Relationship between Food Allergy and Endotoxin Concentration and the Toleration Status at 2 Years: The Japan Environment and Children’s Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Participants
2.2. Variables
2.3. Measurement of Endotoxin Concentration
2.4. Measurement of Food Allergen-Specific Ig Levels
2.5. Bias and Study Size
2.6. Statistical Analysis
3. Results
3.1. Participants
3.2. Endotoxin Concentrations and House Dust Mite Allergens
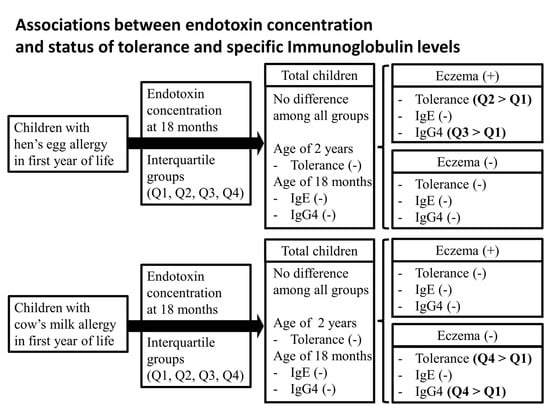
3.3. Endotoxin Concentrations and the Toleration Statuses of HE and CM
3.4. Endotoxin Concentrations and EW- and CM-Specific Ig Levels
3.5. EW- and CM-Specific Ig Levels and Toleration Statuses
3.6. Subgroup Analysis by Eczema in the Toleration Statuses of HE and CM
3.7. Subgroup Analysis by Eczema in EW- and CM-Specific IgE and IgG4 Levels
3.8. Correlation between Endotoxin Concentration and Specific IgE and IgG4 Levels
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Skypala, I.J.; McKenzie, R. Nutritional Issues in Food Allergy. Clin. Rev. Allergy Immunol. 2019, 57, 166–178. [Google Scholar] [CrossRef]
- Golding, M.A.; Batac, A.L.R.; Gunnarsson, N.V.; Ahlstedt, S.; Middelveld, R.; Protudjer, J.L.P. The burden of food allergy on children and teens: A systematic review. Pediatr. Allergy Immunol. 2022, 33, e13743. [Google Scholar] [CrossRef]
- Golding, M.A.; Gunnarsson, N.V.; Middelveld, R.; Ahlstedt, S.; Protudjer, J.L.P. A scoping review of the caregiver burden of pediatric food allergy. Ann. Allergy Asthma. Immunol. 2021, 127, 536–547. [Google Scholar] [CrossRef]
- Sampath, V.; Abrams, E.M.; Adlou, B.; Akdis, C.; Akdis, M.; Brough, H.A.; Chan, S.; Chatchatee, P.; Chinthrajah, R.S.; Cocco, R.R.; et al. Food allergy across the globe. J. Allergy Clin. Immunol. 2021, 148, 1347–1364. [Google Scholar] [CrossRef]
- Yamamoto-Hanada, K.; Pak, K.; Saito-Abe, M.; Yang, L.; Sato, M.; Irahara, M.; Mezawa, H.; Sasaki, H.; Nishizato, M.; Ishitsuka, K.; et al. Allergy and immunology in young children of Japan: The JECS cohort. World Allergy Organ. J. 2020, 13, 100479. [Google Scholar] [CrossRef]
- Tedner, S.G.; Asarnoj, A.; Thulin, H.; Westman, M.; Konradsen, J.R.; Nilsson, C. Food allergy and hypersensitivity reactions in children and adults-A review. J. Intern. Med. 2022, 291, 283–302. [Google Scholar] [CrossRef] [PubMed]
- Cardwell, F.S.; Elliott, S.J.; Chin, R.; St Pierre, Y.; Ben-Shoshan, M.; Chan, E.S.; Gerdts, J.; Harada, L.; Asai, Y.; La Vieille, S.; et al. Economic Burden of Food Allergy in Canada: Estimating Costs and Identifying Determinants. Ann. Allergy Asthma Immunol. 2022, 129, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Savage, J.H.; Matsui, E.C.; Skripak, J.M.; Wood, R.A. The natural history of egg allergy. J. Allergy Clin. Immunol. 2007, 120, 1413–1417. [Google Scholar] [CrossRef]
- Clark, A.; Islam, S.; King, Y.; Deighton, J.; Szun, S.; Anagnostou, K.; Ewan, P. A longitudinal study of resolution of allergy to well-cooked and uncooked egg. Clin. Exp. Allergy 2011, 41, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Høst, A.; Halken, S.; Jacobsen, H.P.; Christensen, A.E.; Herskind, A.M.; Plesner, K. Clinical course of cow’s milk protein allergy/intolerance and atopic diseases in childhood. Pediatr. Allergy Immunol. 2002, 13, 23–28. [Google Scholar] [CrossRef]
- Hansen, M.M.; Nissen, S.P.; Halken, S.; Høst, A. The natural course of cow’s milk allergy and the development of atopic diseases into adulthood. Pediatr. Allergy Immunol. 2021, 32, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Schoemaker, A.A.; Sprikkelman, A.B.; Grimshaw, K.E.; Roberts, G.; Grabenhenrich, L.; Rosenfeld, L.; Siegert, S.; Dubakiene, R.; Rudzeviciene, O.; Reche, M.; et al. Incidence and natural history of challenge-proven cow’s milk allergy in European children-EuroPrevall birth cohort. Allergy 2015, 70, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Xepapadaki, P.; Fiocchi, A.; Grabenhenrich, L.; Roberts, G.; Grimshaw, K.E.; Fiandor, A.; Larco, J.I.; Sigurdardottir, S.; Clausen, M.; Papadopoulos, N.G.; et al. Incidence and natural history of hen’s egg allergy in the first 2 years of life-the EuroPrevall birth cohort study. Allergy 2016, 71, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Schoos, A.M.; Bullens, D.; Chawes, B.L.; Costa, J.; De Vlieger, L.; DunnGalvin, A.; Epstein, M.M.; Garssen, J.; Hilger, C.; Knipping, K.; et al. Immunological Outcomes of Allergen-Specific Immunotherapy in Food Allergy. Front. Immunol. 2020, 11, 568598. [Google Scholar] [CrossRef]
- Kim, E.H.; Burks, A.W. Food allergy immunotherapy: Oral immunotherapy and epicutaneous immunotherapy. Allergy 2020, 75, 1337–1346. [Google Scholar] [CrossRef]
- Perrett, K.P.; Sindher, S.B.; Begin, P.; Shanks, J.; Elizur, A. Advances, Practical Implementation, and Unmet Needs Regarding Oral Immunotherapy for Food Allergy. J. Allergy Clin. Immunol. Pract. 2022, 10, 19–33. [Google Scholar] [CrossRef]
- Bohle, B.; Werfel, T. Treatment Approaches to Food Allergy. Handb. Exp. Pharmacol. 2022, 268, 173–193. [Google Scholar] [CrossRef]
- Celebi Sözener, Z.; Cevhertas, L.; Nadeau, K.; Akdis, M.; Akdis, C.A. Environmental factors in epithelial barrier dysfunction. J. Allergy Clin. Immunol. 2020, 145, 1517–1528. [Google Scholar] [CrossRef]
- Celebi Sozener, Z.; Ozdel Ozturk, B.; Cerci, P.; Turk, M.; Gorgulu Akin, B.; Akdis, M.; Altiner, S.; Ozbey, U.; Ogulur, I.; Mitamura, Y.; et al. Epithelial barrier hypothesis: Effect of the external exposome on the microbiome and epithelial barriers in allergic disease. Allergy 2022, 77, 1418–1449. [Google Scholar] [CrossRef]
- Heinrich, J.; Pitz, M.; Bischof, W.; Krug, N.; Borm, P.J.A. Endotoxin in fine (PM2.5) and coarse (PM2.5–10) particle mass of ambient aerosols. A temporo-spatial analysis. Atmos. Environ. 2003, 37, 3659–3667. [Google Scholar] [CrossRef]
- Thorne, P.S. Environmental endotoxin exposure and asthma. J. Allergy Clin. Immunol. 2021, 148, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Yoda, Y.; Tamura, K.; Shima, M. Airborne endotoxin concentrations in indoor and outdoor particulate matter and their predictors in an urban city. Indoor Air 2017, 27, 955–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasunuma, H.; Yoda, Y.; Tokuda, N.; Taniguchi, N.; Takeshima, Y.; Shima, M. Effects of early-life exposure to dust mite allergen and endotoxin on the development of asthma and wheezing: The Japan Environment and Children’s Study. Clin. Transl. Allergy 2021, 11, e12071. [Google Scholar] [CrossRef] [PubMed]
- Tsuang, A.; Grishin, A.; Grishina, G.; Do, A.N.; Sordillo, J.; Chew, G.L.; Bunyavanich, S. Endotoxin, food allergen sensitization, and food allergy: A complementary epidemiologic and experimental study. Allergy 2020, 75, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Iwai-Shimada, M.; Nakayama, S.F.; Isobe, T.; Michikawa, T.; Yamazaki, S.; Nitta, H.; Takeuchi, A.; Kobayashi, Y.; Tamura, K.; Suda, E.; et al. Questionnaire results on exposure characteristics of pregnant women participating in the Japan Environment and Children Study (JECS). Environ. Health Prev. Med. 2018, 23, 45. [Google Scholar] [CrossRef]
- Sekiyama, M.; Yamazaki, S.; Michikawa, T.; Nakayama, S.F.; Nitta, H.; Taniguchi, Y.; Suda, E.; Isobe, T.; Kobayashi, Y.; Iwai-Shimada, M.; et al. Study Design and Participants’ Profile in the Sub-Cohort Study in the Japan Environment and Children’s Study (JECS). J. Epidemiol. 2022, 32, 228–236. [Google Scholar] [CrossRef]
- Kawamoto, T.; Nitta, H.; Murata, K.; Toda, E.; Tsukamoto, N.; Hasegawa, M.; Yamagata, Z.; Kayama, F.; Kishi, R.; Ohya, Y.; et al. Rationale and study design of the Japan environment and children’s study (JECS). BMC Public Health 2014, 14, 25. [Google Scholar] [CrossRef] [Green Version]
- Michikawa, T.; Nitta, H.; Nakayama, S.F.; Yamazaki, S.; Isobe, T.; Tamura, K.; Suda, E.; Ono, M.; Yonemoto, J.; Iwai-Shimada, M.; et al. Baseline Profile of Participants in the Japan Environment and Children’s Study (JECS). J. Epidemiol. 2018, 28, 99–104. [Google Scholar] [CrossRef] [Green Version]
- Asher, M.I.; Keil, U.; Anderson, H.R.; Beasley, R.; Crane, J.; Martinez, F.; Mitchell, E.A.; Pearce, N.; Sibbald, B.; Stewart, A.W.; et al. International Study of Asthma and Allergies in Childhood (ISAAC): Rationale and methods. Eur. Respir. J. 1995, 8, 483–491. [Google Scholar] [CrossRef] [Green Version]
- Weiland, S.K.; Björkstén, B.; Brunekreef, B.; Cookson, W.O.; von Mutius, E.; Strachan, D.P. Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): Rationale and methods. Eur. Respir. J. 2004, 24, 406–412. [Google Scholar] [CrossRef]
- Ellwood, P.; Asher, M.I.; Beasley, R.; Clayton, T.O.; Stewart, A.W. The international study of asthma and allergies in childhood (ISAAC): Phase three rationale and methods. Int. J. Tuberc. Lung Dis. 2005, 9, 10–16. [Google Scholar] [PubMed]
- Suzuki, K.; Hiyoshi, M.; Tada, H.; Bando, M.; Ichioka, T.; Kamemura, N.; Kido, H. Allergen diagnosis microarray with high-density immobilization capacity using diamond-like carbon-coated chips for profiling allergen-specific IgE and other immunoglobulins. Anal. Chim. Acta 2011, 706, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Irahara, M.; Shinahara, W.; Sugimoto, M.; Ogawa, Y.; Shitsukawa, K.; Kubota, K.; Yang, L.; Ohya, Y.; Saito, H.; Kagami, S.; et al. Trajectories of class-switching-related egg and cow’s milk allergen-specific immunoglobulin isotype formation and its modification by eczema with low- and high-affinity immunoglobulin E during early infancy. Immun. Inflamm. Dis. 2019, 7, 74–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sato, M.; Yamamoto-Hanada, K.; Tada, H.; Irahara, M.; Saito-Abe, M.; Matsumoto, K.; Pak, K.; Kido, H.; Ohya, Y. Diagnostic performance of IgE avidity for hen’s egg allergy in young infants. J. Allergy Clin. Immunol. Pract. 2020, 8, 2417–2420. [Google Scholar] [CrossRef]
- Irahara, M.; Yamamoto-Hanada, K.; Saito-Abe, M.; Sato, M.; Miyaji, Y.; Yang, L.; Mitsubuchi, H.; Oda, M.; Sanefuji, M.; Ohga, S.; et al. Fluctuations of aeroallergen-specific immunoglobulins and children’s allergic profiles: Japan Environment & Children’s Study of a pilot cohort. Allergol. Int. 2022, 73, 335–344. [Google Scholar] [CrossRef]
- Peel, M.C.; Finlayson, B.L.; McMahon, T.A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 2007, 11, 1633–1644. [Google Scholar] [CrossRef] [Green Version]
- Peters, R.L.; Guarnieri, I.; Tang, M.L.K.; Lowe, A.J.; Dharmage, S.C.; Perrett, K.P.; Gurrin, L.C.; Koplin, J.J. The natural history of peanut and egg allergy in children up to age 6 years in the HealthNuts population-based longitudinal study. J. Allergy Clin. Immunol. 2022, 150, 657–665. [Google Scholar] [CrossRef]
- Mendy, A.; Wilkerson, J.; Salo, P.M.; Cohn, R.D.; Zeldin, D.C.; Thorne, P.S. Exposure and Sensitization to Pets Modify Endotoxin Association with Asthma and Wheeze. J. Allergy Clin. Immunol. Pract. 2018, 6, 2006. [Google Scholar] [CrossRef]
- Tulic, M.K.; Hodder, M.; Forsberg, A.; McCarthy, S.; Richman, T.; D’Vaz, N.; van den Biggelaar, A.H.; Thornton, C.A.; Prescott, S.L. Differences in innate immune function between allergic and nonallergic children: New insights into immune ontogeny. J. Allergy Clin. Immunol. 2011, 127, 470–478. [Google Scholar] [CrossRef]
- Wang, N.; McKell, M.; Dang, A.; Yamani, A.; Waggoner, L.; Vanoni, S.; Noah, T.; Wu, D.; Kordowski, A.; Köhl, J.; et al. Lipopolysaccharide suppresses IgE-mast cell-mediated reactions. Clin. Exp. Allergy 2017, 47, 1574–1585. [Google Scholar] [CrossRef]
- Kumar, S.; Adhikari, A. Dose-dependent immunomodulating effects of endotoxin in allergic airway inflammation. Innate Immun. 2017, 23, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, M.; Kamemura, N.; Nagao, M.; Irahara, M.; Kagami, S.; Fujisawa, T.; Kido, H. Differential response in allergen-specific IgE, IgGs, and IgA levels for predicting outcome of oral immunotherapy. Pediatr. Allergy Immunol. 2016, 27, 276–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shamji, M.H.; Kappen, J.H.; Akdis, M.; Jensen-Jarolim, E.; Knol, E.F.; Kleine-Tebbe, J.; Bohle, B.; Chaker, A.M.; Till, S.J.; Valenta, R.; et al. Biomarkers for monitoring clinical efficacy of allergen immunotherapy for allergic rhinoconjunctivitis and allergic asthma: An EAACI Position Paper. Allergy 2017, 72, 1156–1173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shamji, M.H.; Valenta, R.; Jardetzky, T.; Verhasselt, V.; Durham, S.R.; Würtzen, P.A.; van Neerven, R.J.J. The role of allergen-specific IgE, IgG and IgA in allergic disease. Allergy 2021, 76, 3627–3641. [Google Scholar] [CrossRef] [PubMed]
- Suaini, N.H.A.; Wang, Y.; Soriano, V.X.; Martino, D.J.; Allen, K.J.; Ellis, J.A.; Koplin, J.J. Genetic determinants of paediatric food allergy: A systematic review. Allergy 2019, 74, 1631–1648. [Google Scholar] [CrossRef] [Green Version]
- Dimitrov, I.; Doytchinova, I. Associations between Milk and Egg Allergens and the HLA-DRB1/DQ Polymorphism: A Bioinformatics Approach. Int. Arch. Allergy Immunol. 2016, 169, 33–39. [Google Scholar] [CrossRef]
- Poole, A.; Song, Y.; O’Sullivan, M.; Lee, K.H.; Metcalfe, J.; Guo, J.; Brown, H.; Mullins, B.; Loh, R.; Zhang, G.B. Children with nut allergies have impaired gene expression of Toll-like receptors pathway. Pediatr. Allergy Immunol. 2020, 31, 671–677. [Google Scholar] [CrossRef]
- Simpson, A.; John, S.L.; Jury, F.; Niven, R.; Woodcock, A.; Ollier, W.E.; Custovic, A. Endotoxin exposure, CD14, and allergic disease: An interaction between genes and the environment. Am. J. Respir. Crit. Care Med. 2006, 174, 386–392. [Google Scholar] [CrossRef]
- Kitazawa, H.; Yamamoto-Hanada, K.; Saito-Abe, M.; Ayabe, T.; Mezawa, H.; Ishitsuka, K.; Konishi, M.; Nakayama, S.F.; Michikawa, T.; Senju, A.; et al. Egg antigen was more abundant than mite antigen in children’s bedding: Findings of the pilot study of the Japan Environment and Children’s Study (JECS). Allergol. Int. 2019, 68, 391–393. [Google Scholar] [CrossRef]
- Kulis, M.D.; Smeekens, J.M.; Immormino, R.M.; Moran, T.P. The airway as a route of sensitization to peanut: An update to the dual allergen exposure hypothesis. J. Allergy Clin. Immunol. 2021, 148, 689–693. [Google Scholar] [CrossRef]
- Caffarelli, C.; Giannetti, A.; Rossi, A.; Ricci, G. Egg Allergy in Children and Weaning Diet. Nutrients 2022, 14, 1540. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, W.J.; Taylor, S.L.; Phipatanakul, W.; Brough, H.A. Environmental Food Exposure: What Is the Risk of Clinical Reactivity From Cross-Contact and What Is the Risk of Sensitization. J. Allergy Clin. Immunol. Pract. 2018, 6, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Brough, H.A.; Simpson, A.; Makinson, K.; Hankinson, J.; Brown, S.; Douiri, A.; Belgrave, D.C.; Penagos, M.; Stephens, A.C.; McLean, W.H.; et al. Peanut allergy: Effect of environmental peanut exposure in children with filaggrin loss-of-function mutations. J. Allergy Clin. Immunol. 2014, 134, 867–875. [Google Scholar] [CrossRef] [PubMed]







| Hen’s Egg Allergy at 1 y | Cow’s Milk Allergy at 1 y | |||
|---|---|---|---|---|
| All, N # | Intake at 2 y N (%) in the Item | All, N # | Intake at 2 y N (%) in the Item | |
| Sex | 204 | 72 | ||
| Male | 107 | 53 (49.5) | 45 | 24 (53.3) |
| Female | 97 | 54 (55.7) | 27 | 14 (51.9) |
| Mode of delivery | 204 | 72 | ||
| Cesarean section | 43 | 18 (41.9) | 14 | 7 (50.0) |
| Vaginal | 161 | 89 (55.3) | 58 | 31 (53.4) |
| Birth weight | 204 | 72 | ||
| <2500 g | 12 | 9 (75.0) | 2 | 1 (50.0) |
| ≥2500 g | 192 | 98 (51.0) | 70 | 37 (52.9) |
| Sibling | 203 | 72 | ||
| YES | 108 | 54 (50.0) | 56 | 27 (48.2) |
| NO | 95 | 52 (54.7) | 16 | 11 (68.8) |
| Maternal allergy | 204 | 72 | ||
| YES | 105 | 56 (53.3) | 47 | 23 (48.9) |
| NO | 99 | 51 (51.5) | 25 | 15 (60.0) |
| Household Income | 201 | 66 | ||
| <4 million yen | 74 | 46 (62.2) | 21 | 14 (66.7) |
| ≥4 million yen | 127 | 60 (47.2) | 45 | 20 (44.4) |
| Climate of residence | 204 | 72 | ||
| Subarctic | 49 | 30 (61.2) | 21 | 14 (66.7) |
| Temperate | 155 | 77 (49.7) | 51 | 24 (47.1) |
| Indoor pet owner at 6 m | 204 | 72 | ||
| YES | 22 | 15 (68.2) | 3 | 1 (33.3) |
| NO | 182 | 92 (50.5) | 69 | 37 (53.6) |
| Breastfeeding until 1 y | 204 | 72 | ||
| YES | 145 | 69 (47.6) | 54 | 25 (46.3) |
| NO | 59 | 38 (64.4) | 18 | 13 (72.2) |
| Current eczema at 2 y | 202 | 71 | ||
| YES | 70 | 30 (42.9) | 34 | 11 (32.4) |
| NO | 132 | 76 (57.6) | 37 | 27 (73.0) |
| Specific Immunoglobulin | Allergen | Current Eczema | Correlation Coefficient | p-Value |
|---|---|---|---|---|
| Specific IgE | Egg white | Yes | −0.087 | 0.48 |
| No | 0.014 | 0.87 | ||
| Cow’s milk | Yes | −0.11 | 0.54 | |
| No | −0.28 | 0.090 | ||
| Specific IgG4 | Egg white | Yes | 0.24 | 0.048 |
| No | 0.18 | 0.042 | ||
| Cow’s milk | YES | −0.16 | 0.36 | |
| No | 0.35 | 0.033 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Irahara, M.; Yamamoto-Hanada, K.; Sato, M.; Saito-Abe, M.; Miyaji, Y.; Yang, L.; Nishizato, M.; Kumasaka, N.; Mezawa, H.; Ohya, Y.; et al. Relationship between Food Allergy and Endotoxin Concentration and the Toleration Status at 2 Years: The Japan Environment and Children’s Study. Nutrients 2023, 15, 968. https://doi.org/10.3390/nu15040968
Irahara M, Yamamoto-Hanada K, Sato M, Saito-Abe M, Miyaji Y, Yang L, Nishizato M, Kumasaka N, Mezawa H, Ohya Y, et al. Relationship between Food Allergy and Endotoxin Concentration and the Toleration Status at 2 Years: The Japan Environment and Children’s Study. Nutrients. 2023; 15(4):968. https://doi.org/10.3390/nu15040968
Chicago/Turabian StyleIrahara, Makoto, Kiwako Yamamoto-Hanada, Miori Sato, Mayako Saito-Abe, Yumiko Miyaji, Limin Yang, Minaho Nishizato, Natsuhiko Kumasaka, Hidetoshi Mezawa, Yukihiro Ohya, and et al. 2023. "Relationship between Food Allergy and Endotoxin Concentration and the Toleration Status at 2 Years: The Japan Environment and Children’s Study" Nutrients 15, no. 4: 968. https://doi.org/10.3390/nu15040968