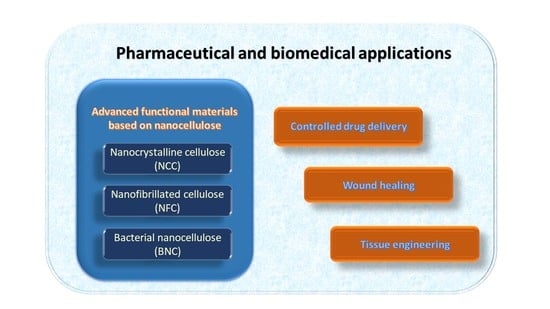
Advanced Functional Materials Based on Nanocellulose for Pharmaceutical/Medical Applications
Abstract
:1. Introduction
2. Advanced Functional Materials Based on Nanocellulose—General Characteristics
2.1. Hydrogels
2.2. Nanogels
2.3. Nanocomposites
2.3.1. Nanocellulose Materials as “Reinforcing Agents” into Polymer Matrices
2.3.2. Nanocellulose Materials as “Matrices” for Different Reinforcing Agents
3. Nanocellulose-Based Materials in Pharmaceutical/Medical Applications
3.1. Nanocellulose-Based Materials in Drug-Delivery Systems (DDS)
3.1.1. CNC-Based Materials in Drug-Delivery Systems
3.1.2. BNC-Based Materials in Drug-Delivery Systems
3.2. Nanocellulose-Based Materials in Wound-Healing Applications
3.2.1. CNC-Based Materials in Wound-Dressing Applications
3.2.2. NFC-Based Materials in Wound-Dressing Applications
3.2.3. BNC-Based Materials in Wound-Dressing Applications
3.3. Nanocellulose-Based Materials in Tissue Engineering Applications
3.3.1. Nanocellulose-Based Materials as Scaffolds in Skin Tissue Engineering
3.3.2. Nanocellulose-Based Materials as Scaffolds in Bone Tissue Engineering
3.3.3. Nanocellulose-Based Materials as Scaffolds in Vascular and Cardiac Tissue Engineering
3.3.4. Nanocellulose-Based Materials as Scaffolds in Cartilage Tissue Engineering
3.3.5. Nanocellulose-Based Materials as Scaffolds in Soft Tissue Engineering
4. Toxicological Evaluation and Potential Limitations of NCs-Based Materials
4.1. Toxicological Evaluation of NC-Based Materials
4.1.1. In Vitro Cytotoxicity Analysis
| Material | Cellulose Source | Toxicological Experiment | Cells Lines | Toxicological Results | Results and Possible Application | Ref. |
|---|---|---|---|---|---|---|
| CNC | ||||||
| CNC | Cotton (Whatman 1 filter paper) | MTS assay; ATP assay. | BEAS 2B hMDMs | Cytotoxicity at 100 mg/mL; No micronuclei induction after exposure to 2.5–100 mg/mL; No induction of proinflammatory cytokines in hMDMs. | Toxicity impact on lungs or bone marrow | [181] |
| CNC CNC- carboxyl groups | Softwood cellulose pulp | MTS assay | CaCO-2, HeLa, MDCK, J774 | CNC not exhibit any significant cytotoxicity; can exert stress on cells if they possess a high charge density; Charge-dependent decrease in mitochondrial activity (charge contents > 3.9 mmol/g). | Drug delivery | [180] |
| c-CNCs t-CNCs | Cotton Tunicate from Stuela clava | LDH assay | A549 MDM MDDC | The aspect ratio in combination with CNCs dose influences the uptake by the 3D co-culture system of the human epithelial airway barrier system. | Toxicity impact on lungs | [205] |
| CNC | Wood pulp | TB assay | A549 | CNC were nontoxic to A549 cells; CNC induced a robust inflammatory response; CNC particles induced a more robust inflammatory response compared to NCF. | Comparable toxicity of CNC with CNF | [185] |
| CNCgel CNCdry | Wood pulp | LDH assay | MH-S | Low conc. (1.5 and 5 μg/cm2) induce no cytotoxicity; A high dose of CNCdry induced a decrease in cell viability; CNC exposure further altered the secretion of cytokines. | Toxicity impact on lungs | [182] |
| CNC | Wheat bran | MTT assay | Caco-2 | Dose-dependent decrease in cell viability, but only with significant results above 1000 μg/mL; The cell viability decreased significantly upon contact with CNC90 (88.09%) at 2000 μg/mL, although CNC30 (92.81%) and CNC60 (93.11%) did not significantly decrease the cell viability. | Biocompatible nanocomposites | [197] |
| K-CNC R-CNC | Rubberwood fiber Kenaf-bast fiber | MTT assay | RAW 264.7 HaCaT | Cytotoxicity of K-CNC and R-CNC is not significant up to 700 μg/mL; K-CNC and R-CNC induced the formation of ROS in RAW264.7 macrophages. | Biocompatible nanocomposites | [183] |
| CNC CNC-FL CNC-HM | Cellulose pulp | MTT assay | ATCC PCS201012, A375 | No cytotoxicity in direct and indirect contact assays. | Drug delivery | [118] |
| CNC in nanocomposites | ||||||
| Collagen/CNCs/ GMs scaffolds | MCC | MTT assay | HUVECs | No cytotoxicity; Excellent biocompatibility. | Vascular TE | [133] |
| CNC CNC-AEM CNC-AEMA | Softwood pulp | ATP assay | J774 A.1 PBMNC | One cationic CNC induced secretion of proinflammatory cytokine IL-1b associated with increase mitochondrial-derived ROS and extracellular ATP levels. | Drug and DNA delivery systems | [206] |
| PLA/CNCg-PEG nanocomposites | Southern pine | Live/dead assays | hMSCs | Suitable biocompatibility; Nontoxic effect on hMSCs proliferation. | Bone TE | [134] |
| TEMPO-CNC reinforced PVA hydrogels | MCC | AB assay | HCE-2cells | Nontoxicity; Excellent biocompatibility; The HCE-2 cells viability above the 70%. | Ophthalmic applications | [138] |
| PVA/CNC nanocomposites | Sugarcane bagasse | MTT assay | L929 | Noncytotoxic effect; Strong attachment and proliferation of human fibroblast skin cells on the scaffold. | TE scaffolds | [131] |
| GA-HA-CNC hydrogels | MCC | CCK-8 assay | NIH-3T3 | Cell viability, at 1, 4, and 7 days, higher than 70% limit; No foreign body response. | Skin TE | [132] |
| CS/Gel/NCC/CP nanocomposites | Soft wood cellulose fibers | MTT assay | Fibroblast cell | Lack of cytotoxicity after 3 days of increasing the cells’ viability. | Wound healing | [113] |
| CNC/PVA | MCC | AB assay | HCE-2 | Nontoxic and cytocompatible profile of the CNC-PVA hydrogel; Suitable biocompatibility toward HCE-2. | Ophthalmic applications | [207] |
| Material | Cellulose Source | Toxicological Experiment | Cells Lines | Toxicological Results | Results and Possible Application | Ref. |
|---|---|---|---|---|---|---|
| CNF | ||||||
| CNF | Bleached dissolving pulp Norway spruce (Picea bies) | MTT assay [3H]-thymidine uptake assay | L929; Thymocytes PBMNCs | CNFs were not cytotoxic; CNC has non-inflammatory and on-immunogenic properties. | Implantable biomaterials TE | [184] |
| CNF | Pinus radiata pulp | LDH assay MTT assay | HEK NHDF | No toxic effect for keratinocytes and fibroblasts; Non-immunotoxic. | Wound dressings | [208] |
| CNF CNC | Wood pulp | TB assay | A549 | CNF caused a significant decrease in cell viability, at 72 h; Decrease in GSH levels after exposure to CNF. | CNC toxicity | [185] |
| U-NFC A-NFC C-NFC | Never-dried bleached sulfite softwood dissolving pulp | AB assay LDH assays | HDF MRC-5 THP-1 | No cytotoxicity for treated NFC; HDF and MRC-5 cells: the metabolic activity of the treated cells was comparable to that of the negative control; THP-1 cells: a higher metabolic activity of the NFC-treated; U-CNF has an inflammatory response, which was suppressed when surface charges were introduced on the CNFs. | Toxicity impacts on dermal, lung, and macrophage cells | [187] |
| CNF | Bleached Eucalyptus Globulus kraft pulp | MTT assay | A549 THP-1 | Cytotoxic effect at the highest dose tested; Genotoxic effects in A549 cells in the co-cultures; No oxidative DNA damages. | TE | [209] |
| CNF | Curauá fibers (Ananas erectifolius L. B. Smith) | Cytotoxicity assays ISO 10993-5 | Vero | CNF shows no cytotoxicity and suitable biocompatibility; The morphology and basic functions of the cells are not affected by the direct contact with the tested materials. | Scaffold TE | [186] |
| CNF | Softwood bleached kraft fiber | LDH assay | Caco-2, HT-29MTX Raji B | Minimal or no cytotoxicity in a cellular model of the intestinal epithelium (for CNC-25 at 0.75% and 1.5% w/w, as well as for CNF-50 at 0.75% w/w). | Biocompatible material | [210] |
| CNF | Banana peel bran | MTT assay | Caco-2 | CNF conc. < 500 mg/mL are not cytotoxic to Caco-2 cells; Viability of Caco-2 decreased with increasing CNF conc. | Biocompatible material | [211] |
| U-NFC A-NFC C-NFC P-NFC S-NFC | Never-dried bleached sulfite softwood dissolving pulp | Resazurin Assay | Caco-2 | None of the NFCs inducing cytotoxic effects in the intestinal cells; The differences in physics-chemical properties of the studied NFCs were not reflected in the Caco-2 response in terms of metabolic activity and cell membrane integrity. | Drug release in gastrointestinal tract (GIT) | [188] |
| U-NFC C-NFC H-NFC P-NFC S-NFC | Never-dried bleached sulfite softwood dissolving pulp | MTS Assay | BEAS-2B | No cytotoxicity for the highest tested dose (500 μg/mL) for any of the NFCs; None of the NFCs induced genotoxic effects; All samples were able to increase intracellular formation of ROS. | In vitro toxicity of NFCs | [189] |
| c-CNF cys-CNF | Never-dried bleached sulfite softwood dissolving pulp | PB assay | hDF | cys-CNF did not induce toxic effects on hDF when tested at a concentration up to 0.5 mg/mL, nor did the starting material c-NF cys-CNF presented a dual action in vitro: inhibition of metalloproteinase and radical scavenging activity. | Wound dressing | [190] |
| CNF in nanocomposites | ||||||
| CNF L-CNF CNC L-CNC | Dissolving pulp | AB assay | A549 THP-1 | Cytotoxic and inflammatory responses were dependent on type, size, and hydrophobicity Low or inexistent toxicity of all CNMs in A549 cells Dose-dependent cytotoxic and inflammatory responses in THP-1 cells. | TE | [199] |
| CNF /GEL/ApA | Bleached birch pulp | MTT assay | MSCs | CNFs and CNF-COOHs have no cytotoxicity; CNF-COOH-ApA cells expressed a low level of stress, visible through lower cell density and the cell inclusions. | Bone TE | [130] |
| NFC hydrogels crosslinked with Ca2+ | Bleached sulfite softwood pulp | AB assay | hDF | Cell viability about 78% indicates no toxic effects. No inflammatory response of blood-derived mononuclear cells was observed in relation to the cytokines secretion. | Wound healing | [27] |
| TEMPO-CNF hydrogel | Bleached birch kraft pulp | MTT assay | hDF | Nontoxicity effect and great hDF cells viability. | Wound healing | [172] |
| NFC/QCRs nanocomposites | Brown algae | MTT assay | L929 | Cells viability is higher than 80% (for 5 to 1000 μg/mL CNFs/QCRs), indicating that there is no cytotoxicity. | Wound healing | [119] |
| Material | Cellulose Source | Toxicological Experiment | Cells Lines | Toxicological Results | Results and Possible Application | Ref. |
|---|---|---|---|---|---|---|
| BNC | ||||||
| BNC scaffolds | G. xylinus | CCk-8 assay | HUVECs, SMCs, Fibroblasts | BC tubes have no toxic or side effects on vessel-related cells cultured on their surface; the surface of BC tubes was beneficial for cell attachment, proliferation, and ingrowth. | Vascular TE | [161] |
| Octenidine-loaded BNC | K. xylinus | ATP assay | HaCaT | Pure BNC has no influence on HaCaT viability; OCT/BNC extracts exhibited time and concentration-dependent toxicity; cell-damaging effects were observed at extract conc >10% and longer incubation times (24 and 48 h). | Active wound dressing | [101] |
| BNC | Sugar cane molasses | LDH activity | HepG2/C3A | BC is not cytotoxic (conc. < 170 μg/mL); BNC has a protective effect against CP-induced myelotoxicity and enotoxicity. | Biomaterial TE | [193] |
| Vaccarin- loaded BNC | G. xylinus | MTT assay | L929 | BNC-Vac has lower toxicity and better biocompatibility than BNC; RGR for both BNC and BNC-Vac was above 74%. | Wound dressing | [110] |
| Gentamycin-loaded BNC | K. xylinus | NR assay | U2-OS | No cytotoxicity on osteoblast culture after 24 h; gentamycin released from G-BNC after 8 h (400 mg/L) and 16 h (600 mg/L) is enough to eliminate S. aureus and P. aeruginosa biofilms. | Bone regeneration TE | [212] |
| Curcumin- loaded BNC | K. xylinus | MTS assay | HNDF | The cytotoxic effect on the cells depended on the conc. of curcumin; at 0.5 mg/mL C, a strong cytotoxicity for BNC-C and BNC-DC180; BNC-DC300 suitable cytotoxicity, even at higher extract conc. | Wound dressing | [191] |
| BNC-GTMAC BNC-GHDE | G. xylinus | AB assay | HaCaT | No cytotoxicity; Suitable wound closure rates in the presence of the samples, with complete coverage of the scratched area after 5 days. | Wound dressing | [192] |
| BNC in nanocomposites | ||||||
| BNC/ALG bilayer composites | G. xylinus | ISO10993-5:2009 | hNCs hMNC | The composites were found to be noncytotoxic, with a cell viability of 98% and a uniform distribution of cells on the entire porous layer. | Neocartilage TE | [147] |
| BNC-COL-Ap composites | G. xylinus | MTT assay | Osteoblastic cells | The composites did not exhibit cytotoxicity effects. | Bone regeneration TE | [144] |
| ALG/BCN/COL composite | A. xylinum | CCk-8 assay | MC3T3-E1 hAMS | MC3T3-E1 and hams cells were viable and proliferate well, after 2 and 5 days of incubation—suitable cytocompatibility. | TE | [140] |
| BC-PHEMA composites | A. xylinum | AB assay | rMSCs | BC-PHEMA composites are nontoxic and biocompatible; did not influence the morphology and proliferation of the rMSCs. | Wound dressing | [213] |
| BC/COL composites | G. xylinus | Live/ Dead assay | UCBMSCs | No cytotoxicity; Provide advanced microenvironment for UCB-MSCs viability and in vitro proliferation; Significantly elevated proteins and calcium deposition. | Bone regeneration TE | [214] |
| GEL/BNC nanocomposite | A. xylinum | MTT assay | HEK293 | BNG showed negligible cytotoxicity. | Wound dressing | [215] |
| BNC-GEL nanocomposite | - | MTS assay | MRC-5 | The samples have no cytotoxicity, and the cells retained their morphology in direct contact with the membrane, The cells attaching to the GEL porous site, while not attaching to the GEL thin-coated BC side. | Bone regeneration TE | [216] |
| Chitosan-BNC | K. xylinus | MTT assay | GM07492 | No cytotoxicity for the BC group and BC-Chi-Cip group; Ciprofloxacin-loaded BC-Chi samples exhibited a significant but slight decrease in the metabolic activity of cells (moderate cytotoxicity). | Wound dressing | [217] |
| GO/n-HAp/BNC/b-glucan biocomposite | - | NR assay | MC3T3-E1 | All samples had suitable potential for cell adhesion and proliferation with very low cytotoxicity The order of the cell viability: BgC-1.4 (93%) > BgC-1.3 (79.8%) > BgC-1.2 (71.4%) > BgC-1.1 (68.9%). | Bone regeneration TE | [194] |
4.1.2. In Vivo Cytotoxicity Analysis
4.2. In Vivo Degradability of Nanocellulose-Based Materials
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mokhena, T.C.; John, M.J. Cellulose nanomaterials: New generation materials for solving global issues. Cellulose 2020, 27, 1149–1194. [Google Scholar] [CrossRef]
- Pachuau, L. Application of Nanocellulose for Controlled Drug Delivery. In Nanocellulose and Nanohydrogel Matrices: Biotechnological and Biomedical Applications, 1st ed.; Jawaid, M., Mohammad, F., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; Chapter 1; pp. 1–19. [Google Scholar]
- Klemm, D.; Kramer, F.; Moritz, S.; Lindström, T.; Ankerfors, M.; Gray, D.; Dorris, A. Nanocelluloses: A New Family of Nature-Based Materials. Angew. Chem. Int. Ed. 2011, 50, 5438–5466. [Google Scholar] [CrossRef]
- Raghav, N.; Sharma, M.R.; Kennedy, J.F. Nanocellulose: A mini-review on types and use in drug delivery systems. Carbohydr. Polym. Technol. Appl. 2021, 2, 100031. [Google Scholar] [CrossRef]
- Kamel, S.; Khattab, T.A. Recent Advances in Cellulose-Based Biosensors for Medical Diagnosis. Biosensors 2020, 10, 67. [Google Scholar] [CrossRef]
- Naderi, A. Nanofibrillated cellulose: Properties reinvestigated. Cellulose 2017, 24, 1933–1945. [Google Scholar] [CrossRef]
- Maiuolo, L.; Algieri, V.; Olivito, F.; Tallarida, M.A.; Costanzo, P.; Jiritano, A.; De Nino, A. Chronicle of Nanocelluloses (NCs) for Catalytic Applications: Key Advances. Catalysts 2021, 11, 96. [Google Scholar] [CrossRef]
- Mirtaghavi, A.; Luo, J.; Muthuraj, R. Recent Advances in Porous 3D Cellulose Aerogels for Tissue Engineering Applications: A Review. J. Compos. Sci. 2020, 4, 152. [Google Scholar] [CrossRef]
- Klemm, D.; Cranston, E.D.; Fischer, D.; Gama, M.; Kedzior, S.A.; Kralisch, D.; Kramer, F.; Kondo, T.; Lindström, T.; Nietzsche, S.; et al. Nanocellulose as a natural source for groundbreaking applications in materials science: Today’s state. Mater. Today 2018, 21, 720–748. [Google Scholar] [CrossRef] [Green Version]
- Ioelovich, M. Characterization of Various Kinds of Nanocellulose. In Handbook of Nanocellulose and Cellulose Nanocom-Posites, 1st ed.; Kargarzadeh, H., Ahmad, I., Thomas, S., Dufresne, A., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; Chapter 2; pp. 51–100. [Google Scholar]
- Khalil, H.A.; Adnan, A.; Yahya, E.; Olaiya, N.; Safrida, S.; Hossain, S.; Balakrishnan, V.; Gopakumar, D.; Abdullah, C.; Oyekanmi, A.; et al. A Review on Plant Cellulose Nanofibre-Based Aerogels for Biomedical Applications. Polymers 2020, 12, 1759. [Google Scholar] [CrossRef] [PubMed]
- Hamad, W.Y. Cellulose Nanocrystals and Nanofibrils in Advanced Applications. In Handbook of Nanocellulose and Cellulose Nanocomposites, 1st ed.; Kargarzadeh, H., Ahmad, I., Thomas, S., Dufresne, A., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; Chapter 24; pp. 799–832. [Google Scholar]
- Ludwicka, K.; Kaczmarek, M.; Białkowska, A. Bacterial Nanocellulose—A Biobased Polymer for Active and Intelligent Food Packaging Applications: Recent Advances and Developments. Polymers 2020, 12, 2209. [Google Scholar] [CrossRef]
- Xue, Y.; Mou, Z.; Xiao, H. Nanocellulose as a sustainable biomass material: Structure, properties, present status and future prospects in biomedical applications. Nanoscale 2017, 9, 14758–14781. [Google Scholar] [CrossRef] [PubMed]
- Ciolacu, D.E.; Nicu, R.; Ciolacu, F. Cellulose-Based Hydrogels as Sustained Drug-Delivery Systems. Materials 2020, 13, 5270. [Google Scholar] [CrossRef] [PubMed]
- Jorfi, M.; Foster, E.J. Recent advances in nanocellulose for biomedical applications. J. Appl. Polym. Sci. 2015, 132, 41719–41737. [Google Scholar] [CrossRef]
- Omran, A.A.B.; Mohammed, A.A.B.A.; Sapuan, S.M.; Ilyas, R.A.; Asyraf, M.R.M.; Koloor, S.S.R.; Petrů, M. Micro- and Nanocellulose in Polymer Composite Materials: A Review. Polymers 2021, 13, 231. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Nair, A.; Shah, J.; Sreeharsha, N.; Gupta, S.; Shinu, P. Emerging Role of Hydrogels in Drug Delivery Systems, Tissue Engineering and Wound Management. Pharmaceutics 2021, 13, 357. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.K.; Basu, S.; Sen, B.; Lin, M.-H.; Kumar, A.N.; Yuan, Y.; Cullen, P.J.; Sarkar, D. Colloidal Gels with Tunable Mechanomorphology Regulate Endothelial Morphogenesis. Sci. Rep. 2019, 9, 1–17. [Google Scholar] [CrossRef]
- Ciolacu, D.; Cazacu, G. New Green Hydrogels Based on Lignin. J. Nanosci. Nanotechnol. 2018, 18, 2811–2822. [Google Scholar] [CrossRef]
- Del Valle, L.J.; Díaz, A.; Puiggalí, J. Hydrogels for Biomedical Applications: Cellulose, Chitosan, and Protein/Peptide Derivatives. Gels 2017, 3, 27. [Google Scholar] [CrossRef] [Green Version]
- Ciolacu, D.; Rudaz, C.; Vasilescu, M.; Budtova, T. Physically and chemically cross-linked cellulose cryogels: Structure, properties and application for controlled release. Carbohydr. Polym. 2016, 151, 392–400. [Google Scholar] [CrossRef]
- Ooi, S.Y.; Ahmad, I.; Amin, M.C.I.M. Effect of Cellulose Nanocrystals Content and pH on Swelling Behaviour of Gelatin Based Hydrogel. Sains Malays. 2015, 44, 793–799. [Google Scholar] [CrossRef]
- Shojaeiarani, J.; Bajwa, D.; Shirzadifar, A. A review on cellulose nanocrystals as promising biocompounds for the synthesis of nanocomposite hydrogels. Carbohydr. Polym. 2019, 216, 247–259. [Google Scholar] [CrossRef]
- Pandey, M.; Mohamad, N.; Amin, M.C.I.M. Bacterial Cellulose/Acrylamide pH-Sensitive Smart Hydrogel: Development, Characterization, and Toxicity Studies in ICR Mice Model. Mol. Pharm. 2014, 11, 3596–3608. [Google Scholar] [CrossRef]
- Tummala, G.K.; Felde, N.; Gustafsson, S.; Bubholz, A.; Schröder, S.; Mihranyan, A. Light scattering in poly(vinyl alcohol) hydrogels reinforced with nanocellulose for ophthalmic use. Opt. Mater. Express 2017, 7, 2824. [Google Scholar] [CrossRef]
- Basu, A.; Lindh, J.; Ålander, E.; Strømme, M.; Ferraz, N. On the use of ion-crosslinked nanocellulose hydrogels for wound healing solutions: Physicochemical properties and application-oriented biocompatibility studies. Carbohydr. Polym. 2017, 174, 299–308. [Google Scholar] [CrossRef]
- Li, J.; Yu, F.; Chen, G.; Liu, J.; Li, X.-L.; Cheng, B.; Mo, X.-M.; Chen, C.; Pan, J.-F. Moist-Retaining, Self-Recoverable, Bioadhesive, and Transparent in Situ Forming Hydrogels to Accelerate Wound Healing. ACS Appl. Mater. Interfaces 2019, 12, 2023–2038. [Google Scholar] [CrossRef] [PubMed]
- Jansen, K.; Schuurmans, C.C.; Jansen, J.; Masereeuw, R.; Vermonden, T. Hydrogel-Based Cell Therapies for Kidney Regeneration: Current Trends in Biofabrication and In Vivo Repair. Curr. Pharm. Des. 2017, 23, 3845–3857. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Farnood, R.; O’Kelly, K.; Chen, B. Mechanical behavior of transparent nanofibrillar cellulose–chitosan nanocomposite films in dry and wet conditions. J. Mech. Behav. Biomed. Mater. 2014, 32, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Latifi, N.; Asgari, M.; Vali, H.; Mongeau, L. A tissue-mimetic nano-fibrillar hybrid injectable hydrogel for potential soft tissue engineering applications. Sci. Rep. 2018, 8, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaston, J.; Thibeault, S.L. Hyaluronic acid hydrogels for vocal fold wound healing. Biomatter 2013, 3, e23799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, R.; Zhang, S.; Chen, X. Injectable hydrogels for tendon and ligament tissue engineering. J. Tissue Eng. Regen. Med. 2020, 14, 1333–1348. [Google Scholar] [CrossRef] [PubMed]
- De Lima, C.S.A.; Balogh, T.S.; Varca, J.P.R.O.; Varca, G.H.C.; Lugão, A.B.; Camacho-Cruz, L.A.; Bucio, E.; Kadlubowski, S.S. An Updated Review of Macro, Micro, and Nanostructured Hydrogels for Biomedical and Pharmaceutical Applications. Pharmaceutics 2020, 12, 970. [Google Scholar] [CrossRef] [PubMed]
- Rusu, D.; Ciolacu, D.; Simionescu, B.C. Cellulose-Based Hydrogels in Tissue Engineering Applications. Cellul. Chem. Technol. 2019, 53, 907–923. [Google Scholar] [CrossRef]
- Moscovici, M.; Hlevca, C.; Casarica, A.; Pavaloiu, R.D. Nanocellulose and Nanogels as Modern Drug Delivery Systems. In Nanocellulose and Nanohydrogel Matrices: Biotechnological and Biomedical Applications, 1st ed.; Jawaid, M., Mo-hammad, F., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; Chapter 9; pp. 209–269. [Google Scholar]
- Hamidi, M.; Azadi, A.; Rafiei, P. Hydrogel nanoparticles in drug delivery. Adv. Drug Deliv. Rev. 2008, 60, 1638–1649. [Google Scholar] [CrossRef]
- Miao, L.; Zhang, M.; Tu, Y.; Lin, S.; Hu, J. Stimuli-Responsive Cellulose-Based Hydrogels. In Cellulose-Based Super-Absorbent Hydrogels, Polymers and Polymeric Composites: A Reference Series, 1st ed.; Mondal, M.I.H., Ed.; Springer: Cham, Switzerland, 2019; Chapter 9; pp. 269–308. [Google Scholar]
- Yallapu, M.M.; Jaggi, M.; Chauhan, S.C. Design and engineering of nanogels for cancer treatment. Drug Discov. Today 2011, 16, 457–463. [Google Scholar] [CrossRef] [Green Version]
- Xu, F.; Zhu, J.; Lin, L.; Zhang, C.; Sun, W.; Fan, Y.; Yin, F.; Van Hest, J.C.M.; Wang, H.; Du, L.; et al. Multifunctional PVCL nanogels with redox-responsiveness enable enhanced MR imaging and ultrasound-promoted tumor chemotherapy. Theranostics 2020, 10, 4349–4358. [Google Scholar] [CrossRef] [PubMed]
- Sivaram, A.J.; Rajitha, P.; Maya, S.; Jayakumar, R.; Sabitha, M. Nanogels for delivery, imaging and therapy. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2015, 7, 509–533. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, S.A.R.M.; Gama, F.M.; Vilanova, M. Polymeric nanogels as vaccine delivery systems. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 159–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, M.; Ge, J.; Liu, Z.; Ouyang, P. Encapsulation of Single Enzyme in Nanogel with Enhanced Biocatalytic Activity and Stability. J. Am. Chem. Soc. 2006, 128, 11008–11009. [Google Scholar] [CrossRef]
- Chou, H.-S.; Larsson, M.; Hsiao, M.-H.; Chen, Y.-C.; Röding, M.; Nydén, M.; Liu, D.-M. Injectable insulin-lysozyme-loaded nanogels with enzymatically-controlled degradation and release for basal insulin treatment: In vitro characterization and in vivo observation. J. Control. Release 2016, 224, 33–42. [Google Scholar] [CrossRef]
- Kandil, R.; Merkel, O.M. Recent progress of polymeric nanogels for gene delivery. Curr. Opin. Colloid Interface Sci. 2019, 39, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Akram, M.; Hussain, R. Nanohydrogels: History, development, and applications in drug delivery. In Nanocellulose and Nanohydrogel Matrices: Biotechnological and Biomedical Applications, 1st ed.; Jawaid, M., Mohammad, F., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; Chapter 11; pp. 297–330. [Google Scholar]
- Lewis, L.; Derakhshandeh, M.; Hatzikiriakos, S.G.; Hamad, W.Y.; MacLachlan, M. Hydrothermal Gelation of Aqueous Cellulose Nanocrystal Suspensions. Biomacromolecules 2016, 17, 2747–2754. [Google Scholar] [CrossRef]
- Krontiras, P.; Gatenholm, P.; AHägg, D. Adipogenic differentiation of stem cells in three-dimensional porous bacterial nanocellulose scaffolds. J. Biomed. Mater. Res. Part B Appl. Biomater. 2014, 103, 195–203. [Google Scholar] [CrossRef]
- Picheth, G.F.; Pirich, C.; Sierakowski, M.R.; Woehl, M.A.; Sakakibara, C.N.; de Souza, C.F.; Martin, A.A.; da Silva, R.; de Freitas, R.A. Bacterial cellulose in biomedical applications: A review. Int. J. Biol. Macromol. 2017, 104, 97–106. [Google Scholar] [CrossRef]
- Sanandiya, N.D.; Vasudevan, J.; Das, R.; Lim, C.T.; Fernandez, J.G. Stimuli-responsive injectable cellulose thixogel for cell encapsulation. Int. J. Biol. Macromol. 2019, 130, 1009–1017. [Google Scholar] [CrossRef]
- De France, K.; Chan, K.J.W.; Cranston, E.D.; Hoare, T. Enhanced Mechanical Properties in Cellulose Nanocrystal–Poly(oligoethylene glycol methacrylate) Injectable Nanocomposite Hydrogels through Control of Physical and Chemical Cross-Linking. Biomacromolecules 2016, 17, 649–660. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Han, J.; Ding, Q.; Yue, Y.; Xia, C.; Ge, S.; Van Le, Q.; Dou, X.; Sonne, C.; Lam, S.S. TEMPO-oxidized cellulose nanofibers/polyacrylamide hybrid hydrogel with intrinsic self-recovery and shape memory properties. Cellulose 2021, 28, 1469–1488. [Google Scholar] [CrossRef]
- Song, K.; Zhu, W.; Li, X.; Yu, Z. A novel mechanical robust, self-healing and shape memory hydrogel based on PVA reinforced by cellulose nanocrystal. Mater. Lett. 2020, 260, 126884–126887. [Google Scholar] [CrossRef]
- Liu, S.; Jin, M.; Chen, Y.; Gao, H.; Shi, X.; Cheng, W.; Ren, L.; Wang, Y. High internal phase emulsions stabilised by supramolecular cellulose nanocrystals and their application as cell-adhesive macroporous hydrogel monoliths. J. Mater. Chem. B 2017, 5, 2671–2678. [Google Scholar] [CrossRef] [PubMed]
- Masruchin, N.; Park, B.-D.; Causin, V. Influence of sonication treatment on supramolecular cellulose microfibril-based hydrogels induced by ionic interaction. J. Ind. Eng. Chem. 2015, 29, 265–272. [Google Scholar] [CrossRef]
- Hua, J.; Liu, C.; Ng, P.F.; Fei, B. Bacterial cellulose reinforced double-network hydrogels for shape memory strand. Carbohydr. Polym. 2021, 259, 117737. [Google Scholar] [CrossRef]
- McKee, J.R.; Hietala, S.; Seitsonen, J.; Laine, J.; Kontturi, E.; Ikkala, O. Thermoresponsive Nanocellulose Hydrogels with Tunable Mechanical Properties. ACS Macro. Lett. 2014, 3, 266–270. [Google Scholar] [CrossRef]
- Talantikite, M.; Beury, N.; Moreau, C.; Cathala, B.; Leray, N. Arabinoxylan/Cellulose Nanocrystal Hydrogels with Tunable Mechanical Properties. Langmuir 2019, 35, 13427–13434. [Google Scholar] [CrossRef]
- Sabet, S.S. Shear Rheology of Cellulose Nanocrystal (CNC) Aqueous Suspensions. Ph.D. Thesis, University of British Columbia Library, Vancouver, BC, Canada, 2013. [Google Scholar]
- Shafiei-Sabet, S.; Hamad, W.Y.; Hatzikiriakos, S.G. Ionic strength effects on the microstructure and shear rheology of cellulose nanocrystal suspensions. Cellulose 2014, 21, 3347–3359. [Google Scholar] [CrossRef]
- Heath, L.; Thielemans, W. Cellulose nanowhisker aerogels. Green Chem. 2010, 12, 1448–1453. [Google Scholar] [CrossRef]
- Thomas, B.; Raj, M.C.; Athira, K.B.; Rubiah, M.H.; Joy, J.; Moores, A.; Drisko, G.L.; Sanchez, C. Nanocellulose, a Versatile Green Platform: From Biosources to Materials and Their Applications. Chem. Rev. 2018, 118, 11575–11625. [Google Scholar] [CrossRef] [PubMed]
- Heise, K.; Kontturi, E.; Allahverdiyeva, Y.; Tammelin, T.; Linder, M.B.; Ikkala, O. Nanocellulose: Recent Fundamental Advances and Emerging Biological and Biomimicking Applications. Adv. Mater. 2021, 33, e2004349. [Google Scholar] [CrossRef] [PubMed]
- Kontturi, E.; Laaksonen, P.; Linder, M.; Nonappa, N.; Gröschel, A.H.; Rojas, O.J.; Ikkala, O. Advanced Materials through Assembly of Nanocelluloses. Adv. Mater. 2018, 30, e1703779. [Google Scholar] [CrossRef] [Green Version]
- Saba, N.; Jawaid, M. Recent advances in nanocellulose-based polymer nanocomposites. In Woodhead Publishing Series in Composites Science and Engineering, Cellulose-Reinforced Nanofibre Composites, 1st ed.; Jawaid, M., Boufi, S., Abdul Khalil, H.P.S., Eds.; Woodhead Publishing: Cambridge, UK, 2017; Chapter 4; pp. 89–112. [Google Scholar]
- Dufresne, A. Cellulose nanomaterial reinforced polymer nanocomposites. Curr. Opin. Colloid Interface Sci. 2017, 29, 1–8. [Google Scholar] [CrossRef]
- Prusty, K.; Swain, S.K. Cellulose-based nanohydrogels for tissue engineering applications. In Nanocellulose and Nanohydrogel Matrices: Biotechnological and Biomedical Applications, 1st ed.; Jawaid, M., Mohammad, F., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; Chapter 4; pp. 67–90. [Google Scholar]
- Gonzalez, J.S.; Ludueña, L.N.; Ponce, A.; Alvarez, V.A. Poly(vinyl alcohol)/cellulose nanowhiskers nanocomposite hydrogels for potential wound dressings. Mater. Sci. Eng. C 2014, 34, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, F.V.; Pinheiro, I.F.; De Souza, S.F.; Mei, L.H.I.; Lona, L.M.F. Polymer Composites Reinforced with Natural Fibers and Nanocellulose in the Automotive Industry: A Short Review. J. Compos. Sci. 2019, 3, 51. [Google Scholar] [CrossRef] [Green Version]
- Nascimento, D.M.D.; Nunes, Y.L.; Figueirêdo, M.C.B.; Azeredo, H.; Aouada, F.; Feitosa, J.P.A.; Rosa, M.F.; Dufresne, A. Nanocellulose nanocomposite hydrogels: Technological and environmental issues. Green Chem. 2018, 20, 2428–2448. [Google Scholar] [CrossRef] [Green Version]
- Halib, N.; Perrone, F.; Cemazar, M.; Dapas, B.; Farra, R.; Abrami, M.; Chiarappa, G.; Forte, G.; Zanconati, F.; Pozzato, G.; et al. Potential Applications of Nanocellulose-Containing Materials in the Biomedical Field. Materials 2017, 10, 977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.; Xu, W.; Liu, W.; Zeng, G. Responsiveness, swelling, and mechanical properties of PNIPA nanocomposite hydrogels reinforced by nanocellulose. J. Mater. Res. 2015, 30, 1797–1807. [Google Scholar] [CrossRef]
- Abitbol, T.; Johnstone, T.; Quinn, T.M.; Gray, D.G. Reinforcement with cellulose nanocrystals of poly(vinyl alcohol) hydrogels prepared by cyclic freezing and thawing. Soft Matter 2011, 7, 2373–2379. [Google Scholar] [CrossRef]
- Han, J.; Lei, T.; Wu, Q. High-water-content mouldable polyvinyl alcohol-borax hydrogels reinforced by well-dispersed cellulose nanoparticles: Dynamic rheological properties and hydrogel formation mechanism. Carbohydr. Polym. 2014, 102, 306–316. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Liu, F.; Jiang, L.; Zhu, J.Y.; Haagenson, D.; Wiesenborn, D.P. Cellulose Nanocrystals vs. Cellulose Nanofibrils: A Comparative Study on Their Microstructures and Effects as Polymer Reinforcing Agents. ACS Appl. Mater. Interfaces 2013, 5, 2999–3009. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Han, C.-R.; Duan, J.-F.; Xu, F.; Sun, R.-C. Mechanical and Viscoelastic Properties of Cellulose Nanocrystals Reinforced Poly(ethylene glycol) Nanocomposite Hydrogels. ACS Appl. Mater. Interfaces 2013, 5, 3199–3207. [Google Scholar] [CrossRef]
- Jonoobi, M.; Oladi, R.; Davoudpour, Y.; Oksman, K.; Dufresne, A.; Hamzeh, Y.; Davoodi, R. Different preparation methods and properties of nanostructured cellulose from various natural resources and residues: A review. Cellulose 2015, 22, 935–969. [Google Scholar] [CrossRef]
- Huang, Y.; Zhu, C.; Yang, J.; Nie, Y.; Chen, C.; Sun, D. Recent advances in bacterial cellulose. Cellulose 2014, 21, 1–30. [Google Scholar] [CrossRef]
- Sulaeva, I.; Henniges, U.; Rosenau, T.; Potthast, A. Bacterial cellulose as a material for wound treatment: Properties and modifications. A review. Biotechnol. Adv. 2015, 33, 1547–1571. [Google Scholar] [CrossRef]
- Kaushik, M.; Moores, A. Review: Nanocelluloses as versatile supports for metal nanoparticles and their applications in catalysis. Green Chem. 2016, 18, 622–637. [Google Scholar] [CrossRef] [Green Version]
- Hu, Z.; Cranston, E.D.; Ng, R.; Pelton, R. Tuning Cellulose Nanocrystal Gelation with Polysaccharides and Surfactants. Langmuir 2014, 30, 2684–2692. [Google Scholar] [CrossRef]
- Chinga-Carrasco, G. Potential and Limitations of Nanocelluloses as Components in Biocomposite Inks for Three-Dimensional Bioprinting and for Biomedical Devices. Biomacromolecules 2018, 19, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Li, S.-M.; Jia, N.; Ma, M.-G.; Zhang, Z.; Liu, Q.-H.; Sun, R.-C. Cellulose—Silver nanocomposites: Microwave-assisted synthesis, characterization, their thermal stability, and antimicrobial property. Carbohydr. Polym. 2011, 86, 441–447. [Google Scholar] [CrossRef]
- Barua, S.; Das, G.; Aidew, L.; Buragohain, A.K.; Karak, N. Copper-copper oxide coated nanofibrillar cellulose: A promising biomaterial. RSC Adv. 2013, 3, 14997–15004. [Google Scholar] [CrossRef]
- Kupnik, K.; Primožič, M.; Kokol, V.; Leitgeb, M. Nanocellulose in Drug Delivery and Antimicrobially Active Materials. Polymers 2020, 12, 2825. [Google Scholar] [CrossRef] [PubMed]
- Mertaniemi, H.; Escobedo-Lucea, C.; Sanz-Garcia, A.; Gandía, C.; Mäkitie, A.; Partanen, J.; Ikkala, O.; Yliperttula, M. Human stem cell decorated nanocellulose threads for biomedical applications. Biomaterials 2016, 82, 208–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abitbol, T.; Rivkin, A.; Cao, Y.; Nevo, Y.; Abraham, E.; Ben-Shalom, T.; Lapidot, S.; Shoseyov, O. Nanocellulose, a tiny fiber with huge applications. Curr. Opin. Biotechnol. 2016, 39, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Salas, C.; Nypelö, T.; Rodriguez-Abreu, C.; Carrillo, C.; Rojas, O. Nanocellulose properties and applications in colloids and interfaces. Curr. Opin. Colloid Interface Sci. 2014, 19, 383–396. [Google Scholar] [CrossRef]
- Lin, N.; Gèze, A.; Wouessidjewe, D.; Huang, J.; Dufresne, A. Biocompatible Double-Membrane Hydrogels from Cationic Cellulose Nanocrystals and Anionic Alginate as Complexing Drugs Codelivery. ACS Appl. Mater. Interfaces 2016, 8, 6880–6889. [Google Scholar] [CrossRef]
- Akhlaghi, S.P. Surface Modification and Characterization of Cellulose Nanocrystals for Biomedical Applications. Ph.D. Thesis, University of Waterloo, Waterloo, ON, Canada, 2014. [Google Scholar]
- Taheri, A.; Mohammadi, M. The Use of Cellulose Nanocrystals for Potential Application in Topical Delivery of Hydroquinone. Chem. Biol. Drug Des. 2014, 86, 102–106. [Google Scholar] [CrossRef]
- Gunathilake, T.M.S.U.; Ching, Y.C.; Chuah, C.H. Enhancement of Curcumin Bioavailability Using Nanocellulose Reinforced Chitosan Hydrogel. Polymers 2017, 9, 64. [Google Scholar] [CrossRef] [Green Version]
- You, J.; Cao, J.; Zhao, Y.; Zhang, L.; Zhou, J.; Chen, Y. Improved Mechanical Properties and Sustained Release Behavior of Cationic Cellulose Nanocrystals Reinforeced Cationic Cellulose Injectable Hydrogels. Biomacromolecules 2016, 17, 2839–2848. [Google Scholar] [CrossRef]
- Ooi, S.Y.; Ahmad, I.; Amin, M.C.I.M. Cellulose nanocrystals extracted from rice husks as a reinforcing material in gelatin hydrogels for use in controlled drug delivery systems. Ind. Crop. Prod. 2016, 93, 227–234. [Google Scholar] [CrossRef]
- Supramaniam, J.; Adnan, R.; Kaus, N.H.M.; Bushra, R. Magnetic nanocellulose alginate hydrogel beads as potential drug delivery system. Int. J. Biol. Macromol. 2018, 118, 640–648. [Google Scholar] [CrossRef]
- Liu, Y.; Sui, Y.; Liu, C.; Liu, C.; Wu, M.; Li, B.; Li, Y. A physically crosslinked polydopamine/nanocellulose hydrogel as potential versatile vehicles for drug delivery and wound healing. Carbohydr. Polym. 2018, 188, 27–36. [Google Scholar] [CrossRef]
- Orasugh, J.T.; Saha, N.R.; Rana, D.; Sarkar, G.; Mollick, M.R.; Chattoapadhyay, A.; Mitra, B.C.; Mondal, D.; Ghosh, S.K.; Chattopadhyay, D. Jute cellulose nano-fibrils/hydroxypropylmethylcellulose nanocomposite: A novel material with potential for application in packaging and transdermal drug delivery system. Ind. Crop. Prod. 2018, 112, 633–643. [Google Scholar] [CrossRef]
- Guo, T.; Pei, Y.; Tang, K.; He, X.; Huang, J.; Wang, F. Mechanical and drug release properties of alginate beads reinforced with cellulose. J. Appl. Polym. Sci. 2017, 134, 44495–44503. [Google Scholar] [CrossRef]
- Shi, X.; Zheng, Y.; Wang, G.; Lin, Q.; Fan, J. pH- and electro-response characteristics of bacterial cellulose nanofiber/sodium alginate hybrid hydrogels for dual controlled drug delivery. RSC Adv. 2014, 4, 47056–47065. [Google Scholar] [CrossRef]
- Shao, W.; Liu, H.; Wang, S.; Wu, J.; Huang, M.; Min, H.; Liu, X. Controlled release and antibacterial activity of tetracycline hydrochloride-loaded bacterial cellulose composite membranes. Carbohydr. Polym. 2016, 145, 114–120. [Google Scholar] [CrossRef]
- Moritz, S.; Wiegand, C.; Wesarg, F.; Hessler, N.; Müller, F.A.; Kralisch, D.; Hipler, U.-C.; Fischer, D. Active wound dressings based on bacterial nanocellulose as drug delivery system for octenidine. Int. J. Pharm. 2014, 471, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, C.; Moritz, S.; Hessler, N.; Kralisch, D.; Wesarg, F.; Müller, F.A.; Fischer, D.; Hipler, U.-C. Antimicrobial functionalization of bacterial nanocellulose by loading with polihexanide and povidone-iodine. J. Mater. Sci. Mater. Med. 2015, 26, 1–14. [Google Scholar] [CrossRef]
- Dong, S.; Cho, H.J.; Lee, Y.W.; Roman, M. Synthesis and Cellular Uptake of Folic Acid-Conjugated Cellulose Nanocrystals for Cancer Targeting. Biomacromolecules 2014, 15, 1560–1567. [Google Scholar] [CrossRef]
- Chime, S.A.; Onunkwo, G.C.; Onyishi, I.I. Kinetics and mechanisms of drug release from swellable and non swellable matrices: A review. Res. J. Pharm. Biol. Chem. Sci. 2013, 4, 97–103. [Google Scholar]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol. Pharm. 2010, 67, 217–223. [Google Scholar]
- Pavaloiu, R.D.; Stroescu, M.; Parvulescu, O.; Dobre, T. Composite hydrogels of bacterial cellulose-carboxymethyl cellulose for drug release. Rev. Chim. 2014, 65, 948–951. [Google Scholar]
- Bacakova, L.; Pajorova, J.; Bacakova, M.; Skogberg, A.; Kallio, P.; Kolarova, K.; Svorcik, V. Versatile Application of Nanocellulose: From Industry to Skin Tissue Engineering and Wound Healing. Nanomaterials 2019, 9, 164. [Google Scholar] [CrossRef] [Green Version]
- Hakkarainen, T.; Koivuniemi, R.; Kosonen, M.; Escobedo-Lucea, C.; Sanz-García, A.; Vuola, J.; Valtonen, J.; Tammela, P.; Mäkitie, A.; Luukko, K.; et al. Nanofibrillar cellulose wound dressing in skin graft donor site treatment. J. Control. Release 2016, 244, 292–301. [Google Scholar] [CrossRef]
- Cattelaens, J.; Turco, L.; Berclaz, L.M.; Huelsse, B.; Hitzl, W.; Vollkommer, T.; Bodenschatz, K.J. The Impact of a Nanocellulose-Based Wound Dressing in the Management of Thermal Injuries in Children: Results of a Retrospective Evaluation. Life 2020, 10, 212. [Google Scholar] [CrossRef]
- Qiu, Y.; Qiu, L.; Cui, J.; Wei, Q. Bacterial cellulose and bacterial cellulose-vaccarin membranes for wound healing. Mater. Sci. Eng. C 2016, 59, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Mohamad, N.; Amin, M.C.I.M.; Pandey, M.; Ahmad, N.; Rajab, N.F. Bacterial cellulose/acrylic acid hydrogel synthesized via electron beam irradiation: Accelerated burn wound healing in an animal model. Carbohydr. Polym. 2014, 114, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Zubik, K.; Singhsa, P.; Wang, Y.; Manuspiya, H.; Narain, R. Thermo-Responsive Poly(N-Isopropylacrylamide)-Cellulose Nanocrystals Hybrid Hydrogels for Wound Dressing. Polymers 2017, 9, 119. [Google Scholar] [CrossRef] [Green Version]
- Akhavan-Kharazian, N.; Izadi-Vasafi, H. Preparation and characterization of chitosan/gelatin/nanocrystalline cellulose/calcium peroxide films for potential wound dressing applications. Int. J. Biol. Macromol. 2019, 133, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Lansdown, A.B.G. Calcium: A potential central regulator in wound healing in the skin. Wound Repair Regen. 2002, 10, 271–285. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Molino, B.Z.; Wang, X.; Cheng, F.; Xu, W.; Molino, P.; Bacher, M.; Su, D.; Rosenau, T.; Willför, S.; et al. 3D printing of nanocellulose hydrogel scaffolds with tunable mechanical strength towards wound healing application. J. Mater. Chem. B 2018, 6, 7066–7075. [Google Scholar] [CrossRef] [PubMed]
- Raghavendra, G.M.; Jayaramudu, T.; Varaprasad, K.; Ramesh, S.; Raju, K.M. Microbial resistant nanocurcumin-gelatin-cellulose fibers for advanced medical applications. RSC Adv. 2014, 4, 3494–3501. [Google Scholar] [CrossRef]
- Zander, N.E.; Dong, H.; Steele, J.; Grant, J.T. Metal Cation Cross-Linked Nanocellulose Hydrogels as Tissue Engineering Substrates. ACS Appl. Mater. Interfaces 2014, 6, 18502–18510. [Google Scholar] [CrossRef] [PubMed]
- Meschini, S.; Pellegrini, E.; Maestri, C.A.; Condello, M.; Bettotti, P.; Condello, G.; Scarpa, M. In vitro toxicity assessment of hydrogel patches obtained by cation-induced cross-linking of rod-like cellulose nanocrystals. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Zhong, Z.; Xia, H.; Hu, Q.; Ye, Q.; Wang, Y.; Chen, L.; Du, Y.; Shi, X.; Zhang, L. Construction of cellulose nanofibers/quaternized chitin/organic rectorite composites and their application as wound dressing materials. Biomater. Sci. 2019, 7, 2571–2581. [Google Scholar] [CrossRef]
- Ullah, H.; Wahid, F.; Santos, H.A.; Khan, T. Advances in biomedical and pharmaceutical applications of functional bacterial cellulose-based nanocomposites. Carbohydr. Polym. 2016, 150, 330–352. [Google Scholar] [CrossRef]
- Swingler, S.; Gupta, A.; Gibson, H.; Kowalczuk, M.; Heaselgrave, W.; Radecka, I. Recent Advances and Applications of Bacterial Cellulose in Biomedicine. Polymers 2021, 13, 412. [Google Scholar] [CrossRef]
- Barud, H.G.D.O.; da Silva, R.R.; Barud, H.D.S.; Tercjak, A.; Gutierrez, J.; Lustri, W.R.; de Oliveira, O.B.; Ribeiro, S. A multipurpose natural and renewable polymer in medical applications: Bacterial cellulose. Carbohydr. Polym. 2016, 153, 406–420. [Google Scholar] [CrossRef] [Green Version]
- Khalid, A.; Khan, R.; Ul-Islam, M.; Khan, T.; Wahid, F. Bacterial cellulose-zinc oxide nanocomposites as a novel dressing system for burn wounds. Carbohydr. Polym. 2017, 164, 214–221. [Google Scholar] [CrossRef]
- Sanyang, M.L.; Saba, N.; Jawaid, M.; Mohammad, F.; Salit, M.S. Bacterial nanocellulose applications for tissue engineering. In Nanocellulose and Nanohydrogel Matrices: Biotechnological and Biomedical Applications, 1st ed.; Jawaid, M., Mohammad, F., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; Chapter 3; pp. 47–66. [Google Scholar]
- Sharma, C.; Bhardwaj, N.K. Bacterial nanocellulose: Present status, biomedical applications and future perspectives. Mater. Sci. Eng. C 2019, 104, 109963. [Google Scholar] [CrossRef]
- Murizan, N.I.S.; Mustafa, N.S.; Ngadiman, N.H.A.; Yusof, N.M.; Idris, A. Review on Nanocrystalline Cellulose in Bone Tissue Engineering Applications. Polymers 2020, 12, 2818. [Google Scholar] [CrossRef]
- Huang, A.; Peng, X.; Geng, L.; Zhang, L.; Huang, K.; Chen, B.; Gu, Z.; Kuang, T. Electrospun poly (butylene succinate)/cellulose nanocrystals bio-nanocomposite scaffolds for tissue engineering: Preparation, characterization and in vitro evaluation. Polym. Test. 2018, 71, 101–109. [Google Scholar] [CrossRef]
- Subhedar, A.; Bhadauria, S.; Ahankari, S.; Kargarzadeh, H. Nanocellulose in biomedical and biosensing applications: A review. Int. J. Biol. Macromol. 2021, 166, 587–600. [Google Scholar] [CrossRef]
- Ghafari, R.; Jonoobi, M.; Amirabad, L.M.; Oksman, K.; Taheri, A.R. Fabrication and characterization of novel bilayer scaffold from nanocellulose based aerogel for skin tissue engineering applications. Int. J. Biol. Macromol. 2019, 136, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Gorgieva, S.; Girandon, L.; Kokol, V. Mineralization potential of cellulose-nanofibrils reinforced gelatine scaffolds for promoted calcium deposition by mesenchymal stem cells. Mater. Sci. Eng. C 2017, 73, 478–489. [Google Scholar] [CrossRef]
- Lam, N.T.; Chollakup, R.; Smitthipong, W.; Nimchua, T.; Sukyai, P. Utilizing cellulose from sugarcane bagasse mixed with poly(vinyl alcohol) for tissue engineering scaffold fabrication. Ind. Crop. Prod. 2017, 100, 183–197. [Google Scholar] [CrossRef]
- Yin, F.; Lin, L.; Zhan, S. Preparation and properties of cellulose nanocrystals, gelatin, hyaluronic acid composite hydrogel as wound dressing. J. Biomater. Sci. Polym. Ed. 2019, 30, 190–201. [Google Scholar] [CrossRef]
- Li, W.; Lan, Y.; Guo, R.; Zhang, Y.; Xue, W.; Zhang, Y. In vitro and in vivo evaluation of a novel collagen/cellulose nanocrystals scaffold for achieving the sustained release of basic fibroblast growth factor. J. Biomater. Appl. 2015, 29, 882–893. [Google Scholar] [CrossRef]
- Zhang, C.; Salick, M.R.; Cordie, T.M.; Ellingham, T.; Dan, Y.; Turng, L.-S. Incorporation of poly(ethylene glycol) grafted cellulose nanocrystals in poly(lactic acid) electrospun nanocomposite fibers as potential scaffolds for bone tissue engineering. Mater. Sci. Eng. C 2015, 49, 463–471. [Google Scholar] [CrossRef]
- Tummala, G.K. Hydrogels of Poly(Vinyl Alcohol) and Nanocellulose for Ophthalmic Applications. Synthesis, Characterization, Biocompatibility and Drug Delivery Studies. Ph.D. Thesis, UPPSALA University, Uppsala, Sweden, 2018. [Google Scholar]
- Yang, J.; Han, C. Mechanically Viscoelastic Properties of Cellulose Nanocrystals Skeleton Reinforced Hierarchical Composite Hydrogels. ACS Appl. Mater. Interfaces 2016, 8, 25621–25630. [Google Scholar] [CrossRef]
- Prince, E.; Alizadehgiashi, M.; Campbell, M.; Khuu, N.; Albulescu, A.; De France, K.; Ratkov, D.; Li, Y.; Hoare, T.; Kumacheva, E. Patterning of Structurally Anisotropic Composite Hydrogel Sheets. Biomacromolecules 2018, 19, 1276–1284. [Google Scholar] [CrossRef]
- Tummala, G.K.; Rojas, R.; Mihranyan, A. Poly(vinyl alcohol) Hydrogels Reinforced with Nanocellulose for Ophthalmic Applications: General Characteristics and Optical Properties. J. Phys. Chem. B 2016, 120, 13094–13101. [Google Scholar] [CrossRef]
- Martínez Ávila, H.; Schwarz, S.; Feldmann, E.M.; Mantas, A.; von Bomhard, A.; Gatenholm, P.; Rotter, N. Biocompatibility evaluation of densified bacterial nanocellulose hydrogel as an implant material for auricular cartilage regeneration. Appl. Microbiol. Biotechnol. 2014, 98, 7423–7435. [Google Scholar] [CrossRef]
- Yan, H.; Huang, D.; Chen, X.; Liu, H.; Feng, Y.; Zhao, Z.; Dai, Z.; Zhang, X.; Lin, Q. A novel and homogeneous scaffold material: Preparation and evaluation of alginate/bacterial cellulose nanocrystals/collagen composite hydrogel for tissue engineering. Polym. Bull. 2017, 75, 985–1000. [Google Scholar] [CrossRef]
- Osorio, M.; Fernández-Morales, P.; Gañán, P.; Zuluaga, R.; Kerguelen, H.; Ortiz, I.; Castro, C. Development of novel three-dimensional scaffolds based on bacterial nanocellulose for tissue engineering and regenerative medicine: Effect of processing methods, pore size, and surface area. J. Biomed. Mater. Res. Part A 2019, 107, 348–359. [Google Scholar] [CrossRef]
- Zheng, Y.; Wen, X.; Wu, J.; Wang, L.-N.; Yuan, Z.; Peng, J.; Meng, H. Immobilization of collagen peptide on dialdehyde bacterial cellulose nanofibers via covalent bonds for tissue engineering and regeneration. Int. J. Nanomed. 2015, 10, 4623–4637. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.; Wang, J.; Yang, F.; Shao, Y.; Zhang, X.; Dai, K. Modification and evaluation of micro-nano structured porous bacterial cellulose scaffold for bone tissue engineering. Mater. Sci. Eng. C 2017, 75, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Saska, S.; Teixeira, L.N.; Raucci, L.M.S.D.C.; Scarel-Caminaga, R.M.; Franchi, L.P.; dos Santos, R.A.; Santagneli, S.H.; Capela, M.V.; de Oliveira, P.T.; Takahashi, C.S.; et al. Nanocellulose-collagen-apatite composite associated with osteogenic growth peptide for bone regeneration. Int. J. Biol. Macromol. 2017, 103, 467–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.; Park, J.; Jo, I.; Cho, S.-P.; Sung, D.; Ryu, S.; Park, M.; Min, K.-A.; Kim, J.; Hong, S.; et al. In situ hybridization of carbon nanotubes with bacterial cellulose for three-dimensional hybrid bioscaffolds. Biomaterials 2015, 58, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Nimeskern, L.; Ávila, H.M.; Sundberg, J.; Gatenholm, P.; Müller, R.; Stok, K.S. Mechanical evaluation of bacterial nanocellulose as an implant material for ear cartilage replacement. J. Mech. Behav. Biomed. Mater. 2013, 22, 12–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez Ávila, H.; Feldmann, E.M.; Pleumeekers, M.M.; Nimeskern, L.; Kuo, W.; de Jong, W.C.; Schwarz, S.; Müller, R.; Hendriks, J.; Rotter, N.; et al. Novel bilayer bacterial nanocellulose scaffold supports neocartilage formation in vitro and in vivo. Biomaterials 2015, 44, 122–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, G.; Nandgaonkar, A.G.; Habibi, Y.; Krause, W.E.; Wei, Q.; Lucia, L.A. An environmentally benign approach to achieving vectorial alignment and high microporosity in bacterial cellulose/chitosan scaffolds. RSC Adv. 2017, 7, 13678–13688. [Google Scholar] [CrossRef] [Green Version]
- Dugan, J.M.; Gough, J.E.; Eichhorn, S.J. Directing the Morphology and Differentiation of Skeletal Muscle Cells Using Oriented Cellulose Nanowhiskers. Biomacromolecules 2010, 11, 2498–2504. [Google Scholar] [CrossRef]
- Dugan, J.M.; Collins, R.F.; Gough, J.E.; Eichhorn, S.J. Oriented surfaces of adsorbed cellulose nanowhiskers promote skeletal muscle myogenesis. Acta Biomater. 2013, 9, 4707–4715. [Google Scholar] [CrossRef]
- Kanimozhi, K.; Basha, S.K.; Kumari, V.S. Processing and characterization of chitosan/PVA and methylcellulose porous scaffolds for tissue engineering. Mater. Sci. Eng. C 2016, 61, 484–491. [Google Scholar] [CrossRef]
- Monteiro, I.P.; Shukla, A.; Marques, A.P.; Reis, R.L.; Hammond, P.T. Spray-assisted layer-by-layer assembly on hyaluronic acid scaffolds for skin tissue engineering. J. Biomed. Mater. Res. Part A 2014, 103, 330–340. [Google Scholar] [CrossRef] [Green Version]
- Yuan, F.; Lin, L.-X.; Zhang, H.-H.; Huang, D.; Sun, Y.-L. Effect of carbodiimide-derivatized hyaluronic acid gelatin on preventing postsurgical intra-abdominal adhesion formation and promoting healing in a rat model. J. Biomed. Mater. Res. Part A 2016, 104, 1175–1181. [Google Scholar] [CrossRef]
- Torgbo, S.; Sukyai, P. Bacterial cellulose-based scaffold materials for bone tissue engineering. Appl. Mater. Today 2018, 11, 34–49. [Google Scholar] [CrossRef]
- Seyednejad, H.; Gawlitta, D.; Kuiper, R.; de Bruin, A.; van Nostrum, C.F.; Vermonden, T.; Dhert, W.J.; Hennink, W.E. In vivo biocompatibility and biodegradation of 3D-printed porous scaffolds based on a hydroxyl-functionalized poly(ε-caprolactone). Biomaterials 2012, 33, 4309–4318. [Google Scholar] [CrossRef] [PubMed]
- Parithimarkalaignan, S.; Padmanabhan, T.V. Osseointegration: An Update. J. Indian Prosthodont. Soc. 2013, 13, 2–6. [Google Scholar] [CrossRef]
- Pigossi, S.C.; De Oliveira, G.J.P.L.; Finoti, L.S.; Nepomuceno, R.; Spolidorio, L.C.; Rossa, C.; Ribeiro, S.J.L.; Saska, S.; Scarel-Caminaga, R.M. Bacterial cellulose-hydroxyapatite composites with osteogenic growth peptide (OGP) or pentapeptide OGP on bone regeneration in critical-size calvarial defect model. J. Biomed. Mater. Res. Part A 2015, 103, 3397–3406. [Google Scholar] [CrossRef]
- Ran, J.; Jiang, P.; Liu, S.; Sun, G.; Yan, P.; Shen, X.; Tong, H. Constructing multi-component organic/inorganic composite bacterial cellulose-gelatin/hydroxyapatite double-network scaffold platform for stem cell-mediated bone tissue engineering. Mater. Sci. Eng. C 2017, 78, 130–140. [Google Scholar] [CrossRef]
- Ahn, S.-J.; Shin, Y.M.; Kim, S.E.; Jeong, S.I.; Jeong, J.-O.; Park, J.-S.; Gwon, H.-J.; Seo, D.E.; Nho, Y.-C.; Kang, S.S.; et al. Characterization of hydroxyapatite-coated bacterial cellulose scaffold for bone tissue engineering. Biotechnol. Bioprocess Eng. 2015, 20, 948–955. [Google Scholar] [CrossRef]
- Xu, B.; Ju, Y.; Cui, Y.; Song, G. Carbon nanotube array inducing osteogenic differentiation of human mesenchymal stem cells. Mater. Sci. Eng. C 2015, 51, 182–188. [Google Scholar] [CrossRef]
- Zang, S.; Zhang, R.; Chen, H.; Lu, Y.; Zhou, J.; Chang, X.; Qiu, G.; Wu, Z.; Yang, G. Investigation on artificial blood vessels prepared from bacterial cellulose. Mater. Sci. Eng. C 2015, 46, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Cha, R.; Li, J.; Hao, W.; Zhang, Y.; Zhou, F. Advances in tissue engineering of nanocellulose-based scaffolds: A review. Carbohydr. Polym. 2019, 224, 115144. [Google Scholar] [CrossRef] [PubMed]
- Seifu, D.G.; Meghezi, S.; Unsworth, L.; Mequanint, K.; Mantovani, D. Viscoelastic properties of multi-layered cellularized vascular tissues fabricated from collagen gel. J. Mech. Behav. Biomed. Mater. 2018, 80, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Lykov, A.P.; Poveshchenko, O.V.; Surovtseva, M.A.; Bondarenko, N.A.; Kim, I.I.; Karpenko, A.; Pokushalov, E.A.; Karaskov, A.M. Effect of Polyethylene Terephthalate on Functional Properties of Endothelial and Mesenchymal Cells. Bull. Exp. Biol. Med. 2019, 166, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Keshk, S.M. Bacterial Cellulose Production and its Industrial Applications. J. Bioprocess Biotech. 2014, 4, 1000150–1000159. [Google Scholar] [CrossRef]
- Jo, B.-H.; Van Lerberghe, L.; Motsegood, K.; Beebe, D. Three-dimensional micro-channel fabrication in polydimethylsiloxane (PDMS) elastomer. J. Microelectromech. Syst. 2000, 9, 76–81. [Google Scholar] [CrossRef]
- Rouillard, A.; Berglund, C.M.; Lee, J.Y.; Polacheck, W.; Tsui, Y.; Bonassar, L.J.; Kirby, B. Methods for Photocrosslinking Alginate Hydrogel Scaffolds with High Cell Viability. Tissue Eng. Part C Methods 2011, 17, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Marijnissen, W.J.; van Osch, G.J.; Aigner, J.; van der Veen, S.W.; Hollander, A.P.; Verwoerd-Verhoef, H.L.; Verhaar, J. Alginate as a chondrocyte-delivery substance in combination with a non-woven scaffold for cartilage tissue engineering. Biomaterials 2002, 23, 1511–1517. [Google Scholar] [CrossRef]
- Cernencu, A.; Lungu, A.; Stancu, I.-C.; Serafim, A.; Heggset, E.B.; Syverud, K.; Iovu, H. Bioinspired 3D printable pectin-nanocellulose ink formulations. Carbohydr. Polym. 2019, 220, 12–21. [Google Scholar] [CrossRef]
- Donderwinkel, I.; Van Hest, J.C.M.; Cameron, N.R. Bio-inks for 3D bioprinting: Recent advances and future prospects. Polym. Chem. 2017, 8, 4451–4471. [Google Scholar] [CrossRef] [Green Version]
- Markstedt, K.; Mantas, A.; Tournier, I.; Ávila, H.M.; Hägg, D.; Gatenholm, P. 3D Bioprinting Human Chondrocytes with Nanocellulose–Alginate Bioink for Cartilage Tissue Engineering Applications. Biomacromolecules 2015, 16, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Pranovich, A.; Uppstu, P.; Wang, X.; Kronlund, D.; Hemming, J.; Öblom, H.; Moritz, N.; Preis, M.; Sandler, N.; et al. Novel biorenewable composite of wood polysaccharide and polylactic acid for three dimensional printing. Carbohydr. Polym. 2018, 187, 51–58. [Google Scholar] [CrossRef]
- Heggset, E.B.; Strand, B.L.; Sundby, K.W.; Simon, S.; Chinga-Carrasco, G.; Syverud, K. Viscoelastic properties of nanocellulose based inks for 3D printing and mechanical properties of CNF/alginate biocomposite gels. Cellulose 2019, 26, 581–595. [Google Scholar] [CrossRef]
- Liu, C.; Li, B.; Du, H.; Lv, D.; Zhang, Y.; Yu, G.; Mu, X.; Peng, H. Properties of nanocellulose isolated from corncob residue using sulfuric acid, formic acid, oxidative and mechanical methods. Carbohydr. Polym. 2016, 151, 716–724. [Google Scholar] [CrossRef]
- Shao, C.; Wang, M.; Meng, L.; Chang, H.; Wang, B.; Xu, F.; Yang, J.; Wan, P. Mussel-Inspired Cellulose Nanocomposite Tough Hydrogels with Synergistic Self-Healing, Adhesive, and Strain-Sensitive Properties. Chem. Mater. 2018, 30, 3110–3121. [Google Scholar] [CrossRef]
- Cheng, S.; Zhang, Y.; Cha, R.; Yang, J.; Jiang, X. Water-soluble nanocrystalline cellulose films with highly transparent and oxygen barrier properties. Nanoscale 2015, 8, 973–978. [Google Scholar] [CrossRef] [PubMed]
- Lu, Z.; An, X.; Zhang, H.; Guan, M.; Liu, J.; Sun, Y.; Nie, S.; Cao, H.; Lu, B.; Liu, H. Study on the wet-web strength and pressability of paper sheet during the press process with the addition of nano-fibrillated cellulose (NFC). Carbohydr. Polym. 2019, 210, 332–338. [Google Scholar] [CrossRef]
- Hua, K.; Rocha, I.; Zhang, P.; Gustafsson, S.; Ning, Y.; Strømme, M.; Mihranyan, A.; Ferraz, N. Transition from Bioinert to Bioactive Material by Tailoring the Biological Cell Response to Carboxylated Nanocellulose. Biomacromolecules 2016, 17, 1224–1233. [Google Scholar] [CrossRef]
- Ventura, C.; Pinto, F.; Lourenço, A.F.; Ferreira, P.; Louro, H.; Silva, M.J. On the toxicity of cellulose nanocrystals and nanofibrils in animal and cellular models. Cellulose 2020, 27, 5509–5544. [Google Scholar] [CrossRef]
- Hosseinidoust, Z.; Sim, G.; Alam, N.; Tufenkji, N.; Van De Ven, T.G.M. Cellulose nanocrystals with tunable surface charge for nanomedicine. Nanoscale 2015, 7, 16647–16657. [Google Scholar] [CrossRef] [Green Version]
- Catalán, J.; Ilves, M.; Järventaus, H.; Hannukainen, K.-S.; Kontturi, E.; Vanhala, E.; Alenius, H.; Savolainen, K.M.; Norppa, H. Genotoxic and immunotoxic effects of cellulose nanocrystals in vitro. Environ. Mol. Mutagen. 2015, 56, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Erdem, J.S.; Alswady-Hoff, M.; Ervik, T.K.; Skare, Ø.; Ellingsen, D.G.; Zienolddiny, S. Cellulose nanocrystals modulate alveolar macrophage phenotype and phagocytic function. Biomaterials 2019, 203, 31–42. [Google Scholar] [CrossRef]
- Tuerxun, D.; Pulingam, T.; Nordin, N.I.; Chen, Y.W.; Bin Kamaldin, J.; Julkapli, N.B.M.; Lee, H.V.; Leo, B.F.; Bin Johan, M.R. Synthesis, characterization and cytotoxicity studies of nanocrystalline cellulose from the production waste of rubber-wood and kenaf-bast fibers. Eur. Polym. J. 2019, 116, 352–360. [Google Scholar] [CrossRef]
- Colic, M.; Mihajlović, D.; Mathew, A.P.; Naseri, N.; Kokol, V. Cytocompatibility and immunomodulatory properties of wood based nanofibrillated cellulose. Cellulose 2015, 22, 763–778. [Google Scholar] [CrossRef]
- Menas, A.L.; Yanamala, N.; Farcas, M.; Russo, M.; Friend, S.; Fournier, P.M.; Star, A.; Iavicoli, I.; Shurin, G.V.; Vogel, U.; et al. Fibrillar vs. crystalline nanocellulose pulmonary epithelial cell responses: Cytotoxicity or inflammation? Chemosphere 2017, 171, 671–680. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Souza, S.F.; Mariano, M.; Reis, D.; Lombello, C.B.; Ferreira, M.; Sain, M. Cell interactions and cytotoxic studies of cellulose nanofibers from Curauá natural fibers. Carbohydr. Polym. 2018, 201, 87–95. [Google Scholar] [CrossRef]
- Lopes, V.R.; Sanchez-Martinez, C.; Strømme, M.; Ferraz, N. In vitro biological responses to nanofibrillated cellulose by human dermal, lung and immune cells: Surface chemistry aspect. Part. Fibre Toxicol. 2017, 14, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Lopes, V.R.; Strømme, M.; Ferraz, N. In Vitro Biological Impact of Nanocellulose Fibers on Human Gut Bacteria and Gastrointestinal Cells. Nanomaterials 2020, 10, 1159. [Google Scholar] [CrossRef] [PubMed]
- Aimonen, K.; Suhonen, S.; Hartikainen, M.; Lopes, V.; Norppa, H.; Ferraz, N.; Catalán, J. Role of Surface Chemistry in the In Vitro Lung Response to Nanofibrillated Cellulose. Nanomaterials 2021, 11, 389. [Google Scholar] [CrossRef]
- Blasi-Romero, A.; Palo-Nieto, C.; Sandström, C.; Lindh, J.; Strømme, M.; Ferraz, N. In Vitro Investigation of Thiol-Functionalized Cellulose Nanofibrils as a Chronic Wound Environment Modulator. Polymers 2021, 13, 249. [Google Scholar] [CrossRef]
- Zikmundova, M.; Vereshaka, M.; Kolarova, K.; Pajorova, J.; Svorcik, V.; Bacakova, L. Effects of Bacterial Nanocellulose Loaded with Curcumin and Its Degradation Products on Human Dermal Fibroblasts. Materials 2020, 13, 4759. [Google Scholar] [CrossRef]
- Orlando, I.; Basnett, P.; Nigmatullin, R.; Wang, W.; Knowles, J.C.; Roy, I. Chemical Modification of Bacterial Cellulose for the Development of an Antibacterial Wound Dressing. Front. Bioeng. Biotechnol. 2020, 8, 1–19. [Google Scholar] [CrossRef]
- Pinto, F.C.M.; De-Oliveira, A.C.A.; De-Carvalho, R.R.; Gomes-Carneiro, M.R.; Coelho, D.R.; Lima, S.V.C.; Paumgartten, F.J.R.; Aguiar, J.L.A. Acute toxicity, cytotoxicity, genotoxicity and antigenotoxic effects of a cellulosic exopolysaccharide obtained from sugarcane molasses. Carbohydr. Polym. 2016, 137, 556–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.U.A.; Haider, S.; Haider, A.; Razak, S.I.A.; Kadir, M.R.A.; AShah, S.; Javed, A.; Shakir, I.; Al-Zahrani, A.A. Development of porous, antibacterial and biocompatible GO/n-HAp/bacterial cellulose/β-glucan biocomposite scaffold for bone tissue engineering. Arab. J. Chem. 2021, 14, 102924. [Google Scholar] [CrossRef]
- Salimi, S.; Sotudeh-Gharebagh, R.; Zarghami, R.; Chan, S.Y.; Yuen, K.H. Production of Nanocellulose and Its Applications in Drug Delivery: A Critical Review. ACS Sustain. Chem. Eng. 2019, 7, 15800–15827. [Google Scholar] [CrossRef]
- Yanamala, N.; Farcas, M.; Hatfield, M.K.; Kisin, E.R.; Kagan, V.E.; Geraci, C.L.; Shvedova, A.A. In Vivo Evaluation of the Pulmonary Toxicity of Cellulose Nanocrystals: A Renewable and Sustainable Nanomaterial of the Future. ACS Sustain. Chem. Eng. 2014, 2, 1691–1698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiao, Y.; Liu, Y.; Wang, X.; Li, M.; Lei, H.; Xu, H. Cellulose nanocrystals prepared from wheat bran: Characterization and cytotoxicity assessment. Int. J. Biol. Macromol. 2019, 140, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Park, E.-J.; Khaliullin, T.O.; Shurin, M.R.; Kisin, E.R.; Yanamala, N.; Fadeel, B.; Chang, J.; Shvedova, A.A. Fibrous nanocellulose, crystalline nanocellulose, carbon nanotubes, and crocidolite asbestos elicit disparate immune responses upon pharyngeal aspiration in mice. J. Immunotoxicol. 2017, 15, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Yanamala, N.; Kisin, E.R.; Menas, A.L.; Farcas, M.; Khaliullin, T.O.; Vogel, U.; Shurin, G.V.; Schwegler-Berry, D.; Fournier, P.M.; Star, A.; et al. In Vitro Toxicity Evaluation of Lignin-(Un)coated Cellulose Based Nanomaterials on Human A549 and THP-1 Cells. Biomacromolecules 2016, 17, 3464–3473. [Google Scholar] [CrossRef]
- Braakhuis, H.M.; Park, M.V.D.Z.; Gosens, I.; De Jong, W.H.; Cassee, F.R. Physicochemical characteristics of nanomaterials that affect pulmonary inflammation. Part. Fibre Toxicol. 2014, 11, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maestri, C.A.; Bettotti, P.; Scarpa, M. Fabrication of complex-shaped hydrogels by diffusion controlled gelation of nanocellulose crystallites. J. Mater. Chem. B 2017, 5, 8096–8104. [Google Scholar] [CrossRef]
- Shpichka, A.; Butnaru, D.; Bezrukov, E.A.; Sukhanov, R.B.; Atala, A.; Burdukovskii, V.; Zhang, Y.; Timashev, P. Skin tissue regeneration for burn injury. Stem Cell Res. Ther. 2019, 10, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Kwak, M.H.; Kim, J.E.; Go, J.; Koh, E.K.; Song, S.H.; Son, H.J.; Kim, H.S.; Yun, Y.H.; Jung, Y.J.; Hwang, D.Y. Bacterial cellulose membrane produced by Acetobacter sp. A10 for burn wound dressing applications. Carbohydr. Polym. 2015, 122, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Alexandrescu, L.; Syverud, K.; Gatti, A.; Chinga-Carrasco, G. Cytotoxicity tests of cellulose nanofibril-based structures. Cellulose 2013, 20, 1765–1775. [Google Scholar] [CrossRef]
- Endes, C.; Mueller, S.; Kinnear, C.; Vanhecke, D.; Foster, E.J.; Petri-Fink, A.; Weder, C.; Clift, M.J.D.; Rothen-Rutishauser, B. Fate of Cellulose Nanocrystal Aerosols Deposited on the Lung Cell Surface In Vitro. Biomacromolecules 2015, 16, 1267–1275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sunasee, R.; Araoye, E.; Pyram, D.; Hemraz, U.D.; Boluk, Y.; Ckless, K. Cellulose nanocrystal cationic derivative induces NLRP3 inflammasome-dependent IL-1β secretion associated with mitochondrial ROS production. Biochem. Biophys. Rep. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Tummala, G.K.; Lopes, V.R.; Mihranyan, A.; Ferraz, N. Biocompatibility of Nanocellulose-Reinforced PVA Hydrogel with Human Corneal Epithelial Cells for Ophthalmic Applications. J. Funct. Biomater. 2019, 10, 35. [Google Scholar] [CrossRef] [Green Version]
- Nordli, H.R.; Chinga-Carrasco, G.; Rokstad, A.M.; Pukstad, B. Producing ultrapure wood cellulose nanofibrils and evaluating the cytotoxicity using human skin cells. Carbohydr. Polym. 2016, 150, 65–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ventura, C.; Lourenço, A.F.; Sousa-Uva, A.; Ferreira, P.J.; Silva, M.J. Evaluating the genotoxicity of cellulose nanofibrils in a co-culture of human lung epithelial cells and monocyte-derived macrophages. Toxicol. Lett. 2018, 291, 173–183. [Google Scholar] [CrossRef]
- DeLoid, G.M.; Cao, X.; Molina, R.M.; Silva, D.I.; Bhattacharya, K.; Ng, K.W.; Loo, S.C.J.; Brain, J.D.; Demokritou, P. Toxicological effects of ingested nanocellulose in in vitro intestinal epithelium and in vivo rat models. Environ. Sci. Nano 2019, 6, 2105–2115. [Google Scholar] [CrossRef] [PubMed]
- Tibolla, H.; Pelissari, F.; Martins, J.; Lanzoni, E.M.; Vicente, A.; Menegalli, F.; Cunha, R. Banana starch nanocomposite with cellulose nanofibers isolated from banana peel by enzymatic treatment: In vitro cytotoxicity assessment. Carbohydr. Polym. 2019, 207, 169–179. [Google Scholar] [CrossRef] [Green Version]
- Junka, A.; Bartoszewicz, M.; Dziadas, M.; Szymczyk, P.; Dydak, K.; Żywicka, A.; Owczarek, A.; Bil-Lula, I.; Czajkowska, J.; Fijałkowski, K. Application of bacterial cellulose experimental dressings saturated with gentamycin for management of bone biofilm in vitro and ex vivo. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 30–37. [Google Scholar] [CrossRef]
- Hobzova, R.; Hrib, J.; Sirc, J.; Karpushkin, E.; Michálek, J.; Janouskova, O.; Gatenholm, P. Embedding of Bacterial Cellulose Nanofibers within PHEMA Hydrogel Matrices: Tunable Stiffness Composites with Potential for Biomedical Applications. J. Nanomater. 2018, 2018, 5217095. [Google Scholar] [CrossRef] [Green Version]
- Noh, Y.K.; Costa, A.D.S.D.; Park, Y.S.; Du, P.; Kim, I.-H.; Park, K. Fabrication of bacterial cellulose-collagen composite scaffolds and their osteogenic effect on human mesenchymal stem cells. Carbohydr. Polym. 2019, 219, 210–218. [Google Scholar] [CrossRef]
- Ye, S.; Jiang, L.; Su, C.; Zhu, Z.; Wen, Y.; Shao, W. Development of gelatin/bacterial cellulose composite sponges as potential natural wound dressings. Int. J. Biol. Macromol. 2019, 133, 148–155. [Google Scholar] [CrossRef]
- Gorgieva, S.; Hribernik, S. Microstructured and Degradable Bacterial Cellulose–Gelatin Composite Membranes: Mineralization Aspects and Biomedical Relevance. Nanomaterials 2019, 9, 303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cacicedo, M.L.; Pacheco, G.; Islan, G.A.; Alvarez, V.A.; Barud, H.S.; Castro, G.R. Chitosan-bacterial cellulose patch of ciprofloxacin for wound dressing: Preparation and characterization studies. Int. J. Biol. Macromol. 2020, 147, 1136–1145. [Google Scholar] [CrossRef]
- Ilves, M.; Vilske, S.; Aimonen, K.; Lindberg, H.K.; Pesonen, S.; Wedin, I.; Nuopponen, M.; Vanhala, E.; Højgaard, C.; Winther, J.R.; et al. Nanofibrillated cellulose causes acute pulmonary inflammation that subsides within a month. Nanotoxicology 2018, 12, 729–746. [Google Scholar] [CrossRef]
- Roman, M. Toxicity of Cellulose Nanocrystals: A Review. Ind. Biotechnol. 2015, 11, 25–33. [Google Scholar] [CrossRef]
- Farcas, M.; Kisin, E.R.; Menas, A.L.; Gutkin, D.W.; Star, A.; Reiner, R.S.; Yanamala, N.; Savolainen, K.; Shvedova, A.A. Pulmonary exposure to cellulose nanocrystals caused deleterious effects to reproductive system in male mice. J. Toxicol. Environ. Health Part A 2016, 79, 984–997. [Google Scholar] [CrossRef] [Green Version]
- Shvedova, A.A.; Kisin, E.R.; Yanamala, N.; Farcas, M.; Menas, A.L.; Williams, A.; Fournier, P.M.; Reynolds, J.S.; Gutkin, D.W.; Star, A.; et al. Gender differences in murine pulmonary responses elicited by cellulose nanocrystals. Part. Fibre Toxicol. 2015, 13, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Catalán, J.; Rydman, E.; Aimonen, K.; Hannukainen, K.-S.; Suhonen, S.; Vanhala, E.; Moreno, C.; Meyer, V.; Perez, D.D.S.; Sneck, A.; et al. Genotoxic and inflammatory effects of nanofibrillated cellulose in murine lungs. Mutagenesis 2017, 32, 23–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hadrup, N.; Knudsen, K.B.; Berthing, T.; Wolff, H.; Bengtson, S.; Kofoed, C.; Espersen, R.; Højgaard, C.; Winther, J.R.; Willemoës, M.; et al. Pulmonary effects of nanofibrillated celluloses in mice suggest that carboxylation lowers the inflammatory and acute phase responses. Environ. Toxicol. Pharmacol. 2019, 66, 116–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindberg, H.K.; Catalán, J.; Aimonen, K.J.; Wolff, H.; Wedin, I.; Nuopponen, M.; Savolainen, K.M.; Norppa, H. Evaluation of the genotoxic potential of different types of nanofibrillated celluloses. Adv. Mater. TechConnect Brief 2017, 1, 229–232. [Google Scholar]
- Jeong, S.I.; Lee, S.E.; Yang, H.; Jin, Y.-H.; Park, C.-S.; Park, Y.S. Toxicologic evaluation of bacterial synthesized cellulose in endothelial cells and animals. Mol. Cell. Toxicol. 2010, 6, 370–377. [Google Scholar] [CrossRef]
- Piasecka-Zelga, J.; Zelga, P.; Szulc, J.; Wietecha, J.; Ciechańska, D. An in vivo biocompatibility study of surgical meshes made from bacterial cellulose modified with chitosan. Int. J. Biol. Macromol. 2018, 116, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Muhle, H.; Pott, F. Asbestos as reference material for fibre-induced cancer. Int. Arch. Occup. Environ. Health 2000, 73, S53–S59. [Google Scholar] [CrossRef]
- Rydman, E.M.; Ilves, M.; Koivisto, A.J.; Kinaret, P.A.S.; Fortino, V.; Savinko, T.S.; Lehto, M.T.; Pulkkinen, V.; Vippola, M.; Hämeri, K.J.; et al. Inhalation of rod-like carbon nanotubes causes unconventional allergic airway inflammation. Part. Fibre Toxicol. 2014, 11, 48. [Google Scholar] [CrossRef] [Green Version]
- Queirós, E.; Pinheiro, S.; Pereira, J.; Prada, J.; Pires, I.; Dourado, F.; Parpot, P.; Gama, M. Hemostatic Dressings Made of Oxidized Bacterial Nanocellulose Membranes. Polysaccharides 2021, 2, 6. [Google Scholar] [CrossRef]
- Goswami, P.; O’Haire, T. Developments in the use of green (biodegradable), recycled and biopolymer materials in technical nonwovens. In Advances in Technical Nonwovens; Elsevier BV: Amsterdam, The Netherlands, 2016; Volume 181, pp. 97–114. [Google Scholar]
- Ghalia, M.A.; Dahman, Y. Advanced nanobiomaterials in tissue engineering: Synthesis, properties, and applications. In Nanobiomaterials in Soft Tissue Engineering, 1st ed.; Grumezescu, A.M., Ed.; William Andrew Publishing: Norwich, NY, USA, 2016; Chapter 6; pp. 141–172. [Google Scholar]
- Lin, N.; Dufresne, A. Nanocellulose in biomedicine: Current status and future prospect. Eur. Polym. J. 2014, 59, 302–325. [Google Scholar] [CrossRef] [Green Version]
- Singh, G.; Chandoha-Lee, C.; Zhang, W.; Renneckar, S.; Vikesland, P.J.; Pruden, A. Biodegradation of nanocrystalline cellulose by two environmentally-relevant consortia. Water Res. 2016, 104, 137–146. [Google Scholar] [CrossRef]
- Shelke, N.B.; James, R.; Laurencin, C.T.; Kumbar, S.G. Polysaccharide biomaterials for drug delivery and regenerative engineering. Polym. Adv. Technol. 2014, 25, 448–460. [Google Scholar] [CrossRef]
- Athukoralalage, S.S.; Balu, R.; Dutta, N.K.; Choudhury, N.R. 3D Bioprinted Nanocellulose-Based Hydrogels for Tissue Engineering Applications: A Brief Review. Polymers 2019, 11, 898. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.; Catchmark, J.M. In vitro biodegradability and mechanical properties of bioabsorbable bacterial cellulose incorporating cellulases. Acta Biomater. 2011, 7, 2835–2845. [Google Scholar] [CrossRef] [PubMed]
- Jacek, P.; Dourado, F.; Gama, M.; Bielecki, S. Molecular aspects of bacterial nanocellulose biosynthesis. Microb. Biotechnol. 2019, 12, 633–649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yadav, V.; Paniliatis, B.J.; Shi, H.; Lee, K.; Cebe, P.; Kaplan, D.L. Novel In Vivo-Degradable Cellulose-Chitin Copolymer from Metabolically Engineered Gluconacetobacter xylinus. Appl. Environ. Microbiol. 2010, 76, 6257–6265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levanič, J.; Šenk, V.P.; Nadrah, P.; Poljanšek, I.; Oven, P.; Haapala, A. Analyzing TEMPO-Oxidized Cellulose Fiber Morphology: New Insights into Optimization of the Oxidation Process and Nanocellulose Dispersion Quality. ACS Sustain. Chem. Eng. 2020, 8, 17752–17762. [Google Scholar] [CrossRef]
- Isogai, A.; Hänninen, T.; Fujisawa, S.; Saito, T. Review: Catalytic oxidation of cellulose with nitroxyl radicals under aqueous conditions. Prog. Polym. Sci. 2018, 86, 122–148. [Google Scholar] [CrossRef]
- Yang, H.; Chen, D.; Van De Ven, T.G.M. Preparation and characterization of sterically stabilized nanocrystalline cellulose obtained by periodate oxidation of cellulose fibers. Cellulose 2015, 22, 1743–1752. [Google Scholar] [CrossRef]
- Czaja, W.; Kyryliouk, D.D.; De Paula, C.A.; Buechter, D.D. Oxidation of γ-irradiated microbial cellulose results in bioresorbable, highly conformable biomaterial. J. Appl. Polym. Sci. 2014, 131, 39995–40006. [Google Scholar] [CrossRef]
- Bulut, Y.; Aksit, A. A comparative study on chemical treatment of jute fiber: Potassium dichromate, potassium permanganate and sodium perborate trihydrate. Cellulose 2013, 20, 3155–3164. [Google Scholar] [CrossRef]
- Li, J.; Wan, Y.; Li, L.; Liang, H.; Wang, J. Preparation and characterization of 2,3-dialdehyde bacterial cellulose for potential biodegradable tissue engineering scaffolds. Mater. Sci. Eng. C 2009, 29, 1635–1642. [Google Scholar] [CrossRef]
- Elçin, A.E. In VitroandIn VivoDegradation of Oxidized Acetyl- and Ethyl-Cellulose Sponges. Artif. Cells Blood Substit. Biotechnol. 2006, 34, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Potter, M.J.; Chauhan, A.; Rowe, D. Surgicel: An effective tool to avoid free flap pedicle kinking in the head and neck. ANZ J. Surg. 2013, 83, 95–96. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Chen, L.; Hong, F.F. A Biodegradable Antibacterial Nanocomposite Based on Oxidized Bacterial Nanocellulose for Rapid Hemostasis and Wound Healing. ACS Appl. Mater. Interfaces 2019, 12, 3382–3392. [Google Scholar] [CrossRef]
- Sultana, T.; Van Hai, H.; Abueva, C.; Kang, H.J.; Lee, S.-Y.; Lee, B.-T. TEMPO oxidized nano-cellulose containing thermo-responsive injectable hydrogel for post-surgical peritoneal tissue adhesion prevention. Mater. Sci. Eng. C 2019, 102, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Song, S.H.; Kim, J.E.; Lee, Y.J.; Kwak, M.H.; Sung, G.Y.; Kwon, S.H.; Son, H.J.; Lee, H.S.; Jung, Y.J.; Hwang, D.Y. Cellulose film regenerated from Styela clava tunics have biodegradability, toxicity and biocompatibility in the skin of SD rats. J. Mater. Sci. Mater. Electron. 2014, 25, 1519–1530. [Google Scholar] [CrossRef] [PubMed]











| NCs Type | Drug Delivery System | Drug | Drug-Release Conditions | Drug Release Mechanism | Ref. |
|---|---|---|---|---|---|
| CNC | cCNC/SA double-membrane hydrogels | CH, EGF | PBS, pH 7.4, 37 °C; t90% = 3 days (CH); t90% = 4 to 8 days (EGF). | Swelling/erosion | [89] |
| TEMPO-oxidized CNC/CSos | PrHy, IMI | PBS, pH 7.4, room temp.; t40% = 12 min (PrHy); t80% = 2 h (IMI). | - | [90] | |
| CNC-HDQ complex | HDQ | dH2O, room temp., in the dark; t40% = 1 h; t80% = 4 h. | - | [91] | |
| CS/CNC nanocomposite hydrogels | C | SGF, pH 1.2, 37 °C; 120 min: 65% (0.5% CS/CNC); 50% (2.5% CS/CNC). | Ritger–Peppas model; n = 0.61–0.66; Non-Fickian diffusion. | [92] | |
| QC/cCNC/β-GP nanocomposite hydrogels | DOX | PBS, pH 7.4, 37 °C; t90% = 4 days (0% cCNC); t90% = 7 days (1% cCNC); t90% = 17 days (2.5% cCNC). | Swelling/erosion | [93] | |
| Gel/CNC nanocomposite hydrogels | TPh | SGF, pH 1.2, 37 °C; 24 h: 90% (5% CNC); 85% (10% CNC); 60% (25% CNC). | - | [94] | |
| m-CNC/Alg hydrogels | Ibu | PBS, pH 7.4, 37 °C; t = 0–30 min; 45%–60% burst release; t = 30–330 min; sustained release. | Fickian diffusion | [95] | |
| CNF | PDA/TEMPO-CNF composite hydrogels | TCH | PBS; “On-off” drug release under NIR irradiation; 120 min: 60% (pH 5.0); 30% (pH 7.4); 15 h: 70% (pH 5.0); 55% (pH 7.4). | Korsmeyer–Peppas model; Non-Fickian diffusion. | [96] |
| CNF/HPMC nanocomposites | KT | PBS, pH 7.4; 8 h: 95% (5% CNF), 62% (0.5% CNF), 56% (0.75% CNF), 37% (1% CNF). | Non-Fickian diffusion; n = 0.52–0.61. | [97] | |
| CNF/Alg hydrogels | MH | SGF, pH 1.2; SIF, pH 7.4, 37 °C; T40% = 90 min (CNF/Alg-50/50, SGF) t80% = 145 min (CNF/Alg-50/50, SIF). | Fickian diffusion mechanism | [98] | |
| BNC | BNC-SA hybrid hydrogels | Ibu | PBS, pH 1.5, 7.0 and 11.8; 37 °C; 24 h: 90% (pH 11.8); 80% (pH 7.0); and 60% (pH 1.5); PBS, pH 7.4; 0.15 V, 0.3 V, 0.5 V; 24 h: 95% (0.5 V); 85% (0.3 V and 0.15 V); 80% (0 V). | Korsmeyer–Peppas model; Non-Fickian diffusion; pH; n = 0.498–0.772; E-field; n = 0.700–0.491. | [99] |
| TCH-loaded BNC composites | TCH | HEPES buffers, pH 7, 37 °C; 3 h: ~100% (free TCH); 90% (0.5% TCH); 60% (0.3% TCH); 20% (0.1% TCH); 10% (0.05% TCH); | - | [100] | |
| OCT-loaded BNC | OCT | PBS, pH 7.4, 32 °C; 8 h: 82.7% ± 2.6% in first; 24 h 91.8% ± 2.0% after | Ritger–Peppas model; n = 0.51–0.55; Non-Fickian diffusion. | [101] | |
| PI-loaded BNC | PI | PI buffer, 32 °C; t84% = 48 h. | Ritger–Peppas model; n = 0.608–0.612 | [102] | |
| PHMB-loaded BNC | PHMB | PHMB buffer, 32 °C; t87% = 48 h. | Ritger–Peppas model; n = 0.863–0.871 | [102] |
| CNC, % | Drug-Loading Efficiency, % |
|---|---|
| 0 | 64.2 |
| 5 | 65.3 |
| 10 | 55.5 |
| 15 | 51.7 |
| 20 | 44.8 |
| 25 | 41.1 |
| NCs Type | TE Systems | Applications | References |
|---|---|---|---|
| CNF | CNF/CS nanocomposites | Artificial skin | [30] |
| CNF-based thixotropic gels | Breast cancer | [50] | |
| Double crosslinking 3D-printed CNF hydrogels | Skin TE | [115] | |
| CNF/PVA bilayer scaffold | Skin TE | [129] | |
| CNF/Gel/ApA | Bone TE | [130] | |
| CNC | CNC/PVA nanocomposites | Skin TE | [131] |
| Gel/HA/CNC hydrogels | Skin wound repair | [132] | |
| Col/CNC/GMs | Blood vessel | [133] | |
| PEG-grafted CNC nanocomposites | Bone TE | [134] | |
| CNC/PVA hybrid hydrogels | Soft TE | [135] | |
| CNC/PAAm composite hydrogels | TE | [136] | |
| a-CNC/Gel hydrogels composite | Breast cancer | [137] | |
| TEMPO-CNC reinforced PVA hydrogels | Corneal implant | [138] | |
| BNC | BNC/Fibrin composites | New blood vessel | [78] |
| BNC-Gel/HAp nanocomposites | Bone TE | [139] | |
| Alg/BNC/Col composite | TE | [140] | |
| 3D BNC/PMS scaffolds | TE; soft tissues regeneration | [141] | |
| DBC/Col-p | TE; tissues regeneration | [142] | |
| BNC/PA/Gel/HAp | Bone repair | [143] | |
| (BNC-Col)-Ap/OGP peptides | Bone TE | [144] | |
| BNC-CNTs composites | Bone regeneration | [145] | |
| BNC | Ear cartilage TE | [146] | |
| BNC/Alg bilayer composite | Neocartilage formation | [147] | |
| BNC/CS composites | Cartilage tissue regeneration | [148] |
| NCs Type | NC Source | In Vivo Models | In Vivo Experiments | Toxicological Results | Ref. |
|---|---|---|---|---|---|
| CNC | Wood pulp | Male C57BL/6 mice, 7–8 weeks old | PA: 40 μg/mouse/day, twice a week, for 3 weeks; Sperm chromatin structure assay and 23-Bio-Plex mouse cytokine assay. | Two-fold increase in HNE–protein adducts levels indicated testicular oxidative damage; Significantly elevated proinflammatory cytokines and chemokines. | [220] |
| CNC | Wood pulp | Male and female C57BL/6 mice, 7–8 weeks old | PA: 40 μg/mouse/day, twice a week, for 3 weeks; Bio-Plex system: 23-Plex cytokines/chemokines assay and TGF-β 3-plex assay. | After 3 months, pulmonary inflammation and damage elevated TGF-β and collagen levels in lung; Impaired pulmonary functions more pronounced in female compared to male mice. | [221] |
| CNC, CNF | Wood pulp | Female BALB/c mice, 7–8 weeks old | PA: 40 or 80 μg/mouse; one-time dose; Bio-Plex Pro Mouse Cytokine 23-plex assay. | After 14 days, BALF cytokines and cellular compositions were dose-dependently altered; No specific local or systemic immune cell polarization patterns; No “asbestos-like” behavior of NCs. | [198] |
| CNF | Softwood bleached kraft fibers | Wistar Han rats, 12 weeks old | G: 1% (w/w) susp. (10 mL/kg), twice weekly, for five weeks; Pierce LDH assay. | Little acute toxicity and likely “non-hazardous” behavior of ingested NFC in small quantities; Small inflammatory nodules in lungs of rats who had received food with CNF. | [210] |
| TEMPO- CNF | Spruce sulphite dissolving pulp | Female C57BL/6 mice, 7–8 weeks old | PA: 10, 40, 80 and 200 μg/mouse; one-time dose; Enzyme-linked immune-sorbent assay. | Acute inflammatory response and DNA damage in murine lungs at the lowest doses; The higher doses exhibited levels of damage similar to the untreated mice; No systemic toxicity or genotoxicity in the bone marrow. | [222] |
| CNF, AS-CNF | Wood pulp | Female C57BL/6, mice, 7–8 weeks old | Intratracheal instillation: 6 or 19 μg/mouse, one-time dose; Comet assay. | Pulmonary inflammation, genotoxicity and systemic acute phase response; Carboxylation reduces systemic acute phase response. | [223] |
| F-CNF, MC-CNF, AS-CNF, NS-CNF | Wood pulp | Female C57BL/6 mice, 7–8 weeks old | PA: 10, 40, 80 and 200 μg/mouse; one-time dose; Alkaline comet and micronucleus (MN) assays. | DNA damage in lungs, but no systemic genotoxicity for all NFCs, except AS-NFC; F-NFC induces a dose-dependent response in lung cells at 24 h and 28 days post-exposure. | [224] |
| CNF, MC-CNF, AS-CNF | Wood pulp | Female C57BL/6 mice, 7–8 weeks old | OPA: 10 or 40 μg/mouse; one-time dose; Commercial human IL-1β and TNF-α ELISA kits. | Induced immunity response, after 24 h, for all NFCs; Non-functionalized NFCs caused Th2-type inflammation; Modest immune reactions after 28 days. | [218] |
| BC | G. xylinus | Male C57/Bl6 mice, 9 weeks old | Intraperitoneally injection: 0.5 and 5 mg BC/200 μL PBS. Biochemical parameter tests. | After 7 days, none of the parameters tested (albumin, total cholesterol, aspartate aminotransferase, alanine transaminase and triglyceride) were affected by the BC presence; BC is nontoxic and did not produce any adverse effects in body or organ weight. | [225] |
| BC | Sugar cane molasses | Adult Webster male and female mice, 85 days old | G: 2000 mg BC 0.8%/kg bw/d, for 3 consecutive days; MN assay. | BC cause no alteration of the PCE/NCE ratio; Protective effect against CP-induced myelotoxicity and enotoxicity. | [193] |
| BC-, MBC-PP meshes | A. xylinum | Han Wistar rats and Albino rabbits, both sexes, 2–3 months old; Dunkin-Hartley guinea pigs, 3 months old | PP meshes, BC-, and MBC-coated meshes implantation into the pocket of panniculus camosus muscles along the dorsal midline for a one-month period. | BC- and MBC-coated meshes evoke the lowest immune response to surrounding tissue after implantation; The tested material neither cause any allergic or significant intradermal reactions nor pathological changes in internal organs. | [226] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicu, R.; Ciolacu, F.; Ciolacu, D.E. Advanced Functional Materials Based on Nanocellulose for Pharmaceutical/Medical Applications. Pharmaceutics 2021, 13, 1125. https://doi.org/10.3390/pharmaceutics13081125
Nicu R, Ciolacu F, Ciolacu DE. Advanced Functional Materials Based on Nanocellulose for Pharmaceutical/Medical Applications. Pharmaceutics. 2021; 13(8):1125. https://doi.org/10.3390/pharmaceutics13081125
Chicago/Turabian StyleNicu, Raluca, Florin Ciolacu, and Diana E. Ciolacu. 2021. "Advanced Functional Materials Based on Nanocellulose for Pharmaceutical/Medical Applications" Pharmaceutics 13, no. 8: 1125. https://doi.org/10.3390/pharmaceutics13081125