalcites in nanobiocomposites. In Multifunctional and Nanoreinforced Polymers for Food Packaging; Elsevier: Amsterdam, The Netherlands, 2011; pp. 43–85. [Google Scholar]
- Bugatti, V.; Esposito, L.; Franzetti, L.; Tammaro, L.; Vittoria, V. Influence of the powder dimensions on the antimicrobial properties of modified layered double hydroxide. Appl. Clay Sci. 2013, 75–76, 46–51. [Google Scholar] [CrossRef]
- Stencel, R.; Kasperski, J.; Pakieła, W.; Mertas, A.; Bobela, E.; Barszczewska-Rybarek, I.; Chladek, G. Properties of Experimental Dental Composites Containing Antibacterial Silver-Releasing Filler. Materials 2018, 11, 1031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, H.H.K.; Sun, L.; Weir, M.D.; Antonucci, J.M.; Takagi, S.; Chow, L.C.; Peltz, M. Nano DCPA-whisker composites with high strength and Ca and PO(4) release. J. Dent. Res. 2006, 85, 722–727. [Google Scholar] [CrossRef] [Green Version]
- Tammaro, L.; Vittoria, V.; Calarco, A.; Petillo, O.; Riccitiello, F.; Peluso, G. Effect of layered double hydroxide intercalated with fluoride ions on the physical, biological and release properties of a dental composite resin. J. Dent. 2014, 42, 60–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conte, R.; De Luise, A.; Valentino, A.; Di Cristo, F.; Petillo, O.; Riccitiello, F.; Di Salle, A.; Calarco, A.; Peluso, G. Hydrogel Nanocomposite Systems. In Nanocarriers for Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2019; pp. 319–349. [Google Scholar]
- Chenicheri, S.; Usha, R.; Ramachandran, R.; Thomas, V.; Wood, A. Insight into Oral Biofilm: Primary, Secondary and Residual Caries and Phyto-Challenged Solutions. Open Dent. J. 2017, 11, 312–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zitzmann, N.U.; Berglundh, T. Definition and prevalence of peri-implant diseases. J. Clin. Periodontol. 2008, 35, 286–291. [Google Scholar] [CrossRef]
- Albrektsson, T.; Buser, D.; Chen, S.T.; Cochran, D.; DeBruyn, H.; Jemt, T.; Koka, S.; Nevins, M.; Sennerby, L.; Simion, M.; et al. Statements from the Estepona Consensus Meeting on Peri-implantitis, February 2-4, 2012. Clin. Implant Dent. Relat. Res. 2012, 14, 781–782. [Google Scholar] [CrossRef]
- Wade, W.G. The oral microbiome in health and disease. Pharmacol. Res. 2013, 69, 137–143. [Google Scholar] [CrossRef]
- Calarco, A.; Di Salle, A.; Tammaro, L.; De Luca, I.; Mucerino, S.; Petillo, O.; Riccitiello, F.; Vittoria, V.; Peluso, G. Long-Term Fluoride Release from Dental Resins Affects STRO-1 + Cell Behavior. J. Dent. Res. 2015, 94, 1099–1105. [Google Scholar] [CrossRef] [Green Version]
- Di Salle, A.; Spagnuolo, G.; Conte, R.; Procino, A.; Peluso, G.; Rengo, C. Effects of various prophylactic procedures on titanium surfaces and biofilm formation. J. Periodontal Implant Sci. 2018, 48, 373. [Google Scholar] [CrossRef]
- Constructing and Using a Drip Flow Reactor. Available online: https://www.cs.montana.edu/webworks/projects/stevesbook/contents/chapters/chapter011/section021/blue/page001.html (accessed on 1 September 2019).
- He, Z.; Liang, J.; Zhou, W.; Xie, Q.; Tang, Z.; Ma, R.; Huang, Z. Effect of the quorum-sensing luxS gene on biofilm formation by Enterococcus faecalis. Eur. J. Oral Sci. 2016, 124, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, A.; Tortora, M.; Vittoria, V. Diffusion behavior in polymer-clay nanocomposites. J. Polym. Sci. Part B Polym. Phys. 2006, 44, 265–274. [Google Scholar] [CrossRef]
- Sorrentino, A.; Gorrasi, G.; Tortora, M.; Vittoria, V. Barrier properties of polymer/clay nanocomposites. In Polymer Nanocomposites; Mai, Y.-W., Yu, Z.-Z., Eds.; Elsevier: Cambridge, UK, 2006; pp. 273–296. ISBN 978-1-85573-969-7. [Google Scholar]
- Sorrentino, A. Nanocoatings and ultra-thin films for packaging applications. In Nanocoatings and Ultra-Thin Films; Makhlouf, A.S.H., Tiginyanu, I., Eds.; Elsevier: Oxford, UK, 2011; pp. 203–234. ISBN 9781845698126. [Google Scholar]
- La Noce, M.; Paino, F.; Spina, A.; Naddeo, P.; Montella, R.; Desiderio, V.; De Rosa, A.; Papaccio, G.; Tirino, V.; Laino, L. Dental pulp stem cells: State of the art and suggestions for a true translation of research into therapy. J. Dent. 2014, 42, 761–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, X.; van der Kraan, P.M.; Bian, Z.; Fan, M.; Walboomers, X.F.; Jansen, J.A. Mineralized Tissue Formation by BMP2-transfected Pulp Stem Cells. J. Dent. Res. 2009, 88, 1020–1025. [Google Scholar] [CrossRef] [PubMed]
- Weiss, E.I.; Shalhav, M.; Fuss, Z. Assessment of antibacterial activity of endodontic sealers by a direct contact test. Dent. Traumatol. 1996, 12, 179–184. [Google Scholar] [CrossRef]
- Stewart, P.S. Antimicrobial Tolerance in Biofilms. Microbiol. Spectr. 2015, 3. [Google Scholar] [CrossRef] [Green Version]
- Stoodley, P.; Dodds, I.; Boyle, J.D.; Lappin-Scott, H.M. Influence of hydrodynamics and nutrients on biofilm structure. J. Appl. Microbiol. 1998, 85, 19S–28S. [Google Scholar] [CrossRef] [Green Version]
- Zaltsman, N.; Ionescu, A.C.; Weiss, E.I.; Brambilla, E.; Beyth, S.; Beyth, N. Surface-modified nanoparticles as anti-biofilm filler for dental polymers. PLoS ONE 2017, 12, e0189397. [Google Scholar] [CrossRef] [Green Version]
- Yao, Y.; Berg, E.A.; Costello, C.E.; Troxler, R.F.; Oppenheim, F.G. Identification of protein components in human acquired enamel pellicle and whole saliva using novel proteomics approaches. J. Biol. Chem. 2003, 278, 5300–5308. [Google Scholar] [CrossRef] [Green Version]
- Größner-Schreiber, B.; Teichmann, J.; Hannig, M.; Dörfer, C.; Wenderoth, D.F.; Ott, S.J. Modified implant surfaces show different biofilm compositions under in vivo conditions. Clin. Oral Implants Res. 2009, 20, 817–826. [Google Scholar] [CrossRef]
- Thomas, W.E.; Trintchina, E.; Forero, M.; Vogel, V.; Sokurenko, E.V. Bacterial Adhesion to Target Cells Enhanced by Shear Force. Cell 2002, 109, 913–923. [Google Scholar] [CrossRef] [Green Version]
- Marquis, R.E. Antimicrobial actions of fluoride for oral bacteria. Can. J. Microbiol. 1995, 41, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Marquis, R.E.; Clock, S.A.; Mota-Meira, M. Fluoride and organic weak acids as modulators of microbial physiology. FEMS Microbiol. Rev. 2003, 26, 493–510. [Google Scholar] [CrossRef] [PubMed]
- Sturr, M.G.; Marquis, R.E. Inhibition of proton-translocating ATPases of Streptococcus mutans and Lactobacillus casei by fluoride and aluminum. Arch. Microbiol. 1990, 155, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Guha-Chowdhury, N.; Iwami, Y.; Yamada, T. Effect of Low Levels of Fluoride on Proton Excretion and Intracellular pH in Glycolysing Streptococcal Cells under Strictly Anaerobic Conditions. Caries Res. 1997, 31, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Guha-Chowdhury, N.; Clark, A.G.; Sissons, C.H. Inhibition of purified enolases from oral bacteria by fluoride. Oral Microbiol. Immunol. 1997, 12, 91–97. [Google Scholar] [CrossRef]
- Matsui, R.; Cvitkovitch, D. Acid tolerance mechanisms utilized by Streptococcus mutans. Future Microbiol. 2010, 5, 403–417. [Google Scholar] [CrossRef] [Green Version]














| Streptococcus spp. | B. fragilis | S. epidermidis | |
|---|---|---|---|
| Test details | P | P | P |
| CTL vs. RK | n.s. | n.s. | n.s. |
| CTL vs. RK-FBt5 | n.s. | n.s. | n.s. |
| CTL vs. RK-FBt10 | 0.0041 | 0.0044 | 0.0031 |
| CTL vs. RK-FBt20 | <0.0001 | <0.0001 | <0.0001 |
| RK vs. RK-FBt5 | n.s. | n.s. | n.s. |
| RK vs. RK-FBt10 | n.s. | n.s. | n.s. |
| RK vs. RK-FBt20 | 0.0025 | 0.0033 | 0.0040 |
| RK-FBt5 vs. RK-FBt10 | n.s. | n.s. | n.s. |
| RK-FBt5 vs. RK-FBt20 | n.s. | n.s. | n.s. |
| RK-FBt10 vs. RK-FBt20 | n.s. | n.s. | n.s. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tammaro, L.; Di Salle, A.; Calarco, A.; De Luca, I.; Riccitiello, F.; Peluso, G.; Vittoria, V.; Sorrentino, A. Multifunctional Bioactive Resin for Dental Restorative Materials. Polymers 2020, 12, 332. https://doi.org/10.3390/polym12020332
Tammaro L, Di Salle A, Calarco A, De Luca I, Riccitiello F, Peluso G, Vittoria V, Sorrentino A. Multifunctional Bioactive Resin for Dental Restorative Materials. Polymers. 2020; 12(2):332. https://doi.org/10.3390/polym12020332
Chicago/Turabian StyleTammaro, Loredana, Anna Di Salle, Anna Calarco, Ilenia De Luca, Francesco Riccitiello, Gianfranco Peluso, Vittoria Vittoria, and Andrea Sorrentino. 2020. "Multifunctional Bioactive Resin for Dental Restorative Materials" Polymers 12, no. 2: 332. https://doi.org/10.3390/polym12020332