Emetic Tartar-Loaded Liposomes as a New Strategy for Leishmaniasis Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
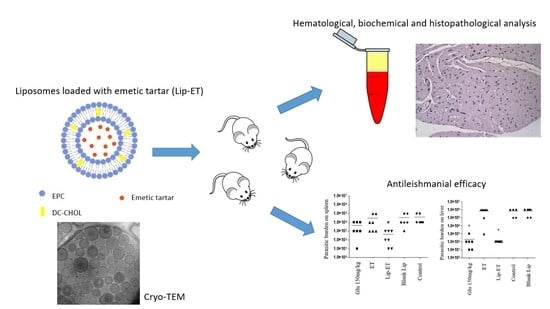
2.2. Liposome Preparation
2.3. Physicochemical Characterization of Liposomes
2.3.1. Size, Polydispersity Index (PDI), Zeta Potential, and Morphology
2.3.2. Amount of Encapsulation
2.4. Preliminary Stability Assessment of Lip-ET
2.5. Acute Toxicity
2.6. In Vivo Antileishmanial Efficacy
2.7. Statistical Analysis
3. Results
3.1. Physicochemical Characterization of Liposomes
3.2. Preliminary Stability Assessment of Lip-ET
3.3. Acute Toxicity
3.4. In Vivo Antileishmanial Efficacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berman, J.D. Human Leishmaniasis: Clinical, Diagnostic, and Chemotherapeutic Developments in the Last 10 Years. Clin. Infect. Dis. 1997, 24, 684–703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvar, J.; Vélez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Jannin, J.; de Boer, M. Leishmaniasis Worldwide and Global Estimates of Its Incidence. PLoS ONE 2012, 7, e35671. [Google Scholar] [CrossRef] [PubMed]
- Pace, D. Leishmaniasis. J. Infect. 2014, 69, S10–S18. [Google Scholar] [CrossRef] [PubMed]
- Hayat, F.; Shah, S.N.A.; ur Rehman, Z.; Bélanger-Gariepy, F. Antimony(III) Dithiocarbamates: Crystal Structures, Supramolecular Aggregations, DNA Binding, Antioxidant and Antileishmanial Activities. Polyhedron 2021, 194, 114909. [Google Scholar] [CrossRef]
- Gielen, M.; Tiekink, E.R.T. Metallotherapeutic Drugs and Metal-Based Diagnostic Agents: The Use of Metals in Medicine; Wiley: Hoboken, NJ, USA, 2005; ISBN 0470864036. [Google Scholar]
- Frézard, F.; Schettini, D.A.; Rocha, O.G.F.; Demicheli, C. Lipossomas: Propriedades Físico-Químicas e Farmacológicas, Aplicações Na Quimioterapia à Base de Antimônio. Quim Nova 2005, 28, 511–518. [Google Scholar] [CrossRef] [Green Version]
- Roberts, W.L.; Mcmurray, W.J.; Rainey, P.M. Characterization of the Antimonial Antileishmanial Agent Meglumine Antimonate (Glucantime). Antimicrob. Agents Chemother. 1998, 42, 1076–1082. [Google Scholar] [CrossRef] [Green Version]
- Sereno, D.; Cavaleyra, M.; Zemzoumi, K.; Maquaire, S.; Ouaissi, A.; Lemesre, J.L. Axenically Grown Amastigotes of Leishmania infantum Used as an In Vitro Model To Investigate the Pentavalent Antimony Mode of Action. Antimicrob. Agents Chemother. 1998, 42, 3097–3102. [Google Scholar] [CrossRef] [Green Version]
- Ouellette, M.; Drummelsmith, J.; Papadopoulou, B. Leishmaniasis: Drugs in the Clinic, Resistance and New Developments. Drug Resist. Updat. 2004, 7, 257–266. [Google Scholar] [CrossRef]
- Ridley, R. The Need for New Approaches to Tropical Disease Drug Discovery and Development for Improved Control Strategies. Drugs Against Parasit. Dis. RD Methodol. Issues 2001, 13, 16–18. [Google Scholar]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, Preparation, and Applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef] [Green Version]
- de Araújo Lopes, S.C.; dos Santos Giuberti, C.; Ribeiro, T.G.; dos Santos Ferreira, D.; Amaral Leite, E.; Cristina, M. Liposomes as Carriers of Anticancer Drugs. In Cancer Treatment—Conventional and Innovative Approaches; InTech: Rijeka, Croatia, 2013. [Google Scholar] [CrossRef] [Green Version]
- de Oliveira Silva, J.; Miranda, S.E.M.; Leite, E.A.; de Paula Sabino, A.; Borges, K.B.G.; Cardoso, V.N.; Cassali, G.D.; Guimarães, A.G.; Oliveira, M.C.; de Barros, A.L.B. Toxicological Study of a New Doxorubicin-Loaded PH-Sensitive Liposome: A Preclinical Approach. Toxicol. Appl. Pharm. 2018, 352, 162–169. [Google Scholar] [CrossRef]
- Ramos, G.S.; Vallejos, V.M.R.; Borges, G.S.M.; Almeida, R.M.; Alves, I.M.; Aguiar, M.M.G.; Fernandes, C.; Guimarães, P.P.G.; Fujiwara, R.T.; Loiseau, P.M.; et al. Formulation of Amphotericin B in PEGylated Liposomes for Improved Treatment of Cutaneous Leishmaniasis by Parenteral and Oral Routes. Pharmaceutics 2022, 14, 989. [Google Scholar] [CrossRef]
- OECD. OECD/OCDE 423 Oecd Guideline for Testing of Chemicals, Acute Oral Toxicity-Acute Toxic Class Method; OECD: Paris, France, 2001. [Google Scholar]
- dos Santos, D.C.M.; de Souza, M.L.S.; Teixeira, E.M.; Alves, L.L.; Vilela, J.M.C.; Andrade, M.; das Carvalho, M.G.; Fernandes, A.P.; Ferreira, L.A.M.; Aguiar, M.M.G. A New Nanoemulsion Formulation Improves Antileishmanial Activity and Reduces Toxicity of Amphotericin B. J. Drug Target 2018, 26, 357–364. [Google Scholar] [CrossRef]
- Loeuillet, C.; Bañuls, A.L.; Hide, M. Study of Leishmania Pathogenesis in Mice: Experimental Considerations. Parasit Vectors 2016, 9, 144. [Google Scholar] [CrossRef] [Green Version]
- Ponte-Sucre, A.; Gamarro, F.; Dujardin, J.-C.; Barrett, M.P.; López-Vélez, R.; García-Hernández, R.; Pountain, A.W.; Mwenechanya, R.; Papadopoulou, B. Drug Resistance and Treatment Failure in Leishmaniasis: A 21st Century Challenge. PLoS Negl. Trop. Dis. 2017, 11, e0006052. [Google Scholar] [CrossRef] [Green Version]
- Maciel, N.R.; Reis, P.G.; Kato, K.C.; Vidal, A.T.; Guimarães, H.N.; Frézard, F.; Silva-Barcellos, N.M.; Grabe-Guimarães, A. Reduced Cardiovascular Alterations of Tartar Emetic Administered in Long-Circulating Liposomes in Rats. Toxicol. Lett. 2010, 199, 234–238. [Google Scholar] [CrossRef] [Green Version]
- Dawidczyk, C.M.; Russell, L.M.; Searson, P.C. Nanomedicines for Cancer Therapy: State-of-the-Art and Limitations to Pre-Clinical Studies That Hinder Future Developments. Front. Chem. 2014, 2, 00069. [Google Scholar] [CrossRef] [Green Version]
- Pereira, M.B.; Sydor, B.G.; Memare, K.G.; Verzignassi Silveira, T.G.; Alessi Aristides, S.M.; Dalmarco, E.M.; Vieira Teixeira, J.J.; Campana Lonardoni, M.V.; Demarchi, I.G. In Vivo Efficacy of Meglumine Antimoniate-Loaded Nanoparticles for Cutaneous Leishmaniasis: A Systematic Review. Nanomedicine 2021, 16, 1505–1518. [Google Scholar] [CrossRef]
- Yang, T.; Cui, F.-D.; Choi, M.-K.; Lin, H.; Chung, S.-J.; Shim, C.-K.; Kim, D.-D. Liposome Formulation of Paclitaxel with Enhanced Solubility and Stability. Drug Deliv. 2007, 14, 301–308. [Google Scholar] [CrossRef]
- Leite, E.A.; dos Santos Giuberti, C.; Wainstein, A.J.A.; Wainstein, A.P.D.L.; Coelho, L.G.V.; Lana, Â.M.Q.; Savassi-Rocha, P.R.; de Oliveira, M.C. Acute Toxicity of Long-Circulating and PH-Sensitive Liposomes Containing Cisplatin in Mice after Intraperitoneal Administration. Life Sci. 2009, 84, 641–649. [Google Scholar] [CrossRef]
- FDA, Food and Drug Administration. Guidance for Industry S9 Nonclinical Evaluation for Anticancer Pharmaceuticals; Center for Drug Evaluation and Research: Rockville, MD, USA, 2010.
- Aoki, H.; Tottori, T.; Sakurai, F.; Fuji, K.; Miyajima, K. Effects of Positive Charge Density on the Liposomal Surface on Disposition Kinetics of Liposomes in Rats. Int. J. Pharm. 1997, 156, 163–174. [Google Scholar] [CrossRef]
- Castro, R.A.O.; Silva-Barcellos, N.M.; Licio, C.S.A.; Souza, J.B.; Souza-Testasicca, M.C.; Ferreira, F.M.; Batista, M.A.; Silveira-Lemos, D.; Moura, S.L.; Frézard, F.; et al. Association of Liposome-Encapsulated Trivalent Antimonial with Ascorbic Acid: An Effective and Safe Strategy in the Treatment of Experimental Visceral Leishmaniasis. PLoS ONE 2014, 9, e104055. [Google Scholar] [CrossRef] [PubMed]
- Gregoriadis, G.; Ryman, B.E. Lysosomal Localization of β-Fructofuranosidase-Containing Liposomes Injected into Rats. Some Implications in the Treatment of Genetic Disorders. Biochem. J. 1972, 129, 123–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azevedo, E.G.; Ribeiro, R.R.; da Silva, S.M.; Ferreira, C.S.; de Souza, L.E.; Ferreira, A.A.; de Oliveira e Castro, R.A.; Demicheli, C.; Rezende, S.A.; Frézard, F. Mixed Formulation of Conventional and Pegylated Liposomes as a Novel Drug Delivery Strategy for Improved Treatment of Visceral Leishmaniasis. Expert Opin. Drug Deliv. 2014, 11, 1551–1560. [Google Scholar] [CrossRef]
- da Silva, S.M.; Amorim, I.F.G.; Ribeiro, R.R.; Azevedo, E.G.; Demicheli, C.; Melo, M.N.; Tafuri, W.L.; Gontijo, N.F.; Michalick, M.S.M.; Frézard, F. Efficacy of Combined Therapy with Liposome-Encapsulated Meglumine Antimoniate and Allopurinol in Treatment of Canine Visceral Leishmaniasis. Antimicrob. Agents Chemother. 2012, 56, 2858–2867. [Google Scholar] [CrossRef] [Green Version]
- Borborema, S.E.T.; Osso Junior, J.A.; de Andrade Junior, H.F.; Nascimento, N. do Biodistribution of Meglumine Antimoniate in Healthy and Leishmania (Leishmania) Infantum Chagasi-Infected BALB/c Mice. Mem. Inst. Oswaldo Cruz 2013, 108, 623–630. [Google Scholar] [CrossRef] [Green Version]
- Carter, K.C.; Baillie, A.J.; Alexander, J.; Dolan, T.F. The Therapeutic Effect of Sodium Stibogluconate in BALB/c Mice Infected with Leishmania donovani Is Organ-Dependent. J. Pharm. Pharmacol. 2011, 40, 370–373. [Google Scholar] [CrossRef]
- Moghimi, S.M.; Parhamifar, L.; Ahmadvand, D.; Wibroe, P.P.; Andresen, T.L.; Farhangrazi, Z.S.; Hunter, A.C. Particulate Systems for Targeting of Macrophages: Basic and Therapeutic Concepts. J. Innate Immun. 2012, 4, 509–528. [Google Scholar] [CrossRef]
- Lukas, G.; Brindle, S.D.; Greengard, P. The Route of Absorption of Intraperitoneally Administered Compounds. J. Pharmacol. Exp. Ther. 1971, 178, 562–564. [Google Scholar]










| Groups | Size (nm) | Polydispersity Index (PDI) | Zeta Potential (mV) | Encapsulation Content (g/L) |
|---|---|---|---|---|
| Lip-ET | 230.0 ± 7.8 | 0.134 ± 0.01 | +17.3 ± 1.3 | 2.34 ± 0.32 |
| Blank-Lip | 163.0 ± 7.7 | 0.076 ± 0.01 | +21.6 ± 1.2 | - |
| Variable | PBS | Lip-ET (16 mg/kg Sb3+) | Blank-Lip | ET (16 mg/kg Sb3+) |
|---|---|---|---|---|
| RBC (106/µL) | 6.58 ± 0.08 | 6.69 ± 0.65 | 6.63 ± 0.12 | 6.82 ± 0.83 |
| Hemoglobin (g/dL) | 12.60 ± 0.26 | 13.12 ± 1.68 | 12.93 ± 0.35 | 14.00 ± 3.62 |
| WBC (103/µL) | 4.17 ± 0.57 | 5.42 ± 1.41 | 5.27 ± 0.80 | 4.37 ± 1.40 |
| Lymphocytes (103/µL) | 1.7 ± 0.5 | 1.8 ± 0.8 | 1.8 ± 0.3 | 1.7 ± 0.6 |
| Granulocytes (%) | 53.6 ± 18.36 | 42.48 ± 10.02 | 43.93 ± 1.83 | 31.35 ± 12.37 |
| Creatinine (mg/dL) | 0.32 ± 0.03 | 0.28 ± 0.07 | 0.36 ± 0.06 | 0.42 ± 0.21 |
| Urea (mg/dL) | 41.32 ± 2.23 | 35.37 ± 9.74 | 39.62 ± 1.11 | 28.44 ± 6.41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coelho, L.D.; Souza, M.M.D.; Cassali, G.D.; Silva, R.A.; Paiva, M.J.N.; Barros, A.L.B.; Teixeira, E.M.; Silveira, J.N.; Coelho, P.M.Z.; Aguiar, M.M.G.; et al. Emetic Tartar-Loaded Liposomes as a New Strategy for Leishmaniasis Treatment. Pharmaceutics 2023, 15, 904. https://doi.org/10.3390/pharmaceutics15030904
Coelho LD, Souza MMD, Cassali GD, Silva RA, Paiva MJN, Barros ALB, Teixeira EM, Silveira JN, Coelho PMZ, Aguiar MMG, et al. Emetic Tartar-Loaded Liposomes as a New Strategy for Leishmaniasis Treatment. Pharmaceutics. 2023; 15(3):904. https://doi.org/10.3390/pharmaceutics15030904
Chicago/Turabian StyleCoelho, Larissa D., Mirna M. D. Souza, Geovanni D. Cassali, Raphaela A. Silva, Maria J. N. Paiva, André L. B. Barros, Eliane M. Teixeira, Josianne N. Silveira, Paulo M. Z. Coelho, Marta M. G. Aguiar, and et al. 2023. "Emetic Tartar-Loaded Liposomes as a New Strategy for Leishmaniasis Treatment" Pharmaceutics 15, no. 3: 904. https://doi.org/10.3390/pharmaceutics15030904