Improvement of Pulmonary Photodynamic Therapy: Nebulisation of Curcumin-Loaded Tetraether Liposomes
Abstract
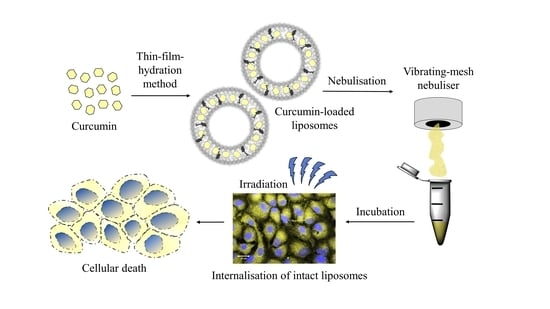
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Cell Culture
2.3. Irradiation Device
2.4. Preparation of Liposomes
2.5. Lyophilisation
2.6. Nebulisation, Aerosol Output and Emitted Volume
2.7. Dynamic Light Scattering and Laser Doppler Anemometry
2.8. Encapsulation Efficiency and Loading Capacity
2.9. Atomic Force Microscopy
2.10. Transmission Electron Microscopy
2.11. Aerodynamic Properties
2.12. Mucous Membrane Compatibility
2.13. In Vitro Cytotoxicity
2.14. Cellular Uptake Studies
2.15. Confocal Laser Scanning Microscopy (CLSM)
2.16. Cellular Migration
2.17. Statistical Analysis
3. Results and Discussion
3.1. Suitability of Nebulisers
3.2. Physicochemical Properties of the Liposomal Formulations
3.3. AFM Visualisation
3.4. TEM Visualisation
3.5. Aerodynamic Properties
3.6. Mucous Membrane Compatibility
3.7. In Vitro Cytotoxicity, Cellular Uptake and Migration
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Health Observatory; World Health Organization: Geneva, Switzerland, 2018; Available online: https://who.int/gho/database/en/ (accessed on 3 August 2019).
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Planchard, D.; Popat, S.; Kerr, K.; Novello, S.; Smit, E.; Faivre-Finn, C.; Mok, T.; Reck, M.; Van Schil, P.; Hellmann, M.; et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2018, 29, iv192–iv237. [Google Scholar] [CrossRef]
- Postmus, P.E.; Kerr, K.M.; Oudkerk, M.; Senan, S.; Waller, D.A.; Vansteenkiste, J.; Escriu, C.; Peters, S. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv1–iv21. [Google Scholar] [CrossRef] [PubMed]
- Forde, P.M.; Chaft, J.E.; Smith, K.N.; Anagnostou, V.; Cottrell, T.R.; Hellmann, M.D.; Zahurak, M.; Yang, S.C.; Jones, D.R.; Broderick, S.; et al. Neoadjuvant PD-1 Blockade in Resectable Lung Cancer. N. Engl. J. Med. 2018, 378, 1976–1986. [Google Scholar] [CrossRef]
- Preis, E.; Anders, T.; Širc, J.; Hobzova, R.; Cocarta, A.-I.; Bakowsky, U.; Jedelská, J. Biocompatible indocyanine green loaded PLA nanofibers for in situ antimicrobial photodynamic therapy. Mater. Sci. Eng. C 2020, 115, 111068. [Google Scholar] [CrossRef]
- Raschpichler, M.; Agel, M.R.; Pinnapireddy, S.R.; Duse, L.; Baghdan, E.; Schäfer, J.; Bakowsky, U. In situ intravenous photodynamic therapy for the systemic eradication of blood stream infections. Photochem. Photobiol. Sci. 2018, 18, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, T.J.; Gomer, C.J.; Henderson, B.W.; Jori, G.; Kessel, D.; Korbelik, M.; Moan, J.; Peng, Q. Photodynamic therapy. J. Natl. Cancer Inst. 1998, 90, 889–905. [Google Scholar] [CrossRef] [Green Version]
- Plenagl, N.; Seitz, B.S.; Pinnapireddy, S.R.; Jedelská, J.; Brüßler, J.; Bakowsky, U. Hypericin Loaded Liposomes for Anti-Microbial Photodynamic Therapy of Gram-Positive Bacteria. Phys. Status Solidi A 2018, 215. [Google Scholar] [CrossRef]
- Moan, J.; Berg, K. The photodegradation of porphyrins in cells can be used to estimate the lifetime of singlet oxygen. Photochem. Photobiol. 1991, 53, 549–553. [Google Scholar] [CrossRef]
- Dolmans, D.E.; Fukumura, D.; Jain, R.K. Photodynamic therapy for cancer. Nat. Rev. Cancer 2003, 3, 380–387. [Google Scholar] [CrossRef]
- Banerjee, S.; Dixit, A.; Karande, A.A.; Chakravarty, A.R. Remarkable Selectivity and Photo-Cytotoxicity of an Oxidovanadium(IV) Complex of Curcumin in Visible Light. Eur. J. Inorg. Chem. 2014, 2015, 447–457. [Google Scholar] [CrossRef]
- Juarranz, A.; Jaén, P.; Sanz-Rodríguez, F.; Cuevas, J.; González, S. Photodynamic therapy of cancer. Basic principles and applications. Clin. Transl. Oncol. 2008, 10, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Duse, L.; Agel, M.R.; Pinnapireddy, S.R.; Schäfer, J.; Selo, M.A.; Ehrhardt, C.; Bakowsky, U. Photodynamic Therapy of Ovarian Carcinoma Cells with Curcumin-Loaded Biodegradable Polymeric Nanoparticles. Pharmaceutics 2019, 11, 282. [Google Scholar] [CrossRef] [Green Version]
- Konopka, K.; Goslinski, T. Photodynamic Therapy in Dentistry. J. Dent. Res. 2007, 86, 694–707. [Google Scholar] [CrossRef]
- Brancaleon, L.; Moseley, H. Laser and Non-laser Light Sources for Photodynamic Therapy. Lasers Med Sci. 2002, 17, 173–186. [Google Scholar] [CrossRef]
- Baghdan, E.; Duse, L.; Schüer, J.J.; Pinnapireddy, S.R.; Pourasghar, M.; Schäfer, J.; Schneider, M.; Bakowsky, U. Development of inhalable curcumin loaded Nano-in-Microparticles for bronchoscopic photodynamic therapy. Eur. J. Pharm. Sci. 2019, 132, 63–71. [Google Scholar] [CrossRef]
- Agel, M.R.; Baghdan, E.; Pinnapireddy, S.R.; Lehmann, J.; Schäfer, J.; Bakowsky, U. Curcumin loaded nanoparticles as efficient photoactive formulations against gram-positive and gram-negative bacteria. Colloids Surf. B Biointerfaces 2019, 178, 460–468. [Google Scholar] [CrossRef]
- Duse, L.; Baghdan, E.; Pinnapireddy, S.R.; Engelhardt, K.H.; Jedelská, J.; Schaefer, J.; Quendt, P.; Bakowsky, U. Preparation and Characterization of Curcumin Loaded Chitosan Nanoparticles for Photodynamic Therapy. Phys. Status Solidi A 2017, 215. [Google Scholar] [CrossRef]
- Shishodia, S.; Sethi, G.; Aggarwal, B.B. Curcumin: Getting Back to the Roots. Ann. N.Y. Acad. Sci. 2005, 1056, 206–217. [Google Scholar] [CrossRef] [Green Version]
- Epstein, J.; Sanderson, I.; Macdonald, T.T. Curcumin as a therapeutic agent: The evidence fromin vitro, animal and human studies. Br. J. Nutr. 2010, 103, 1545–1557. [Google Scholar] [CrossRef] [Green Version]
- Naksuriya, O.; Okonogi, S.; Schiffelers, R.; Hennink, W.E. Curcumin nanoformulations: A review of pharmaceutical properties and preclinical studies and clinical data related to cancer treatment. Biomaterials 2014, 35, 3365–3383. [Google Scholar] [CrossRef]
- Wilken, R.; Veena, M.S.; Wang, M.B.; Srivatsan, E.S. Curcumin: A review of anti-cancer properties and therapeutic activity in head and neck squamous cell carcinoma. Mol. Cancer 2011, 10, 12. [Google Scholar] [CrossRef] [Green Version]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of Curcumin: Problems and Promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef] [PubMed]
- Kaminaga, Y.; Nagatsu, A.; Akiyama, T.; Sugimoto, N.; Yamazaki, T.; Maitani, T.; Mizukami, H. Production of unnatural glucosides of curcumin with drastically enhanced water solubility by cell suspension cultures of Catharanthus roseus. FEBS Lett. 2003, 555, 311–316. [Google Scholar] [CrossRef] [Green Version]
- Duse, L.; Pinnapireddy, S.R.; Strehlow, B.; Jedelská, J.; Bakowsky, U. Low level LED photodynamic therapy using curcumin loaded tetraether liposomes. Eur. J. Pharm. Biopharm. 2018, 126, 233–241. [Google Scholar] [CrossRef]
- Kunwar, A.; Barik, A.; Pandey, R.; Priyadarsini, K.I. Transport of liposomal and albumin loaded curcumin to living cells: An absorption and fluorescence spectroscopic study. Biochim. Biophys. Acta Gen. Subj. 2006, 1760, 1513–1520. [Google Scholar] [CrossRef] [PubMed]
- Melis, V.; Manca, M.L.; Bullita, E.; Tamburini, E.; Castangia, I.; Cardia, M.C.; Valenti, D.; Fadda, A.M.; Peris, J.E.; Manconi, M. Inhalable polymer-glycerosomes as safe and effective carriers for rifampicin delivery to the lungs. Colloids Surf. B Biointerfaces 2016, 143, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Manca, M.L.; Peris, J.E.; Melis, V.; Valenti, D.; Cardia, M.C.; Lattuada, D.; Escribano-Ferrer, E.; Fadda, A.M.; Manconi, M. Nanoincorporation of curcumin in polymer-glycerosomes and evaluation of their in vitro–in vivo suitability as pulmonary delivery systems. RSC Adv. 2015, 5, 105149–105159. [Google Scholar] [CrossRef]
- Preis, E.; Baghdan, E.; Agel, M.R.; Anders, T.; Pourasghar, M.; Schneider, M.; Bakowsky, U. Spray dried curcumin loaded nanoparticles for antimicrobial photodynamic therapy. Eur. J. Pharm. Biopharm. 2019, 142, 531–539. [Google Scholar] [CrossRef]
- Engelhardt, K.H.; Pinnapireddy, S.R.; Baghdan, E.; Jedelská, J.; Bakowsky, U. Transfection Studies with Colloidal Systems Containing Highly Purified Bipolar Tetraether Lipids from Sulfolobus acidocaldarius. Archaea 2017, 2017, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Khan, T.K.; Chong, P.L.-G. Studies of Archaebacterial Bipolar Tetraether Liposomes by Perylene Fluorescence. Biophys. J. 2000, 78, 1390–1399. [Google Scholar] [CrossRef] [Green Version]
- Sitterberg, J.; Özcetin, A.; Ehrhardt, C.; Bakowsky, U. Utilising atomic force microscopy for the characterisation of nanoscale drug delivery systems. Eur. J. Pharm. Biopharm. 2010, 74, 2–13. [Google Scholar] [CrossRef]
- Baghdan, E.; Pinnapireddy, S.R.; Vögeling, H.; Schäfer, J.; Eckert, A.W.; Bakowsky, U. Nano spray drying: A novel technique to prepare well-defined surface coatings for medical implants. J. Drug Deliv. Sci. Technol. 2018, 48, 145–151. [Google Scholar] [CrossRef]
- Luepke, N.; Kemper, F. The HET-CAM test: An alternative to the draize eye test. Food Chem. Toxicol. 1986, 24, 495–496. [Google Scholar] [CrossRef]
- Schüller, M. Entwicklung Eines Geeigneten Modells zur Untersuchung des selektinvermittelten Zellrollens: Das Chorioallantoismembran (CAM)-Modell; Universitäts- und Landesbibliothek Sachsen-Anhalt: Halle, Germany, 2005. [Google Scholar]
- Goergen, N.; Wojcik, M.; Drescher, S.; Pinnapireddy, S.R.; Brüßler, J.; Bakowsky, U.; Jedelská, J. The Use of Artificial Gel Forming Bolalipids as Novel Formulations in Antimicrobial and Antifungal Therapy. Pharmaceutics 2019, 11, 307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Centre for the Validation of Alternative Methods. HET-CAM Test INVITTOX n°47: ECVAM DB-ALM: INVITTOX Protocol; European Centre for the Validation of Alternative Methods: Ispra, Italy, 1992. [Google Scholar]
- Nimmano, N.; Somavarapu, S.; Taylor, K.M. Aerosol characterisation of nebulised liposomes co-loaded with erlotinib and genistein using an abbreviated cascade impactor method. Int. J. Pharm. 2018, 542, 8–17. [Google Scholar] [CrossRef]
- Elhissi, A.M.; Giebultowicz, J.; Stec, A.A.; Wroczyński, P.; Ahmed, W.; Alhnan, M.A.; Phoenix, D.; Taylor, K.M. Nebulization of ultradeformable liposomes: The influence of aerosolization mechanism and formulation excipients. Int. J. Pharm. 2012, 436, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Beck-Broichsitter, M.; Oesterheld, N.; Knuedeler, M.-C.; Seeger, W.; Schmehl, T. On the correlation of output rate and aerodynamic characteristics in vibrating-mesh-based aqueous aerosol delivery. Int. J. Pharm. 2014, 461, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Sang, C.H.; Lin, S.C.; Chen, H.F.; Tseng, H.H.; Lo, H.H. Performance of a New Polymer-Based Vibrating Mesh Nebulizer: A Comparison to Metal-Based Mesh Nebulizer. Presented at Drug Delivery to the Lungs 2018, Edinburgh, Scotland, 12–14 December 2018. [Google Scholar]
- Beck-Broichsitter, M.; Knuedeler, M.-C.; Seeger, W.; Schmehl, T. Controlling the droplet size of formulations nebulized by vibrating-membrane technology. Eur. J. Pharm. Biopharm. 2014, 87, 524–529. [Google Scholar] [CrossRef]
- Manconi, M.; Manca, M.L.; Valenti, D.; Escribano, E.; Hillaireau, H.; Fadda, A.M.; Fattal, E. Chitosan and hyaluronan coated liposomes for pulmonary administration of curcumin. Int. J. Pharm. 2017, 525, 203–210. [Google Scholar] [CrossRef]
- Pritchard, J.N.; Hatley, R.H.; Denyer, J.; Von Hollen, D. Mesh nebulizers have become the first choice for new nebulized pharmaceutical drug developments. Ther. Deliv. 2018, 9, 121–136. [Google Scholar] [CrossRef] [Green Version]
- Taylor, K.; Taylor, G.; Kellaway, I.; Stevens, J. The stability of liposomes to nebulisation. Int. J. Pharm. 1990, 58, 57–61. [Google Scholar] [CrossRef]
- Singh, A.; Bhatia, S.; Rana, V. Inhalable Nanostructures for Lung Cancer Treatment: Progress and Challenges. Curr. Nanomed. 2019, 9, 4–29. [Google Scholar] [CrossRef]
- Abdelaziz, H.M.; Freag, M.S.; Elzoghby, A.O. Solid Lipid Nanoparticle-Based Drug Delivery for Lung Cancer. In Nanotechnology-Based Targeted Drug Delivery Systems for Lung Cancer; Elsevier: Amsterdam, The Netherlands, 2019; pp. 95–121. [Google Scholar]
- Sánchez-López, E.; Guerra, M.; Dias-Ferreira, J.; Lopez-Machado, A.; Ettcheto, M.; Cano, A.; Espina, M.; Camins, A.; Garcia, M.L.; Souto, E.B. Current Applications of Nanoemulsions in Cancer Therapeutics. Nanomaterials 2019, 9, 821. [Google Scholar] [CrossRef] [Green Version]
- Akhter, S.; Ahmad, J.; Rizwanullah, M.; Rahman, M.; Ahmad, M.Z.; Alam Rizvi, M.; Ahmad, F.J.; Amin, S.; Kamal, M.A. Nanotechnology-based inhalation treatments for lung cancer: State of the art. Nanotechnol. Sci. Appl. 2015, 8, 55–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, X.; Wang, N.; Yang, L.-Y.; Ouyang, X.-K.; Huang, F. Folic Acid and PEI Modified Mesoporous Silica for Targeted Delivery of Curcumin. Pharmceutics 2019, 11, 430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bulbake, U.; Doppalapudi, S.; Kommineni, N.; Khan, W. Liposomal Formulations in Clinical Use: An Updated Review. Pharmaceutics 2017, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Rudokas, M.; Najlah, M.; A Alhnan, M.; Elhissi, A. Liposome Delivery Systems for Inhalation: A Critical Review Highlighting Formulation Issues and Anticancer Applications. Med. Princ. Pr. 2016, 25, 60–72. [Google Scholar] [CrossRef] [PubMed]
- Bagatolli, L.; Gratton, E.; Khan, T.K.; Chong, P.L.-G. Two-Photon Fluorescence Microscopy Studies of Bipolar Tetraether Giant Liposomes from Thermoacidophilic Archaebacteria Sulfolobus acidocaldarius. Biophys. J. 2000, 79, 416–425. [Google Scholar] [CrossRef] [Green Version]
- Niven, R.W.; Schreier, H. Nebulization of Liposomes. I. Effects of Lipid Composition. Pharm. Res. 1990, 7, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, H.; Sun, J.; Gao, J.; Liu, W.; Li, B.; Guo, Y.; Chen, J. DC-Chol/DOPE cationic liposomes: A comparative study of the influence factors on plasmid pDNA and siRNA gene delivery. Int. J. Pharm. 2010, 390, 198–207. [Google Scholar] [CrossRef]
- Yang, S.; Chen, J.; Zhao, D.; Han, D.; Chen, X. Comparative study on preparative methods of DC-Chol/DOPE liposomes and formulation optimization by determining encapsulation efficiency. Int. J. Pharm. 2012, 434, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Beck-Broichsitter, M.; Knuedeler, M.-C.; Oesterheld, N.; Seeger, W.; Schmehl, T. Boosting the aerodynamic properties of vibrating-mesh nebulized polymeric nanosuspensions. Int. J. Pharm. 2014, 459, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Zaru, M.; Mourtas, S.; Klepetsanis, P.; Fadda, A.M.; Antimisiaris, S.G. Liposomes for drug delivery to the lungs by nebulization. Eur. J. Pharm. Biopharm. 2007, 67, 655–666. [Google Scholar] [CrossRef]
- Wolfe, J.; Bryant, G. Freezing, Drying, and/or Vitrification of Membrane–Solute–Water Systems. Cryobiology 1999, 39, 103–129. [Google Scholar] [CrossRef] [Green Version]
- Darwis, Y.; Kellaway, I. Nebulisation of rehydrated freeze-dried beclomethasone dipropionate liposomes. Int. J. Pharm. 2001, 215, 113–121. [Google Scholar] [CrossRef]
- Mahmoud, G.; Jedelská, J.; Strehlow, B.; Bakowsky, U. Bipolar tetraether lipids derived from thermoacidophilic archaeon Sulfolobus acidocaldarius for membrane stabilization of chlorin e6 based liposomes for photodynamic therapy. Eur. J. Pharm. Biopharm. 2015, 95, 88–98. [Google Scholar] [CrossRef]
- Chang, E. Unusual Thermal Stability of Liposomes Made from Bipolar Tetraether Lipids. Biochem. Biophys. Res. Commun. 1994, 202, 673–679. [Google Scholar] [CrossRef]
- Freisleben, H.-J. The Main (Glyco) Phospholipid (MPL) of Thermoplasma acidophilum. Int. J. Mol. Sci. 2019, 20, 5217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghazanfari, T.; Elhissi, A.M.; Ding, Z.; Taylor, K.M. The influence of fluid physicochemical properties on vibrating-mesh nebulization. Int. J. Pharm. 2007, 339, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Dailey, L.A.; Schmehl, T.; Gessler, T.; Wittmar, M.; Grimminger, F.; Seeger, W.; Kissel, T. Nebulization of biodegradable nanoparticles: Impact of nebulizer technology and nanoparticle characteristics on aerosol features. J. Control. Release 2003, 86, 131–144. [Google Scholar] [CrossRef]
- Olszewski, O.Z.; MacLoughlin, R.; Blake, A.; O’Neill, M.; Mathewson, A.; Jackson, N. A Silicon-based MEMS Vibrating Mesh Nebulizer for Inhaled Drug Delivery. Procedia Eng. 2016, 168, 1521–1524. [Google Scholar] [CrossRef]
- Nikander, K.; Von Hollen, D.; Larhrib, H. The size and behavior of the human upper airway during inhalation of aerosols. Expert Opin. Drug Deliv. 2016, 14, 621–630. [Google Scholar] [CrossRef]
- Mitra, K.; Basu, U.; Khan, I.; Maity, B.; Kondaiah, P.; Chakravarty, A.R. Remarkable anticancer activity of ferrocenyl-terpyridine platinum(ii) complexes in visible light with low dark toxicity. Dalton Trans. 2014, 43, 751–763. [Google Scholar] [CrossRef] [PubMed]
- Pillai, G.R.; Srivastava, A.S.; I Hassanein, T.; Chauhan, D.P.; Carrier, E. Induction of apoptosis in human lung cancer cells by curcumin. Cancer Lett. 2004, 208, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.-H.; Hang, L.-W.; Yang, J.-S.; Chen, H.-Y.; Lin, H.-Y.; Chiang, J.-H.; Lu, C.-C.; Yang, J.-L.; Lai, T.-Y.; Ko, Y.-C.; et al. Curcumin induces apoptosis in human non-small cell lung cancer NCI-H460 cells through ER stress and caspase cascade- and mitochondria-dependent pathways. Anticancer Res. 2010, 30, 2125–2133. [Google Scholar]
- Torchilin, V.P. Recent advances with liposomes as pharmaceutical carriers. Nat. Rev. Drug Discov. 2005, 4, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Schifter, C.-R. Untersuchungen zum Einfluss der Größe von Liposomen auf deren Endozytose in verschiedenen Zelllinien. Ph.D. Thesis, Universität Freiburg, Freiburg, Germany, 2008. [Google Scholar]
- Fux, C.; Costerton, J.; Stewart, P.; Stoodley, P. Survival strategies of infectious biofilms. Trends Microbiol. 2005, 13, 34–40. [Google Scholar] [CrossRef]
- Liang, C.-C.; Park, A.Y.; Guan, J.-L. In vitro scratch assay: A convenient and inexpensive method for analysis of cell migration in vitro. Nat. Protoc. 2007, 2, 329–333. [Google Scholar] [CrossRef] [Green Version]
- Lin, S.-S.; Lai, K.-C.; Hsu, S.-C.; Yang, J.-S.; Kuo, C.-L.; Lin, J.-P.; Ma, Y.-S.; Wu, C.-C.; Chung, J.-G. Curcumin inhibits the migration and invasion of human A549 lung cancer cells through the inhibition of matrix metalloproteinase-2 and -9 and Vascular Endothelial Growth Factor (VEGF). Cancer Lett. 2009, 285, 127–133. [Google Scholar] [CrossRef]








| Abbreviations | Formulation | Molar Ratio (%) |
|---|---|---|
| DT | DPPC:TEL | 90:10 |
| DC DD | DPPC:Chol DPPC:DOPE | 70:30 75:25 |
| Lipid Compositions | Size (nm) ± SD | PdI 1 ± SD | ζ-Potential (mV) ± SD | |
|---|---|---|---|---|
| DT | 129.7 ± 3.2 | 0.19 ± 0.08 | −13.53 ± 2.42 | |
| CUR-liposomes | DC DD | 109.4 ± 2.4 94.4 ± 5.9 | 0.14 ± 0.09 0.26 ± 0.11 | −5.61 ± 0.79 −2.97 ± 0.81 |
| Nebulised (PARI VELOX®) CUR-liposomes | DT DC DD | 131.1 ± 3.0 116.4 ± 3.2 99.1 ± 5.2 | 0.21 ± 0.06 0.18 ± 0.07 0.30 ± 0.09 | −16.33 ± 1.95 −3.74 ± 0.64 −2.86 ± 0.59 |
| Nebulised (PARI BOY® SX) CUR-liposomes | DT DC DD | 129.5 ± 2.8 113.3 ± 3.5 100.7 ± 4.7 | 0.20 ± 0.08 0.21 ± 0.09 0.32 ± 0.08 | −15.54 ± 2.13 −5.13 ± 0.92 −3.11 ± 0.76 |
| Lyophilised & nebulised (VELOX®) CUR-liposomes | DT DC DD | 149.6 ± 4.1 127.7 ± 4.8 132.1 ± 5.1 | 0.46 ± 0.10 0.47 ± 0.13 0.57 ± 0.13 | −37.89 ± 4.43 −11.47 ± 2.38 −9.62 ± 2.09 |
| Lipid Compositions | EE (%) ± SD | LC (%) ± SD | |
|---|---|---|---|
| DT | 93.9 ± 8.2 | 1.9 ± 0.1 | |
| CUR-liposomes | DC DD | 88.4 ± 12.4 85.1 ± 15.9 | 1.7 ± 0.1 1.7 ± 0.1 |
| Nebulised (PARI VELOX®) CUR-liposomes | DT DC DD | 80.0 ± 12.8 62.5 ± 12.3 57.5 ± 16.6 | 1.6 ± 0.1 1.3 ± 0.1 1.2 ± 0.1 |
| Lyophilised and nebulised (VELOX®) CUR-liposomes | DT DC DD | 74.6 ± 10.9 60.3 ± 9.5 31.2 ± 11.7 | 1.5 ± 0.1 1.2 ± 0.1 0.6 ± 0.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lehmann, J.; Agel, M.R.; Engelhardt, K.H.; Pinnapireddy, S.R.; Agel, S.; Duse, L.; Preis, E.; Wojcik, M.; Bakowsky, U. Improvement of Pulmonary Photodynamic Therapy: Nebulisation of Curcumin-Loaded Tetraether Liposomes. Pharmaceutics 2021, 13, 1243. https://doi.org/10.3390/pharmaceutics13081243
Lehmann J, Agel MR, Engelhardt KH, Pinnapireddy SR, Agel S, Duse L, Preis E, Wojcik M, Bakowsky U. Improvement of Pulmonary Photodynamic Therapy: Nebulisation of Curcumin-Loaded Tetraether Liposomes. Pharmaceutics. 2021; 13(8):1243. https://doi.org/10.3390/pharmaceutics13081243
Chicago/Turabian StyleLehmann, Jennifer, Michael R. Agel, Konrad H. Engelhardt, Shashank R. Pinnapireddy, Sabine Agel, Lili Duse, Eduard Preis, Matthias Wojcik, and Udo Bakowsky. 2021. "Improvement of Pulmonary Photodynamic Therapy: Nebulisation of Curcumin-Loaded Tetraether Liposomes" Pharmaceutics 13, no. 8: 1243. https://doi.org/10.3390/pharmaceutics13081243