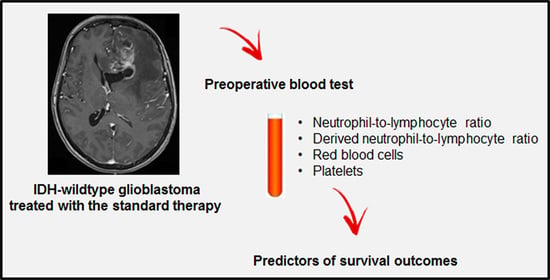
A Simple Preoperative Blood Count to Stratify Prognosis in Isocitrate Dehydrogenase-Wildtype Glioblastoma Patients Treated with Radiotherapy plus Concomitant and Adjuvant Temozolomide
Abstract
:Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Univariate and Multivariate Analyses
3.3. Survival Analysis of Independent Prognostic Hematological Markers
3.4. A Scoring System Based on Preoperative Platelet and RBC Counts plus NLR or dNLR
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Stupp, R.; Hegi, M.E.; Mason, W.P.; van den Bent, M.J.; Taphoorn, M.J.B.; Janzer, R.C.; Ludwin, S.K.; Allgeier, A.; Fisher, B.; Belanger, K.; et al. Effects of Radiotherapy with Concomitant and Adjuvant Temozolomide versus Radiotherapy Alone on Survival in Glioblastoma in a Randomised Phase III Study: 5-Year Analysis of the EORTC-NCIC Trial. Lancet Oncol. 2009, 10, 459–466. [Google Scholar] [CrossRef]
- Poon, M.T.C.; Sudlow, C.L.M.; Figueroa, J.D.; Brennan, P.M. Longer-Term (≥2 Years) Survival in Patients with Glioblastoma in Population-Based Studies Pre- and Post-2005: A Systematic Review and Meta-Analysis. Sci. Rep. 2020, 10, 11622. [Google Scholar] [CrossRef]
- Liang, J.; Lv, X.; Lu, C.; Ye, X.; Chen, X.; Fu, J.; Luo, C.; Zhao, Y. Prognostic Factors of Patients with Gliomas—An Analysis on 335 Patients with Glioblastoma and Other Forms of Gliomas. BMC Cancer 2020, 20, 35. [Google Scholar] [CrossRef] [Green Version]
- Kartik, R.; Lee, G.R.; Lee, C.C.; Tang, P.-Y.; Grace, K.; Chua, L.M.K.; Lee, H.Y.; Koh, W.Y.; Tham, C.K.; Ng, W.H.; et al. Clinical Prognostic Factors of Survival in Glioblastoma Multiforme. Neurology 2020, 94, 2593. [Google Scholar]
- Burgenske, D.M.; Yang, J.; Decker, P.A.; Kollmeyer, T.M.; Kosel, M.L.; Mladek, A.C.; Caron, A.A.; Vaubel, R.A.; Gupta, S.K.; Kitange, G.J.; et al. Molecular Profiling of Long-Term IDH-Wildtype Glioblastoma Survivors. Neuro Oncol. 2019, 21, 1458–1469. [Google Scholar] [CrossRef]
- Cantero, D.; Rodríguez de Lope, Á.; Moreno de la Presa, R.; Sepúlveda, J.M.; Borrás, J.M.; Castresana, J.S.; D’Haene, N.; García, J.F.; Salmon, I.; Mollejo, M.; et al. Molecular Study of Long-Term Survivors of Glioblastoma by Gene-Targeted Next-Generation Sequencing. J. Neuropathol. Exp. Neurol. 2018, 77, 710–716. [Google Scholar] [CrossRef]
- Gately, L.; McLachlan, S.A.; Philip, J.; Rathi, V.; Dowling, A. Molecular Profile of Long-Term Survivors of Glioblastoma: A Scoping Review of the Literature. J. Clin. Neurosci. 2019, 68, 1–8. [Google Scholar] [CrossRef]
- Sylman, J.L.; Mitrugno, A.; Atallah, M.; Tormoen, G.W.; Shatzel, J.J.; Tassi Yunga, S.; Wagner, T.H.; Leppert, J.T.; Mallick, P.; McCarty, O.J.T. The Predictive Value of Inflammation-Related Peripheral Blood Measurements in Cancer Staging and Prognosis. Front. Oncol. 2018, 8, 78. [Google Scholar] [CrossRef] [Green Version]
- Yang, C.; Wen, H.-B.; Zhao, Y.-H.; Huang, W.-H.; Wang, Z.-F.; Li, Z.-Q. Systemic Inflammatory Indicators as Prognosticators in Glioblastoma Patients: A Comprehensive Meta-Analysis. Front. Neurol. 2020, 11, 580101. [Google Scholar] [CrossRef] [PubMed]
- Gomes Dos Santos, A.; de Carvalho, R.F.; de Morais, A.N.L.R.; Silva, T.M.; Baylão, V.M.R.; Azevedo, M.; de Oliveira, A.J.M. Role of Neutrophil-Lymphocyte Ratio as a Predictive Factor of Glioma Tumor Grade: A Systematic Review. Crit. Rev. Oncol. Hematol. 2021, 163, 103372. [Google Scholar] [CrossRef]
- Lei, Y.-Y.; Li, Y.-T.; Hu, Q.-L.; Wang, J.; Sui, A.-X. Prognostic Impact of Neutrophil-to-Lymphocyte Ratio in Gliomas: A Systematic Review and Meta-Analysis. World J. Surg. Oncol. 2019, 17, 152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Lang, F.; Chou, F.-J.; Zaghloul, K.A.; Yang, C. Isocitrate Dehydrogenase Mutations in Glioma: Genetics, Biochemistry, and Clinical Indications. Biomedicines 2020, 8, 294. [Google Scholar] [CrossRef]
- Amankulor, N.M.; Kim, Y.; Arora, S.; Kargl, J.; Szulzewsky, F.; Hanke, M.; Margineantu, D.H.; Rao, A.; Bolouri, H.; Delrow, J.; et al. Mutant IDH1 Regulates the Tumor-Associated Immune System in Gliomas. Genes Dev. 2017, 31, 774–786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Auezova, R.; Ivanova, N.; Akshulakov, S.; Zhetpisbaev, B.; Kozhakhmetova, A.; Ryskeldiyev, N.; Mustafin, K.; Teltayev, D.; Auezova, L. Isocitrate Dehydrogenase 1 Mutation Is Associated with Reduced Levels of Inflammation in Glioma Patients. Cancer Manag. Res. 2019, 11, 3227–3236. [Google Scholar] [CrossRef] [Green Version]
- Sharma, G.; Jain, S.K.; Sinha, V.D. Peripheral Inflammatory Blood Markers in Diagnosis of Glioma and IDH Status. J. Neurosci. Rural Pract. 2021, 12, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Louis, D.N.; Perry, A.; Wesseling, P.; Brat, D.J.; Cree, I.A.; Figarella-Branger, D.; Hawkins, C.; Ng, H.K.; Pfister, S.M.; Reifenberger, G.; et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A Summary. Neuro Oncol. 2021, 23, 1231–1251. [Google Scholar] [CrossRef]
- Métais, A.; Rousseau, A. Histomolecular diagnosis of glial and glioneuronal tumours. Ann. Pathol. 2021, 41, 137–153. [Google Scholar] [CrossRef]
- Wen, P.Y.; Macdonald, D.R.; Reardon, D.A.; Cloughesy, T.F.; Sorensen, A.G.; Galanis, E.; Degroot, J.; Wick, W.; Gilbert, M.R.; Lassman, A.B.; et al. Updated Response Assessment Criteria for High-Grade Gliomas: Response Assessment in Neuro-Oncology Working Group. J. Clin. Oncol. 2010, 28, 1963–1972. [Google Scholar] [CrossRef]
- Alimohammadi, E.; Bagheri, S.R.; Taheri, S.; Dayani, M.; Abdi, A. The Impact of Extended Adjuvant Temozolomide in Newly Diagnosed Glioblastoma Multiforme: A Meta-Analysis and Systematic Review. Oncol. Rev. 2020, 14, 461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darlix, A.; Baumann, C.; Lorgis, V.; Ghiringhelli, F.; Blonski, M.; Chauffert, B.; Zouaoui, S.; Pinelli, C.; Rech, F.; Beauchesne, P.; et al. Prolonged Administration of Adjuvant Temozolomide Improves Survival in Adult Patients with Glioblastoma. Anticancer Res. 2013, 33, 3467–3474. [Google Scholar]
- Zheng, L.; Zhou, Z.-R.; Shi, M.; Chen, H.; Yu, Q.-Q.; Yang, Y.; Liu, L.; Zhang, L.; Guo, Y.; Zhou, X.; et al. Nomograms for Predicting Progression-Free Survival and Overall Survival after Surgery and Concurrent Chemoradiotherapy for Glioblastoma: A Retrospective Cohort Study. Ann. Transl. Med. 2021, 9, 571. [Google Scholar] [CrossRef]
- Bambury, R.M.; Teo, M.Y.; Power, D.G.; Yusuf, A.; Murray, S.; Battley, J.E.; Drake, C.; O’Dea, P.; Bermingham, N.; Keohane, C.; et al. The Association of Pre-Treatment Neutrophil to Lymphocyte Ratio with Overall Survival in Patients with Glioblastoma Multiforme. J. Neuro Oncol. 2013, 114, 149–154. [Google Scholar] [CrossRef]
- Han, S.; Liu, Y.; Li, Q.; Li, Z.; Hou, H.; Wu, A. Pre-Treatment Neutrophil-to-Lymphocyte Ratio Is Associated with Neutrophil and T-Cell Infiltration and Predicts Clinical Outcome in Patients with Glioblastoma. BMC Cancer 2015, 15, 617. [Google Scholar] [CrossRef] [Green Version]
- Wang, P.-F.; Song, H.-W.; Cai, H.-Q.; Kong, L.-W.; Yao, K.; Jiang, T.; Li, S.-W.; Yan, C.-X. Preoperative Inflammation Markers and IDH Mutation Status Predict Glioblastoma Patient Survival. Oncotarget 2017, 8, 50117–50123. [Google Scholar] [CrossRef] [Green Version]
- Kaya, V.; Yıldırım, M.; Yazıcı, G.; Yalçın, A.Y.; Orhan, N.; Güzel, A. Prognostic Significance of Indicators of Systemic Inflammatory Responses in Glioblastoma Patients. Asian Pac. J. Cancer Prev. APJCP 2017, 18, 3287–3291. [Google Scholar] [CrossRef]
- Lopes, M.; Carvalho, B.; Vaz, R.; Linhares, P. Influence of Neutrophil-Lymphocyte Ratio in Prognosis of Glioblastoma Multiforme. J. Neuro Oncol. 2018, 136, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.; Chen, X.; Gong, S.; Guo, L.; Zhang, X. Preoperative Neutrophil-Lymphocyte Ratio Correlated with Glioma Grading and Glioblastoma Survival. Neurol. Res. 2018, 40, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Lv, Y.; Zhang, S.; Liu, Z.; Tian, Y.; Liang, N.; Zhang, J. Prognostic Value of Preoperative Neutrophil to Lymphocyte Ratio Is Superior to Systemic Immune Inflammation Index for Survival in Patients with Glioblastoma. Clin. Neurol. Neurosurg. 2019, 181, 24–27. [Google Scholar] [CrossRef]
- Marini, A.; Dobran, M.; Aiudi, D.; Pesaresi, A.; di Somma, L.G.M.; Iacoangeli, M. Pre-Operative Hematological Markers as Predictive Factors for Overall Survival and Progression Free Survival in Glioblastomas. Clin. Neurol. Neurosurg. 2020, 197, 106162. [Google Scholar] [CrossRef]
- Maas, S.L.N.; Draaisma, K.; Snijders, T.J.; Senders, J.T.; Berendsen, S.; Seute, T.; Schiffelers, R.M.; van Solinge, W.W.; Ten Berg, M.J.; Robe, P.A.; et al. Routine Blood Tests Do Not Predict Survival in Patients with Glioblastoma—Multivariable Analysis of 497 Patients. World Neurosurg. 2019, 126, e1081–e1091. [Google Scholar] [CrossRef] [PubMed]
- Madhugiri, V.S.; Moiyadi, A.V.; Shetty, P.; Gupta, T.; Epari, S.; Jalali, R.; Subeikshanan, V.; Dutt, A.; Sasidharan, G.M.; Roopesh Kumar, V.R.; et al. Analysis of Factors Associated with Long-Term Survival in Patients with Glioblastoma. World Neurosurg. 2021, 149, e758–e765. [Google Scholar] [CrossRef]
- Zhao, C.; Li, L.; Guo, X.; Song, D.; Wang, M.; Zhai, Y.; Yang, F.; Xue, Y.; Wei, X. Preoperative Predictors of Early Mortality Risk in Isocitrate Dehydrogenase-Wild-Type Glioblastoma Patients Treated with Standard Therapy. Cancer Manag. Res. 2021, 13, 1159–1168. [Google Scholar] [CrossRef]
- Alexiou, G.A.; Vartholomatos, E.; Voulgaris, S. Prognostic Value of Neutrophil-to-Lymphocyte Ratio in Patients with Glioblastoma. J. Neuro Oncol. 2013, 115, 521–522. [Google Scholar] [CrossRef]
- Mason, M.; Maurice, C.; McNamara, M.G.; Tieu, M.T.; Lwin, Z.; Millar, B.-A.; Menard, C.; Laperriere, N.; Milosevic, M.; Atenafu, E.G.; et al. Neutrophil-Lymphocyte Ratio Dynamics during Concurrent Chemo-Radiotherapy for Glioblastoma Is an Independent Predictor for Overall Survival. J. Neuro Oncol. 2017, 132, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.-W.; Dong, H.; Yang, Y.; Luo, J.-W.; Wang, X.; Liu, Y.-H.; Mao, Q. Significance of the Prognostic Nutritional Index in Patients with Glioblastoma: A Retrospective Study. Clin. Neurol. Neurosurg. 2016, 151, 86–91. [Google Scholar] [CrossRef]
- Yersal, Ö.; Odabaşi, E.; Özdemir, Ö.; Kemal, Y. Prognostic Significance of Pre-Treatment Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Patients with Glioblastoma. Mol. Clin. Oncol. 2018, 9, 453–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brenner, A.; Friger, M.; Geffen, D.B.; Kaisman-Elbaz, T.; Lavrenkov, K. The Prognostic Value of the Pretreatment Neutrophil/Lymphocyte Ratio in Patients with Glioblastoma Multiforme Brain Tumors: A Retrospective Cohort Study of Patients Treated with Combined Modality Surgery, Radiation Therapy, and Temozolomide Chemotherapy. Oncology 2019, 97, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Garrett, C.; Becker, T.M.; Lynch, D.; Po, J.; Xuan, W.; Scott, K.F.; de Souza, P. Comparison of Neutrophil to Lymphocyte Ratio and Prognostic Nutritional Index with Other Clinical and Molecular Biomarkers for Prediction of Glioblastoma Multiforme Outcome. PLoS ONE 2021, 16, e0252614. [Google Scholar] [CrossRef]
- Proctor, M.J.; McMillan, D.C.; Morrison, D.S.; Fletcher, C.D.; Horgan, P.G.; Clarke, S.J. A Derived Neutrophil to Lymphocyte Ratio Predicts Survival in Patients with Cancer. Br. J. Cancer 2012, 107, 695–699. [Google Scholar] [CrossRef] [Green Version]
- Zheng, S.-H.; Huang, J.-L.; Chen, M.; Wang, B.-L.; Ou, Q.-S.; Huang, S.-Y. Diagnostic Value of Preoperative Inflammatory Markers in Patients with Glioma: A Multicenter Cohort Study. J. Neurosurg. 2018, 129, 583–592. [Google Scholar] [CrossRef] [Green Version]
- Khan, S.; Mittal, S.; McGee, K.; Alfaro-Munoz, K.D.; Majd, N.; Balasubramaniyan, V.; de Groot, J.F. Role of Neutrophils and Myeloid-Derived Suppressor Cells in Glioma Progression and Treatment Resistance. Int. J. Mol. Sci. 2020, 21, 1954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, J.; Piao, Y.; Holmes, L.; Fuller, G.N.; Henry, V.; Tiao, N.; de Groot, J.F. Neutrophils Promote the Malignant Glioma Phenotype through S100A4. Clin. Cancer Res. 2014, 20, 187–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massara, M.; Persico, P.; Bonavita, O.; Mollica Poeta, V.; Locati, M.; Simonelli, M.; Bonecchi, R. Neutrophils in Gliomas. Front. Immunol. 2017, 8, 1349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahbar, A.; Cederarv, M.; Wolmer-Solberg, N.; Tammik, C.; Stragliotto, G.; Peredo, I.; Fornara, O.; Xu, X.; Dzabic, M.; Taher, C.; et al. Enhanced Neutrophil Activity Is Associated with Shorter Time to Tumor Progression in Glioblastoma Patients. Oncoimmunology 2016, 5, e1075693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sippel, T.R.; White, J.; Nag, K.; Tsvankin, V.; Klaassen, M.; Kleinschmidt-DeMasters, B.K.; Waziri, A. Neutrophil Degranulation and Immunosuppression in Patients with GBM: Restoration of Cellular Immune Function by Targeting Arginase I. Clin. Cancer Res. 2011, 17, 6992–7002. [Google Scholar] [CrossRef] [Green Version]
- Yee, P.P.; Wei, Y.; Kim, S.-Y.; Lu, T.; Chih, S.Y.; Lawson, C.; Tang, M.; Liu, Z.; Anderson, B.; Thamburaj, K.; et al. Neutrophil-Induced Ferroptosis Promotes Tumor Necrosis in Glioblastoma Progression. Nat. Commun. 2020, 11, 5424. [Google Scholar] [CrossRef] [PubMed]
- Zha, C.; Meng, X.; Li, L.; Mi, S.; Qian, D.; Li, Z.; Wu, P.; Hu, S.; Zhao, S.; Cai, J.; et al. Neutrophil Extracellular Traps Mediate the Crosstalk between Glioma Progression and the Tumor Microenvironment via the HMGB1/RAGE/IL-8 Axis. Cancer Biol. Med. 2020, 17, 154–168. [Google Scholar] [CrossRef]
- Fossati, G.; Ricevuti, G.; Edwards, S.W.; Walker, C.; Dalton, A.; Rossi, M.L. Neutrophil Infiltration into Human Gliomas. Acta Neuropathol. 1999, 98, 349–354. [Google Scholar] [CrossRef]
- Masucci, M.T.; Minopoli, M.; Carriero, M.V. Tumor Associated Neutrophils. Their Role in Tumorigenesis, Metastasis, Prognosis and Therapy. Front. Oncol. 2019, 9, 1146. [Google Scholar] [CrossRef] [Green Version]
- Mukaida, N.; Sasaki, S.-I.; Baba, T. Two-Faced Roles of Tumor-Associated Neutrophils in Cancer Development and Progression. Int. J. Mol. Sci. 2020, 21, 3457. [Google Scholar] [CrossRef]
- Kaplan, M.J.; Radic, M. Neutrophil Extracellular Traps: Double-Edged Swords of Innate Immunity. J. Immunol. 2012, 189, 2689–2695. [Google Scholar] [CrossRef] [Green Version]
- Brockmann, M.A.; Giese, A.; Mueller, K.; Kaba, F.J.; Lohr, F.; Weiss, C.; Gottschalk, S.; Nolte, I.; Leppert, J.; Tuettenberg, J.; et al. Preoperative Thrombocytosis Predicts Poor Survival in Patients with Glioblastoma. Neuro Oncol. 2007, 9, 335–342. [Google Scholar] [CrossRef]
- Lee, Y.S.; Suh, K.W.; Oh, S.Y. Preoperative Thrombocytosis Predicts Prognosis in Stage II Colorectal Cancer Patients. Ann. Surg. Treat. Res. 2016, 90, 322–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, A.J.; Madden, A.C.; Cass, I.; Leuchter, R.S.; Lagasse, L.D.; Karlan, B.Y. The Prognostic Significance of Thrombocytosis in Epithelial Ovarian Carcinoma. Gynecol. Oncol. 2004, 92, 211–214. [Google Scholar] [CrossRef]
- Yu, D.; Liu, B.; Zhang, L.; Du, K. Platelet Count Predicts Prognosis in Operable Non-Small Cell Lung Cancer. Exp. Ther. Med. 2013, 5, 1351–1354. [Google Scholar] [CrossRef] [Green Version]
- Tahtaci, G.; Gunel, N.; Uner, A.; Tahtaci, M. Prognostic Value of Mean Platelet Volume in Glioblastoma Multiforme. Gazi Med. J. 2018, 29, 336–339. [Google Scholar] [CrossRef]
- Marx, S.; Xiao, Y.; Baschin, M.; Splittstöhser, M.; Altmann, R.; Moritz, E.; Jedlitschky, G.; Bien-Möller, S.; Schroeder, H.W.S.; Rauch, B.H. The Role of Platelets in Cancer Pathophysiology: Focus on Malignant Glioma. Cancers 2019, 11, 569. [Google Scholar] [CrossRef] [Green Version]
- Brockmann, M.A.; Bender, B.; Plaxina, E.; Nolte, I.; Erber, R.; Lamszus, K.; Groden, C.; Schilling, L. Differential Effects of Tumor-Platelet Interaction in Vitro and in Vivo in Glioblastoma. J. Neuro Oncol. 2011, 105, 45–56. [Google Scholar] [CrossRef]
- Campanella, R.; Guarnaccia, L.; Cordiglieri, C.; Trombetta, E.; Caroli, M.; Carrabba, G.; La Verde, N.; Rampini, P.; Gaudino, C.; Costa, A.; et al. Tumor-Educated Platelets and Angiogenesis in Glioblastoma: Another Brick in the Wall for Novel Prognostic and Targetable Biomarkers, Changing the Vision from a Localized Tumor to a Systemic Pathology. Cells 2020, 9, 294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Vito, C.; Navone, S.E.; Marfia, G.; Abdel Hadi, L.; Mancuso, M.E.; Pecci, A.; Crisà, F.M.; Berno, V.; Rampini, P.; Campanella, R.; et al. Platelets from Glioblastoma Patients Promote Angiogenesis of Tumor Endothelial Cells and Exhibit Increased VEGF Content and Release. Platelets 2017, 28, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Marx, S.; Splittstöhser, M.; Kinnen, F.; Moritz, E.; Joseph, C.; Paul, S.; Paland, H.; Seifert, C.; Marx, M.; Böhm, A.; et al. Platelet Activation Parameters and Platelet-Leucocyte-Conjugate Formation in Glioblastoma Multiforme Patients. Oncotarget 2018, 9, 25860–25876. [Google Scholar] [CrossRef] [PubMed]
- Wach, J.; Apallas, S.; Schneider, M.; Weller, J.; Schuss, P.; Vatter, H.; Herrlinger, U.; Güresir, E. Mean Platelet Volume/Platelet Count Ratio and Risk of Progression in Glioblastoma. Front. Oncol. 2021, 11, 695316. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.-Z.; Yang, Y.-C.; Chen, Y.; Wu, C.-C.; Lin, R.-F.; Wang, Z.-N.; Zhang, X. Preoperative Anemia or Low Hemoglobin Predicts Poor Prognosis in Gastric Cancer Patients: A Meta-Analysis. Dis. Markers 2019, 2019, 7606128. [Google Scholar] [CrossRef]
- Liu, Z.; Luo, J.-J.; Pei, K.Y.; Khan, S.A.; Wang, X.-X.; Zhao, Z.-X.; Yang, M.; Johnson, C.H.; Wang, X.-S.; Zhang, Y. Joint Effect of Pre-Operative Anemia and Perioperative Blood Transfusion on Outcomes of Colon-Cancer Patients Undergoing Colectomy. Gastroenterol. Rep. 2020, 8, 151–157. [Google Scholar] [CrossRef]
- Wilson, M.J.; van Haaren, M.; Harlaar, J.J.; Park, H.C.; Bonjer, H.J.; Jeekel, J.; Zwaginga, J.J.; Schipperus, M. Long-Term Prognostic Value of Preoperative Anemia in Patients with Colorectal Cancer: A Systematic Review and Meta-Analysis. Surg. Oncol. 2017, 26, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Xia, L.; Guzzo, T.J. Preoperative Anemia and Low Hemoglobin Level Are Associated With Worse Clinical Outcomes in Patients With Bladder Cancer Undergoing Radical Cystectomy: A Meta-Analysis. Clin. Genitourin. Cancer 2017, 15, 263–272.e4. [Google Scholar] [CrossRef] [PubMed]
- Kaisman-Elbaz, T.; Elbaz, Y.; Merkin, V.; Dym, L.; Noy, A.; Atar-Vardi, M.; Bari, R.; Turiel, S.; Alt, A.; Zamed, T.; et al. Hemoglobin Levels and Red Blood Cells Distribution Width Highlights Glioblastoma Patients Subgroup With Improved Median Overall Survival. Front. Oncol. 2020, 10, 432. [Google Scholar] [CrossRef]
- Lutterbach, J.; Sauerbrei, W.; Guttenberger, R. Multivariate Analysis of Prognostic Factors in Patients with Glioblastoma. Strahlenther. Onkol. 2003, 179, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Liang, R.-F.; Li, M.; Yang, Y.; Mao, Q.; Liu, Y.-H. Significance of Pretreatment Red Blood Cell Distribution Width in Patients with Newly Diagnosed Glioblastoma. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 3217–3223. [Google Scholar] [CrossRef] [Green Version]
- Höckel, M.; Vaupel, P. Tumor Hypoxia: Definitions and Current Clinical, Biologic, and Molecular Aspects. J. Natl. Cancer Inst. 2001, 93, 266–276. [Google Scholar] [CrossRef] [Green Version]
- Monteiro, A.R.; Hill, R.; Pilkington, G.J.; Madureira, P.A. The Role of Hypoxia in Glioblastoma Invasion. Cells 2017, 6, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chédeville, A.L.; Madureira, P.A. The Role of Hypoxia in Glioblastoma Radiotherapy Resistance. Cancers 2021, 13, 542. [Google Scholar] [CrossRef] [PubMed]
- Stüben, G.; Thews, O.; Pöttgen, C.; Knühmann, K.; Sack, H.; Stuschke, M.; Vaupel, P. Impact of Anemia Prevention by Recombinant Human Erythropoietin on the Sensitivity of Xenografted Glioblastomas to Fractionated Irradiation. Strahlenther. Onkol. 2003, 179, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.Y.; Kim, S. Determination of Cutoff Values for Biomarkers in Clinical Studies. Precis. Future Med. 2020, 4, 2–8. [Google Scholar] [CrossRef]
- Clavreul, A.; Menei, P. Mesenchymal Stromal-Like Cells in the Glioma Microenvironment: What Are These Cells? Cancers 2020, 12, 2628. [Google Scholar] [CrossRef]
- Clavreul, A.; Soulard, G.; Lemée, J.-M.; Rigot, M.; Fabbro-Peray, P.; Bauchet, L.; Figarella-Branger, D.; Menei, P.; FGB network. The French Glioblastoma Biobank (FGB): A National Clinicobiological Database. J. Transl. Med. 2019, 17, 133. [Google Scholar] [CrossRef]


| Patients | Number | % | |
|---|---|---|---|
| Patient characteristics | |||
| Age | median (range): 60 (36–81) | ||
| ● ≤60 years | 43 | 51 | |
| ● >60 years | 42 | 49 | |
| Sex | |||
| ● Male | 65 | 76 | |
| ● Female | 20 | 24 | |
| Preoperative KPS | |||
| ● ≤80% | 14 | 16 | |
| ● >80% | 71 | 84 | |
| Tumor location | |||
| Hemisphere | |||
| ● Left | 42 | 49 | |
| ● Right | 43 | 51 | |
| Unilobar | 46 | 54 | |
| ● Frontal | 16 | 19 | |
| ● Temporal | 12 | 14 | |
| ● Parietal | 13 | 15 | |
| ● Occipital | 4 | 5 | |
| ● Limbic | 1 | 1 | |
| Multilobar | 39 | 46 | |
| Extent of surgery | |||
| GTR | 46 | 54 | |
| STR | 26 | 31 | |
| PR | 13 | 15 | |
| Preoperative hematological markers | |||
| RBC | median (range): 4.79 (3.16–5.78) | ||
| ● ≤4.59 × 1012/L | 23 | 27 | |
| ● >4.59 × 1012/L | 62 | 73 | |
| WBC | median (range): 8.66 (4.20–19.25) | ||
| ● ≤6.28 × 109/L | 9 | 11 | |
| ● >6.28 × 109/L | 76 | 89 | |
| Neutrophils | median (range): 6.10 (2.03–16.56) | ||
| ● ≤3.68 × 109/L | 10 | 12 | |
| ● >3.68 × 109/L | 75 | 88 | |
| Lymphocytes | median (range): 1.78 (0.40–5.51) | ||
| ● ≤1.31 × 109/L | 20 | 24 | |
| ● >1.31 × 109/L | 65 | 76 | |
| Monocytes | median (range): 0.65 (0.06–1.22) | ||
| ● ≤0.37 × 109/L | 10 | 12 | |
| ● >0.37 × 109/L | 75 | 88 | |
| Platelets | median (range): 237 (106–522) | ||
| ● ≤236 × 109/L | 41 | 48 | |
| ● >236 × 109/L | 44 | 52 | |
| NLR | median (range): 3.18 (0.85–22.00) | ||
| ● ≤2.42 | 27 | 32 | |
| ● >2.42 | 58 | 68 | |
| dNLR | median (range): 2.30 (0.69–12.29) | ||
| ● ≤1.89 | 32 | 38 | |
| ● >1.89 | 53 | 62 | |
| LMR | median (range): 2.76 (0.83–24.54) | ||
| ● ≤2.06 | 24 | 28 | |
| ● >2.06 | 61 | 72 | |
| PLR | median (range): 137.64 (51.08–645.00) | ||
| ● ≤180.90 | 62 | 73 | |
| ● >180.90 | 23 | 27 | |
| SII | median (range): 772.13 (236.57–5715.87) | ||
| ● ≤502.39 | 23 | 27 | |
| ● >502.39 | 62 | 73 | |
| SIRI | median (range): 1.95 (0.24–19.94) | ||
| ● ≤2.55 | 54 | 64 | |
| ● >2.55 | 31 | 36 | |
| Stupp regimen | |||
| Concurrent radiotherapy + TMZ | 85 | 100 | |
| Adjuvant TMZ duration | |||
| ● ≤6 cycles | 70 | 82 | |
| ● >6 cycles | 15 | 18 | |
| Survival outcomes | |||
| Median PFS: 7.4 months (95% CI: [6.7; 8.7]) | |||
| Median OS: 17.7 months (95% CI: [14.5; 21.6]) | |||
| Univariate Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|
| PFS | OS | |||||||
| Variables | OR | 95% CI | p | Adj p | OR | 95% CI | p | Adj p |
| Age (>60 years) | 1.14 | [0.74; 1.76] | 0.556 | 1.000 | 1.32 | [0.83; 2.09] | 0.236 | 1.000 |
| Sex (female) | 0.87 | [0.53; 1.45] | 0.601 | 1.000 | 0.72 | [0.42; 1.23] | 0.232 | 1.000 |
| KPS (>80%) | 0.61 | [0.34; 1.09] | 0.097 | 1.000 | 0.45 | [0.25; 0.82] | 0.009 * | 0.189 |
| Hemisphere (left) | 0.83 | [0.54; 1.29] | 0.410 | 1.000 | 0.85 | [0.54; 1.34] | 0.482 | 1.000 |
| Lobe (multilobar) | 1.38 | [0.89; 2.15] | 0.149 | 1.000 | 1.73 | [1.08; 2.76] | 0.022 * | 0.462 |
| EOR (GTR) | 1.02 | [0.65; 1.58] | 0.945 | 1.000 | 0.99 | [0.63; 1.57] | 0.971 | 1.000 |
| TMZ (>6 cycles) | 0.13 | [0.06; 0.29] | <0.001 * | <0.001 * | 0.24 | [0.12; 0.49] | <0.001 * | 0.002 * |
| RBC (>4.59 × 1012/L) | 0.58 | [0.36; 0.95] | 0.032 * | 0.672 | 0.44 | [0.26; 0.75] | 0.002 * | 0.042 * |
| WBC (>6.28 × 109/L) | 2.28 | [1.09; 4.78] | 0.029 * | 0.609 | 3.89 | [1.55; 9.77] | 0.004 * | 0.084 |
| Neutrophils (>3.68 × 109/L) | 1.98 | [0.98; 3.98] | 0.056 | 1.000 | 3.80 | [1.52; 9.50] | 0.004 * | 0.084 |
| Lymphocytes (>1.31 × 109/L) | 1.43 | [0.84; 2.43] | 0.190 | 1.000 | 1.95 | [1.09; 3.49] | 0.025 * | 1.000 |
| Monocytes (>0.37 × 109/L) | 1.25 | [0.64; 2.43] | 0.519 | 1.000 | 1.94 | [0.88; 4.26] | 0.099 | 1.000 |
| Platelets (>236 × 109/L) | 1.19 | [0.76; 1.85] | 0.444 | 1.000 | 1.61 | [1.01; 2.57] | 0.046 * | 0.966 |
| NLR (>2.42) | 1.73 | [1.06; 2.82] | 0.027 * | 0.567 | 2.11 | [1.23; 3.61] | 0.007 * | 0.147 |
| dNLR (>1.89) | 2.12 | [1.32; 3.39] | 0.002 * | 0.042 * | 2.21 | [1.32; 3.70] | 0.002 * | 0.042 * |
| LMR (>2.06) | 0.64 | [0.39; 1.06] | 0.082 | 1.000 | 0.67 | [0.41; 1.11] | 0.122 | 1.000 |
| PLR (>180.90) | 0.92 | [0.56; 1.50] | 0.731 | 1.000 | 0.72 | [0.43; 1.20] | 0.208 | 1.000 |
| SII (>502.39) | 1.42 | [0.86; 2.33] | 0.170 | 1.000 | 1.83 | [1.05; 3.21] | 0.034 * | 0.714 |
| SIRI (>2.55) | 1.62 | [1.01; 2.59] | 0.045 * | 0.945 | 2.11 | [1.29; 3.45] | 0.003 * | 0.063 |
| Multivariate Analyses | ||||||
|---|---|---|---|---|---|---|
| PFS | OS | |||||
| Variables | OR | 95% CI | p | OR | 95% CI | p |
| Multivariate analysis including NLR | ||||||
| Sex (female) | 0.86 | [0.50; 1.46] | 0.571 | 0.52 | [0.29; 0.93] | 0.028 * |
| KPS (>80%) | 0.83 | [0.41; 1.66] | 0.592 | |||
| Lobe (multilobar) | 1.28 | [0.75; 2.20] | 0.361 | |||
| TMZ (>6 cycles) | 0.12 | [0.06; 0.27] | <0.001 * | 0.26 | [0.12; 0.54] | <0.001 * |
| RBC (>4.59 × 1012/L) | 0.60 | [0.36; 1.00] | 0.048 * | 0.42 | [0.23; 0.75] | 0.004 * |
| Platelets (>236 × 109/L) | 1.73 | [1.06; 2.83] | 0.030 * | |||
| NLR (>2.42) | 2.02 | [1.18; 3.44] | 0.010 * | 1.88 | [1.06; 3.32] | 0.030 * |
| Multivariate analysis including dNLR | ||||||
| Sex (female) | 0.79 | [0.46; 1.34] | 0.381 | 0.51 | [0.28; 0.91] | 0.023 * |
| KPS (>80%) | 0.86 | [0.43; 1.71] | 0.665 | |||
| Lobe (multilobar) | 1.33 | [0.78; 2.27] | 0.294 | |||
| TMZ (>6 cycles) | 0.13 | [0.06; 0.29] | <0.001 * | 0.28 | [0.13; 0.60] | <0.001 * |
| RBC (>4.59 × 1012/L) | 0.62 | [0.38; 1.02] | 0.062 | 0.42 | [0.23; 0.74] | 0.003 * |
| Platelets (>236 × 109/L) | 1.67 | [1.02; 2.73] | 0.041 * | |||
| dNLR (>1.89) | 2.28 | [1.37; 3.79] | 0.002 * | 1.81 | [1.05; 3.13] | 0.033 * |
| Multivariate analysis including NLR-P-RBC score | ||||||
| Sex (female) | 0.83 | [0.49; 1.40] | 0.481 | 0.53 | [0.30; 0.95] | 0.034 * |
| KPS (>80%) | 0.77 | [0.39; 1.49] | 0.435 | |||
| Lobe (multilobar) | 1.26 | [0.74; 2.13] | 0.397 | |||
| TMZ (>6 cycles) | 0.13 | [0.06; 0.28] | <0.001 * | 0.26 | [0.12; 0.54] | <0.001 * |
| NLR-P-RBC score | 1.51 | [1.12; 2.02] | 0.006 * | 1.95 | [1.42; 2.69] | <0.001 * |
| Multivariate analysis including dNLR-P-RBC score | ||||||
| Sex (female) | 0.79 | [0.47; 1.33] | 0.373 | 0.53 | [0.30; 0.94] | 0.030 * |
| KPS (>80%) | 0.79 | [0.41; 1.53] | 0.480 | |||
| Lobe (multilobar) | 1.30 | [0.76; 2.21] | 0.333 | |||
| TMZ (>6 cycles) | 0.13 | [0.06; 0.29] | <0.001 * | 0.28 | [0.14; 0.60] | <0.001 * |
| dNLR-P-RBC score | 1.55 | [1.17; 2.05] | 0.002 * | 1.90 | [1.39; 2.60] | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clavreul, A.; Lemée, J.-M.; Soulard, G.; Rousseau, A.; Menei, P. A Simple Preoperative Blood Count to Stratify Prognosis in Isocitrate Dehydrogenase-Wildtype Glioblastoma Patients Treated with Radiotherapy plus Concomitant and Adjuvant Temozolomide. Cancers 2021, 13, 5778. https://doi.org/10.3390/cancers13225778
Clavreul A, Lemée J-M, Soulard G, Rousseau A, Menei P. A Simple Preoperative Blood Count to Stratify Prognosis in Isocitrate Dehydrogenase-Wildtype Glioblastoma Patients Treated with Radiotherapy plus Concomitant and Adjuvant Temozolomide. Cancers. 2021; 13(22):5778. https://doi.org/10.3390/cancers13225778
Chicago/Turabian StyleClavreul, Anne, Jean-Michel Lemée, Gwénaëlle Soulard, Audrey Rousseau, and Philippe Menei. 2021. "A Simple Preoperative Blood Count to Stratify Prognosis in Isocitrate Dehydrogenase-Wildtype Glioblastoma Patients Treated with Radiotherapy plus Concomitant and Adjuvant Temozolomide" Cancers 13, no. 22: 5778. https://doi.org/10.3390/cancers13225778