The Effect of a Combined Gluten- and Casein-Free Diet on Children and Adolescents with Autism Spectrum Disorders: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Study Selection
2.2.1. Population
2.2.2. Intervention
2.2.3. Comparator
2.2.4. Outcomes
- Core autistic symptoms, clinician-/observer-reported.
- Adaptive functional level in the child, clinician-reported.
- Adaptive functional level in the child, parent-reported.
- Core autistic symptoms, parent-reported.
- Gastrointestinal discomfort.
- Behavioral difficulties, clinician-/observer-reported.
- Behavioral difficulties, parent-reported.
- Other side effects, such as constipation, irregular bowel, diarrhea, stomach aches, sleep disturbances, and appetite disturbances.
- Weight change.
- Child quality of life, parent-reported.
- Parental well-being.
2.3. Study Design
2.4. Report Characteristics
2.5. Data Extraction of Individual Randomized Trials
2.6. Quality Assessment
2.7. Meta-Analysis
3. Results
3.1. Literature Search
3.2. Description of the Primary Studies
3.3. Synthesis of Results of Primary Studies
3.3.1. Primary Outcome: Clinician-Assessed Core Symptoms
3.3.2. Secondary Outcomes
3.4. Certainty of Evidence (GRADE)
4. Discussion
Strengths and Limitations
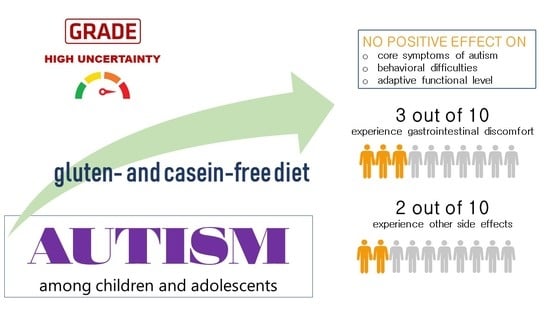
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fakhoury, M. Autistic spectrum disorders: A review of clinical features, theories and diagnosis. Int. J. Dev. Neurosci. 2015, 43, 70–77. [Google Scholar] [CrossRef]
- Autism Spectrum Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders (accessed on 27 January 2021).
- Faras, H.; Al, A.N.; Tidmarsh, L. Autism spectrum disorders. Ann. Saudi Med. 2010, 30, 295–300. [Google Scholar] [CrossRef]
- Buie, T.; Campbell, D.B.; Fuchs, G.J.; Furuta, G.T., III; Levy, J.; Vandewater, J.; Whitaker, A.H.; Atkins, D.; Bauman, M.L.; Beaudet, A.L.; et al. Evaluation, diagnosis, and treatment of gastrointestinal disorders in individuals with ASDs: A consensus report. Pediatrics 2010, 125 (Suppl. 1), 1–18. [Google Scholar] [CrossRef] [Green Version]
- Xu, G.; Snetselaar, L.G.; Jing, J.; Liu, B.; Strathearn, L.; Bao, W. Association of food allergy and other allergic conditions with autism spectrum disorder in children. JAMA Netw. Open 2018, 1, e180279. [Google Scholar] [CrossRef]
- Jyonouchi, H.; Sun, S.; Itokazu, N. Innate immunity associated with inflammatory responses and cytokine production against common dietary proteins in patients with autism spectrum disorder. Neuropsychobiology 2002, 46, 76–84. [Google Scholar] [CrossRef]
- Jyonouchi, H. Food allergy and autism spectrum disorders: Is there a link? Curr. Allergy Asthma Rep. 2009, 9, 194–201. [Google Scholar] [CrossRef]
- Li, H.; Liu, H.; Chen, X.; Zhang, J.; Tong, G.; Sun, Y. Association of food hypersensitivity in children with the risk of autism spectrum disorder: A meta-analysis. Eur. J. Pediatr. 2020, 4, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Fattorusso, A.; Di Genova, L.; Dell’isola, G.B.; Mencaroni, E.; Esposito, S. Autism spectrum disorders and the gut microbiota. Nutrients 2019, 11, 521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srikantha, P.; Mohajeri, H.M. The possible role of the microbiota-gut-brain-axis in autism spectrum disorder. Int. J. Mol. Sci. 2019, 20, 2115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 28, 637–641. [Google Scholar] [CrossRef]
- Genuis, S.J.; Lobo, R.A. Gluten sensitivity presenting as a neuropsychiatric disorder. Gastroenterol. Res. Pract. 2014, 2014, 293206. [Google Scholar] [CrossRef] [PubMed]
- Genuis, S.J.; Bouchard, T.P. Celiac disease presenting as autism. J. Child Neurol. 2010, 25, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Herbert, M.R.; Buckley, J.A. Autism and dietary therapy: Case report and review of the literature. J. Child Neurol. 2013, 28, 975–982. [Google Scholar] [CrossRef]
- Herbert, M.R. Contributions of the environment and environmentally vulnerable physiology to autism spectrum disorders. Curr. Opin. Neurol. 2010, 23, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Knivsberg, A.M.; Reichelt, K.L.; Nodland, M. Dietary intervention for a seven year old girl with autistic behaviour. Nutr. Neurosci. 1999, 2, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.L.; Lin, C.Y.; Chen, C.L.; Wang, C.M.; Wong, M.K. The effects of a gluten and casein-free diet in children with autism: A case report. Chang. Gung. Med. J. 2009, 32, 459–465. [Google Scholar]
- Cormier, E.; Elder, J.H. Diet and child behavior problems: Fact or fiction? Pediatr. Nurs. 2007, 33, 138–143. [Google Scholar]
- Millward, C.; Ferriter, M.; Calver, S.; Connell-Jones, G. Gluten- and casein-free diets for autistic spectrum disorder. Cochrane Database Syst. Rev. 2008. [Google Scholar] [CrossRef]
- Knivsberg, A.M.; Reichelt, K.L.; HØien, T.; NØdland, M. A randomised, controlled study of dietary intervention in autistic syndromes. Nutr. Neurosci. 2002, 5, 251–261. [Google Scholar] [CrossRef]
- Elder, J.H.; Shankar, M.; Shuster, J.; Theriaque, D.; Burns, S.; Sherrill, L. The gluten-free, casein-free diet in autism: Results of a preliminary double blind clinical trial. J. Autism Dev. Disord. 2006, 36, 413–420. [Google Scholar] [CrossRef]
- Hyman, S.L.; Levy, S.E.; Myers, S.M. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics 2020, 145, e20193447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. MetaArXiv 2020. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 2, 350. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.1 (Updated September 2020). Available online: www.training.cochrane.org/handbook (accessed on 27 January 2021).
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Atkins, D.; Brozek, J.; Vist, G.; Alderson, P.; Glasziou, P.; Falck-Ytter, Y.; Schünemann, H.J.; et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J. Clin. Epidemiol. 2011, 64, 395–400. [Google Scholar] [CrossRef]
- Covidence–Better Systematic Review Management. Covidence Systematic Review Software; Veritas Health Innovation: Melbourne, Australia. Available online: www.covidence.org (accessed on 27 January 2021).
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med. Res. Methodol. 2007, 7, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 18, 343. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Brondino, N.; Fusar-Poli, L.; Rocchetti, M.; Provenzani, U.; Barale, F.; Politi, P. Complementary and alternative therapies for autism spectrum disorder. Evid. Based Complement Alternat. Med. 2015, 2015, 258589. [Google Scholar] [CrossRef] [Green Version]
- Elder, J.; Kreider, C.; Schaefer, N.; de Laosa, M. A review of gluten- and casein-free diets for treatment of autism: 2005–2015. Nutr. Diet Suppl. 2015, 7, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piwowarczyk, A.; Horvath, A.; Lukasik, J.; Pisula, E.; Szajewska, H. Gluten- and casein-free diet and autism spectrum disorders in children: A systematic review. Eur. J. Nutr. 2018, 57, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.R.; Handen, B.L.; Zimmer, M.; Sacco, K.; Turner, K. Effects of gluten free/casein free diet in young children with autism: A pilot study. Eur. J. Nutr. 2011, 23, 213–225. [Google Scholar] [CrossRef]
- Whiteley, P.; Haracopos, D.; Knivsberg, A.M.; Reichelt, K.L.; Parlar, S.; Jacobsen, J.; Seim, A.; Pedersen, L.; Schondel, M.; Shattock, P.; et al. The ScanBrit randomised, controlled, single-blind study of a gluten- and casein-free dietary intervention for children with autism spectrum disorders. Nutr. Neurosci. 2010, 13, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Navarro, F.; Pearson, D.A.; Fatheree, N.; Mansour, R.; Hashmi, S.S.; Rhoads, J.M. Are ‘leaky gut’ and behavior associated with gluten and dairy containing diet in children with autism spectrum disorders? Nutr. Neurosci. 2015, 18, 177–185. [Google Scholar] [CrossRef]
- González-Domenech, P.J.; Díaz Atienza, F.; García Pablos, C.; Fernández Soto, M.L.; Martínez-Ortega, J.M.; Gutiérrez-Rojas, L. Influence of a combined gluten-free and casein-free diet on behavior disorders in children and adolescents diagnosed with autism spectrum disorder: A 12-month follow-up clinical trial. J. Autism Dev. Disord. 2020, 50, 935–948. [Google Scholar] [CrossRef]
- Carr, T. Autism Diagnostic Observation Schedule; Springer: New York, NY, USA, 2013. [Google Scholar]
- McCrimmon, A.; Rostad, K. Test review: Autism diagnostic observation schedule, second edition (ADOS-2) manual (Part II): Toddler module. J. Psychoeduc. Asses. 2014, 32, 88–92. [Google Scholar] [CrossRef]
- Kuschner, E.S.; Morton, H.E.; Maddox, B.B.; de Marchena, A.; Anthony, L.G.; Reaven, J. The BUFFET program: Development of a cognitive behavioral treatment for selective eating in youth with autism spectrum disorder. Clin. Child Fam. Psychol. Rev. 2017, 20, 403–421. [Google Scholar] [CrossRef]
- Tanner, K.; Case-Smith, J.; Nahikian-Nelms, M.; Ratliff-Schaub, K.; Spees, C.; Darragh, A.R. Behavioral and physiological factors associated with selective eating in children with autism spectrum disorder. Am. J. Occup. Ther. 2015, 69, 6906180030. [Google Scholar] [CrossRef] [Green Version]
- Kothari, P.; Tate, A.; Adewumi, A.; Kinlin, L.M.; Ritwik, P. The risk for scurvy in children with neurodevelopmental disorders. Spec. Care Dent. 2020, 40, 251–259. [Google Scholar] [CrossRef]
- Bonis, S. Stress and parents of children with autism: A review of literature. Issues Ment. Health Nurs. 2016, 31, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Bonis, S.A.; Sawin, K.J. Risks and protective factors for stress self-management in parents of children with autism spectrum disorder: An integrated review of the literature. J. Pediatr. Nurs. 2016, 31, 567–579. [Google Scholar] [CrossRef] [PubMed]










| Study’s First Author, Year | Region, Country | Trial Registration | Study Design | Conflict of Interest/Sponsorship |
|---|---|---|---|---|
| Elder et al., 2006 [21] | Florida, USA | Not reported | Double-blinded, crossover RCT | Conflict of interest: Not reported University of Florida s College of Nursing Biobehavioral NINR-funded research grant P20 NR 07791-03 and GCRC grant M01RR00082 from the National Institute of Research Resources, National Institutes of Health |
| Gonzalez-Domenech et al., 2019 [39] | Jaen, Granada, Malaga and Almeria, Spain | Not reported | Crossover RCT | The authors declare that they have no conflict of interest. |
| Johnson et al., 2011 [36] | Pennsylvania, USA | Not reported | Single-blinded RCT with parallel group | John F. and Nancy A. Emmerling Fund/The Pittsburgh Foundation. Financial Disclosures Dr. Benjamin Handen disclosed consulting fees for Forest, Bristol Myer Squibband has research funding from Forest, Bristol Myer Squibb, Johnson and Johnson, Neuropharm, and Curemark. |
| Knivsberg et al., 2002 [20] | Stavanger, Norway | Not reported | Single-blinded RCT with parallel group | Not reported |
| Navarro et al., 2015 [38] | Texas, USA | Not reported | Double-blinded RCT with parallel group | Not reported |
| Whiteley et al., 2010 [37] | Copenhagen, Denmark | NCT00614198 Registered in 2008 | Single-blinded RCT with parallel group | Conflict of interest reported. This study was supported by the Center for Autisme, the Nils O. Seim Family Fund for Medical Research, the Eric Birger Christensen Fond, the Norwegian Protein Intolerance Association, and the Robert Luff Foundation. |
| Study’s First Author, Year | N (% Female) | Age (Mean ± SD) (Median (IQR)) | Inclusion Criteria | Exclusion Criteria |
|---|---|---|---|---|
| Elder et al., 2006 [21] | Intervention: 7 Control: 7 (20% Female) | 7.3 ± 4.1 years | Diagnosis of ASD according to DSM-IV criteria | Children with medical histories and/or physical examinations indicated that they had physical or sensory-impairments or significant medical problems, including celiac disease. |
| Gonzalez-Domenech et al., 2019 [39] | Intervention: 15 Control: 16 (46% Female) | Overall 8.9 years | Diagnosis of ASD according to the tenth edition of the International Classification of Diseases (ICD-10). | Patients diagnosed with an allergy to gluten or casein; patients who had previously excluded gluten and/or casein from their diet; patients who were likely to not adhere to the diet properly. |
| Johnson et al., 2011 [36] | Intervention: 8 Control 14 (22% Female) | Intervention 40.1 ± 9.3 months Control 39.5 ± 8.7 months | Diagnosis of ASD according to DSM-IV criteria | Not reported |
| Knivsberg et al., 2002 [20] | Intervention: 10 Control: 10 (Not reported) | Intervention 91 months Control 86 months | Participation included only children with both the diagnosis of autism and abnormal urinary peptide patterns. | Not reported |
| Navarro et al., 2015 [38] | Intervention: 6 Control: 6 (Not reported) | Intervention 5.5 years Control 6 years | Diagnosis of ASD according to DSM-IV criteria | Children with food allergies, celiac disease, inflammatory bowel disease, and infectious GI diseases. Children with neurological problems that could interfere with proper evaluation of behavior. Children with parents unwilling to undertake the GDF diet during the study. |
| Whiteley et al., 2010 [37] | Intervention: 38 Control: 34 (11% Female) | Intervention 94.2 (IQR 76.6–118) months Control 69.4 (ICR 76.3–120.3) months | Children diagnosed with pervasive developmental disorder (ICD-10 code F84) | Children with co-morbid diagnoses of epilepsy, fragile-X syndrome, tuberous sclerosis, or a developmental age below 24 months |
| Study’s First Author, Year | Intervention (Duration) | Monitoring Tools | Control Group | Reported Outcomes | Authors Conclusion |
|---|---|---|---|---|---|
| Elder et al., 2006 [21] | GFCF experimental diet (6 weeks) | Parents received a 3- to 4-day supply of food twice each week + a list of allowed foods in case of emergencies and they were asked to record their child’s diet intake to monitor compliance. Pre and post urinary concentration of casein , gluten peptides, casomorphin and gliadorphin | Regular diet. | Core autistic symptoms, clinician-reported | Null findings |
| Gonzalez-Domenech et al., 2019 [39] | GFCF experimental diet (6 months) | 24 h recall Pre and post urinary concentrations of betacasomorphin | Regular diet | ECO scale | Null findings |
| Johnson et al., 2011 [36] | GFCF experimental diet (3 months) | Parents recorded food intake | Healthy diet without added sugar | CARS | Null findings |
| Knivsberg et al., 2002 [20] | GFCF experimental diet (12 months) | Pre and post urinary concentration of creatine | Regular diet | Improvement of core autistic symptoms on GFCF diet | |
| Navarro et al., 2015 [38] | 2 weeks of GFCF diet followed by 4 weeks of GFCF diet + supplement containing brown rice flour (4 weeks) | Daily food diary form completed by the parents. | 2 weeks of GFCF diet followed by 4 weeks of GFCF diet + supplement containing 0.5 g/kg of gluten powder and 0.5 g/kg of non-fat dried milk | Core autistic symptoms, clinician-reported | Null findings |
| Whiteley et al., 2010 [37] | GFCF experimental diet (12 months) | Nutritionists monitored to ensure dietary compliance and nutritional intake (method not specified). Urinary excretion (details not reported) | Regular diet | ATEC | Clinically irrelevant improvement of core autistic symptoms on GFCF diet |
| Outcome (Timeframe) | Study Results and Measurements | Certainty of the Evidence (Justification for Ratings) |
|---|---|---|
| Clinician assessed core symptoms (Minimum 6 months) | SMD: −0.31 (CI 95% −0.89–0.27) Based on data from 120 patients in four studies Follow up: 3–12 months | Very low a,b,c,d |
| Parent assessed functional level (Minimum 6 months) | MD: 0.61 (CI 95% −5.92–7.14) Based on data from 55 patients in one study Follow up: 12 months | Very low a,e |
| Parent assessed conduct problems (Minimum 6 months) | MD: 1.80 (CI 95% −6.56–10.16) Based on data from 22 patients in one study Follow up: 3 months | Very low a,c,d |
| Body mass index, kg/m2 (Minimum 6 months) | MD: 0.30 (CI 95% −1.81–2.41) Based on data from 63 patients in one study | Very low e,f |
| Number of persons with gastrointestinal discomfort (Minimum 6 months) | RR: 2.33 (CI 95% 0.69–7.90) Based on data from 22 patients in one study Follow up: 3 months | Very low a,c,d |
| Number of persons with side effects (Minimum 6 months) | RR: 1.89 (CI 95% 1.11–3.21) RD: 0.23 (CI 95% −0.26–0.72) Based on data from 94 patients in two studies Follow up: 3–12 months | Very low a,c,d |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keller, A.; Rimestad, M.L.; Friis Rohde, J.; Holm Petersen, B.; Bruun Korfitsen, C.; Tarp, S.; Briciet Lauritsen, M.; Händel, M.N. The Effect of a Combined Gluten- and Casein-Free Diet on Children and Adolescents with Autism Spectrum Disorders: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 470. https://doi.org/10.3390/nu13020470
Keller A, Rimestad ML, Friis Rohde J, Holm Petersen B, Bruun Korfitsen C, Tarp S, Briciet Lauritsen M, Händel MN. The Effect of a Combined Gluten- and Casein-Free Diet on Children and Adolescents with Autism Spectrum Disorders: A Systematic Review and Meta-Analysis. Nutrients. 2021; 13(2):470. https://doi.org/10.3390/nu13020470
Chicago/Turabian StyleKeller, Amélie, Marie Louise Rimestad, Jeanett Friis Rohde, Birgitte Holm Petersen, Christoffer Bruun Korfitsen, Simon Tarp, Marlene Briciet Lauritsen, and Mina Nicole Händel. 2021. "The Effect of a Combined Gluten- and Casein-Free Diet on Children and Adolescents with Autism Spectrum Disorders: A Systematic Review and Meta-Analysis" Nutrients 13, no. 2: 470. https://doi.org/10.3390/nu13020470