Lifestyle Intervention in NAFLD: Long-Term Diabetes Incidence in Subjects Treated by Web- and Group-Based Programs
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Methods
2.3. Sample Size
2.4. Statistical Analysis
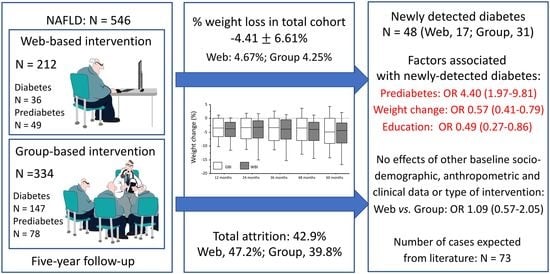
3. Results
3.1. Socio-Demographic and Clinical Data
3.2. Diabetes Prevalence and Incidence
3.3. Weight Loss, Diabetes Incidence and Metabolic Control
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Younossi, Z.M.; Golabi, P.; de Avila, L.; Paik, J.M.; Srishord, M.; Fukui, N.; Qiu, Y.; Burns, L.; Afendy, A.; Nader, F. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J. Hepatol. 2019, 71, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Petroni, M.L.; Brodosi, L.; Bugianesi, E.; Marchesini, G. Management of non-alcoholic fatty liver disease. BMJ 2021, 372, m4747. [Google Scholar] [CrossRef] [PubMed]
- Burgess, E.; Hassmen, P.; Pumpa, K.L. Determinants of adherence to lifestyle intervention in adults with obesity: A systematic review. Clin. Obes. 2017, 7, 123–135. [Google Scholar] [CrossRef]
- Centis, E.; Moscatiello, S.; Bugianesi, E.; Bellentani, S.; Fracanzani, A.L.; Calugi, S.; Petta, S.; Grave, R.D.; Marchesini, G. Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver disease. J. Hepatol. 2013, 58, 771–777. [Google Scholar] [CrossRef]
- Duan, Y.; Shang, B.; Liang, W.; Du, G.; Yang, M.; Rhodes, R.E. Effects of eHealth-based multiple health behavior change interventions on physical activity, healthy diet, and weight in people with noncommunicable diseases: Systematic review and meta-analysis. J. Med. Internet Res. 2021, 23, e23786. [Google Scholar] [CrossRef] [PubMed]
- Lunde, P.; Nilsson, B.B.; Bergland, A.; Kvaerner, K.J.; Bye, A. The effectiveness of smartphone apps for lifestyle improvement in noncommunicable diseases: Systematic review and meta-analyses. J. Med. Internet Res. 2018, 20, e162. [Google Scholar] [CrossRef]
- Hsu, C.H.; Alavi, A.; Dong, M. Editorial: mHealth for non-communicable diseases. Front. Public Health 2022, 10, 918982. [Google Scholar] [CrossRef]
- El Benny, M.; Kabakian-Khasholian, T.; El-Jardali, F.; Bardus, M. Application of the eHealth literacy model in digital health interventions: Scoping review. J. Med. Internet Res. 2021, 23, e23473. [Google Scholar] [CrossRef]
- Kempf, K.; Altpeter, B.; Berger, J.; Reuss, O.; Fuchs, M.; Schneider, M.; Gartner, B.; Niedermeier, K.; Martin, S. Efficacy of the Telemedical Lifestyle intervention Program TeLiPro in Advanced Stages of Type 2 Diabetes: A Randomized Controlled Trial. Diabetes Care 2017, 40, 863–871. [Google Scholar] [CrossRef]
- Mazzotti, A.; Caletti, M.T.; Brodosi, L.; Di Domizio, S.; Forchielli, M.L.; Petta, S.; Bugianesi, E.; Bianchi, G.; Marchesini, G. An internet-based approach for lifestyle changes in patients with NAFLD: Two-year effects on weight loss and surrogate markers. J. Hepatol. 2018, 69, 1155–1163. [Google Scholar] [CrossRef] [Green Version]
- Francque, S.M.; van der Graaff, D.; Kwanten, W.J. Non-alcoholic fatty liver disease and cardiovascular risk: Pathophysiological mechanisms and implications. J. Hepatol. 2016, 65, 425–443. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Petracca, G.; Beatrice, G.; Csermely, A.; Lonardo, A.; Schattenberg, J.M.; Tilg, H.; Byrne, C.D.; Targher, G. Non-alcoholic fatty liver disease and risk of incident chronic kidney disease: An updated meta-analysis. Gut 2022, 71, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Simon, T.G.; Roelstraete, B.; Sharma, R.; Khalili, H.; Hagstrom, H.; Ludvigsson, J.F. Cancer risk in patients with biopsy-confirmed nonalcoholic fatty liver disease: A population-based cohort study. Hepatology 2021, 74, 2410–2423. [Google Scholar] [CrossRef] [PubMed]
- Kanwal, F.; Kramer, J.R.; Mapakshi, S.; Natarajan, Y.; Chayanupatkul, M.; Richardson, P.A.; Li, L.; Desiderio, R.; Thrift, A.P.; Asch, S.M.; et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology 2018, 155, 1828–1837.e2. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.M.; Hicks, S.B.; Mara, K.C.; Larson, J.J.; Therneau, T.M. The risk of incident extrahepatic cancers is higher in non-alcoholic fatty liver disease than obesity—A longitudinal cohort study. J. Hepatol. 2019, 71, 1229–1236. [Google Scholar] [CrossRef]
- Brodosi, L.; Musio, A.; Barbanti, F.A.; Mita, D.; Marchesini, G.; Petroni, M.L. Diabetes and NAFLD: A high-risk cohort with definite therapeutic potential. Hepatoma Res. 2020, 6, 82. [Google Scholar] [CrossRef]
- Vilar-Gomez, E.; Martinez-Perez, Y.; Calzadilla-Bertot, L.; Torres-Gonzalez, A.; Gra-Oramas, B.; Gonzalez-Fabian, L.; Friedman, S.L.; Diago, M.; Romero-Gomez, M. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology 2015, 149, 367–378.e5. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee; Draznin, B.; Aroda, V.R.; Bakris, G.; Benson, G.; Brown, F.M.; Freeman, R.; Green, J.; Huang, E.; Isaacs, D.; et al. 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes-2022. Diabetes Care 2022, 45, S60–S82. [Google Scholar] [CrossRef]
- Guess, N.D. Dietary interventions for the prevention of type 2 diabetes in high-risk groups: Current state of evidence and future research needs. Nutrients 2018, 10, 1245. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing, 2nd ed; The Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Rossini, R.; Moscatiello, S.; Tarrini, G.; Di Domizio, S.; Soverini, V.; Romano, A.; Mazzotti, A.; Grave, R.D.; Marchesini, G. Effects of cognitive-behavioral treatment for weight loss in family members. J. Am. Diet. Assoc. 2011, 111, 1712–1719. [Google Scholar] [CrossRef]
- Melchionda, N.; Forlani, G.; La Rovere, L.; Argnani, P.; Trevisani, F.; Zocchi, D.; Savorani, G.; Covezzoli, A.; De Rosa, M.; Marchesini, G. Disease management of the metabolic syndrome in a community: Study design and process analysis on baseline data. Metab. Syndr. Relat. Disord. 2006, 4, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- The Diabetes Prevention Program Research Group. The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care 1999, 22, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Tuomilehto, J.; Lindstrom, J.; Eriksson, J.G.; Valle, T.T.; Hamalainen, H.; Ilanne-Parikka, P.; Keinanen-Kiukaanniemi, S.; Laakso, M.; Louheranta, A.; Rastas, M.; et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 2001, 344, 1343–1350. [Google Scholar] [CrossRef]
- Marchesini, G.; Bugianesi, E.; Forlani, G.; Cerrelli, F.; Lenzi, M.; Manini, R.; Natale, S.; Vanni, E.; Villanova, N.; Melchionda, N.; et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003, 37, 917–923. [Google Scholar] [CrossRef]
- Marchesini, G.; Petta, S.; Grave, R.D. Diet, weight loss, and liver health in nonalcoholic fatty liver disease: Pathophysiology, evidence, and practice. Hepatology 2016, 63, 2032–2043. [Google Scholar] [CrossRef]
- Goessling, W.; Massaro, J.M.; Vasan, R.S.; D’Agostino, R.B., Sr.; Ellison, R.C.; Fox, C.S. Aminotransferase levels and 20-year risk of metabolic syndrome, diabetes, and cardiovascular disease. Gastroenterology 2008, 135, 1935–1944. [Google Scholar] [CrossRef]
- Nguyen, Q.M.; Srinivasan, S.R.; Xu, J.H.; Chen, W.; Hassig, S.; Rice, J.; Berenson, G.S. Elevated liver function enzymes are related to the development of prediabetes and type 2 diabetes in younger adults: The Bogalusa Heart Study. Diabetes Care 2011, 34, 2603–2607. [Google Scholar] [CrossRef]
- Fraser, A.; Harris, R.; Sattar, N.; Ebrahim, S.; Smith, G.D.; Lawlor, D.A. Alanine aminotransferase, gamma-glutamyltransferase, and incident diabetes: The British Women′s Heart and Health Study and meta-analysis. Diabetes Care 2009, 32, 741–750. [Google Scholar] [CrossRef] [Green Version]
- Targher, G.; Byrne, C.D. Clinical Review: Nonalcoholic fatty liver disease: A novel cardiometabolic risk factor for type 2 diabetes and its complications. J. Clin. Endocrinol. Metab. 2013, 98, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Sung, K.C.; Wild, S.H.; Byrne, C.D. Resolution of fatty liver and risk of incident diabetes. J. Clin. Endocrinol. Metab. 2013, 98, 3637–3643. [Google Scholar] [CrossRef] [PubMed]
- Ekstedt, M.; Franzen, L.E.; Mathiesen, U.L.; Thorelius, L.; Holmqvist, M.; Bodemar, G.; Kechagias, S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006, 44, 865–873. [Google Scholar] [CrossRef]
- Li, G.; Hu, Y.; Yang, W.; Jiang, Y.; Wang, J.; Xiao, J.; Hu, Z.; Pan, X.; Howard, B.V.; Bennett, P.H. Effects of insulin resistance and insulin secretion on the efficacy of interventions to retard development of type 2 diabetes mellitus: The DA Qing IGT and Diabetes Study. Diabetes Res. Clin. Pract. 2002, 58, 193–200. [Google Scholar] [CrossRef]
- Schmiedel, K.; Mayr, A.; Fiessler, C.; Schlager, H.; Friedland, K. Effects of the lifestyle intervention program GLICEMIA in people at risk for type 2 diabetes: A cluster-randomized controlled trial. Diabetes Care 2015, 38, 937–939. [Google Scholar] [CrossRef]
- Seiglie, J.A.; Marcus, M.E.; Ebert, C.; Prodromidis, N.; Geldsetzer, P.; Theilmann, M.; Agoudavi, K.; Andall-Brereton, G.; Aryal, K.K.; Bicaba, B.W.; et al. Diabetes prevalence and its relationship with education, wealth, and BMI in 29 low- and mddle-income Countries. Diabetes Care 2020, 43, 767–775. [Google Scholar] [CrossRef]
- Ackermann, R.T.; Finch, E.A.; Brizendine, E.; Zhou, H.; Marrero, D.G. Translating the Diabetes Prevention Program into the community: The DEPLOY Pilot Study. Am. J. Prev. Med. 2008, 35, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.K.; Kriska, A.M.; Venditti, E.M.; Miller, R.G.; Brooks, M.M.; Burke, L.E.; Siminerio, L.M.; Solano, F.X.; Orchard, T.J. Translating the Diabetes Prevention Program: A comprehensive model for prevention training and program delivery. Am. J. Prev. Med. 2009, 37, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Laatikainen, T.; Dunbar, J.A.; Chapman, A.; Kilkkinen, A.; Vartiainen, E.; Heistaro, S.; Philpot, B.; Absetz, P.; Bunker, S.; O’Neil, A.; et al. Prevention of type 2 diabetes by lifestyle intervention in an Australian primary health care setting: Greater Green Triangle (GGT) Diabetes Prevention Project. BMC Public Health 2007, 7, 249. [Google Scholar] [CrossRef]
- Mayer-Davis, E.J.; D’Antonio, A.M.; Smith, S.M.; Kirkner, G.; Martin, S.L.; Parra-Medina, D.; Schultz, R. Pounds off with empowerment (POWER): A clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities. Am. J. Public Health 2004, 94, 1736–1742. [Google Scholar] [CrossRef]
- McBride, P.E.; Einerson, J.A.; Grant, H.; Sargent, C.; Underbakke, G.; Vitcenda, M.; Zeller, L.; Stein, J.H. Putting the Diabetes Prevention Program into practice: A program for weight loss and cardiovascular risk reduction for patients with metabolic syndrome or type 2 diabetes mellitus. J. Nutr. Health Aging 2008, 12, 745s–749s. [Google Scholar] [CrossRef] [PubMed]
- Ratner, R.E.; Christophi, C.A.; Metzger, B.E.; Dabelea, D.; Bennett, P.H.; Pi-Sunyer, X.; Fowler, S.; Kahn, S.E.; Diabetes Prevention Program Research Group. Prevention of diabetes in women with a history of gestational diabetes: Effects of metformin and lifestyle interventions. J. Clin. Endocrinol. Metab. 2008, 93, 4774–4779. [Google Scholar] [CrossRef]
- McTigue, K.M.; Conroy, M.B.; Hess, R.; Bryce, C.L.; Fiorillo, A.B.; Fischer, G.S.; Milas, N.C.; Simkin-Silverman, L.R. Using the internet to translate an evidence-based lifestyle intervention into practice. Telemed. e-Health 2009, 15, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Moscatiello, S.; Di Luzio, R.; Bugianesi, E.; Suppini, A.; Hickman, I.; Di Domizio, S.; Dalle Grave, R.; Marchesini, G. Cognitive-behavioral treatment of non-alcoholic fatty liver disease: A propensity score-adjusted observational study. Obesity 2011, 19, 763–770. [Google Scholar] [CrossRef]
- Wantland, D.J.; Portillo, C.J.; Holzemer, W.L.; Slaughter, R.; McGhee, E.M. The effectiveness of Web-based vs. non-Web-based interventions: A meta-analysis of behavioral change outcomes. J. Med. Internet Res. 2004, 6, e40. [Google Scholar] [CrossRef]
- Adams, L.A.; Anstee, Q.M.; Tilg, H.; Targher, G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut 2017, 66, 1138–1153. [Google Scholar] [CrossRef] [PubMed]
- Grave, R.D.; Calugi, S.; Compare, A.; El Ghoch, M.; Petroni, M.L.; Tomasi, F.; Mazzali, G.; Marchesini, G. Weight loss expectations and attrition in treatment-seeking obese women. Obes. Facts 2015, 8, 311–318. [Google Scholar] [CrossRef]
- Grave, R.D.; Calugi, S.; Marchesini, G. The influence of cognitive factors in the treatment of obesity: Lessons from the QUOVADIS study. Behav. Res. Ther. 2014, 63, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Grave, R.D.; Melchionda, N.; Calugi, S.; Centis, E.; Tufano, A.; Fatati, G.; Fusco, M.A.; Marchesini, G. Continuous care in the treatment of obesity: An observational multicentre study. J. Intern. Med. 2005, 258, 265–273. [Google Scholar] [CrossRef]
- Wadden, T.A.; Volger, S.; Sarwer, D.B.; Vetter, M.L.; Tsai, A.G.; Berkowitz, R.I.; Kumanyika, S.; Schmitz, K.H.; Diewald, L.K.; Barg, R.; et al. A two-year randomized trial of obesity treatment in primary care practice. N. Engl. J. Med. 2011, 365, 1969–1979. [Google Scholar] [CrossRef] [Green Version]
- Tsai, A.G.; Wadden, T.A. Treatment of obesity in primary care practice in the United States: A systematic review. J. Gen. Intern. Med. 2009, 24, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Akhlaghi, M.; Ghasemi-Nasab, M.; Riasatian, M. Mediterranean diet for patients with non-alcoholic fatty liver disease, a systematic review and meta-analysis of observational and clinical investigations. J. Diabetes Metab. Disord. 2020, 19, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvado, J.; Covas, M.I.; Corella, D.; Aros, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef]
- Prentice, R.L.; Aragaki, A.K.; Van Horn, L.; Thomson, C.A.; Tinker, L.F.; Manson, J.E.; Mossavar-Rahmani, Y.; Huang, Y.; Zheng, C.; Beresford, S.A.A.; et al. Mortality associated with Healthy Eating Index components and an empirical-scores Healthy Eating Index in a cohort of postmenopausal women. J. Nutr. 2022, 152, 2493–2504. [Google Scholar] [CrossRef]
- Ramsden, C.E.; Zamora, D.; Majchrzak-Hong, S.; Faurot, K.R.; Broste, S.K.; Frantz, R.P.; Davis, J.M.; Ringel, A.; Suchindran, C.M.; Hibbeln, J.R. Re-evaluation of the traditional diet-heart hypothesis: Analysis of recovered data from Minnesota Coronary Experiment (1968–73). BMJ 2016, 353, i1246. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Salas-Salvado, J.; Estruch, R.; Corella, D.; Fito, M.; Ros, E.; PREDIMED Investigators. Benefits of the Mediterranean diet: Insights from the PREDIMED Study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Gregg, E.W.; Jakicic, J.M.; Blackburn, G.; Bloomquist, P.; Bray, G.A.; Clark, J.M.; Coday, M.; Curtis, J.M.; Egan, C.; Evans, M.; et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: A post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016, 4, 913–921. [Google Scholar] [CrossRef] [Green Version]



| Total (n = 546) | Web-Treated (n = 212) | Group-Treated (n = 334) | p-Value ° | |
|---|---|---|---|---|
| Sex (Males, %) | 53.8 (49.6–57.9) | 65.1 (58.2–71.0) | 46.7 (41.3–51.9) | <0.001 |
| Age (years) | 50.6 ± 11.8 | 46.0 ± 11.9 | 53.5 ± 10.8 | <0.001 |
| Weight (Kg) | 95.0 ± 18.3 | 100.2 ± 20.3 | 91.6 ± 16.0 | <0.001 |
| Height (cm) | 167.7 ± 10.9 | 171.2 ± 10.3 | 165.5 ± 10.7 | <0.001 |
| BMI (kg/m2) | 33.8 ± 6.0 | 34.1 ± 6.0 | 33.5 ± 6.0 | 0.254 |
| BMI class | 0.291 | |||
| Overweight (%) | 27.7 (24.0–31.5) | 29.2 (27.0–37.9) | 26.6 (23.8–32.1) | |
| Obesity (%) | 72.3 (68.4–75.8) | 70.8 (64.1–76.2) | 73.4 (68.2–77.7) | |
| Waist circumference (cm) | 106.5 ± 12.0 | 107.8 ± 13.7 | 105.6 ± 10.8 | 0.037 |
| High blood pressure (%) | 44.3 (40.1–48.4) | 34.4 (28.1–40.8) | 50.6 (45.1–55.8) | <0.001 |
| Diabetes (%) | 33.5 (29.6–37.5) | 17.0 (12.3–22.4) | 44.0 (38.6–49.2) | <0.001 |
| Prediabetes (IFG/IGT, %) ^ | 23.3 (19.8–26.9) | 23.1 (17.7–29.0) | 23.4 (19.0–28.0) | 0.917 |
| Lifestyle habits | ||||
| Smoking (%) | 0.914 | |||
| Non-smoker | 70.3 (64.8–75.0) | 70.2 (63.4–75.9) | 70.4 (60.2–78.1) | |
| Active | 12.2 (8.8–16.2) | 12.7 (8.6–17.7) | 11.2 (6.0–18.4) | |
| Previous | 17.5 13.5–22.0) | 17.1 (12.3–22.6) | 18.4 (11.5–26.6) | |
| Alcohol intake (%) | 0.314 | |||
| Abstinent | 94.2 (90.9–96.2) | 98.0 (92.2–99.2) | 92.5 (87.9–95.1) | |
| Within safe limits * | 5.8 (3.6–8.7) | 2.0 (0.4–6.3) | 7.5 (4.5–11.6) | |
| Calorie intake (kcal/day) | 1917 ± 350 | 1925 ± 371 | 1910 ± 333 | 0.753 |
| Physical activity (MET/h/week) | 16.8 ± 14.2 | 18.5 ± 14.2 | 16.0 ± 14.1 | <0.001 |
| Education (%) | <0.001 | |||
| Primary | 2.0 (1.1–3.5) | 0.9 (0.2–3.0) | 2.7 (1.3–4.8) | |
| Secondary | 12.8 (10.2–15.8) | 6.1 (3.4–9.9) | 17.1 (13.3–21.3) | |
| Vocational | 47.8 (43.6–51.9) | 49.1 (42.2–55.5) | 47.0 (41.6–52.2) | |
| Degree | 37.4 (33.3–41.4) | 43.9 (37.1–50.4) | 33.2 (28.3–38.3) | |
| Employment status (%) | <0.001 | |||
| Student | 2.2 (1.2–3.7) | 4.3 (2.1–7.6) | 0.9 (0.2–2.4) | |
| Housewife/Unemployed | 7.5 (5.5–9.9) | 2.8 (1.2–5.7) | 10.5 (7.5–14.1) | |
| Employed | 61.1 (56.9–65.0) | 64.0 (57.1–69.9) | 59.3 (53.8–64.3) | |
| Self-employee | 17.2 (14.2–20.5) | 26.1 (20.4–32.1) | 11.7 (8.5–15.4) | |
| Retired | 11.9 (9.4–14.8) | 2.8 (1.2–5.7) | 17.7 (13.8–22.0) | |
| Biochemistry | ||||
| Fasting glucose (mg/dL) | 113.0 ± 34.1 | 101.3 ± 25.6 | 120.3 ± 36.8 | <0.001 |
| Fasting insulin (mU/L) | 20.8 ± 15.2 | 21.4 ± 15.9 | 20.4 ± 14.6 | 0.487 |
| HOMA-R (%) | 5.42 ± 3.76 | 5.31 ± 4.26 | 5.89 ± 3.37 | 0.614 |
| Glycosylated hemoglobin (%) | 6.52 ± 1.43 | 6.07 ± 1.34 | 6.74 ± 1.42 | <0.001 |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| Independent Variable | Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value |
| Female sex | 0.62 | 0.32–1.17 | 0.139 | |||
| Education | 0.58 | 0.39–0.86 | 0.007 | 0.49 | 0.27–0.86 | 0.014 |
| Age (10 years) | 1.32 | 1.01–1.74 | 0.044 | 1.12 | 0.78–1.59 | 0.547 |
| Prediabetes (IFG/IGT) | 3.75 | 1.99–7.04 | <0.001 | 4.40 | 1.97–9.81 | <0.001 |
| Body mass index (5 kg/m2) | 0.99 | 0.78–1.26 | 0.938 | |||
| Calorie intake (100 kcal/day) | 1.01 | 0.88–1.15 | 0.921 | |||
| Physical activity (MET/hour/wk) | 0.88 | 0.34–3.16 | 0.614 | |||
| Smoking | ||||||
| Non-smoker | Reference | |||||
| Active smoker | 1.07 | 0.28–4.01 | 0.925 | |||
| Previous smoker | 2.00 | 0.77–5.16 | 0.157 | |||
| Alcohol intake | ||||||
| Abstinent | Reference | |||||
| Drinking 14–21 Units/wk | 4.98 | 1.07–23.24 | 0.041 | 1.75 | 0.25–12.15 | 0.569 |
| Job status | ||||||
| Housewife/Unemployed | Reference | ------------ | ------- | |||
| Student | NA | NA | ------- | |||
| Employed | 1.14 | 0.32–4.06 | 0.839 | |||
| Self-employee | 1.55 | 0.39–6.11 | 0.530 | |||
| Retired | 0.80 | 0.18–3.48 | 0.766 | |||
| Length of follow-up (months) | 1.01 | 0.99–1.03 | 0.489 | |||
| Educational intervention | ||||||
| Group-based | Reference | ------------ | ------- | |||
| Web-based | 0.61 | 0.31–1.22 | 0.613 | |||
| Weight change (5%) | 0.59 | 0.45–0.77 | <0.001 | 0.57 | 0.41–0.79 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petroni, M.L.; Brodosi, L.; Armandi, A.; Marchignoli, F.; Bugianesi, E.; Marchesini, G. Lifestyle Intervention in NAFLD: Long-Term Diabetes Incidence in Subjects Treated by Web- and Group-Based Programs. Nutrients 2023, 15, 792. https://doi.org/10.3390/nu15030792
Petroni ML, Brodosi L, Armandi A, Marchignoli F, Bugianesi E, Marchesini G. Lifestyle Intervention in NAFLD: Long-Term Diabetes Incidence in Subjects Treated by Web- and Group-Based Programs. Nutrients. 2023; 15(3):792. https://doi.org/10.3390/nu15030792
Chicago/Turabian StylePetroni, Maria Letizia, Lucia Brodosi, Angelo Armandi, Francesca Marchignoli, Elisabetta Bugianesi, and Giulio Marchesini. 2023. "Lifestyle Intervention in NAFLD: Long-Term Diabetes Incidence in Subjects Treated by Web- and Group-Based Programs" Nutrients 15, no. 3: 792. https://doi.org/10.3390/nu15030792