Children, Adolescents, and Young Adults with Borderline Intellectual Functioning: Etiological, Neurophysiological, and Mri Findings in a Cohort of 651 Patients
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Peltopuro, M.; Ahonen, T.; Kaartinen, J.; Seppälä, H.; Närhi, V. Borderline intellectual functioning: A systematic literature review. Intellect. Dev. Disabil. 2014, 52, 419–443. [Google Scholar] [CrossRef] [Green Version]
- Greenspan, S. Borderline intellectual functioning: An update. Curr. Opin. Psychiatry 2017, 30, 113–122. [Google Scholar] [CrossRef]
- Belanger, S.A.; Caron, J. Evaluation of the child with global developmental delay and intellectual disability. Paediatr. Child Health 2018, 23, 403–410. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems (10th Rev.); World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Ninivaggi, F.J. Borderline intellectual functioning in children and adolescents: Reexamining an underrecognized yet prevalent clinical comorbidity. Conn. Med. 2001, 65, 7–11. [Google Scholar] [PubMed]
- Salvador-Carulla, L.; Garcia-Gutierrez, J.C.; Gutierrez-Colosia, M.R.; Artigas-Pallares, J.; Garcia Ibanez, J.; Perez, J.G.; Nadal Pla, M.; Aguilera Ines, F.; Isus, S.; Cereza, J.M.; et al. Borderline intellectual functioning: Consensus and good practice guidelines. Rev. Psiquiatr. Salud. Ment. 2013, 6, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Hassiotis, A. Borderline intellectual functioning and neurodevelopmental disorders: Prevalence, comorbidities and treatment approaches. Adv. Ment. Health Intellect. Disabil. 2015, 9, 275–283. [Google Scholar] [CrossRef]
- Aicardi, J. The etiology of developmental delay. Semin. Pediatr. Neurol. 1998, 5, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, C.; Horne, K.; Witol, A. Neurobehavioral functioning in children with fetal alcohol spectrum disorder. Child Neuropsychol. 2006, 12, 453–468. [Google Scholar] [CrossRef] [PubMed]
- Kodituwakku, P.W. Neurocognitive profile in children with fetal alcohol spectrum disorders. Dev. Disab. Res. Rev. 2009, 15, 218–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomaidis, L.; Zantopoulos, G.Z.; Fouzas, S.; Mantagou, L.; Bakoula, C.; Konstantopoulos, A. Predictors of severity and outcome of global developmental delay without definitive etiologic yield: A prospective observational study. BMC Pediatr. 2014, 14, 40. [Google Scholar] [CrossRef]
- Oh, D.L.; Jerman, P.; Marques, S.S.; Koita, K.; Boparai, S.K.P.; Harris, N.B.; Bucci, M. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018, 18, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, Y.; D´Arcy, C.; Yuan, S.; Meng, X. How does childhood maltreatment influence ensuing cognitive functioning among people with the exposure of childhood maltreatment? A systematic review of prospective cohort studies. J. Affect. Disord. 2019, 252, 278–293. [Google Scholar] [CrossRef]
- Yeoh, S.L.; Eastwood, J.; Wright, I.M.; Morton, R.; Melhuish, E.; Ward, M.; Oei, J.L. Cognitive and motor outcomes of children with prenatal opioid exposure. A systematic review and meta-analysis. JAMA Netw. Open 2019, 2, e197025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gumusoglu, S.B.; Chilukuri, A.S.S.; Santillan, D.A.; Santillan, M.K.; Stevens, H.E. Neurodevelopmental outcomes of prenatal preeclampsia exposure. Trends Neurosci. 2020, 43, 253–268. [Google Scholar] [CrossRef] [PubMed]
- Young-Southward, G.; Eaton, C.; O´Connor, R.; Minnis, H. Investigating the causal relationship between maltreatment and cognition in children: A systematic review. Child Abuse Negl. 2020, 107, 104603. [Google Scholar] [CrossRef]
- Schreglmann, M.; Ground, M.; Vollmer, B.; Johnson, M.J. Systematic review: Long-term cognitive and behavioural outcomes of neonatal hypoxic-ischaemic encephalopathy in children without cerebral palsy. Acta Paediatr. 2020, 109, 20–30. [Google Scholar] [CrossRef]
- Sacchi, C.; Marino, C.; Nosarti, C.; Vieno, A.; Visentin, S.; Simonelli, A. Association of intrauterine growth restriction and small for gestational age status with childhood cognitive outcomes. A systematic review and meta-analysis. JAMA Pediatr. 2020, 174, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Shevell, M.I.; Majnemer, A.; Rosenbaum, P.; Abrahamowicz, M. Etiologic determination of childhood developmental delay. Brain Dev. 2001, 23, 228–235. [Google Scholar] [CrossRef]
- Srour, M.; Mazer, B.; Shevell, M.I. Analysis of clinical features predicting etiologic yield in the assessment of global developmental delay. Pediatrics 2006, 118, 139–145. [Google Scholar] [CrossRef] [Green Version]
- Michelson, D.J.; Shevell, M.I.; Sherr, E.H.; Moeschler, J.B.; Gropman, A.L.; Ashwal, S. Evidence report: Genetic and metabolic testing on children with developmental delay. Report of the quality standards subcommittee of the American academy of neurology and the practice committee of the child neurology society. Neurology 2011, 77, 1629–1635. [Google Scholar] [CrossRef]
- Lopez-Pison, J.; Garcia-Jimenez, M.C.; Monge-Galindo, L.; Lafuente-Hidalgo, M.; Perez-Delgado, R.; Garcia-Oguiza, A.; Pena-Segura, J.L. Our experience with the aetiological diagnosis of global developmental delay and intellectual disability: 2006–2010. Neurologia 2014, 29, 402–407. [Google Scholar] [CrossRef]
- Moeschler, J.B.; Shevell, M.; Committee on genetics. Comprehensive evaluation of the child with intellectual disability or global developmental delays. Pediatrics 2014, 134, e903–e918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mithyantha, R.; Kneen, R.; McCann, E.; Gladstone, M. Current evidence-based recommendations on investigating children with global developmental delay. Arch. Dis. Child 2017, 102, 1071–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O´Byrne, J.J.; Lynch, S.A.; Treacy, E.P.; King, M.D.; Betts, D.R.; Mayne, P.D.; Sharif, F. Unexplained developmental delay/learning disability: Guidelines for best practice protocol for first line assessment and genetic/metabolic/radiological investigations. Ir. J. Med. Sci. 2016, 185, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Alamri, A.; Aljadhai, Y.I.; Alrashed, A.; Alfheed, B.; Abdelmoaty, R.; Alenazi, S.; Sharif, M.D. Identifying clinical clues in children with global developmental delay/intellectual disability with abnormal brain magnetic resonance imaging (MRI). J. Child Neurol. 2020, 36, 432–439. [Google Scholar] [CrossRef] [PubMed]
- D’ Arrigo, S.; Gavazzi, F.; Alfei, E.; Zuffardi, O.; Montomoli, C.; Corso, B.; Buzzi, E.; Sciacca, F.L.; Bulgheroni, S.; Riva, D.; et al. The diagnostic yield of array comparative genomic hybridization is high regardless of severity of intellectual disability/developmental delay in children. J. Child Neurol. 2016, 31, 691–699. [Google Scholar] [CrossRef]
- Srivastava, S.; Love-Nichols, J.A.; Dies, K.A.; Ledbetter, D.H.; Martin, C.L.; Chung, W.K.; Firth, H.V.; Frazier, T.; Hansen, R.L.; Prock, L.; et al. Meta-analysis and multidisciplinary consensus statement: Exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet. Med. 2019, 21, 2413–2421. [Google Scholar] [CrossRef] [Green Version]
- Murias, K.; Moir, A.; Myers, K.A.; Liu, I.; Wei, X.-C. Systematic review of MRI findings in children with developmental delay or cognitive impairment. Brain Dev. 2017, 39, 644–655. [Google Scholar] [CrossRef]
- Maher, C.O.; Piatt, J.H. Incidental findings on brain and spine imaging in children. Pediatrics 2020, 135, e1084–e1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Karnebeek, C.D.; Stockler, S. Treatable inborn errors of metabolism causing intellectual disability: A systematic literature review. Mol. Genet. Metab. 2012, 105, 368–381. [Google Scholar] [CrossRef] [PubMed]
- Vallance, H.; Sinclair, G.; Rakic, B.; Stockler-Ipsiroglu, S. Diagnostic yield from routine metabolic screening tests in evaluation of global developmental delay and intellectual disability. Paediatr. Child Health 2021, 26, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Aldenkamp, A.P.; Arends, J. Effects of epileptiform EEG discharges on cognitive function: Is the concept of “transient cognitive impairment” still valid? Epilepsy Behav. 2004, 5 (Suppl. 1), S25–S34. [Google Scholar] [CrossRef] [PubMed]
- Ontario Health (Quality). Genome-wide sequencing for unexplained developmental disabilities or multiple congenital anomalies: A health technology assessment. Ont. Health Technol. Assess. Ser. 2020, 20, 1–178. Available online: https://www.hqontario.ca/evidence-to-improve-care/health-technology-assessment/reviews-and-recommendations/genome-wide-sequencing-for-unexplained-developmental-disabilities-and-multiple-congenital-anomalies (accessed on 20 October 2022).
- Klau, J.; Jamra, R.A.; Radtke, M.; Oppermann, H.; Lemke, J.R.; Beblo, S.; Pop, B. Exome first approach to reduce diagnostic costs and time—Retrospective analysis of 111 individuals with rare neurodevelopmental disorders. Eur. J. Hum. Genet. 2022, 30, 117–125. [Google Scholar] [CrossRef]
- Aaltio, J.; Hyttinen, V.; Kortelainen, M.; Frederix, G.W.J.; Lönnqvist, T.; Suomalainen, A.; Isohanni, P. Cost-effectiveness of whole-exome sequencing in progressive neurological disorders of children. Eur. J. Paediatr. Neurol. 2022, 36, 30–36. [Google Scholar] [CrossRef]
| Etiologies by Categories | Patients n (%) |
|---|---|
| Pre- or perinatal causes: Asphyxia, periventricular leukomalacia, | 99 (40.4) |
| neonatal CNS infarct or bleeding, low or very low birth weight/ | |
| small for gestational age | |
| Genetic syndromes/Chromosomal abnormalities: | 76 (31.0) |
| NF1, TSC, Spastic paraparesis, Crouzon, CHARGE, Helsmoortel- | |
| Van Der Aa, Holt-Oram, Leopard, Rieger, Rubinstein–Taybi, | |
| Catch-22, Noonan, Sotos, Wiever, Floating–Harbor, | |
| Single abnormal findings in microarray, 47XXX, 47XXY (Klinefelter), | |
| 6/14 balanced translocation, 8/17 balanced translocation, | |
| 9p-tetrasomia mosaicism | |
| Neurologic condition: Severe epilepsy/epileptic encephalopathy, | 22 (9.0) |
| medulloblastoma status post, Becker muscular dystrophy, myoclonus-dystonia syndrome, congenital myasthenia gravis, | |
| Ataxia NAS | |
| Maternal substance use: alcohol (FASD), drugs | 19 (7.8) |
| Cerebral dysgenesis: polymicrogyria, corpus callosum agenesis, | |
| syntelencephaly, vermis hypoplasia, pontocerebellar hypoplasia, | |
| bilateral heterotopia | 14 (5.7) |
| Brain injury (Accidental or non-accidental) | 10 (4.1) |
| Psychosocial deprivation | 4 (1.6) |
| CNS infection: Toxoplasmosis | 1 (0.4) |
| Reported Morbidities in Relatives | Patients n (%) |
|---|---|
| Global developmental delay/intellectual disability | 207 (31.8) |
| Specific learning disorder (dyslexia, dyscalculia) | 173 (26.6) |
| Attention-deficit hyperactivity disorder | 138 (21.2) |
| Specific language impairment/speech delay | 99 (15.2) |
| Emotional/Mood disorder | 93 (14.3) |
| Neuropsychiatric disorder (Tourette, autism spectrum) | 40 (6.1) |
| Epilepsy | 10 (1.5) |
| Illiteracy | 2 (0.3) |
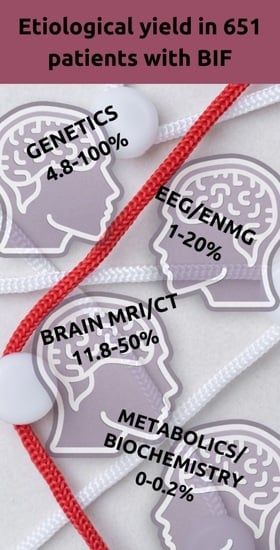
| Investigations, n | Abnormal Result, n | Result Leading to BIF Etiology, n | Overall Etiologic Yield, % | |
|---|---|---|---|---|
| Biochemistry screening | 497 | 3 | 1 | 0.2 |
| Metabolic screening | 324 | 23 * | 0 | 0 |
| TORCH antibodies | 19 | 1 | 1 | 5.3 |
| Genetic studies: | ||||
| Karyotype | 146 | 8 | 7 | 4.8 |
| Fragile-X | 182 | 0 | 0 | 0 |
| Microarray | 189 | 56 | 45 | 23.8 |
| Exome sequencing | 3 | 3 | 3 | 100 |
| Specific gene or panel | 47 | 20 | 19 | 40.4 |
| EEG | 382 | 129 ** | 4 | 1 |
| Brain MRI | 263 | 74 | 31 | 11.8 |
| Spinal cord MRI | 5 | 1 | 0 | 0 |
| Brain CT | 8 | 2 | 1 | 50 |
| ENMG | 5 | 1 | 1 | 20 |
| VEP | 8 | 5 | 0 | 0 |
| ERG | 6 | 0 | 0 | 0 |
| Brain MRI Findings | Total, n | Leading to Etiology, n | Contributing to Etiology, n | Not Related to Etiology, n |
|---|---|---|---|---|
| Non-specific ventricle dilatation/ventriculomegalia | 16 | 16 | ||
| Corpus callosum hypoplasia/agenesia | 9 | 9 | ||
| PVL (+hydrocephalus) | 8 | 8 | ||
| Non-specific white matter signals | 7 | 7 | ||
| Chiari 1 | 6 | 6 | ||
| Empty sella/Hypoplastic neurohypophysis | 5 | 5 | ||
| Arachnoid cyst | 5 | 5 | ||
| Posthemorrhage/Postischemic defect | 4 | 4 | ||
| Posttraumatic/postoperative defect | 4 | 2 | 1 | 1 |
| Astrosytomas, tubers, subependymal noduses related to TSC | 3 | 3 | ||
| Non-specific enlargement of subarachnoid spaces | 3 | 3 | ||
| Hamartomas related to NF1 | 3 | 3 | ||
| Pineal cyst | 3 | 3 | ||
| Venous angioma | 2 | 2 | ||
| Syntelencephalia | 2 | 2 | ||
| Polymicrogyria + Corpus callosum agenesia | 1 | 1 | ||
| Pontocerebellar hypoplasia | 1 | 1 | ||
| Medulloblastooma, status post | 1 | 1 | ||
| Bilateral heterotopia | 1 | 1 | ||
| Dandy–Walker | 1 | 1 | ||
| Tuber cinereum lipoma | 1 | 1 | ||
| Cisterna magna | 1 | 1 | ||
| Papilla atrophy | 1 | 1 | ||
| Porencephalic cyst | 1 | 1 | ||
| Vermis hypoplasia | 3 | 2 | 1 |
| EEG Findings | Total, n | Leading to Etiology, n | Contributing to Etiology, n | Not related to Etiology, n |
|---|---|---|---|---|
| Focal epileptiform abnormalities without epilepsy | 29 | 2 | 27 | |
| Focal epileptiform abnormalities related to focal epilepsy | 27 | 1 | 3 | 22 |
| Diffuse beta/slow waves/abnormal background activity | 26 | 1 | 1 | 24 |
| Bilateral spike/slow waves without epilepsy | 22 | 2 | 20 | |
| Bilateral epileptiform abnormalities related to generalized epilepsy | 17 | 1 | 1 | 15 |
| CSWS | 4 | 1 | 3 | |
| Focal epileptiform abnormalities related to prenatal/perinatal incident | 4 | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sätilä, H.; Jolma, L.M.; Koivu-Jolma, M. Children, Adolescents, and Young Adults with Borderline Intellectual Functioning: Etiological, Neurophysiological, and Mri Findings in a Cohort of 651 Patients. Neurol. Int. 2022, 14, 1007-1017. https://doi.org/10.3390/neurolint14040080
Sätilä H, Jolma LM, Koivu-Jolma M. Children, Adolescents, and Young Adults with Borderline Intellectual Functioning: Etiological, Neurophysiological, and Mri Findings in a Cohort of 651 Patients. Neurology International. 2022; 14(4):1007-1017. https://doi.org/10.3390/neurolint14040080
Chicago/Turabian StyleSätilä, Heli, Laura Mirjami Jolma, and Mikko Koivu-Jolma. 2022. "Children, Adolescents, and Young Adults with Borderline Intellectual Functioning: Etiological, Neurophysiological, and Mri Findings in a Cohort of 651 Patients" Neurology International 14, no. 4: 1007-1017. https://doi.org/10.3390/neurolint14040080