3.2. Optimization and Characterization of MCZ-Loaded SLMs
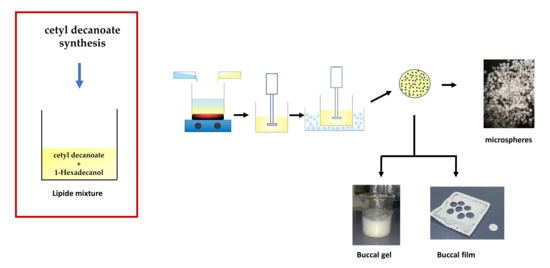
Solid lipid microparticles (SLMs) are lipid-based carriers, which derive from conventional oil-in-water (o/w) emulsions by replacing the liquid oil phase with a solid (at room temperature) lipid component or lipid mix [
13]. Due to their composition, SLMs could be excellent carriers for lipophilic drugs. To design SLMs, the choice of the lipid excipients to be used is crucial as they will affect the properties of the final drug delivery system in terms of both shape, dimension, homogeneity and drug loading capacity. At this point, one of the key factors affecting drug loading ability and drug release kinetics is the lipid’s miscibility in the melted status [
11,
12]. In this work, 1-hexadecanol and cetyl decanoate have been selected as lipid mixture matrices. 1-hexadecanol was chosen as the long-chain aliphatic alcohol having good miscibility with aliphatic esters and, at the same time, self-emulsifying properties [
24]. Moreover, 1-hexadecanol is considered safe and, consequently, is widely used in dermatological products.
As 1-hexadecanol and cetyl decanoate amounts are critical in determining the SLMs characteristics, various ratios were tested, ranging from 10:90 to 90:10 w/w.
Miconazole (MCZ), a potent, lipophilic, antifungal molecule, was chosen as the lipophilic drug model to be conveyed by SLMs. MCZ was homogeneously embedded into the lipid matrix in order to obtain SLMs with the aims of promoting drug entry and accumulation into the epithelial tissues and potentially increase its efficacy for the topical treatment of OC.
In order to maximize the drug content in the SLMs, all attempts to microencapsulation have been performed considering the contribution of 10% in MCZ with respect to the total mass of the drug and lipids. The best results were obtained when combining MCZ:1-hexadecanol:cetyl decanoate in the ratio 10:72:18 w/w.
To prepare SLMs, several methods have been reported in the literature: hot-melt microencapsulation technique, melt emulsification method, solvent emulsification-evaporation method, solvent emulsification-diffusion method, double emulsion (w/o/w) method, sonication method, spray congealing method, supercritical fluid-based method and spray drying method [
25,
26,
27,
28,
29]. In this work, the hot-melt microencapsulation technique was used. The lipophilic drug was dissolved into the melted lipid mix, and the hot clear mixture is emulsified into a pre-warmed water solution. Afterward, the obtained o/w emulsion was poured into an ice bath in order to promote quick solidification of the lipid phase, thus obtaining the SLMs [
11,
13].
The key factors affecting the suitability of the preparation method were the following: the pH of the employed aqueous medium and the rate during the emulsification process.
Generally, MCZ has been successfully entrapped because of its poor aqueous solubility and hence low partitioning into the external aqueous phase during microsphere formation. However, the entrapment amount of MCZ was pH-dependent. As the pH value of the external phase increased, the solubility of MCZ lowered, thus increasing the encapsulated amount of the drug. The maximum DL% value (8 ± 0.5%) was obtained at pH 8.0 (due to Na2CO3). The decrease of the pH value to 7.0 dropped the SLMs drug content below 6%.
The addition of a surfactant was not necessary to obtain spherical particles, probably due to the emulsifying activity of 1-hexadecanol. Furthermore, the insertion of limonene in the aqueous phase, though being immiscible with it, led to the encapsulation of very small amounts of terpene in SLMs, proven by the strong smell emanated by the microparticles when crushed between the fingers. The presence of limonene in SLMs could promote MCZ absorption into mucosal tissues due to its well-known properties as a chemical penetration enhancer [
30].
The main other factor affecting the size distribution was the stirring rate used during the SLMs preparation. A restricted range of dimensional distribution and a high yield percentage value (97.0 ± 0.5% w/w) related to the starting material were obtained at a stirring speed of 800 rpm. All batches produced in such a way resulted as reproducible in terms of particle sizes, indicating that stirring condition, cooling rate and separation process were well controlled. The batches produced by increasing the stirring rate (800–1200 rpm) resulted in a sharp decrease of the average particle size, as well as in the particle recovery yield. Recovery was lower when the particle size was smaller because smaller SLMs could be lost during the filtration process. Accordingly, larger particles were obtained by setting the stirring speed to values less than 800 rpm. However, in these cases, a reduction of the recovery yield was also observed due to lipid material adhesion to the beaker walls during the cooling process.
The obtained optimized MCZ-loaded SLMs were subjected to further characterization in order to evaluate the efficacy of drug encapsulation, as well as their homogeneity in terms of dimension and shape.
To determine the MCZ content, UV-VIS analysis has been performed. The drug loading % (DL%) resulted in 8.0 ± 0.5% (
w/
w) and thus the loading efficacy % (LE%) value was 80 ± 5%. These data confirmed the suitability of the microencapsulation technique, even if a little but acceptable loss in MCZ was observed. The presence of MCZ into the microsphere was also confirmed by the FTIR analysis of MCZ loaded SLMs versus MCZ crystalline pure (
Figure S1).
To evaluate SLMs shape and dimension, morphological analysis has been conducted by optical microscopy (
Figure 5).
As observable, the collected photographs confirmed the presence of spherical microparticles, approximately in the range of 100–200 µm. Moreover, the absence of irregularly shaped particles or crystalline material between the SLMs is evident, suggesting that no crystallization phenomena of MCZ occurred during the cooling step and the formation of the SLMs by the starting hot emulsion. To evaluate the dimensional distribution of the microspheres, two methods were used: sieves and light scattering analyses. The first provided information on the size distribution of the coarse particles and simultaneously enables the separation of the particles according to classes, highlighting the potential presence of non-spherical aggregates of lipid material (
Table 2). The second method provided information on small particles that cannot be measured by sieving (see
Figure S2 in the Supplementary Materials to observe the particle size distribution graph).
Both sieve and light scattering analyses showed that most of the isolated SLMs were of the particle size range 45–310 µm. Light scattering analysis highlights that about 18% of the microparticles ranged from 3 to 45 µm, whereas by sieve analysis, these resulted in 6.7%. This difference in the data is likely due to the method used. Indeed, during sieving, very small particles adhere to the larger ones, thus not falling into the lower sieve. The light scattering analysis, being in dispersion, was not susceptible to this drawback.
These data indicate that the obtained powder is sufficiently homogeneous to handle and workable (e.g., processing, mixing, to be used as intermediate for semisolid or solid formulations) and that the prepared SLMs are small enough to distribute on the tissues well but not too small to be lost during application or even inhaled during handling.
Two other crucial characteristics to be considered and evaluated are the SLMs melting point as well as the physical state of MCZ (amorphous or crystalline). Both these evaluations could be relevant in determining the usefulness of the proposed microparticles and thus the potential enhanced effectiveness of MCZ when embedded into SLMs.
The SLMs melting point could be a key parameter. The melting points of each component of the SLMs and the MCZ-loaded microparticles as a whole are reported in
Table 3.
As observable, the proposed drug-loaded SLMs showed a melting point value compatible with the physiological temperature of the oral cavity. This could lead to SLMs melting when applied strictly in contact with the buccal mucosa and, consequently, the release of MCZ as molecular dispersion. This could lead to an improvement in drug penetration into the mucosal tissue and thus increased effectiveness.
Another relevant parameter to be considered is the physical state of the encapsulated drug. Indeed, the obtainment of the amorphous form is generally preferred in order to promote drug solubility and, as a consequence, absorption/accumulation and efficacy. To evaluate whereas MCZ was amorphous or crystalline when embedded into the SLMs, DSC analyses were conducted.
Figure 6A–C reports the DSC thermograms of every single component of the SLMs by itself. As observable, each raw material is characterized by the presence of an endothermic peak related to its previously reported melting point.
Figure 6D shows the thermogram obtained after physical mixing of all the components in the appropriate and selected ratio. It is possible to highlight that the simple mixing procedure already led to drug-excipient interactions, which allow drug amorphization. Indeed, the two endothermic peaks related to cetyl decanoate and 1-hexadecanol are still present, while the MCZ endothermic peak is missed. This is, obviously, also observable in the SLMs thermogram (
Figure 6E). Moreover, it is important to notice that the ratio between the intensity of the two endothermic peaks related to the excipients reflects their actual ratio in terms of microparticles composition (the enlarged version of
Figure 6 is reported in the
Supplementary Materials).
3.3. Preparation of SLMs-Loaded Buccal Gel and SLMs-Loaded Buccal Film
As the aim of this work was to propose an effective and innovative therapeutic strategy to replace the currently available ones in the treatment of OC while overcoming their relevant limitations, it is important to conceive and design an easily applicable dosage form having good patient compliance. Although SLMs are promising candidates for improving the efficacy of MCZ by enhancing its penetration into the buccal tissue, they consist of a powder, which could result in difficulty to evenly distribute inside the oral cavity, thus being not patient-friendly, leading to the administration of poorly reproducible doses, thus compromising the therapeutic outcomes.
From this view, the prepared MCZ-loaded SLMs were alternatively embedded into a buccal gel and a buccal film in order to obtain easily administrable, comfortable and homogeneous dosage forms.
To prepare the SLMs-loaded gel, hydroxyethylcellulose (HEC), trehalose and PVP-K90 were chosen as excipients in order to obtain a homogenous, transparent and bubble-free gel in which to incorporate MCZ-loaded SLMs. HEC is a gelling and thickening agent derived from cellulose and widely used in the cosmetic and pharmaceutical fields [
31]. Polyvinylpyrrolidone (PVP) is a biocompatible, biodegradable, water-soluble polymer often used to prepare formulations with strong mucoadhesive properties [
32,
33]. Trehalose (α-D-glucopyranosyl-α-D-glucopyranoside) is a nonreducing sugar widely used in food, cosmetics and pharmaceutics for its unique ability to sustain and preserve a wide array of biological molecules due to its functions as a stress protectant, preventing protein degradation and preserving the cell membrane structure under stress conditions [
34]. In addition, new findings suggest that the targeting of the trehalose pathway might compromise fungal viability and virulence in
Cryptococcus neoformans [
35], indicating this sugar as a potential antifungal agent [
36]. Finally, trehalose possesses sweetening properties suitable for diabetic patients, which could improve the palatability of the formulation. To enhance palatability and prevent microbial proliferation, thus extending the expiration date of the formulation, limonene was added to formulations B and D. Moreover, as already reported, limonene is well-known as a chemical penetration enhancer, and thus, it could further improve the effectiveness of the proposed formulation.
MCZ-loaded SLMs were added to the obtained optimized gel (ratio SLMs:gel = 1:8
w/
w). The obtained SLMs-loaded gel (appearance was shown in
Figure S3, see
Supplementary Materials) was evaluated in terms of drug distribution homogeneity in the semisolid mass, resulting in 0.89 ± 0.04% in terms MCZ.
To prepare the SLMs-loaded buccal film (also indicated as microcomposite), firstly, a screening intended to identify the best formulations was performed. Four different film compositions were tested starting from HEC and PVP-K90 as principal excipients and varying in terms of presence/absence of trehalose and limonene as further components. The first formulation screening step consisted of the preparation of empty buccal films (
Table 1, see
Section 2) to be evaluated in terms of appearance and folding endurance. Film A and B were immediately discharged as they were rigid and brittle when subjected to the folding endurance evaluation. On the other hand, films C and D did not show any cracks even after folding more than 300 times. Furthermore, they were transparent, air bubble-free and flexible. This evidence is probably due to the presence of trehalose, which has a high water retention capacity and thus acts as a plasticizer, allowing suitable films with the desired characteristics to be obtained. In view of these encouraging results, two SLMs-loaded buccal films (according to C and D films compositions) have been prepared by the solvent casting method.
The proposed film preparation method is simple, inexpensive and does not imply the use of organic solvents. The method was the most appropriate to obtain microcomposite formulations characterized by a homogenous dispersion of SLMs embedded into the hydrophilic solid matrix system resulting in highly reproducible products. The oven temperature to dry the prepared gel, thus obtaining the final microcomposite, was fixed at 30 °C to avoid SLMs melting, whereas to establish the drying time, preliminary tests were conducted. The best results were obtained after 20 h of drying in an oven. A drying procedure protracted over 28 h leads to brittle and stiff films.
From the obtained formulations, small disks (area 0.5 cm
2) were collected by the careful use of a biopsy punch (
Figure 7) and subsequently used for further studies.
The reproducibility of the films was assessed by measuring the average weight and drug content of three disks obtained from the same batch and repeating this procedure on three different batches. The obtained data are reported in
Table 4.
All data confirmed high product reproducibility, though the microcomposite film D shows slightly better characteristics.
Another relevant parameter to be considered in the design of an effective buccal formulation is the swelling degree. This parameter is related to the ability of the formulation to absorb water from the surrounding environment and swell, thus influencing film bioadhesion and drug release. Indeed, the amount of water absorbed must be the compromise between the development of the interactions through dosage form and mucosal mucins and the increase in the volume of the formulation, which, if excessive, could cause patient discomfort [
37]. Formulations characterized by too high a swelling degree risk being too bulky, causing discomfort for the presence of an extraneous body in the oral cavity. The water uptake of the films was quantified gravimetrically at three different time points (5, 10 and 15 min) by using artificial saliva as the swelling fluid. Data are reported as a swelling degree of the SLMs-loaded buccal films, which resulted in a maximum after 5 min being 7.54 ± 0.91 and 6.70 ± 0.87 for SLMs-loaded film C and SLMs-loaded film D, respectively. After that, no more water was absorbed, and the microcomposite films remained unmodified (
Figure S4).
These results indicate that the microcomposite films, despite the presence of a lipid portion, are able to uptake the environmental fluids and swell, producing a dense layer of gel capable of retaining the SLMs on the target site. A seven or eight-fold weight increase determines a variation in volume that should not be uncomfortable. Additionally, the application of the film could protect the OC lesions from further external insults.
While both films were promising in terms of uniformity and swelling degree, SLMs-loaded film D was chosen as the final formulation to be further characterized, as it contains limonene, which could additionally improve patients’ compliance.
The mucoadhesive properties of a buccal thin layer film are fundamental, as long as they influence the ability of the formulation to be retained on the target site avoiding intraoral detachment and the consequent ingestion. The bioadhesive behavior of a dosage form can be studied by using a wide variety of methods, which are influenced by instrumental variables and experiment design [
38]. Here, the mucoadhesiveness of the proposed buccal film was measured by using an analytical balance modified according to the literature [
16]. Data are expressed as a force of adhesion and detachment force, calculated as reported in the equations described in the
Section 2.2. The force of adhesion and the detachment force of SLMs-loaded film D resulted in 0.1223 ± 0.015 N and 2446.43 ± 53.57 (N/m
2), respectively, confirming suitable mucoadhesive properties.
3.4. MCZ Permeation/Penetration Enhancement Studies: Formulations Comparison
The final proof of concept to evaluate the possible usefulness of the proposed formulations, as well as the actual effectiveness of SLMs to act as penetration and permeation enhancers for a lipophilic drug, such as MCZ, consists in the ex vivo evaluation. To better highlight the potential of the here proposed novel dosage forms, all the preparations (SLMs, buccal gel and buccal film) were compared with a currently available, well-known and widely employed formulation: Daktarin® oral gel, containing 2% of MCZ (w/w).
The ex vivo tests were conducted by using vertical Franz cells and porcine buccal mucosa. However, due to the poor solubility of MCZ in buffer pH 7.4, this cannot be used as a receiving fluid because it will imply the absence of the sink conditions required to observe the permeation phenomenon. To overcome this drawback, 1 mM citric acid solution (pH 3) was used as the acceptor fluid, as it can cause protonation of the imidazole ring (pKa ≈ 6.5) and, therefore, makes MCZ partially water-soluble.
Firstly, MCZ’s ability to cross the buccal membrane was evaluated after administration of Daktarin
® oral gel (80 mg = 1.6 mg of MCZ) and MCZ loaded SLMs (15 mg = 1.2 mg of MCZ). While the amount of MCZ into the acceptor fluid was quantified at different time points until 6 h, at the end of each experiment, the amount of MCZ entrapped into the buccal tissue was also evaluated.
Figure 8 reports the obtained MCZ permeation profile and the amount of MCZ entrapped into the mucosa after six hours of the application of two formulations.
As observable, the encapsulation of MCZ into solid lipid microparticles determines a significant permeation enhancer effect. This is probably due to the ability of the SLMs to melt when kept in contact with the epithelia at 37 °C, fuse with the physiological lipids and penetrate the mucosa entraining the solubilized MCZ. Mucosal entrapment values also indicate that SLMs increase the MCZ capability of partitioning into the mucosal tissue and accumulating.
In particular, the values obtained in terms of MCZ entrapped into the membrane (0.0434 ± 0.0013 and 0.123 ± 0.0037 mg for Daktarin® oral gel and MCZ loaded SLMs, respectively) suggested a high affinity between the SLMs components and the lipids of the epithelium, thus probably producing the “lipidization” of the tissue, which favors MCZ partition resulting in enhanced drug ability to cross the buccal mucosa due to a high concentration gradient between the mucosa and the acceptor fluid.
To better understand the timing of this effect determined by the SLMs as well as to establish if the membrane reach a saturation condition, a set of permeation experiments was performed to evaluate the amount of MCZ entrapped into the buccal mucosa at different time points (from 1 to 6 h).
As reported in
Figure 9, the amount of drug entrapped into the tissue after the administration of 15 mg of SLMs (1.2 mg of MCZ) grows with time until a plateau was reached at 5 h (membrane saturation). The maximum amount of MCZ accumulated was 125 µg (10.4% of the dose).
However, the aim of a topical antifungal treatment for the OC is not to promote drug permeation in systemic circulation but to ensure an optimal therapeutic concentration in the target tissue by administering the dose sufficient to reach it. Indeed, plasma levels of the topically administered drug could cause adverse effects [
39].
As the results obtained suggest the high permeation enhancing effect of SLMs, it should be convenient to reduce the administered dose. In this view, further ex vivo permeation studies were conducted by loading into the donor chamber 2.5 mg of SLMs (corresponding to 0.2 mg of MCZ). At the same time, the behaviors of the two proposed new formulations, the SLMs-loaded buccal gel and the microcomposite buccal film, administered in comparable doses, were analyzed. In particular, the donor compartment of the Franz cell diffusion was filled with 22.5 mg of SLMs-loaded buccal gel (corresponding to 0.2 mg of MCZ) or 12.3 mg of SLMs-loaded film disk D (corresponding to 0.86 mg of MCZ, 8 mm diameter according to Franz cell orifice).
Figure 10 shows the cumulative amount of MCZ permeated after 6 h of experiment both in terms of quantity (mg) and percent of the administered dose.
As observable, the cumulative amount of MCZ (mg) in the acceptor chamber at the end of the experiments (6 h) is approximatively the same when administering Daktarin® gel, 2.5 mg of SLMs or the SLMs-loaded buccal gel. Although, it should be considered that in the case of Daktarin®, the administered dose is eight-fold higher than that contained in 2.5 mg of SLMs or in SLMs-loaded buccal gel (1.6 vs. 0.2 mg). Moreover, when administering the SLMs-loaded buccal film, despite the MCZ dose was 0.86 mg, no drug was found in the acceptor compartment after six hours, highlighting that negligible permeation phenomena occur.
Once again, at the end of the permeation experiments, the amount of MCZ entrapped into the buccal tissue was quantified. Indeed, as already mentioned, the goal of an effective topic drug delivery system to be employed in the treatment of OC is to enhance drug accumulation into the target tissue in order to promote in situ drug effectiveness and, consequently, allow a reduction of the dose to be administered to achieve the therapeutic effect. In
Figure 11, the cumulative amount of MCZ entrapped in the buccal tissue after 6 h of application is reported both as the amount (mg) (panel a) and percentage of the dose (panel b).
These findings highlighted the penetration enhancer effect of the SLMs. The amount (mg) of MCZ entrapped in the buccal mucosa was always higher when it was delivered by the SLMs, compared to Daktarin
® gel. This effect is more evident when data are expressed as a percentage of the administered dose. It is possible to make a quick and easy comparison between SLMs (dose 2.5 mg, blue bars) and SLMs-loaded gel (green bars) as they are characterized by the same MCZ starting amount (0.2 mg). It is likely to notice that the presence of the buccal gel slightly limits the amount of MCZ entrapped in the mucosa, as well as the amount of MCZ permeated (
Figure 11). This is certainly due to the hydrophilic swellable surrounding matrix, which should be crossed by the lipophilic SLMs in order to get in touch with the tissue, melt and promote MCZ accumulation.
Similar behavior is also observed for the SLMs-loaded film, considering the higher dose of MCZ administered. However, it should be noted that the MCZ accumulated in the membrane is consistent, and importantly, it represents approximately 10% of the administered dose. This means that the film is able to release the embedded drug for an extended time, and this could lead to a reduction in the number of daily administrations required.
In any case, the buccal microcomposite film is better than the conventional dosage form, both in the ability to enhance MCZ accumulation in the mucosal tissue and the capability to avoid MCZ bloodstream distribution, which could be potentially unsafe.
Finally, as already mentioned, it is unlikely to propose the administration of free SLMs, and thus, a comparison between the two proposed final formulations (semisolid and solid) must be done. Both of the SLMs-loaded formulations are extremely promising as they are capable of promoting MCZ entry and accumulation into the buccal mucosa, allowing a reduction of the administered dose to achieve the therapeutic effect. Although the results obtained by applying the gel may seem better than those obtained by the film, the advantages of the solid dosage form should be considered. Indeed, a solid dosage form is more stable, easily administrable and patient-friendly compared to a semisolid one. Moreover, the proposed buccal film highlighted no drug permeation, and thus, no MCZ should be lost in the systemic circulation, and no systemic side effects should occur. Finally, a semisolid dosage form could be partially lost by swallowing (thus, consequently, allowing drug loss), remaining, generally, in situ for a shorter period of time than the solid one. This is particularly true when further considering that the proposed buccal film was accurately designed to be mucoadhesive.