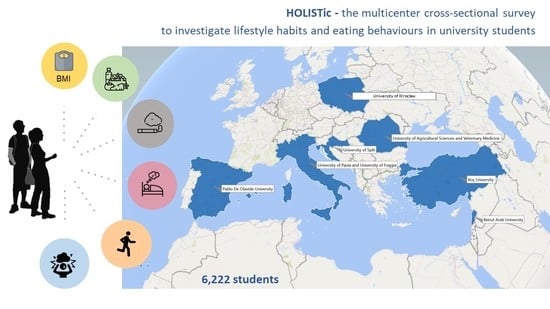
How Healthy Are Health-Related Behaviors in University Students: The HOLISTic Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
- (i)
- General information
- (ii)
- Dietary habits
- (iii)
- Lifestyle and nutrition knowledge
- (iv)
- Orthorexic eating behavior
- (v)
- Physical activity
- (vi)
- Sleeping habits and screen-time
- (vii)
- Perceived level of stress
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Study Registration
References
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef] [Green Version]
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [Green Version]
- The Lancet. Join the Lancet 2020 Campaign on child and adolescent health. Lancet 2020, 395, 89. [Google Scholar] [CrossRef]
- Azzopardi, P.S.; Hearps, S.J.C.; Francis, K.L.; Kennedy, E.C.; Mokdad, A.H.; Kassebaum, N.J.; Lim, S.; Irvine, C.M.S.; Vos, T.; Brown, A.D.; et al. Progress in adolescent health and wellbeing: Tracking 12 headline indicators for 195 countries and territories, 1990–2016. Lancet 2019, 393, 1101–1118. [Google Scholar] [CrossRef] [Green Version]
- Woolf, S.H.; Schoomaker, H. Life Expectancy and Mortality Rates in the United States, 1959–2017. JAMA 2019, 322, 1996–2016. [Google Scholar] [CrossRef]
- Sinha, R. Role of addiction and stress neurobiology on food intake and obesity. Biol. Psychol. 2018, 131, 5–13. [Google Scholar] [CrossRef]
- Allegri, C.; Turconi, G.; Cena, H. Dietary attitudes and diseases of comfort. Eat. Weight Disord. 2011, 16, e226–e235. [Google Scholar] [CrossRef] [PubMed]
- De Vriendt, T.; Clays, E.; Huybrechts, I.; De Bourdeaudhuij, I.; Moreno, L.A.; Patterson, E.; Molnár, D.; Mesana, M.I.; Beghin, L.; Widhalm, K.; et al. European adolescents’ level of perceived stress is inversely related to their diet quality: The Healthy Lifestyle in Europe by Nutrition in Adolescence study. Br. J. Nutr. 2012, 108, 371–380. [Google Scholar] [CrossRef]
- Costa, G. The 24-h society between myth and reality. J. Hum. Ergol. 2001, 30, 15–20. [Google Scholar]
- Crawford, R. Healthism and the medicalization of everyday life. Int. J. Health Serv. Plan. Adm. Eval. 1980, 10, 365–388. [Google Scholar] [CrossRef]
- Håman, L.; Barker-Ruchti, N.; Patriksson, G.; Lindgren, E.C. Orthorexia nervosa: An integrative literature review of a lifestyle syndrome. Int. J. Qual. Stud. Health Well-Being 2015, 10, 26799. [Google Scholar] [CrossRef]
- Cena, H.; Barthels, F.; Cuzzolaro, M.; Bratman, S.; Brytek-Matera, A.; Dunn, T.; Varga, M.; Missbach, B.; Donini, L.M. Definition and diagnostic criteria for orthorexia nervosa: A narrative review of the literature. Eat. Weight Disord. 2019, 24, 209–246. [Google Scholar] [CrossRef] [PubMed]
- Crowley, J.; Ball, L.; Hiddink, G.J. Nutrition in medical education: A systematic review. Lancet Planet. Health 2019, 3, e379–e389. [Google Scholar] [CrossRef]
- Donini, L.M.; Leonardi, F.; Rondanelli, M.; Banderali, G.; Battino, M.; Bertoli, E.; Bordoni, A.; Brighenti, F.; Caccialanza, R.; Muscaritoli, M.; et al. The Domains of Human Nutrition: The Importance of Nutrition Education in Academia and Medical Schools. Front. Nutr. 2017, 4, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiler, R.; Chew, S.; Coombs, N.; Hamer, M.; Stamatakis, E. Physical activity education in the undergraduate curricula of all UK medical schools. Are tomorrow’s doctors equipped to follow clinical guidelines? Br. J. Sports Med. 2012, 46, 1024–1026. [Google Scholar] [CrossRef]
- Hill, M.R.; Goicochea, S.; Merlo, L.J. In their own words: Stressors facing medical students in the millennial generation. Med. Educ. Online 2018, 23, 1530558. [Google Scholar] [CrossRef] [Green Version]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef] [Green Version]
- Maffoni, S.I.; Kalmpourtzidou, A.; Cena, H. The potential role of nutrition in mitigating the psychological impact of COVID-19 in healthcare workers. NFS J. 2021, 22, 6–8. [Google Scholar] [CrossRef]
- WHO-Process of Translation and Adaptation of Instruments. Available online: https://www.who.int/substance_abuse/research_tools/translation/en/ (accessed on 2 April 2018).
- Monteagudo, C.; Mariscal-Arcas, M.; Rivas, A.; Lorenzo-Tovar, M.L.; Tur, J.A.; Olea-Serrano, F. Proposal of a Mediterranean Diet Serving Score. PLoS ONE 2015, 10, e0128594. [Google Scholar] [CrossRef] [Green Version]
- Gleaves, D.H.; Graham, E.C.; Ambwani, S. Measuring ‘Orthorexia’: Development of the Eating Habits Questionnaire. Int. J. Educ. Psychol. Assess. 2013, 12, 1–18. [Google Scholar]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat. Weight Disord. 2004, 9, 151–157. [Google Scholar] [CrossRef]
- Haddad, C.; Hallit, R.; Akel, M.; Honein, K.; Akiki, M.; Kheir, N.; Obeid, S.; Hallit, S. Validation of the Arabic version of the ORTO-15 questionnaire in a sample of the Lebanese population. Eat. Weight Disord. 2020, 25, 951–960. [Google Scholar] [CrossRef]
- Parra-Fernandez, M.L.; Rodríguez-Cano, T.; Perez-Haro, M.J.; Onieva-Zafra, M.D.; Fernandez-Martinez, E.; Notario-Pacheco, B. Structural validation of ORTO-11-ES for the diagnosis of orthorexia nervosa, Spanish version. Eat. Weight Disord. 2018, 23, 745–752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brytek-Matera, A.; Krupa, M.; Poggiogalle, E.; Donini, L.M. Adaptation of the ORTHO-15 test to Polish women and men. Eat. Weight Disord. 2014, 19, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Oja, P.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Physical Activity Questionnaire (IPAQ). Available online: https://sites.google.com/site/theipaq/questionnaire_links (accessed on 2 April 2018).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 386–396. [Google Scholar] [CrossRef]
- Remor, E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span. J. Psychol. 2006, 9, 86–93. [Google Scholar] [CrossRef] [Green Version]
- Drosopoulou, G.; Sergentanis, T.N.; Mastorako, G.; Vlachopapadopoulou, E.; Michalacos, S.; Tzavara, C.; Bacopoulou, F.; Psaltopoulou, T.; Tsitsika, A. Psychosocial health of adolescents in relation to underweight, overweight/obese status: The EU NET ADB survey. Eur. J. Public Health 2020, ckaa189. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, M. Adolescent smoking: The relationship between cigarette consumption and BMI. Addict. Behav. Rep. 2018, 9, 100153. [Google Scholar] [CrossRef]
- Cena, H.; Fonte, M.L.; Turconi, G. Relationship between smoking and metabolic syndrome. Nutr. Rev. 2011, 69, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Cena, H.; Tesone, A.; Niniano, R.; Cerveri, I.; Roggi, C.; Turconi, G. Prevalence rate of Metabolic Syndrome in a group of light and heavy smokers. Diabetol. Metab. Syndr. 2013, 5, 28. [Google Scholar] [CrossRef] [Green Version]
- Fonte, M.L.; Casali, M.P.; Roggi, C.; Turconi, G.; Cena, H. Does Physical Activity and Sport Practice Lead to a Healthier Lifestyle and Eating Habits in Male Adolescents? J. Nutr. Health Sci. 2014, 1, 1–8. [Google Scholar]
- Hemmingsson, E.; Ekelund, U. Is the association between physical activity and body mass index obesity dependent? Int. J. Obes. 2007, 31, 663–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Li, G.; Liu, L.; Wu, H. Correlations between mobile phone addiction and anxiety, depression, impulsivity, and poor sleep quality among college students: A systematic review and meta-analysis. J. Behav. Addict. 2020, 9, 551–571. [Google Scholar] [CrossRef] [PubMed]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index. PLoS Med. 2004, 1, e62. [Google Scholar] [CrossRef]
- Papaconstantinou, E.; Quick, V.; Vogel, E.; Coffey, S.; Miller, A.; Zitzelsberger, H. Exploring Relationships of Sleep Duration with Eating and Physical Activity Behaviors among Canadian University Students. Clocks Sleep 2020, 2, 194–207. [Google Scholar] [CrossRef]
- St-Onge, M.P.; McReynolds, A.; Trivedi, Z.B.; Roberts, A.L.; Sy, M.; Hirsch, J. Sleep restriction leads to increased activation of brain regions sensitive to food stimuli. Am. J. Clin. Nutr. 2012, 95, 818–824. [Google Scholar] [CrossRef] [Green Version]
- Fiore, M.; Ledda, C.; Rapisarda, V.; Sentina, E.; Mauceri, C.; D’Agati, P.; Conti, G.O.; Serra-Majem, L.; Ferrante, M. Medical school fails to improve Mediterranean diet adherence among medical students. Eur. J. Public Health 2015, 25, 1019–1023. [Google Scholar] [CrossRef] [Green Version]
- Navarro-González, I.; López-Nicolás, R.; Rodríguez-Tadeo, A.; Ros-Berruezo, G.; Martínez-Marín, M.; Doménech-Asensi, G. Adherence to the Mediterranean diet by nursing students of Murcia (Spain). Nutr. Hosp. 2014, 30, 165–172. [Google Scholar]
- Baydemir, C.; Ozgur, E.G.; Balci, S. Evaluation of adherence to Mediterranean diet in medical students at Kocaeli University, Turkey. J. Int. Med. Res. 2018, 46, 1585–1594. [Google Scholar] [CrossRef]
- La Fauci, V.; Alessi, V.; Assefa, D.Z.; Giudice, D.L.; Calimeri, S.; Ceccio, C.; Antonuccio, G.M.; Genovese, C.; Squeri, R. Mediterranean diet: Knowledge and adherence in Italian young people. Clin. Ter. 2020, 171, e437–e443. [Google Scholar]
- Naja, F.; Hwalla, N.; Hachem, F.; Abbas, N.; Chokor, F.A.Z.; Kharroubi, S.; Chamieh, M.-C.; Jomaa, L.; Nasreddine, L. Erosion of the Mediterranean diet among adolescents: Evidence from an Eastern Mediterranean Country. Br. J. Nutr. 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Naja, F.; Itani, L.; Kharroubi, S.; El Harake, M.D.; Hwalla, N.; Jomaa, L. Food insecurity is associated with lower adherence to the Mediterranean dietary pattern among Lebanese adolescents: A cross-sectional national study. Eur. J. Nutr. 2020, 59, 3281–3292. [Google Scholar] [CrossRef]
- Gramaglia, C.; Gambaro, E.; Delicato, C.; Marchetti, M.; Sarchiapone, M.; Ferrante, D.; Roncero, M.; Perpiñá, C.; Brytek-Matera, A.; Wojtyna, E.; et al. Orthorexia nervosa, eating patterns and personality traits: A cross-cultural comparison of Italian, Polish and Spanish university students. BMC Psychiatry 2019, 19, 235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalra, S.; Kapoor, N.; Jacob, J. Orthorexia nervosa. J. Pak. Med. Assoc. 2020, 70, 1282–1284. [Google Scholar] [PubMed]
- Strahler, J.; Hermann, A.; Walter, B.; Stark, R. Orthorexia nervosa: A behavioral complex or a psychological condition? J. Behav. Addict. 2018, 7, 1143–1156. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A. The Polish version of the Düsseldorf Orthorexia Scale (PL-DOS) and its comparison with the English version of the DOS (E-DOS). Eat. Weight Disord. 2020. [Google Scholar] [CrossRef]
- Poobalan, A.S.; Aucott, L.S.; Clarke, A.; Smith, W.C.S. Diet behaviour among young people in transition to adulthood (18–25 years old): A mixed method study. Health Psychol. Behav. Med. 2014, 2, 909–928. [Google Scholar] [CrossRef] [PubMed]
- Shadid, A.; Shadid, A.M.; Shadid, A.; Almutairi, F.E.; Almotairi, K.E.; Aldarwish, T.; Alzamil, O.; Alkholaiwi, F.; Khan, S.U.D. Stress, Burnout, and Associated Risk Factors in Medical Students. Cureus 2020, 12, e6633. [Google Scholar] [CrossRef] [Green Version]
- Ioannidis, J.P.A. Neglecting Major Health Problems and Broadcasting Minor, Uncertain Issues in Lifestyle Science. JAMA 2019, 322, 2069–2070. [Google Scholar] [CrossRef] [PubMed]
- Trilk, J.; Nelson, L.; Briggs, A.; Muscato, D. Including Lifestyle Medicine in Medical Education: Rationale for American College of Preventive Medicine/American Medical Association Resolution 959. Am. J. Prev. Med. 2019, 56, e169–e175, Erratum in: Am. J. Prev. Med. 2019, 57, 134. [Google Scholar] [CrossRef] [Green Version]
- Pocol, C.B.; Marinescu, V.; Amuza, A.; Cadar, R.L.; Rodideal, A.A. Sustainable vs. Unsustainable Food Consumption Behaviour: A Study among Students from Romania, Bulgaria and Moldova. Sustainability 2020, 12, 4699. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Murray, C.J.; et al. Food in the Anthropocene: The EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Medical Association House of Delegates Resolution C. 2012. Available online: https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/hod/a12-resolutions_0.pdf (accessed on 4 February 2021).
- Pasarica, M.; Kay, D. Teaching evidence-based lifestyle management in family medicine training. Educ. Prim. Care 2018, 29, 60–61. [Google Scholar] [CrossRef]
- Sagner, M.; Katz, D.; Egger, G.; Lianov, L.; Schulz, K.-H.; Braman, M.; Behbod, B.; Phillips, E.; Dysinger, W.; Ornish, D. Lifestyle medicine potential for reversing a world of chronic disease epidemics: From cell to community. Int. J. Clin. Pract. 2014, 68, 1289–1292. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Plasonja, N.; Décamps, G. Assessing Orthorexia Nervosa: Validation of the Polish Version of the Eating Habits Questionnaire in a General Population Sample. Nutrients 2020, 12, 3820. [Google Scholar] [CrossRef] [PubMed]
| Croatia n = 1402 | Foggia, Italy n = 2324 | Pavia, Italy n = 898 | Lebanon n = 401 | Poland n = 245 | Romania n = 209 | Spain n = 535 | Turkey n = 208 | p¶ | |
|---|---|---|---|---|---|---|---|---|---|
| Age (years) median (IQR) | 21.0 (3.0) | 23.0 (1.0) | 21.0 (2.0) | 19.0 (2.0) | 22.0 (2.0) | 24.0 (2.0) | 21.0 (3.0) | 21.0 (2.0) | <0.001 § |
| Female gender n (%) | 1096 (78.2) | 1308 (56.3) | 62 (69.7) | 261 (65.1) | 202 (82.4) | 155 (74.2) | 213 (39.8) | 129 (62.6) | <0.001 * |
| Grade point average (percentile) median (IQR) | 0.67 (0.2) | 0.67 (0.3) | 0.69 (0.3) | 0.57 (0.3) | 0.75 (0.2) | 0.68 (0.2) | 0.56 (0.2) | 0.43 (0.3) | <0.001 § |
| Smoking n (%) | <0.001 * | ||||||||
| yes | 323 (23.1) | 590 (25.4) | 192 (21.6) | 105 (26.2) | 61 (24.9) | 74 (35.4) | 64 (12.0) | 45 (21.8) | |
| ex-smokers | 189 (13.5) | 134 (5.8) | 55 (6.2) | 35 (8.7) | 36 (14.7) | 28 (13.4) | 62 (11.6) | 17 (8.3) | |
| never smoked | 885 (63.4) | 1600 (68.8) | 641 (72.2) | 261 (65.1) | 148 (60.4) | 107 (51.2) | 409 (76.4) | 144 (69.9) | |
| BMI (kg/m2) median (IQR) | 21.7 (3.5) | 23.0 (2.4) | 21.1 (3.6) | 23.2 (5.8) | 21.3 (4.1) | 22.1 (4.9) | 22.3 (2.9) | 21.7 (4.3) | <0.001 § |
| Self-rated health perception median (IQR) | 9.0 (1.0) | 8.0 (2.0) | 8.0 (2.0) | 8.0 (2.0) | 8.0 (1.5) | 8.0 (2.0) | 8.0 (1.0) | 8.0 (2.0) | <0.001 § |
| Breakfast daily n (%) | 765 (54.8) | 1760 (75.7) | 675 (75.3) | 173 (43.3) | 157 (64.1) | 88 (42.1) | 337 (64.3) | 72 (36.7) | <0.001 * |
| ORTO-15 score median (IQR) | 36.0 (5.0) | 35.0 (6.0) | 37.0 (6.0) | 37.0 (6.0) | 38.0 (8.0) | 36.0 (6.0) | - | 36.0 (7.0) | <0.001 § |
| MDSS score median (IQR) | 6.0 (5.0) | 8.5 (6.8) | 10.0 (6.0) | 6.0 (5.0) | 6.0 (5.0) | 8.0 (6.0) | 10.0 (9.0) | 5.0 (6.0) | <0.001 § |
| Sleep duration on working days (h) median (IQR) | 7.0 (1.8) | 8.0 (1.5) | 7.7 (1.5) | 7.0 (2.0) | 8.0 (1.3) | 7.5 (1.5) | 8.0 (1.5) | 7.0 (1.5) | <0.001 § |
| Sleep duration on non-working days (h) median (IQR) | 9.0 (1.5) | 8.0 (2.0) | 8.0 (1.5) | 9.0 (2.0) | 9.0 (2.0) | 9.0 (2.0) | 8.5 (1.0) | 8.5 (1.0) | <0.001 § |
| Total METs per week † median (IQR) | 2796.0 (2964.0) | 3462.0 (3885.0) | 3222.0 (3480.0) | 2220.0 (3501.0) | 2457.0 (3133.5) | 3274.5 (3740.9) | 4072.8 (3829.8) | 1653.0 (2572.0) | <0.001 § |
| Daily mobile use (h) median (IQR) | 3.0 (3.0) | 4.0 (4.0) | 3.0 (2.0) | 5.0 (4.0) | 3.0 (3.0) | 4.0 (3.0) | 3.0 (3.0) | 3.0 (2.0) | <0.001 § |
| Daily study time (h) median (IQR) | 3.0 (3.0) | 5.0 (3.0) | 4.0 (3.0) | 3.0 (2.0) | 2.0 (2.0) | 2.0 (3.0) | 2.0 (2.0) | 3.0 (3.0) | <0.001 § |
| PSS-10 score median (IQR) | 19.0 (9.0) | 20.0 (7.0) | 19.0 (9.0) | 21.0 (7.0) | 20.0 (9.0) | 20.0 (6.0) | 17.0 (9.0) | 22.0 (7.0) | <0.001 § |
| Students asking for more education on lifestyle and health n (%) | 432 # (49.3) | 939 (40.4) | 332 (37.3) | 196 (48.9) | - | 65 (31.1) | 261 (48.8) | 57 (28.5) | <0.001 * |
| Breakfast Frequency | ORTO-15 | Working Days Sleep Duration | Non-Working Days Sleep Duration | Total METs Per Week | Mobile Phone Use | Study Time | PSS-10 Score | Self-Rated Health Perception | BMI | Age | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| MDSS score | 0.22 <0.001 | −0.15 <0.001 | 0.10 <0.001 | −0.10 <0.001 | 0.16 <0.001 | −0.02 0.133 | 0.13 <0.001 | −0.02 0.122 | 0.03 0.008 | −0.01 0.950 | 0.10 <0.001 |
| Breakfast frequency | −0.07 <0.001 | 0.13 <0.001 | −0.12 <0.001 | 0.04 0.001 | −0.06 <0.001 | 0.12 <0.001 | −0.08 <0.001 | 0.06 <0.001 | −0.03 0.009 | 0.04 0.006 | |
| ORTO-15 | −0.07 <0.001 | 0.06 <0.001 | −0.11 <0.001 | −0.04 0.011 | −0.05 <0.001 | −0.03 0.030 | −0.02 0.153 | −0.09 <0.001 | −0.05 0.001 | ||
| Working days sleep duration | 0.18 <0.001 | 0.03 0.017 | 0.02 0.246 | 0.04 0.001 | −0.04 0.001 | 0.03 0.028 | −0.01 0.920 | 0.06 <0.001 | |||
| Non-working days sleep duration | −0.06 <0.001 | −0.01 0.711 | −0.12 <0.001 | 0.02 0.140 | −0.00 0.849 | −0.05 <0.001 | −0.08 <0.001 | ||||
| Total METs per week | −0.05 0.001 | −0.06 <0.001 | −0.12 <0.001 | 0.13 <0.001 | 0.09 <0.001 | 0.06 <0.001 | |||||
| Mobile phone use | 0.09 <0.001 | 0.15 <0.001 | −0.03 0.058 | 0.04 0.003 | −0.06 <0.001 | ||||||
| Study time | 0.06 <0.001 | 0.01 0.491 | 0.00 0.847 | 0.09 <0.001 | |||||||
| PSS-10 score | −0.27 <0.001 | 0.00 0.972 | −0.06 <0.001 | ||||||||
| Self-rated health perception | −0.05 <0.001 | 0.05 <0.001 | |||||||||
| BMI | 0.14 <0.001 |
| Self-Rated Health Perception Beta (p Value) | BMI Beta (p Value) | |
|---|---|---|
| Age (years) | 0.01 (0.509) | 0.13 (<0.001) |
| Female gender (males are referent) | 0.03 (0.018) | 0.30 (<0.001) |
| Smoking (nonsmokers are referent group) | ||
| Active smokers | −0.06 (<0.001) | 0.03 (0.016) |
| Ex-smokers | −0.00 (0.898) | −0.01 (0.347) |
| BMI (kg/m2) | −0.10 (<0.001) | na |
| Cohort (Croatia is referent group) * | ||
| Foggia, Italy | −0.09 (<0.001) | 0.00 (0.940) |
| Pavia, Italy | −0.12 (<0.001) | −0.10 (<0.001) |
| Lebanon | −0.08 (<0.001) | 0.13 (<0.001) |
| Poland | −0.12 (<0.001) | −0.03 (0.009) |
| Romania | −0.03 (0.028) | 0.02 (0.174) |
| Spain | −0.05 (<0.001) | −0.03 (0.053) |
| Turkey | −0.07 (<0.001) | −0.01 (0.264) |
| MDSS score | 0.02 (0.171) | 0.01 (0.311) |
| Breakfast frequency (days per week) | 0.04 (0.003) | −0.01 (0.335) |
| Working days sleep duration (h) | 0.02 (0.071) | −0.01 (0.355) |
| Non-working days sleep duration (h) | −0.02 (0.059) | −0.03 (0.040) |
| Total METs per week | 0.08 (<0.001) | 0.04 (0.002) |
| Mobile phone use (h/day) | −0.00 (0.878) | 0.05 (<0.001) |
| Study time (h/day) | 0.03 (0.039) | 0.00 (0.970) |
| PSS-10 score (h/day) | −0.23 (<0.001) | 0.04 (0.002) |
| Self-rated health perception | na | −0.10 (<0.001) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cena, H.; Porri, D.; De Giuseppe, R.; Kalmpourtzidou, A.; Salvatore, F.P.; El Ghoch, M.; Itani, L.; Kreidieh, D.; Brytek-Matera, A.; Pocol, C.B.; et al. How Healthy Are Health-Related Behaviors in University Students: The HOLISTic Study. Nutrients 2021, 13, 675. https://doi.org/10.3390/nu13020675
Cena H, Porri D, De Giuseppe R, Kalmpourtzidou A, Salvatore FP, El Ghoch M, Itani L, Kreidieh D, Brytek-Matera A, Pocol CB, et al. How Healthy Are Health-Related Behaviors in University Students: The HOLISTic Study. Nutrients. 2021; 13(2):675. https://doi.org/10.3390/nu13020675
Chicago/Turabian StyleCena, Hellas, Debora Porri, Rachele De Giuseppe, Aliki Kalmpourtzidou, Fiorella Pia Salvatore, Marwan El Ghoch, Leila Itani, Dima Kreidieh, Anna Brytek-Matera, Cristina Bianca Pocol, and et al. 2021. "How Healthy Are Health-Related Behaviors in University Students: The HOLISTic Study" Nutrients 13, no. 2: 675. https://doi.org/10.3390/nu13020675