mRNA-Based Nanomedicinal Products to Address Corneal Inflammation by Interleukin-10 Supplementation
Abstract
:1. Introduction
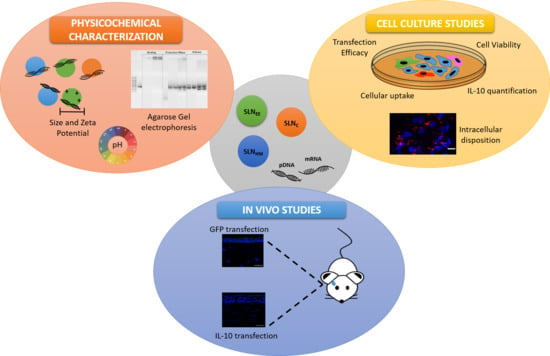
2. Materials and Methods
2.1. Materials
2.2. Formulation of SLNs and Vectors
2.3. Characterization of SLNs and Vectors: Size, Polydispersity Index and ζ-Potential Measurements
2.4. Agarose Gel Electrophoresis Assay
2.5. pH Measurement
2.6. Cell Culture Studies
2.6.1. Transfection Efficacy and Cell Viability
2.6.2. Cellular Uptake
2.6.3. Intracellular Disposition of the Vectors
2.6.4. Quantification of IL-10
2.7. In Vivo Studies
2.7.1. Topical Administration
2.7.2. Evaluation of Gene Expression
2.8. Data Analysis
3. Results
3.1. Size and Zeta Potential of SLNs and Vectors
3.2. Agarose Gel Electrophoresis Assay
3.3. pH Measurement
3.4. Cell Culture Studies
3.4.1. Transfection Efficacy and Cell Viability
3.4.2. Cellular Uptake
3.4.3. Intracellular Disposition of the Vectors
3.4.4. Quantification of IL-10
3.5. In Vivo Studies
3.5.1. In Vivo Transfection with mRNA and pDNA Encoding GFP
3.5.2. In Vivo Transfection with mRNA Encoding Human IL-10
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- del Pozo-Rodríguez, A.; Torrecilla, J.; Rodríguez-Gascón, A.; Solinís, M.Á. Nonviral Delivery Systems for Gene Therapy for Retina and Posterior Segment Disease BT. In Drug Delivery for the Retina and Posterior Segment Disease; Patel, J.K., Sutariya, V., Kanwar, J.R., Pathak, Y.V., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 131–149. ISBN 978-3-319-95807-1. [Google Scholar]
- Trigueros, S.; Domènech, E.B.; Toulis, V.; Marfany, G. In vitro gene delivery in retinal pigment epithelium cells by plasmid dna-wrapped gold nanoparticles. Genes 2019, 10, 289. [Google Scholar] [CrossRef] [PubMed]
- Di Iorio, E.; Barbaro, V.; Alvisi, G.; Trevisan, M.; Ferrari, S.; Masi, G.; Nespeca, P.; Ghassabian, H.; Ponzin, D.; Palù, G. New Frontiers of Corneal Gene Therapy. Hum. Gene Ther. 2019, 30, 923–945. [Google Scholar] [CrossRef] [PubMed]
- Gene Therapy Clinical Trials Worldwide. Provided by Journal of Gene Medicine, John Wileys and Sons LTD. 2021. Available online: https://a873679.fmphost.com/fmi/webd/GTCT (accessed on 31 May 2021).
- Torrecilla, J.; del Pozo-Rodríguez, A.; Vicente-Pascual, M.; Solinís, M.Á.; Rodríguez-Gascón, A. Targeting corneal inflammation by gene therapy: Emerging strategies for keratitis. Exp. Eye Res. 2018, 176, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Beeken, L.J.; Ting, D.S.J.; Sidney, L.E. Potential of mesenchymal stem cells as topical immunomodulatory cell therapies for ocular surface inflammatory disorders. Stem Cells Transl. Med. 2021, 10, 39–49. [Google Scholar] [CrossRef]
- Ghasemi, H.; Ghazanfari, T.; Yaraee, R.; Owlia, P.; Hassan, Z.M.; Faghihzadeh, S. Roles of IL-10 in Ocular Inflammations: A Review. Ocul. Immunol. Inflamm. 2012, 20, 406–418. [Google Scholar] [CrossRef]
- Vicente-Pascual, M.; Albano, A.; Solinís, M.; Serpe, L.; Rodríguez-Gascón, A.; Foglietta, F.; Muntoni, E.; Torrecilla, J.; Pozo-Rodríguez, A.D.; Battaglia, L. Gene delivery in the cornea: In vitro & ex vivo evaluation of solid lipid nanoparticle-based vectors. Nanomedicine 2018, 13, 1847–1864. [Google Scholar] [CrossRef]
- Gómez-Aguado, I.; Rodríguez-Castejón, J.; Vicente-Pascual, M.; Rodríguez-Gascón, A.; Solinís, M.Á.; del Pozo-Rodríguez, A. Nanomedicines to Deliver mRNA: State of the Art and Future Perspectives. Nanomaterials 2020, 10, 364. [Google Scholar] [CrossRef]
- Damase, T.R.; Sukhovershin, R.; Boada, C.; Taraballi, F.; Pettigrew, R.I.; Cooke, J.P. The Limitless Future of RNA Therapeutics. Front. Bioeng. Biotechnol. 2021, 9, 1–24. [Google Scholar] [CrossRef]
- Del Pozo-Rodríguez, A.; Rodríguez-Gascón, A.; Rodríguez-Castejón, J.; Vicente-Pascual, M.; Gómez-Aguado, I.; Battaglia, L.S.; Solinís, M.Á. Gene Therapy. In Advances in Biochemical Engineering/Biotechnology; Springer: Berlin/Heidelberg, Germany, 2019; Volume 171, pp. 321–368. ISBN 978-3-030-40464-2. [Google Scholar]
- May, M. After COVID-19 successes, researchers push to develop mRNA vaccines for other diseases. Nat. Med. 2021, 27, 930–932. [Google Scholar] [CrossRef]
- Igyártó, B.Z.; Jacobsen, S.; Ndeupen, S. Future considerations for the mRNA-lipid nanoparticle vaccine platform. Curr. Opin. Virol. 2021, 48, 65–72. [Google Scholar] [CrossRef]
- Chakraborty, C.; Sharma, A.R.; Bhattacharya, M.; Lee, S.-S. From COVID-19 to Cancer mRNA Vaccines: Moving From Bench to Clinic in the Vaccine Landscape. Front. Immunol. 2021, 12, 1–17. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services; Food and Drug Administration. COVID-19 Vaccines. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-COVID-19/COVID-19-vaccines (accessed on 22 July 2021).
- European Medicines Agency; Science Medicines Health. COVID-19 Vaccines. Available online: https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-COVID-19/treatments-vaccines/COVID-19-vaccines (accessed on 22 July 2021).
- Gediz Erturk, A.; Sahin, A.; Ay, E.B.; Pelit, E.; Bagdatli, E.; Kulu, I.; Gul, M.; Mesci, S.; Eryilmaz, S.; Yildirim, T.; et al. molecules A Multidisciplinary Approach to Coronavirus Disease (COVID-19). Molecules 2021, 26, 3526. [Google Scholar] [CrossRef] [PubMed]
- Paganelli, R.; Frasca, D.; Nisini, R.; Bajaj, V.; Gadi, N.; Spihlman, A.P.; Wu, S.C.; Choi, C.H.; Moulton, V.R. Aging, Immunity, and COVID-19: How Age Influences the Host Immune Response to Coronavirus Infections? Front. Physiol. 2020, 11, 1793. [Google Scholar] [CrossRef]
- del Pozo-Rodríguez, A.; Solinís, M.Á.; Rodríguez-Gascón, A. Applications of lipid nanoparticles in gene therapy. Eur. J. Pharm. Biopharm. 2016, 109, 184–193. [Google Scholar] [CrossRef]
- Wang, Y.; Rajala, A.; Rajala, R.V.S. Lipid Nanoparticles for Ocular Gene Delivery. J. Funct. Biomater. 2015, 6, 379–394. [Google Scholar] [CrossRef]
- Barba, A.A.; Bochicchio, S.; Dalmoro, A.; Lamberti, G. Lipid delivery systems for nucleic-acid-based-drugs: From production to clinical applications. Pharmaceutics 2019, 11, 360. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, W.; Mader, K. Advances in the Cognitive Neuroscience of Neurodevelopmental Disorders: Views from Child Psychiatry and Medical Genetics. Neurodev. Disord. 2020, 47, 165–196. [Google Scholar] [CrossRef]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv. Drug Deliv. Rev. 2002, 54, 131–155. [Google Scholar] [CrossRef]
- Yadav, N.; Khatak, S.; Sara, U.S. Solid lipid nanoparticles—A review. Int. J. Appl. Pharm. 2013, 5, 8–18. [Google Scholar] [CrossRef]
- Ramamoorth, M.; Narvekar, A. Non viral vectors in gene therapy—An overview. J. Clin. Diagn. Res. 2015, 9, GE01–GE06. [Google Scholar] [CrossRef] [PubMed]
- Trucillo, P.; Campardelli, R. Production of solid lipid nanoparticles with a supercritical fluid assisted process. J. Supercrit. Fluids 2019, 143, 16–23. [Google Scholar] [CrossRef]
- Chattopadhyay, P.; Shekunov, B.Y.; Yim, D.; Cipolla, D.; Boyd, B.; Farr, S. Production of solid lipid nanoparticle suspensions using supercritical fluid extraction of emulsions (SFEE) for pulmonary delivery using the AERx system. Adv. Drug Deliv. Rev. 2007, 59, 444–453. [Google Scholar] [CrossRef]
- Singh, M.; Guzman-Aranguez, A.; Hussain, A.; Srinivas, C.S.; Kaur, I.P. Solid lipid nanoparticles for ocular delivery of isoniazid: Evaluation, proof of concept and in vivo safety & kinetics. Nanomedicine 2019, 14, 465–491. [Google Scholar] [CrossRef] [PubMed]
- Mobaraki, M.; Soltani, M.; Harofte, S.Z.; Zoudani, E.L.; Daliri, R.; Aghamirsalim, M.; Raahemifar, K. Biodegradable nanoparticle for cornea drug delivery: Focus review. Pharmaceutics 2020, 12, 1232. [Google Scholar] [CrossRef]
- Battaglia, L.; Serpe, L.; Foglietta, F.; Muntoni, E.; Gallarate, M.; Del Pozo Rodriguez, A.; Solinis, M.A. Application of lipid nanoparticles to ocular drug delivery. Expert Opin. Drug Deliv. 2016, 13, 1743–1757. [Google Scholar] [CrossRef] [PubMed]
- Bachu, R.D.; Chowdhury, P.; Al-Saedi, Z.H.F.; Karla, P.K.; Boddu, S.H.S. Ocular Drug Delivery Barriers—Role of Nanocarriers in the Treatment of Anterior Segment Ocular Diseases. Pharmaceutics 2018, 10, 28. [Google Scholar] [CrossRef]
- Vicente-Pascual, M.; Gómez-Aguado, I.; Rodríguez-Castejón, J.; Rodríguez-Gascón, A.; Muntoni, E.; Battaglia, L.; Del Pozo-Rodríguez, A.; Aspiazu, M.Á.S. Topical Administration of SLN-Based Gene Therapy for the Treatment of Corneal Inflammation by De Novo IL-10 Production. Pharmaceutics 2020, 12, 584. [Google Scholar] [CrossRef]
- Gómez-Aguado, I.; Rodríguez-Castejón, J.; Vicente-Pascual, M.; Rodríguez-Gascón, A.; Del Pozo-Rodríguez, A.; Solinís Aspiazu, M.Á. Nucleic Acid Delivery by Solid Lipid Nanoparticles Containing Switchable Lipids: Plasmid DNA vs. Messenger RNA. Molecules 2020, 25, 5995. [Google Scholar] [CrossRef]
- Sloot, Y.J.E.; Rabold, K.; Ulas, T.; De Graaf, D.M.; Heinhuis, B.; Händler, K.; Schultze, J.L.; Netea, M.G.; Smit, J.W.A.; Joosten, L.A.B.; et al. Interplay between thyroid cancer cells and macrophages: Effects on IL-32 mediated cell death and thyroid cancer cell migration. Cell. Oncol. 2019, 42, 691–703. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.-C.; Tsai, T.-H.; Chang, C.-P.; Chen, S.-F.; Lee, Y.-M.; Shyue, S.-K. Linear correlation between average fluorescence intensity of green fluorescent protein and the multiplicity of infection of recombinant adenovirus. J. Biomed. Sci. 2015, 22, 31. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, K.S.; Al-Rubeai, M. Monitoring of the Adenovirus Production Process by Flow Cytometry. Biotechnol. Prog. 2008, 24, 250–261. [Google Scholar] [CrossRef]
- Xu, X.; Lambrecht, A.D.; Xiao, W. Chapter 13—Yeast Survival and Growth Assays. Methods Mol. Biol. 2014, 1163, 33–44. [Google Scholar] [CrossRef]
- Mahareek, O.; Fahmi, A.; Abdur-Rahman, M.; Shemis, M. Synthesis, Characterization and Optimization of PCL-based Nanocapsules for Delivery of Anticancer Chemotheraputic Drug. J. Sci. Res. Sci. 2019, 36, 412–423. [Google Scholar] [CrossRef]
- Delgado, D.; Del Pozo-Rodríguez, A.; Solinís, M.Á.; Rodríguez-Gascón, A. Understanding the mechanism of protamine in solid lipid nanoparticle-based lipofection: The importance of the entry pathway. Eur. J. Pharm. Biopharm. 2011, 79, 495–502. [Google Scholar] [CrossRef]
- Ruseska, I.; Fresacher, K.; Petschacher, C.; Zimmer, A. Use of protamine in nanopharmaceuticals—A review. Nanomaterials 2021, 11, 1508. [Google Scholar] [CrossRef]
- Delgado, D.; Gascón, A.R.; Del Pozo-Rodríguez, A.; Echevarría, E.; Ruiz De Garibay, A.P.; Rodríguez, J.M.; Solinís, M.Á. Dextran-protamine-solid lipid nanoparticles as a non-viral vector for gene therapy: In vitro characterization and in vivo transfection after intravenous administration to mice. Int. J. Pharm. 2012, 425, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Apaolaza, P.S.; del Pozo-Rodríguez, A.; Torrecilla, J.; Rodríguez-Gascón, A.; Rodríguez, J.M.; Friedrich, U.; Weber, B.H.F.; Solinís, M.A. Solid lipid nanoparticle-based vectors intended for the treatment of X-linked juvenile retinoschisis by gene therapy: In vivo approaches in Rs1h-deficient mouse model. J. Control. Release 2015, 217, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Apaolaza, P.S.; Delgado, D.; Del Pozo-Rodríguez, A.; Gascón, A.R.; Solinís, M.Á. A novel gene therapy vector based on hyaluronic acid and solid lipid nanoparticles for ocular diseases. Int. J. Pharm. 2014, 465, 413–426. [Google Scholar] [CrossRef]
- Omerović, N.; Vranić, E. Application of nanoparticles in ocular drug delivery systems. Health Technol. 2020, 10, 61–78. [Google Scholar] [CrossRef]
- Wong, C.W.; Metselaar, J.M.; Storm, G.; Wong, T.T. A review of the clinical applications of drug delivery systems for the treatment of ocular anterior segment inflammation. Br. J. Ophthalmol. 2020, 1–6. [Google Scholar] [CrossRef]
- Li, J.; Chen, Q.; Zha, Z.; Li, H.; Toh, K.; Dirisala, A.; Matsumoto, Y.; Osada, K.; Kataoka, K.; Ge, Z. Ternary polyplex micelles with PEG shells and intermediate barrier to complexed DNA cores for efficient systemic gene delivery. J. Control. Release 2015, 209, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Al Khafaji, A.S.; Donovan, M.D. Endocytic uptake of solid lipid nanoparticles by the nasal mucosa. Pharmaceutics 2021, 13, 761. [Google Scholar] [CrossRef] [PubMed]
- Manzanares, D.; Ceña, V. Endocytosis: The nanoparticle and submicron nanocompounds gateway into the cell. Pharmaceutics 2020, 12, 371. [Google Scholar] [CrossRef]
- Nagai, N.; Ogata, F.; Otake, H.; Nakazawa, Y.; Kawasaki, N. Energy-dependent endocytosis is responsible for drug transcorneal penetration following the instillation of ophthalmic formulations containing indomethacin nanoparticles. Int. J. Nanomedicine 2019, 14, 1213–1227. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Coradin, T.; Hélary, C. Modulating inflammation in a cutaneous chronic wound model by IL-10 released from collagen-silica nanocomposites: Via gene delivery. Biomater. Sci. 2018, 6, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Reimondez-Troitiño, S.; Csaba, N.; Alonso, M.J.; de la Fuente, M. Nanotherapies for the treatment of ocular diseases. Eur. J. Pharm. Biopharm. 2015, 95, 279–293. [Google Scholar] [CrossRef]
- Dubashynskaya, N.; Poshina, D.; Raik, S.; Urtti, A.; Skorik, Y.A. Polysaccharides in Ocular Drug Delivery. Pharmaceutics 2020, 12, 22. [Google Scholar] [CrossRef]
- Basa, B.; Jakab, G.; Kállai-Szabó, N.; Borbás, B.; Fülöp, V.; Balogh, E.; Antal, I. Evaluation of biodegradable PVA-based 3D printed carriers during dissolution. Materials 2021, 14, 1350. [Google Scholar] [CrossRef]
- Bhattarai, R.S.; Das, A.; Alzhrani, R.M.; Kang, D.; Bhaduri, S.B.; Boddu, S.H.S. Comparison of electrospun and solvent cast polylactic acid (PLA)/poly(vinyl alcohol) (PVA) inserts as potential ocular drug delivery vehicles. Mater. Sci. Eng. C 2017, 77, 895–903. [Google Scholar] [CrossRef]
- Akbari, E.; Imani, R.; Shokrollahi, P.; Heidari keshel, S. Preparation of Nanoparticle-Containing Ring-Implanted Poly(Vinyl Alcohol) Contact Lens for Sustained Release of Hyaluronic Acid. Macromol. Biosci. 2021, 21, 2100043. [Google Scholar] [CrossRef]
- Hao, J.; Wang, X.; Bi, Y.; Teng, Y.; Wang, J.; Li, F.; Li, Q.; Zhang, J.; Guo, F.; Liu, J. Fabrication of a composite system combining solid lipid nanoparticles and thermosensitive hydrogel for challenging ophthalmic drug delivery. Colloids Surfaces B Biointerfaces 2014, 114, 111–120. [Google Scholar] [CrossRef]
- Battaglia, L.; Gallarate, M.; Serpe, L.; Foglietta, F.; Muntoni, E.; del Pozo Rodriguez, A.; Angeles Solinis Aspiazu, M. Ocular delivery of solid lipid nanoparticles. In Lipid Nanocarriers for Drug Targeting; Elsevier: Amsterdam, The Netherlands, 2018; pp. 269–312. ISBN 9780128136874. [Google Scholar]
- Abelson, M.B.; Udell, I.J.; Weston, J.H. Normal Human Tear pH by Direct Measurement. Arch. Ophthalmol. 1981, 99, 301. [Google Scholar] [CrossRef]
- Garcia-Valldecabres, M.; López-Alemany, A.; Refojo, M.F. pH Stability of ophthalmic solutions. Optometry 2004, 75, 161–168. [Google Scholar] [CrossRef]
- Račić, A.; Čalija, B.; Milić, J.; Dukovski, B.J.; Lovrić, J.; Dobričić, V.; Micov, A.; Vuković, M.; Stepanović-Petrović, R.; Krajišnik, D. Formulation of olopatadine hydrochloride viscous eye drops—physicochemical, biopharmaceutical and efficacy assessment using in vitro and in vivo approaches. Eur. J. Pharm. Sci. 2021, 105906. [Google Scholar] [CrossRef]
- Stocum, D.L. Regeneration of Epidermal Structures. Regen. Biol. Med. 2012, 1, 43–65. [Google Scholar] [CrossRef]
- Struve, C.; Krogfelt, K.A. Role of capsule in Klebsiella pneumoniae virulence: Lack of correlation between in vitro and in vivo studies. FEMS Microbiol. Lett. 2003, 218, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Hulsart-Billström, G.; Dawson, J.I.; Hofmann, S.; Müller, R.; Stoddart, M.J.; Alini, M.; Redl, H.; El Haj, A.; Brown, R.; Salih, V.; et al. A surprisingly poor correlation between in vitro and in vivo testing of biomaterials for bone regeneration: Results of a multicentre analysis. Eur. Cells Mater. 2016, 31, 312–322. [Google Scholar] [CrossRef]
- Zheng, Y.F.; Bae, S.H.; Huang, Z.; Chae, S.U.; Jo, S.J.; Shim, H.J.; Lee, C.B.; Kim, D.; Yoo, H.; Bae, S.K. Lack of Correlation between In Vitro and In Vivo Studies on the Inhibitory Effects of (‒)-Sophoranone on CYP2C9 Is Attributable to Low Oral Absorption and Extensive Plasma Protein Binding of (‒)-Sophoranone. Pharmaceutics 2020, 12, 328. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.S.; Watson, A.J.M.; Sheng, H.; Helou, R.; Shao, J.; DuBois, R.N. Celecoxib prevents tumor growth in vivo without toxicity to normal gut: Lack of correlation between in vitro and in vivo models. Cancer Res. 2000, 60, 6045–6051. [Google Scholar]







| Name of the Vector | Weight Ratio |
|---|---|
| mRNA-DX-SLNEE | DX:P:mRNA:SLNEE 1:0.25:1:5 |
| mRNA-HA-SLNEE | HA:P:mRNA:SLNEE 0.5:0.5:1:5 |
| mRNA-DX-SLNHM | DX:P:mRNA:SLNHM 1:0.25:1:5 |
| mRNA-HA-SLNHM | HA:P:mRNA:SLNHM 0.5:0.5:1:5 |
| mRNA-SLNC | P:mRNA:SLNC 2:1:10 |
| mRNA-HA-SLNC | HA:P:mRNA:SLNC 0.5:2:1:10 |
| pDNA-DX-SLNHM | DX:P:pDNA:SLNHM 1:2:1:5 |
| pDNA-HA-SLNHM | HA:P:pDNA:SLNHM 0.5:2:1:5 |
| SLNs | Size (nm) | PDI | ζ-Potential (mV) |
|---|---|---|---|
| SLNEE | 198.7 ± 2.0 | 0.26 ± 0.01 | +57.8 ± 1.7 |
| SLNHM | 93.3 ± 0.4 | 0.28 ± 0.01 | +68.5 ± 0.7 |
| SLNC | 307.8 ± 3.5 | 0.17 ± 0.01 | +21.1 ± 0.8 |
| Size (nm) | PDI | ζ-Potential (mV) | |
|---|---|---|---|
| CleanCapTM EGFP mRNA (5moU) | |||
| mRNA-DX-SLNEE | 241.7 ± 4.8 | 0.29 ± 0.01 | +43.9 ± 0.25 |
| mRNA-HA-SLNEE | 287.2 ± 1.8 | 0.36 ± 0.01 | +37.7 ± 0.3 |
| mRNA-DX-SLNHM | 132.3 ± 1.9 | 0.25 ± 0.01 | +38.0 ± 1.3 |
| mRNA-HA-SLNHM | 132.4 ± 1.6 | 0.20 ± 0.01 | +32.7 ± 0.3 |
| mRNA-SLNC | 292.0 ± 1.2 | 0.17 ± 0.02 | +9.5 ± 0.4 |
| mRNA-HA-SLNC | 348.4 ± 2.9 | 0.26 ± 0.01 | +13.2 ± 0.6 |
| IL-10 mRNA | |||
| mRNA-DX-SLNEE | 180.1 ± 1.1 | 0.21 ± 0.00 | +49.2 ± 0.3 |
| mRNA-HA-SLNEE | 199.4 ± 0.7 | 0.21 ± 0.00 | +46.3 ± 0.1 |
| mRNA-DX-SLNHM | 116.9 ± 0.9 | 0.25 ± 0.00 | +42.1 ± 2.0 |
| mRNA-HA-SLNHM | 121.3 ± 1.0 | 0.24 ± 0.00 | +41.7 ± 0.2 |
| mRNA-SLNC | 242.8 ± 1.7 | 0.25 ± 0.01 | +19.4 ± 0.9 |
| mRNA-HA-SLNC | 283.9 ± 4.6 | 0.26 ± 0.02 | +19.5 ± 1.6 |
| Size (nm) | PDI | ζ-Potential (mV) | |
|---|---|---|---|
| Plasmid pcDNA3-EGFP | |||
| pDNA-DX-SLNHM | 94.5 ± 1.0 | 0.27 ± 0.00 | +43.9 ± 1.01 |
| pDNA-HA-SLNHM | 204.0 ± 2.8 | 0.25 ± 0.01 | +26.3 ± 0.1 |
| Plasmid pUNO1-hIL10 | |||
| pDNA-DX-SLNHM | 101.1 ± 1.1 | 0.27 ± 0.00 | +44.7 ± 0.6 |
| pDNA-HA-SLNHM | 193.7 ± 15.1 | 0.48 ± 0.01 | +41.4 ± 0.2 |
| Sample | pH |
|---|---|
| mRNA-DX-SLNEE | 7.31 ± 0.04 |
| mRNA-HA-SLNEE | 7.20 ± 0.16 |
| mRNA-DX-SLNHM | 7.31 ± 0.04 |
| mRNA-HA-SLNHM | 7.44 ± 0.21 |
| mRNA-SLNC | 7.08 ± 0.29 |
| mRNA-HA-SLNC | 7.13 ± 0.11 |
| pDNA-DX-SLNHM | 7.39 ± 0.06 |
| pDNA-HA-SLNHM | 7.53 ± 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Aguado, I.; Rodríguez-Castejón, J.; Beraza-Millor, M.; Vicente-Pascual, M.; Rodríguez-Gascón, A.; Garelli, S.; Battaglia, L.; del Pozo-Rodríguez, A.; Solinís, M.Á. mRNA-Based Nanomedicinal Products to Address Corneal Inflammation by Interleukin-10 Supplementation. Pharmaceutics 2021, 13, 1472. https://doi.org/10.3390/pharmaceutics13091472
Gómez-Aguado I, Rodríguez-Castejón J, Beraza-Millor M, Vicente-Pascual M, Rodríguez-Gascón A, Garelli S, Battaglia L, del Pozo-Rodríguez A, Solinís MÁ. mRNA-Based Nanomedicinal Products to Address Corneal Inflammation by Interleukin-10 Supplementation. Pharmaceutics. 2021; 13(9):1472. https://doi.org/10.3390/pharmaceutics13091472
Chicago/Turabian StyleGómez-Aguado, Itziar, Julen Rodríguez-Castejón, Marina Beraza-Millor, Mónica Vicente-Pascual, Alicia Rodríguez-Gascón, Sara Garelli, Luigi Battaglia, Ana del Pozo-Rodríguez, and María Ángeles Solinís. 2021. "mRNA-Based Nanomedicinal Products to Address Corneal Inflammation by Interleukin-10 Supplementation" Pharmaceutics 13, no. 9: 1472. https://doi.org/10.3390/pharmaceutics13091472