Sonoporation Using Nanoparticle-Loaded Microbubbles Increases Cellular Uptake of Nanoparticles Compared to Co-Incubation of Nanoparticles and Microbubbles
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Synthesis of Polymeric Nanoparticles
2.3. Synthesis of Microbubbles
2.4. Experimental Setup and Ultrasound Treatment
2.5. Sonoporation Experiments
2.6. Confocal Imaging
2.7. Image and Data Analysis
3. Results
4. Discussion
4.1. Comparison of Microbubbles
4.2. Effect of Ultrasound Parameters
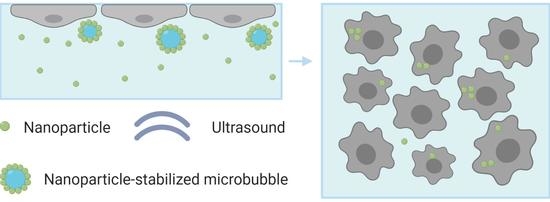
4.3. Delivery Mechanisms
4.4. Clinical Relevance
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kooiman, K.; Vos, H.J.; Versluis, M.; de Jong, N. Acoustic Behavior of Microbubbles and Implications for Drug Delivery. Adv. Drug Deliv. Rev. 2014, 72, 28–48. [Google Scholar] [CrossRef] [PubMed]
- Lajoinie, G.; De Cock, I.; Coussios, C.C.; Lentacker, I.; Le Gac, S.; Stride, E.; Versluis, M. In Vitro Methods to Study Bubble-Cell Interactions: Fundamentals and Therapeutic Applications. Biomicrofluidics 2016, 10, 011501. [Google Scholar] [CrossRef] [Green Version]
- Versluis, M.; Stride, E.; Lajoinie, G.; Dollet, B.; Segers, T. Ultrasound Contrast Agent Modeling: A Review. Ultrasound Med. Biol. 2020, 46, 2117–2144. [Google Scholar] [CrossRef] [PubMed]
- Stride, E.; Segers, T.; Lajoinie, G.; Cherkaoui, S.; Bettinger, T.; Versluis, M.; Borden, M. Microbubble Agents: New Directions. Ultrasound Med. Biol. 2020, 46, 1326–1343. [Google Scholar] [CrossRef] [PubMed]
- Frenkel, V. Ultrasound Mediated Delivery of Drugs and Genes to Solid Tumors. Adv. Drug Deliv. Rev. 2008, 60, 1193–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roovers, S.; Segers, T.; Lajoinie, G.; Deprez, J.; Versluis, M.; De Smedt, S.C.; Lentacker, I. The Role of Ultrasound-Driven Microbubble Dynamics in Drug Delivery: From Microbubble Fundamentals to Clinical Translation. Langmuir 2019, 35, 10173–10191. [Google Scholar] [CrossRef] [PubMed]
- Leighton, T.G. What is Ultrasound? Prog. Biophys. Mol. Biol. 2007, 93, 3–83. [Google Scholar] [CrossRef] [PubMed]
- Postema, M.; van Wamel, A.; Lancee, C.T.; de Jong, N. Ultrasound-Induced Encapsulated Microbubble Phenomena. Ultrasound Med. Biol. 2004, 30, 827–840. [Google Scholar] [CrossRef] [PubMed]
- Marmottant, P.; Hilgenfeldt, S. Controlled Vesicle Deformation and Lysis by Single Oscillating Bubbles. Nature 2003, 423, 153–156. [Google Scholar] [CrossRef]
- Lentacker, I.; De Cock, I.; Deckers, R.; De Smedt, S.C.; Moonen, C.T. Understanding Ultrasound Induced Sonoporation: Definitions and Underlying Mechanisms. Adv. Drug Deliv. Rev. 2014, 72, 49–64. [Google Scholar] [CrossRef] [Green Version]
- Prentice, P.; Cuschieri, A.; Dholakia, K.; Prausnitz, M.; Campbell, P. Membrane Disruption by Optically Controlled Microbubble Cavitation. Nat. Phys. 2005, 1, 107–110. [Google Scholar] [CrossRef] [Green Version]
- Delalande, A.; Kotopoulis, S.; Postema, M.; Midoux, P.; Pichon, C. Sonoporation: Mechanistic Insights and Ongoing Challenges for Gene Transfer. Gene 2013, 525, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Van Wamel, A.; Kooiman, K.; Harteveld, M.; Emmer, M.; ten Cate, F.J.; Versluis, M.; de Jong, N. Vibrating Microbubbles Poking Individual Cells: Drug Transfer into Cells via Sonoporation. J. Control. Release 2006, 112, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Kotopoulis, S.; Postema, M. Microfoam Formation in a Capillary. Ultrasonics 2010, 50, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Dayton, P.A.; Allen, J.S.; Ferrara, K.W. The Magnitude of Radiation Force on Ultrasound Contrast Agents. J. Acoust. Soc. Am. 2002, 112, 2183–2192. [Google Scholar] [CrossRef] [PubMed]
- Castle, J.; Butts, M.; Healey, A.; Kent, K.; Marino, M.; Feinstein, S.B. Ultrasound-Mediated Targeted Drug Delivery: Recent Success and Remaining Challenges. Am. J. Physiol. Heart Circ. Physiol. 2013, 304, H350–H357. [Google Scholar] [CrossRef]
- Snipstad, S.; Sulheim, E.; de Lange Davies, C.; Moonen, C.; Storm, G.; Kiessling, F.; Schmid, R.; Lammers, T. Sonopermeation to Improve Drug Delivery to Tumors: From Fundamental Understanding to Clinical Translation. Expert Opin. Drug Deliv. 2018, 15, 1249–1261. [Google Scholar] [CrossRef]
- Wang, S.; Olumolade, O.O.; Sun, T.; Samiotaki, G.; Konofagou, E.E. Noninvasive, Neuron-Specific Gene Therapy Can be Facilitated by Focused Ultrasound and Recombinant Adeno-Associated Virus. Gene Ther. 2015, 22, 104–110. [Google Scholar] [CrossRef] [Green Version]
- Kooiman, K.; Foppen-Harteveld, M.; van der Steen, A.F.; de Jong, N. Sonoporation of Endothelial Cells by Vibrating Targeted Microbubbles. J. Control. Release 2011, 154, 35–41. [Google Scholar] [CrossRef]
- Helfield, B.; Chen, X.; Watkins, S.C.; Villanueva, F.S. Biophysical Insight into Mechanisms of Sonoporation. Proc. Natl. Acad. Sci. USA 2016, 113, 9983–9988. [Google Scholar] [CrossRef] [Green Version]
- Escoffre, J.M.; Piron, J.; Novell, A.; Bouakaz, A. Doxorubicin Delivery into Tumor Cells with Ultrasound and Microbubbles. Mol. Pharm. 2011, 8, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Skachkov, I.; Luan, Y.; van der Steen, A.; de Jong, N.; Kooiman, K. Targeted Microbubble Mediated Sonoporation of Endothelial Cells in Vivo. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2014, 61, 1661–1667. [Google Scholar] [CrossRef] [PubMed]
- Meijering, B.D.; Juffermans, L.J.; van Wamel, A.; Henning, R.H.; Zuhorn, I.S.; Emmer, M.; Versteilen, A.M.; Paulus, W.J.; van Gilst, W.H.; Kooiman, K.; et al. Ultrasound and Microbubble-Targeted Delivery of Macromolecules is Regulated by Induction of Endocytosis and Pore Formation. Circ. Res. 2009, 104, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Afadzi, M.; Strand, S.P.; Nilssen, E.A.; Måsøy, S.E.; Johansen, T.F.; Hansen, R.; Angelsen, B.A.; de Lange Davies, C. Mechanisms of the Ultrasound-Mediated Intracellular Delivery of Liposomes and Dextrans. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2013, 60, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Idone, V.; Tam, C.; Goss, J.W.; Toomre, D.; Pypaert, M.; Andrews, N.W. Repair of Injured Plasma Membrane by Rapid Ca2+-Dependent Endocytosis. J. Cell Biol. 2008, 180, 905–914. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Leow, R.S.; Hu, Y.; Wan, J.M.; Yu, A.C. Single-Site Sonoporation Disrupts Actin Cytoskeleton Organization. J. R. Soc. Interface 2014, 11, 20140071. [Google Scholar] [CrossRef] [Green Version]
- Nejad, S.M.; Hosseini, H.; Akiyama, H.; Tachibana, K. Reparable Cell Sonoporation in Suspension: Theranostic Potential of Microbubble. Theranostics 2016, 6, 446–455. [Google Scholar] [CrossRef]
- Fan, Z.; Chen, D.; Deng, C.X. Improving Ultrasound Gene Transfection Efficiency by Controlling Ultrasound Excitation of Microbubbles. J. Control. Release 2013, 170, 401–413. [Google Scholar] [CrossRef] [Green Version]
- Fan, Z.; Liu, H.; Mayer, M.; Deng, C.X. Spatiotemporally Controlled Single Cell Sonoporation. Proc. Natl. Acad. Sci. USA 2012, 109, 16486–16491. [Google Scholar] [CrossRef] [Green Version]
- Karshafian, R.; Samac, S.; Bevan, P.D.; Burns, P.N. Microbubble Mediated Sonoporation of Cells in Suspension: Clonogenic Viability and Influence of Molecular Size on Uptake. Ultrasonics 2010, 50, 691–697. [Google Scholar] [CrossRef]
- Burke, C.W.; Alexander, E., IV; Timbie, K.; Kilbanov, A.L.; Price, R.J. Ultrasound-Activated Agents Comprised of 5FU-Bearing Nanoparticles Bonded to Microbubbles Inhibit Solid Tumor Growth and Improve Survival. Mol. Ther. 2014, 22, 321–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burke, C.W.; Hsiang, Y.H.; Alexander, E., IV; Kilbanov, A.L.; Price, R.J. Covalently Linking Poly(Lactic-co-glycolic Acid) Nanoparticles to Microbubbles before Intravenous Injection Improves Their Ultrasound-Targeted Delivery to Skeletal Muscle. Small 2011, 7, 1227–1235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Cock, I.; Lajoinie, G.; Versluis, M.; De Smedt, S.C.; Lentacker, I. Sonoprinting and the Importance of Microbubble Loading for the Ultrasound Mediated Cellular Delivery of Nanoparticles. Biomaterials 2016, 83, 294–307. [Google Scholar] [CrossRef] [PubMed]
- Roovers, S.; Deprez, J.; Priwitaningrum, D.; Lajoinie, G.; Rivron, N.; Declercq, H.; De Wever, O.; Stride, E.; Le Gac, S.; Versluis, M.; et al. Sonoprinting Liposomes on Tumor Spheroids by Microbubbles and Ultrasound. J. Control. Release 2019, 316, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Roovers, S.; Lajoinie, G.; De Cock, I.; Brans, T.; Dewitte, H.; Braeckmans, K.; Versuis, M.; De Smedt, S.C.; Lentacker, I. Sonoprinting of Nanoparticle-Loaded Microbubbles: Unraveling the Multi-Timescale Mechanism. Biomaterials 2019, 217, 119250. [Google Scholar] [CrossRef] [Green Version]
- Vandenbroucke, R.E.; Lentacker, I.; Demeester, J.; De Smedt, S.C.; Sanders, N.N. Ultrasound Assisted siRNA Delivery Using PEG-siPlex Loaded Microbubbles. J. Control. Release 2008, 126, 265–273. [Google Scholar] [CrossRef] [Green Version]
- Snipstad, S.; Berg, S.; Morch, Y.; Bjorkoy, A.; Sulheim, E.; Hansen, R.; Grimstad, I.; van Wamel, A.; Maaland, A.F.; Torp, S.H.; et al. Ultrasound Improves the Delivery and Therapeutic Effect of Nanoparticle-Stabilized Microbubbles in Breast Cancer Xenografts. Ultrasound Med. Biol. 2017, 43, 2651–2669. [Google Scholar] [CrossRef] [Green Version]
- Yemane, P.T.; Aslund, A.K.O.; Snipstad, S.; Bjorkoy, A.; Grendstad, K.; Berg, S.; Morch, Y.; Torp, S.H.; Hansen, R.; de Lange Davies, C. Effect of Ultrasound on the Vasculature and Extravasation of Nanoscale Particles Imaged in Real Time. Ultrasound Med. Biol. 2019, 45, 3028–3041. [Google Scholar] [CrossRef] [Green Version]
- Snipstad, S.; Mørch, Ý.; Sulheim, E.; Åslund, A.; Pedersen, A.; de Lange Davies, C.; Berg, S. Sonopermeation Enhances Uptake and Therapeutic Effect of Free and Encapsulated Cabazitaxel. Ultrasound Med. Biol. 2021, 47, 1319–1333. [Google Scholar] [CrossRef]
- Sulheim, E.; Morch, Y.; Snipstad, S.; Borgos, S.E.; Miletic, H.; Bjerkvig, R.; de Lange Davies, C.; Aslund, A.K.O. Therapeutic Effect of Cabazitaxel and Blood-Brain Barrier Opening in a Patient-Derived Glioblastoma Model. Nanotheranostics 2019, 3, 103–112. [Google Scholar] [CrossRef] [Green Version]
- Åslund, A.K.O.; Berg, S.; Hak, S.; Mørch, Ý.; Torp, S.H.; Sandvig, A.; Widerøe, M.; Hansen, R.; de Lange Davies, C. Nanoparticle Delivery to the Brain--By Focused Ultrasound and Self-Assembled Nanoparticle-Stabilized Microbubbles. J. Control. Release 2015, 220, 287–294. [Google Scholar] [CrossRef]
- Baghirov, H.; Snipstad, S.; Sulheim, E.; Berg, S.; Hansen, R.; Thorsen, F.; Morch, Y.; de Lange Davies, C.; Aslund, A.K.O. Ultrasound-Mediated Delivery and Distribution of Polymeric Nanoparticles in the Normal Brain Parenchyma of a Metastatic Brain Tumour Model. PLoS ONE 2018, 13, e0191102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Snipstad, S.; Hak, S.; Baghirov, H.; Sulheim, E.; Mørch, Ý.; Lélu, S.; von Haartman, E.; Bäck, M.; Nilsson, K.P.R.; Klymchenko, A.S.; et al. Labeling Nanoparticles: Dye Leakage and Altered Cellular Uptake. Cytom. A 2016, 91, 760–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mørch, Ý.; Hansen, R.; Berg, S.; Åslund, A.K.O.; Glomm, W.R.; Eggen, S.; Schmid, R.B.; Johnsen, H.; Kubowicz, S.; Snipstad, S.; et al. Nanoparticle-Stabilized Microbubbles for Multimodal Imaging and Drug Delivery. Contrast Media Mol. Imaging 2015, 10, 356–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klymchenko, A.S.; Roger, E.; Anton, N.; Anton, H.; Shulov, I.; Vermot, J.; Mely, Y.; Vandamme, T.F. Highly Lipophilic Fluorescent Dyes in Nano-Emulsions: Towards Bright Non-Leaking Nano-Droplets. RSC Adv. 2012, 2, 11876–11886. [Google Scholar] [CrossRef] [Green Version]
- Sulheim, E.; Baghirov, H.; von Haartman, E.; Bøe, A.; Åslund, A.K.O.; Mørch, Ý.; de Lange Davies, C. Cellular Uptake and Intracellular Degradation of Poly(Alkyl Cyanoacrylate) Nanoparticles. J. Nanobiotechnology 2016, 14, 1. [Google Scholar] [CrossRef] [Green Version]
- Sulheim, E.; Iversen, T.G.; To Nakstad, V.; Klinkenberg, G.; Sletta, H.; Schmid, R.; Hatletveit, A.R.; Wagbo, A.M.; Sundan, A.; Skotland, T.; et al. Cytotoxicity of Poly(Alkyl Cyanoacrylate) Nanoparticles. Int. J. Mol. Sci. 2017, 18, 2454. [Google Scholar] [CrossRef] [Green Version]
- Åslund, A.K.O.; Sulheim, E.; Snipstad, S.; von Haartman, E.; Baghirov, H.; Starr, N.J.; Kvåle Løvmo, M.; Lelu, S.; Scurr, D.J.; de Lange Davies, C.; et al. Quantification and Qualitative Effects of Different PEGylations on Poly(Butyl Cyanoacrylate) Nanoparticles. Mol. Pharm. 2017, 14, 2560–2569. [Google Scholar] [CrossRef] [Green Version]
- Sontum, P.C. Physicochemical Characteristics of Sonazoid, a New Contrast Agent for Ultrasound Imaging. Ultrasound Med. Biol. 2008, 34, 824–833. [Google Scholar] [CrossRef]
- Nawijn, C.; Segers, T.; Lajoinie, G.; Mørch, Ý.; Berg, S.; Snipstad, S.; de Lange Davies, C.; Versluis, M. Multi-Time-Scale Microscopy Methods for the Characterization of Fluorescently-Labeled Microbubbles Aimed at Ultrasound-Triggered Drug Release; JoVE: Cambridge, MA, USA, 2021. [Google Scholar]
- Schlicher, R.K.; Radhakrishna, H.; Tolentino, T.P.; Apkarian, R.P.; Zarnitsyn, V.; Prausnitz, M.R. Mechanism of Intracellular Delivery by Acoustic Cavitation. Ultrasound Med. Biol. 2006, 32, 915–924. [Google Scholar] [CrossRef]
- Zhou, Y.; Shi, J.; Cui, J.; Deng, C.X. Effects of Extracellular Calcium on Cell Membrane Resealing in Sonoporation. J. Control. Release 2008, 126, 34–43. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.; Wan, J.M.; Yu, A.C. Membrane Perforation and Recovery Dynamics in Microbubble-Mediated Sonoporation. Ultrasound Med. Biol. 2013, 39, 2393–2405. [Google Scholar] [CrossRef]
- Luan, Y.; Lajoinie, G.; Gelderblom, E.; Skachkov, I.; van der Steen, A.F.; Vos, H.J.; Versluis, M.; De Jong, N. Lipid Shedding from Single Oscillating Microbubbles. Ultrasound Med. Biol. 2014, 40, 1834–1846. [Google Scholar] [CrossRef]
- Collis, J.; Manasseh, R.; Liovic, P.; Tho, P.; Ooi, A.; Petkovic-Duran, K.; Zhu, Y. Cavitation Microstreaming and Stress Fields Created by Microbubbles. Ultrasonics 2010, 50, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Bloch, S.H.; Wan, M.; Dayton, P.A.; Ferrara, K.W. Optical Observation of Lipid-and Polymer-Shelled Ultrasound Microbubble Contrast Agents. Appl. Phys. Lett. 2004, 84, 631–633. [Google Scholar] [CrossRef] [Green Version]
- Bouakaz, A.; Versluis, M.; de Jong, N. High-Speed Optical Observations of Contrast Agent Destruction. Ultrasound Med. Biol. 2005, 31, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Luan, Y.; Faez, T.; Gelderblom, E.; Skachkov, I.; Geers, B.; Lentacker, I.; van der Steen, T.; Versluis, M.; de Jong, N. Acoustical Properties of Individual Liposome-Loaded Microbubbles. Ultrasound Med. Biol. 2012, 38, 2174–2185. [Google Scholar] [CrossRef] [PubMed]
- Doinikov, A.A.; Haac, J.F.; Dayton, P.A. Resonance Frequencies of Lipid-Shelled Microbubbles in the Regime of Nonlinear Oscillations. Ultrasonics 2009, 49, 263–268. [Google Scholar] [CrossRef] [Green Version]
- Ibsen, S.; Shi, G.; Schutt, C.; Shi, L.; Suico, K.D.; Benchimol, M.; Serra, V.; Simberg, D.; Berns, M.; Esener, S. The Behavior of Lipid Debris Left on Cell Surfaces from Microbubble Based Ultrasound Molecular Imaging. Ultrasonics 2014, 54, 2090–2098. [Google Scholar] [CrossRef] [Green Version]
- Wang, T.Y.; Choe, J.W.; Pu, K.Y.; Devulapally, R.; Bachawal, S.; Machtaler, S.; Chowdhury, S.M.; Luong, R.; Tian, L.; Khuri-Yakub, B.; et al. Ultrasound-Guided Delivery of microRNA Loaded Nanoparticles into Cancer. J. Control. Release 2015, 203, 99–108. [Google Scholar] [CrossRef] [Green Version]
- Qiu, Y.; Luo, Y.; Zhang, Y.; Cui, W.; Zhang, D.; Wu, J.; Zhang, J.; Tu, J. The Correlation between Acoustic Cavitation and Sonoporation Involved in Ultrasound-Mediated DNA Transfection with Polyethylenimine (PEI) in Vitro. J. Control. Release 2010, 145, 40–48. [Google Scholar] [CrossRef]
- Chen, H.; Konofagou, E.E. The Size of Blood-Brain Barrier Opening Induced by Focused Ultrasound is Dictated by the Acoustic Pressure. J. Cereb. Blood Flow Metab. 2014, 34, 1197–1204. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Yang, K.; Cui, J.; Ye, J.Y.; Deng, C.X. Controlled Permeation of Cell Membrane by Single Bubble Acoustic Cavitation. J. Control. Release 2012, 157, 103–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kokhuis, T.J.; Garbin, V.; Kooiman, K.; Naaijkens, B.A.; Juffermans, L.J.; Kamp, O.; van der Steen, A.F.; Versluis, M.; de Jong, N. Secondary Bjerknes Forces Deform Targeted Microbubbles. Ultrasound Med. Biol. 2013, 39, 490–506. [Google Scholar] [CrossRef]
- Qin, P.; Jin, L.; Li, F.; Han, T.; Du, L.; Yu, A.C.H. The Relationship between Microbubble Size and Heterogeneous Sonoporation at the Single-Cell Level. In Proceedings of the IEEE International Ultrasonics Symposium Proceedings, Tours, France, 18–21 September 2016. [Google Scholar]
- Kokhuis, T.J.A.; Skachkov, I.; Naaijkens, B.A.; Juffermans, L.J.M.; Kamp, O.; Kooiman, K.; van der Steen, A.F.W.; Versluis, M.; de Jong, N. Intravital Microscopy of Localized Stem Cell Delivery Using Microbubbles and Acoustic Radiation Force. Biotechnol. Bioeng. 2015, 112, 220–227. [Google Scholar] [CrossRef]
- Fernandes, D.A.; Fernandes, D.D.; Li, Y.; Wang, Y.; Zhang, Z.; Rousseau, D.; Gradinaru, C.C.; Kolios, M.C. Synthesis of Stable Multifunctional Perfluorocarbon Nanoemulsions for Cancer Therapy and Imaging. Langmuir 2016, 32, 10870–10880. [Google Scholar] [CrossRef] [PubMed]
- Kwan, J.J.; Myers, R.; Coviello, C.M.; Graham, S.M.; Shah, A.R.; Stride, E.; Carlisle, R.C.; Coussios, C.C. Ultrasound-Propelled Nanocups for Drug Delivery. Small 2015, 11, 5305–5314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, K.; Walker, W.R.; Williams, R.; Tremblay-Darveau, C.; Burns, P.N.; Sheeran, P.S. Impact of Encapsulation on in Vitro and in Vivo Performance of Volatile Nanoscale Phase-Shift Perfluorocarbon Droplets. Ultrasound Med. Biol. 2018, 44, 1836–1852. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, N. Drug-Loaded Perfluorocarbon Nanodroplets for Ultrasound-Mediated Drug Delivery. Adv. Exp. Med. Biol. 2016, 880, 221–241. [Google Scholar] [CrossRef] [PubMed]
- Unger, E.; Porter, T.; Lindner, J.; Grayburn, P. Cardiovascular Drug Delivery with Ultrasound and Microbubbles. Adv. Drug Deliv. Rev. 2014, 72, 110–126. [Google Scholar] [CrossRef]
- Mayer, C.R.; Bekeredjian, R. Ultrasonic Gene and Drug Delivery to the Cardiovascular System. Adv. Drug Deliv. Rev. 2008, 60, 1177–1192. [Google Scholar] [CrossRef] [PubMed]
- Dewitte, H.; Van Lint, S.; Heirman, C.; Thielemans, K.; De Smedt, S.C.; Breckpot, K.; Lentacker, I. The Potential of Antigen and TriMix Sonoporation Using mRNA-Loaded Microbubbles for Ultrasound-Triggered Cancer Immunotherapy. J. Control. Release 2014, 194, 28–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]








Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Snipstad, S.; Hanstad, S.; Bjørkøy, A.; Mørch, Ý.; de Lange Davies, C. Sonoporation Using Nanoparticle-Loaded Microbubbles Increases Cellular Uptake of Nanoparticles Compared to Co-Incubation of Nanoparticles and Microbubbles. Pharmaceutics 2021, 13, 640. https://doi.org/10.3390/pharmaceutics13050640
Snipstad S, Hanstad S, Bjørkøy A, Mørch Ý, de Lange Davies C. Sonoporation Using Nanoparticle-Loaded Microbubbles Increases Cellular Uptake of Nanoparticles Compared to Co-Incubation of Nanoparticles and Microbubbles. Pharmaceutics. 2021; 13(5):640. https://doi.org/10.3390/pharmaceutics13050640
Chicago/Turabian StyleSnipstad, Sofie, Sigurd Hanstad, Astrid Bjørkøy, Ýrr Mørch, and Catharina de Lange Davies. 2021. "Sonoporation Using Nanoparticle-Loaded Microbubbles Increases Cellular Uptake of Nanoparticles Compared to Co-Incubation of Nanoparticles and Microbubbles" Pharmaceutics 13, no. 5: 640. https://doi.org/10.3390/pharmaceutics13050640